Abstract
Studies examining physical activity behavior suggest that activity levels decline with age. Such declines are particularly problematic among older adults in light of the research suggesting a protective effect of physical activity on numerous physical health outcomes associated with independent living. Despite a growing recognition of the importance of a physically active lifestyle, little is known about the role of demographic and psychosocial variables on this trajectory of change. In this study, the roles played by outcome expectations, self-efficacy, and functional limitations on changes in physical activity levels over a 2-year period in older women were assessed using latent growth curve modeling. Data were obtained from 249 community-dwelling older women (M age = 68.12, n = 81 Black, and n = 168 White). Demographic, health status, and psychosocial data were collected via self-report upon entry into the study. Self-reported physical activity was assessed at baseline and again at 12 and 24 months. As expected, physical activity declined over the 2-year period. Self-efficacy demonstrated an indirect association with the trajectory of decline in physical activity through functional limitations. Importantly, the pattern of relationships appears independent of demographic factors and chronic health conditions.
Keywords: Physical activity, Social cognitive, Women
In a recent position article from the Centers for Disease Control and Prevention's Healthy Aging Network, Prohaska and colleagues (2006) identified four key questions relative to physical activity, public health, and aging. One of those questions reflected the need to identify factors influencing the physical activity patterns of older adults. Additionally, little is known relative to which factors influence the change in activity over time. Prohaska and colleagues further recommended that existing models and theories be expanded to incorporate factors associated with the aging process, including disability and functional limitations, and to examine these processes in subgroups of aging adults.
Although social cognitive theory (Bandura, 1986, 1997) has been one of the most frequently used theoretical models for understanding physical activity behavior, these applications have rarely incorporated more than one or two model constructs. Indeed, self-efficacy is often relied upon as the sole social cognitive determinant of physical activity. However, the social cognitive model hypothesizes that self-efficacy has both direct and indirect influences on behavioral outcomes. In a recent article, Bandura (2004) clearly articulates that the theoretical pathways from self-efficacy to behavioral outcomes are both direct and indirect. The indirect pathways are proposed to operate through a number of social cognitive constructs including outcome expectations, goals, and facilitators and impediments to behavioral performance. Individuals with higher levels of self-efficacy have more positive expectations about what the behavior will bring about, set higher goals for themselves, and are more likely to take the view that they are capable of overcoming difficulties and barriers with effort and coping skills.
Although many studies have used a social cognitive framework to understand an array of health behaviors, most of them have adopted one of two approaches. That is, a minimum set of social cognitive variables, often only self-efficacy, have been either correlated with current behavior or used at one point in time to predict behavior prospectively at a later point in time. It has been very rare that a more complete set of social cognitive variables have been used to predict subsequent trajectories of change in health behaviors such as physical activity. Given that physical activity levels typically decline with age, it is important to try to identify factors that might contribute to this pattern of decline. The information gathered from such an approach may be of particular importance in designing activity programs for older adults by focusing on those modifiable factors that are amenable to change and influence behavior over time.
Self-efficacy has consistently been associated with the adoption and maintenance of physical activity behavior in older adults (McAuley & Blissmer, 2000; McAuley et al., 2007). Moreover, efficacy beliefs have been significantly associated with functional limitations and disability (McAuley, Konopack, Motl, Rosengren, & Morris, 2005; Seeman & Chen, 2002). Outcome expectations, in the form of perceived benefits, have also been associated with physical activity (King, 2001; Williams, Anderson, & Winett, 2005) but on a less consistent basis than self-efficacy. These benefits can take the form of physical, social, or self-evaluative outcomes. Although physical activity has been suggested to confer a protective benefit against functional limitations associated with mobility, reaching and lifting, and balance in older adults (Keysor, 2003), the case might be successfully made that such limitations represent a real and significant barrier or impediment to being physically active (Morris, McAuley, & Motl, 2008). Importantly, women are less active than their male counterparts across the lifespan and also report a higher prevalence of age-related functional impairments than do men (Centers for Disease Control and Prevention [CDC], 1992–2004). Indeed, the prevalence of functional limitations and disability among community-dwelling older adults is considerable, with 84% of persons aged 65 years or older reporting difficulties with activities of daily living or instrumental activities of daily living (Fried & Guralnik, 1997).
As implied by Prohaska and colleagues (2006), applications of social cognitive theory do not typically take into account the part to be played by demographic characteristics and health conditions in understanding the patterns of physical activity. For example, the lowest levels of physical activity participation are found in adults of poorer socioeconomic status (SES; Sproston & Primatesta, 2004), and fewer exercise facilities are found in low SES neighborhoods (Estabrooks, Lee, & Gyurcsik, 2003). Additionally, individuals from minority groups are less active than Whites (CDC, 2005), and chronic health conditions, such as diabetes, cardiovascular disease, and hyperlipidemia and hypertension, consistently covary with sedentary behavior (Schutzer & Graves, 2004). Thus, it would appear important to examine whether the relationships hypothesized by social cognitive theory hold up when controlling for such factors.
The objectives of the present study were (a) to examine the trajectory of change in physical activity across a 2-year period in a sample of community-dwelling older women; (b) to examine the role played by self-efficacy, outcome expectations, and functional limitations as predictors of changes in physical activity levels in older women over a 2-year period; and (c) to determine whether demographic and chronic health conditions influenced these relationships. We hypothesized that physical activity would decline over time in the absence of any intervention. In addition, it was hypothesized that baseline social cognitive factors would be predictive of these declines over time. Specifically, more efficacious women at baseline would report fewer functional limitations and have more positive outcome expectations and, subsequently, less of a decline in physical activity across a 2-year period. Second, it was hypothesized that self-efficacy would have a direct association with declines in physical activity in addition to the hypothesized indirect associations through functional limitations and outcome expectations. Finally, it was hypothesized that the proposed social cognitive model of declines in activity across time would be supported when controlling for demographic and chronic disease factors.
Methods
Participants
Older women (M age = 68.12, range 59–84 years; N = 249; Black = 81 and White = 168) were recruited via advertisements in the local media to participate in a study of women’s health. Of the 249 participants who entered the study at baseline, 231 (92.8% of total sample) and 217 (86.3% of total sample) women agreed to participate at 12- and 24-month follow-up, respectively. All procedures were approved by a University Institutional Review Board, and written informed consent was obtained from each participant prior to enrollment in the study.
Measures
Demographic and health information.
Basic demographic data including age, education, household income, and race (Black or White) were collected at baseline. A brief medical history was also collected at baseline. The latter measure was used to compile an index of chronic health conditions that documented whether participants had reported incidence of cardiovascular disease, pulmonary disease, functional impairment of the musculoskeletal system, hypertension, or diabetes. Affirmative responses were coded as a “1” and negative as a “0,” resulting in an aggregated chronic health conditions score from 0 to 5.
Physical activity participation.
Physical activity was assessed at baseline, 12, and 24 months by the Physical Activity Scale for the Elderly (PASE; Washburn, Smith, Jette, & Janney, 1993). The PASE is a well-validated, self-report measure developed for community-dwelling older adults (Martin et al., 1999). The PASE combines information from several domains including leisure, household, and occupational activity. The total PASE score was computed by multiplying the amount of time spent in each activity (hours/week) or participation (yes/no) in an activity by the empirically derived item weights and summing overall activities. This provides an overall activity count for participation in physical activity over the previous 7 days. Higher activity counts reflect greater physical activity participation.
Self-efficacy.
We used two measures of self-efficacy which were then used as indicators of a latent self-efficacy construct in our analyses. Higher scores on each measure reflect a stronger sense of efficacy for engaging in physical activity. The Self-Efficacy for Walking scale (McAuley, 1993) assessed expectations for successfully walking incremental bouts of 5–40 min at a moderately fast pace without stopping. The Lifestyle Self-Efficacy scale measured individuals’ confidence in their ability to accumulate 30 min of physical activity on 5 or more days of the week for incremental monthly periods. Items for each measure are scored on a 0–100 scale, summed, and divided by the total number of items to achieve an overall efficacy strength score ranging from 0 to 100. Both efficacy measures had excellent internal consistencies (αs ≥ .95).
Outcome expectations.
Three baseline measures of outcome expectations for exercise were assessed, and, in subsequent analyses, these were used as indicators of a latent outcome expectation variable. The first was the Outcome Expectations for Exercise scale (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000). This is a nine-item measure that was developed to assess the perceived consequences of physical activity participation in older adults. It has been reported to have acceptable psychometric properties. Sample items include “exercise makes me more alert mentally” and “exercise improves my endurance in performing my daily activities.” The second measure, developed by Conn (1997), also consisted of nine items, reflecting positive outcomes that would be expected to result from exercise participation. Sample items include “exercise helps me feel less tired” and “exercise is good for aches and pains.” The final measure was the exercise benefits subscale of the Osteoporosis Health Belief Scale (Kim, Horan, Gendler, & Patel, 1991), which comprises five items such as “exercising regularly reduces risks of broken bones.” All three measures instructed participants to indicate the degree to which they agreed with each statement using 5-point Likert scales, with items scored from 1 (strongly disagree) to 5 (strongly agree). Items for each measure were summed and divided by the total number of items, resulting in a possible range of 1–5 for the scale score. All outcome expectation measures had acceptable internal consistencies (αs ≥ .85).
Functional limitations.
We measured basic and advanced lower extremity function subscales of the abbreviated version (McAuley et al., 2005) of the Late-Life Function and Disability Instrument (LL-FDI; Haley et al., 2002; Jette et al., 2002). Each subscale comprises five items, reflecting the degree to which participants are limited in their performance of lower extremity activities. Sample items included “walking a mile taking rests as necessary” and “bending over from a standing position to pick up a piece of clothing from the floor.” The items are scored from 1 (cannot do) to 5 (no limitations), and items on each subscale are aggregated. In turn, the two lower extremity function scores were modeled as latent variables in our analyses. It is important to note that scores on each scale can range from 5 to 25 and that higher scores reflect fewer limitations in performing tasks.
Procedure
To be eligible for participation in this study, interested individuals had to meet the following criteria for inclusion: (a) female, (b) Black or White, (c) no previous history of a neurological disorder, (d) no physical disability that would preclude balance assessments, and (e) satisfactory cognitive status (McAuley et al., 2005). The Pfeiffer Mental Status Questionnaire (Pfeiffer, 1975) was used to assess cognitive status. Physical activity data (PASE) were collected at baseline, 12, and 24 months. Baseline demographics, general health information, physical activity, self-efficacy, and outcome expectations were collected by questionnaire upon entry into the study, following completion of the informed consent form. The LL-FDI data were collected via interview at baseline.
Data Analysis
Our analyses followed a series of stages. First, we conducted a latent growth curve (LGC) analysis to examine the trajectory and rate of change in physical activity across the three time points (i.e., baseline, 12, and 24 months). LGC analysis is a very useful approach to determine individual-level growth trajectories on measures of the same construct over time. Moreover, it can also be used to examine determinants or consequences of longitudinal growth trajectories at both the individual and the group level (Duncan, Duncan, Strycker, Li, & Alpert, 1999). The LGC analyses were conducted using AMOS (Version 6.0, Small Waters Corp., Chicago, IL, 2003) and Mplus (Version 3.0, Muthén & Muthén, 1998–2004) covariance modeling software and the full-information maximum likelihood estimator (FIML). FIML was used due to the presence of missing data and has been identified as an optimal method for the treatment of missing data (Enders & Bandalos, 2001).
The next set of analysis examined the fit of the proposed social cognitive model in accounting for the trajectory of change in physical activity across time. In this model, self-efficacy was hypothesized to have both a direct effect on the intercept and slope of change in physical activity and an indirect effect through outcome expectations and functional limitations. Finally, the previous model was once again estimated controlling for demographic factors (i.e., age, income, race, and education) and chronic health conditions also modeled as predictors of model constructs. In all analyses, initial status (i.e., the intercept) was statistically controlled when predicting change in physical activity (i.e., slope) based on a correlation between initial status and change factors as is standard in LGC modeling (Duncan et al., 1999).
Missing data.—
As mentioned previously, we had 231 and 217 participants at 12- and 24-month follow-up, respectively, resulting in 7.2% missing PASE data at 12 months and 13.3% missing PASE data at 24 months. There were no missing data at baseline for the social cognitive variables or the demographic and chronic health conditions data.
Evaluation of model fit.—
Several indices of model fit were used. The chi-square statistic assessed absolute fit of the model to the data (Jöreskog & Sörbom, 1996). Values for the root mean square error of approximation (RMSEA) of 0.06 or less are indicative of good model fit (Browne & Cudeck, 1993; Hu & Bentler, 1999). Finally, we calculated the comparative fit index (CFI; Bentler, 1990) for which a value of 0.95 or greater indicates a good model–data fit (Hu & Bentler).
Results
Descriptive statistics for all measures included in the data analysis are provided in Table 1. As can be seen, the sample had moderate to high levels of self-efficacy and positive outcome expectations, and participants were moderately high functioning. At baseline, 8.8% reported cardiovascular disease, 15.3% reported pulmonary disease, 44.2% reported functional impairments of the musculoskeletal system, 32.5% reported hypertension, and 12.4% reported diabetes (McAuley et al., 2005). Additionally, the sample was well educated, with 60% of the participants having an education beyond high school, and 35.7% of the sample had a mean household income of $40,000 or greater per year.
Table 1.
Descriptive Statistics for All Measures for the Overall Sample
| Variable and time point | M | SD |
| Physical activity at baseline | 156.44 | 70.89 |
| Physical activity at Month 12 | 137.59 | 64.78 |
| Physical activity at Month 24 | 128.84 | 60.12 |
| Variables measured at baseline only | ||
| Walking self-efficacy | 71.75 | 31.80 |
| Lifestyle self-efficacy | 90.91 | 13.20 |
| FDI: advanced lower extremity function | 17.90 | 4.85 |
| FDI: basic lower extremity function | 23.63 | 2.30 |
| Outcome expectations for exercise (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000) | 4.35 | 0.59 |
| Outcome expectations for exercise (Conn, 1997) | 4.63 | 0.44 |
| Outcome expectations (Kim, Horan, Gendler, & Patel, 1991) | 4.13 | 0.69 |
Note: FDI = Function and Disability Instrument.
Estimating Trajectories of Change in Physical Activity
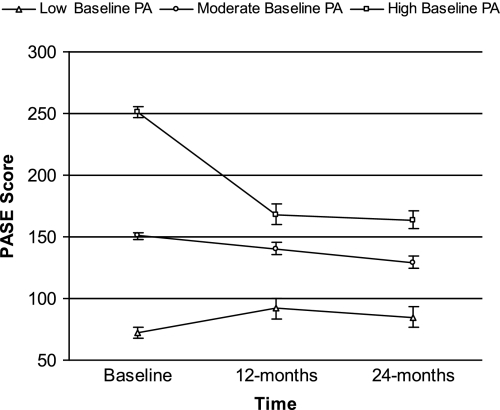
The overall fit of the LGC model describing a linear trajectory of change in physical activity was excellent (χ2 = 0.30, df = 1, p = .59, RMSEA [90% CI] = 0.00 [0.00–0.13], CFI = 1.0). Both the intercept (L = 156.4, p < .001) and the slope were significant (L = −21.27, p < .01), indicating a significant rate of decline in physical activity over the 2-year period. Additionally, the variances of the intercept and slope were significant (p < .05), as was the correlation between initial status and slope (r = −.62, p < .001). This suggests variation in the rate of change over time and that individuals with higher levels of baseline physical activity experience the greatest declines across time, respectively. This relationship is shown in Figure 1, where the trajectories of change are shown for those with high, medium, and low PASE scores at baseline based on tertile scores.
Figure 1.
Trajectories of change in physical activity for individuals with high, medium, and low activity scores at baseline.
Predicting Physical Activity Decline
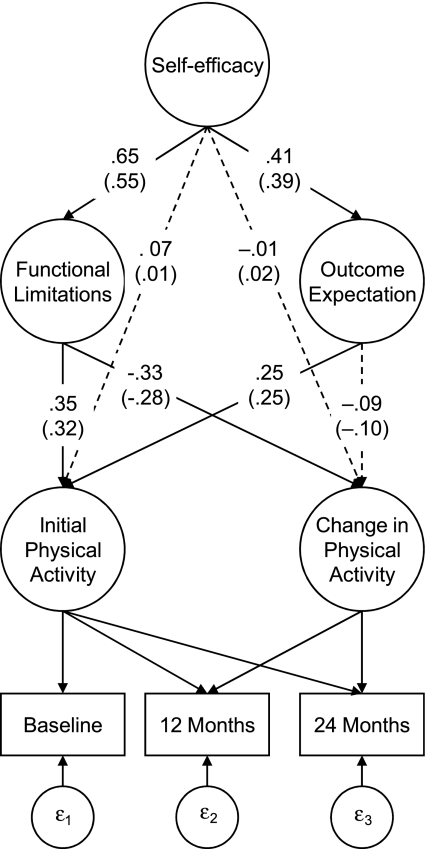
We next specified an LGC model that tested the direct effects of self-efficacy on physical activity decline and the indirect effects through outcome expectations and functional limitations as predictors of a linear decline in physical activity over time. This model provided an excellent fit to the data (χ2 = 33.75, df = 30, p = .31, RMSEA [90% CI] = 0.02 [0.00–0.05], CFI = 0.99). As predicted, self-efficacy was significantly (p < .05) associated with outcome expectations (β = .41) and functional limitations (β = .65), with more efficacious women having more positive outcome expectancies and reporting fewer limitations. Additionally, women with fewer limitations at baseline reported significantly greater activity at baseline (β = .35) and fewer declines in activity over time (β = −.33). More positive outcome expectations were associated with higher levels of activity at baseline (β = .25) but not across time. Self-efficacy was not significantly associated with either physical activity at baseline or declines across time when controlling for outcome expectations and functional limitations. We conducted an additional analysis examining the indirect effect of efficacy on physical activity by way of functional limitations and outcome expectations. The first analysis included self-efficacy, outcome expectations, and functional limitations. This analysis freely estimated the paths between self-efficacy and initial status and change in physical activity while fixing the paths between outcome expectations and functional limitations with initial status and change in physical activity to be zero. There were direct effects of self-efficacy on both initial status (.40) and change (−.26) in physical activity in this model, but the model fit (χ2 = 60.06, df = 34, p = .004, RMSEA [90% CI] = 0.06 [0.03–0.08], CFI = 0.97) was significantly worse than the previous model that did not fix the paths to be zero (χ2difference = 26.31, df = 4, p < .001). The next analysis tested the statistical significance of the indirect effect of self-efficacy on change in physical activity by way of outcome expectation and functional limitation. There was no longer a statistically significant direct effect of self-efficacy on change in physical activity (−.01), and the indirect effect of self-efficacy on change in physical activity was statistically significant via functional limitations (−.21) but not outcome expectations (−.04). This finding suggests that self-efficacy’s effect on the linear trajectory of physical activity decline in this sample is indirect rather than direct. All significant path coefficients are shown in Figure 2.
Figure 2.
Predicting declines in physical activity across 24 months using social cognitive variables. Note that values in parentheses are path coefficients adjusted for age, income, race, education, and number of reported chronic health conditions. All loadings are standardized, and significant paths are shown by solid lines. Nonsignificant paths are indicated by dashed lines.
Our final analysis estimated the previously tested model while saturating the hypothesized model for race, age, income, education, and chronic health conditions. Again, this model fit the data well (χ2 = 74.91, df = 57, p = .06, RMSEA [90% CI] = 0.04 [0.00–0.06], CFI = 0.98). As can be seen in Figure 2, the standardized path coefficients (in parentheses) for predicted relationships did not dramatically change. However, the covariates were associated with some of the model components. Specifically, White women had more positive outcome expectations (β = .16), and older women were less active (β = −.13) and had lower self-efficacy (β = −.17) at baseline. Additionally, women who reported more chronic health conditions were less efficacious (β = −.36) and less active (β = −.14) at baseline. Interestingly, declines in physical activity across time appear not to have been affected by demographic or health condition factors. Rather, their influence is indirect and operates through social cognitive factors in this sample.
Discussion
Studies examining social cognitive constructs as potential determinants of change in physical activity in older adults have been limited by a failure to test models that adequately reflect the breadth of social cognitive constructs. Additionally, Prohaska and colleagues (2006) have argued that there is a need to consider factors associated with the aging process, including disability and functional limitations, and to examine these processes in subgroups of aging adults. To this end, we included three key elements of social cognitive theory—self-efficacy, outcome expectations, and impediments to behavior (i.e., functional limitations)—in a model of physical activity change in older, community-dwelling women.
As expected, without specific intervention, participation in physical activity declined over the 2-year period, a finding that is consistent with previous reports (Keysor, 2003). Of particular interest was the relationship between initial status of physical activity and the linear trajectory of change across time, which suggested that the most active participants at baseline showed the largest declines across time. One explanation for this finding might be that given the poor physical activity rates of older adults, decline may be the most likely pattern to expect. However, such a pattern does have implication for program planners and the design of intervention strategies to change these patterns of behavior. For example, strategies for maintaining activity patterns in women who are already active are likely to be quite different from those in women who are low active or sedentary and who need to embark upon a physical activity regimen. Those women who are already active might be encouraged to broaden their activity repertoire, to continue to set goals for going beyond minimum public health guidelines, and to view themselves as good role models for their less active peers. For those individuals who are about to begin or are in the early stages of exercise regimens, strategies should focus on those elements over which the individual has control. These strategies might include choice of activities, setting of modest and achievable goals, doing activities that are enjoyable and fulfilling (e.g., playing with grandchildren), and keeping logs to determine progress and achievements. Whether the pattern of findings that we report herein can be replicated across and within activity categories will require large enough samples to make such comparisons, which are certainly warranted.
Our findings also revealed a social cognitive influence on physical activity patterns, but one that did not completely support our hypotheses. We had expected any change in physical activity to be influenced both directly and indirectly by self-efficacy. Such a position was based on social cognitive theory predictions (Bandura, 2004) and previous reports of the consistency of self-efficacy as a determinant of physical activity (King, Stokols, Talen, Brassington, & Killingsworth, 2002; McAuley & Blissmer, 2000). There was a partial support for the hypotheses, in that more efficacious women reported more positive outcome expectations and fewer functional limitations. However, self-efficacy’s association with declines in physical activity across the 2-year time period in this sample was indirect, operating through functional limitations. That is, more efficacious women reported fewer lower extremity limitations and, in turn, fewer declines in physical activity. We would argue that this is not an indictment of self-efficacy as a determinant of behavior but rather testimony to the importance of examining functional limitations as part of the aging process when predicting behavior change.
The hypothesized indirect effect of self-efficacy on physical-activity declines through outcome expectations was not supported. Indeed, the relationship between outcome expectations and physical activity is equivocal, with some studies showing strong support for the association and others demonstrating no relationship at all (for a review, see Williams et al., 2005). One possible reason for this equivocality concerns the measures typically used to assess outcome expectations. Although all three measures used in the present study have been validated in older populations and have suggested significant relationships between outcome expectations and physical activity, all these measures suffer from a fundamental limitation (Wójcicki, White, & McAuley, 2009), namely, the collapsing together of multiple categories of outcome expectations. Bandura (1997, 2004) has clearly stated the case for three related but conceptually distinct classes of outcome expectations: physical, social, and self-evaluative. Unfortunately, existing measures of outcome expectations for physical activity have tended to aggregate items representing different types of outcome expectations or rely solely on measures of physical outcome expectations. This precludes the opportunity to determine whether some outcome expectations may be more important than others in understanding behavior change. This is an important area of inquiry, as it is quite likely that older adults’ outcome expectations might be driven by personal and environmental factors. For example, for individuals who have lost a partner, the social benefits to be gained by group exercise participation may be particularly salient. Among participants with disease or disabling conditions, physical activity might be expected to improve functional performance (physical outcome expectations), making independent living easier. The development of new outcome expectations measures (Wójcicki et al., 2009) will allow such comparisons to be made.
Outcome expectations were not significantly associated with changes in physical activity behavior, although Bandura (1997) has noted that outcomes expected from the performance of behavior often make little contribution to the prediction of this behavior when performance is synonymous with the outcome (i.e., physical activity). However, this is not to suggest that outcome expectations are unimportant relative to physical activity behavior. Indeed, formulating realistic outcome expectations at the onset of an activity program may be an important consideration for motivating behavior change, especially in older adults. It must also be noted that scores on the outcome measures used in the present study were very high, suggesting a possible ceiling effect and a limitation in interpreting the findings.
The indirect effect of self-efficacy on physical activity through functional limitations is particularly interesting from at least two perspectives. First, it offers support for the proposed social cognitive pathway suggested by Bandura (1997, 2004), from self-efficacy to behavior through potential impediments or facilitators. Second, it clearly speaks to the importance of expanding existing theoretical models to include factors that are associated with the aging process and that have implications for the maintenance of a healthy lifestyle. Given the changing demographic landscape (U.S. Census Bureau, 2008) and the increasingly large numbers of adults with functional limitations and disabilities, such factors must be considered as important mediators or moderators of traditional correlates of physical activity behavior change. Consequently, including assessments of perceived limitations along with measures of functional performance in behavior interventions appears warranted.
Clearly, demographic factors and the accumulation of chronic health conditions with age should be factors considered in the application of any theoretical model to understanding behavior. In the present study, we studied a subgroup of older adults, women, who are typically less active than men. Additionally, more than half of all women aged 65 years and older suffer from at least one disability, typically brought about by chronic conditions associated with aging (CDC, 2006). Our analyses, in which we examined the relative influence of demographic (i.e., age, race, education, and income) and chronic health conditions, did not serve to change the relationships among self-efficacy, functional limitations, outcome expectations, and physical activity.
However, it is important to recognize that factors such as age, education, and health status may well act as important sources of information for shaping social cognitive constructs. For example, in the present study, being older and suffering from more chronic health conditions was significantly associated with reporting lower levels of self-efficacy and physical activities. One possible explanation for this is that perceptions of community and environmental impediments negatively influence efficacy beliefs. Alternatively, older adults with chronic health conditions may be counseled to “take it easy” instead of taking an active role in their recovery or prevention of further decline. Efficacy beliefs are informed by a number of important sources, including performance or mastery accomplishments, social persuasion, social modeling, and the interpretation of physical and affective stimuli. Behavioral interventions such as community activity programs should target such sources of information to stimulate initiation of physical activity, as well as encourage adherence, and maintenance of this important health behavior.
Although a relatively comprehensive social cognitive model of physical activity behavior was tested, future approaches should also consider the inclusion of goal constructs that may further mediate effects of self-efficacy. Whereas past performance accomplishments represent a potent source of efficacy expectations, such expectations are implicated in the types of goals one sets for oneself relative to future behaviors (Bandura, 2004). Subsequent applications of social cognitive models should consider the inclusion of goal structures and, as argued earlier, determine whether social, physical, and self-evaluative outcome expectations differentially influence physical activity behavior. Furthermore, an important contribution to understanding the process of physical activity behavior change will necessitate multiple assessments of multiple social cognitive constructs across time. Such an approach would allow for the examination of how certain social cognitive factors and behavioral outcomes might be reciprocally determined. An additional limitation of this study is the reliance on self-report measures of physical activity. Corroborating the reported declines in physical activity with objective measures such as accelerometers is recommended, although not always feasible in larger samples.
In conclusion, we believe that this study addresses some of the issues recently raised by Prohaska and colleagues (2006). We used a theoretical model of understanding changes in physical activity that incorporated factors relevant to the aging process, including functional limitations and chronic health conditions in older women, a third of whom were African American. The use of LGC modeling is an additional strength of the study as we were able to examine how a baseline social cognitive model predicted change (declines) in physical activity across a 2-year period while controlling for baseline physical activity. That modifiable constructs, such as self-efficacy, play an important role in perceived functional limitations has implications for effectively structuring physical activity programs that may serve to attenuate the frequently reported declines in activity with aging.
Funding
This material is based upon work supported by the National Institute on Aging under award no. R01-AG20118. E.M. is also supported by a Shahid and Ann Carlson Khan Professorship in Applied Health Sciences and grant no. R37AG025667.
References
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Centers for Disease Control and Prevention. Difficulty performing activities of daily living, by age, residence, sex, race and ethnicity: Medicare beneficiaries from the Medicare Current Beneficiary Survey, 1992–2004. (MAADL04) 1992–2004. Retrieved November 5, 2007, from http://209.217.72.34/aging/TableViewer/tableView.aspx?ReportId=362. [Google Scholar]
- Centers for Disease Control and Prevention. U.S. physical activity statistics: State comparison by demographics. 2005. Retrieved October 25, 2007, from http://apps.nccd.cdc.gov/PASurveillance/DemoCompareResultV.asp?State=0&Cat=4&Year=2005&Go=GO#result. [Google Scholar]
- Centers for Disease Control and Prevention. Women and disabilities. 2006. Retrieved October 1, 2007, from http://www.cdc.gov/ncbddd/women/default.htm. [Google Scholar]
- Conn VS. Older women: Social cognitive theory correlates of health behavior. Women & Health. 1997;26(3):71–84. doi: 10.1300/j013v26n03_05. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA, Li F, Alpert A. An introduction to latent variable growth curve modeling. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [PubMed] [Google Scholar]
- Estabrooks PA, Lee RE, Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine. 2003;25:100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. Journal of the American Geriatrics Society. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Haley SM, Jette AM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, Ashba J. Late life function and disability instrument: II. Development and evaluation of the function component. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2002;57:M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jette AM, Haley SM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, Ashba J. Late life function and disability instrument: I. Development and evaluation of the disability component. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2002;57:M209–M216. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User’s reference guide. Chicago: Scientific Software International; 1996. [Google Scholar]
- Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of scientific evidence. American Journal of Preventive Medicine. 2003;25(Suppl. 2):129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the osteoporosis health belief scale. Research in Nursing & Health. 1991;14:155–163. doi: 10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001;56(Spec No 2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- King AC, Stokols D, Talen E, Brassington GS, Killingsworth R. Theoretical approaches to the promotion of physical activity: Forging a transdisciplinary paradigm. American Journal of Preventive Medicine. 2002;23(Suppl. 1):15–25. doi: 10.1016/s0749-3797(02)00470-1. [DOI] [PubMed] [Google Scholar]
- Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH, Messier SP. Validation of the PASE in older adults with knee pain and physical disability. Medicine and Science in Sports and Exercise. 1999;31:627–633. doi: 10.1097/00005768-199905000-00001. [DOI] [PubMed] [Google Scholar]
- McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. Journal of Behavioral Medicine. 1993;16:103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exercise and Sport Sciences Reviews. 2000;28:85–88. [PubMed] [Google Scholar]
- McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: Psychometric properties of the late life function and disability instrument. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005;60:901–909. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- McAuley E, Morris KS, Motl RW, Hu L, Konopack JF, Elavsky S. Long-term follow-up of physical activity behavior in older adults. Health Psychology. 2007;26:375–380. doi: 10.1037/0278-6133.26.3.375. [DOI] [PubMed] [Google Scholar]
- Morris KS, McAuley E, Motl RW. Self-efficacy and environmental correlates of physical activity among older women and women with multiple sclerosis. Health Education Research. 2008;23(4):744–752. doi: 10.1093/her/cym067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 3rd ed. Los Angeles: Author; 1998–2004. [Google Scholar]
- Pfeiffer E. A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Prohaska T, Belansky E, Belza B, Buchner D, Marshall V, McTigue K, Santariano W, Wilcox S. Physical activity, public health, and aging: Critical issues and research priorities. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61:S267–S273. doi: 10.1093/geronb/61.5.s267. [DOI] [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for Exercise Scale: Utility and psychometrics. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;6:S352–S356. doi: 10.1093/geronb/55.6.s352. [DOI] [PubMed] [Google Scholar]
- Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Preventive Medicine. 2004;39:1056–1061. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Seeman T, Chen XG. Risk and protective factors for physical functioning in older adults with and without chronic conditions: MacArthur studies of successful aging. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57:S135–S144. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- Sproston K, Primatesta P, editors. Health survey for England volume 2: Risk factors for cardiovascular disease. London: The Stationery Office; 2004. [Google Scholar]
- U.S. Census Bureau. U.S. population projections. 2008. Retrieved October 1, 2008, from http://www.census.gov/population/www/projections/projectionsagesex.html. [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Annals of Behavioral Medicine. 2005;29:70–79. doi: 10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]
- Wojcicki T, White SM, McAuley E. Assessing outcome expectations in older adults: The Multidimensional Outcome Expectations for Exercise Scale (MOEES) Journal of Gerontology: Psychological Sciences. 2009;64:33–40. doi: 10.1093/geronb/gbn032. [DOI] [PMC free article] [PubMed] [Google Scholar]