Abstract
Objective
This study was designed to evaluate the difference in the degree of patient pain for an ultrasound-guided fine-needle aspiration biopsy (USFNAB) of a thyroid nodule with one needle puncture with and without local anesthesia.
Materials and Methods
A total of 50 patients participated in the study. We examined prospective patients who would undergo US-FNABs of two thyroid nodules (larger than 10 mm maximum diameter), which were located in separate thyroid lobes. For one of these thyroid nodules, US-FNAB was performed following the administration of local anesthesia; for the other nodule, no anesthesia was administered. The application of anesthesia was alternatively administered between patients (either prior to the first US-FNAB procedure or prior to the second procedure). For all patients, the degree of pain during and after each US-guided FNAB was evaluated according to a 4-category verbal rating scale (VRS), an 11-point numeric rating scale (NRS) and a 100-mm visual analogue scale (VAS).
Results
The mean maximum diameters of thyroid nodules examined by US-FNAB with the use of local anesthesia and with no local anesthesia were 13.6 mm and 13.0 mm, respectively. There was no significant difference in nodule size (p > 0.05) between two groups. For the VRS, there were 27 patients with a higher pain score when local anesthesia was used and four patients with a higher pain score when no local anesthesia was administered. Nineteen patients had equivalent pain score for both treatments. This finding was statistically significant (p < 0.001). For the NRS, there were 33 patients with a higher pain score when local anesthesia was used and 10 patients with a higher pain score when no local anesthesia was administered. Seven patients had an equivalent pain score for each treatment. This finding was statistically significant (p < 0.001). For the VAS, there were 35 patients with a higher pain score when local anesthesia was used and 11 patients with a higher pain score where no local anesthesia was administered. Four patients had an equivalent pain score for both treatments. This finding was also statistically significant (p = 0.001).
Conclusion
In our study, patient pain scales were significantly lower when no local anesthesia was used prior to US-FNABs of thyroid nodules as compared to when local anesthesia was administered. Therefore, we believe that when one needle puncture is used, US-FNAB should be performed without administering local anesthesia.
Keywords: Thyroid nodule, Fine-needle biopsy, Pain, Local anesthesia, Ultrasound (US)
An ultrasound-guided fine-needle aspiration biopsy (US-FNAB) is widely used for the evaluation of thyroid and other neck masses because it is a simple, safe, accurate and minimally invasive procedure (1-5). At the Busan Paik Hospital, US-FNABs of thyroid nodules are commonly performed if a non-palpable thyroid nodule shows a likelihood for malignancy on ultrasonography (US), or if the cytology result of a conventional fine-needle aspiration biopsy (FNAB) obtained without imaging guidance is unsatisfactory. However, various US-FNAB techniques have been used depending on the medical institution or physician. It remains unclear if the administration of local anesthesia is required and/or appropriate. Although there have been many reports regarding US-FNABs of thyroid nodules, no study has suggested the appropriate criteria for determining if local anesthesia is required. Yokozawa et al. (1) and Danese et al. (2), for example, have performed US-FNABs of thyroid nodules without local anesthesia; however, Rausch et al. (3) and O'Malley et al. (4) have performed the same procedure with local anesthesia.
Based on our own experience performing US-FNABs of thyroid nodules, we hypothesized that, when only one needle puncture is used, the degree of patient pain caused by the administration of local anesthesia during US-FNAB is no less than the degree of patient pain experienced during US-FNAB performed without local anesthesia. The purpose of this study was to compare the pain scales for patients undergoing US-FNABs of thyroid nodules with or without the use of local anesthesia.
MATERIALS AND METHODS
A total of 50 patients participated in this study between March 2008 and May 2008. The Inje University Busan Paik Hospital Institutional Review Board approved this study and all participants provided informed written consent. This study was a single blind, controlled clinical trial and was designed for consecutive patients who met the inclusion criteria at a thyroid outpatient clinic. The inclusion criteria for study participants were as follows. First, each participant had two thyroid nodules that required an US-FNAB and which were located in two separate lobes. Second, the thyroid nodules that required an US-FNAB were 10 mm or larger in the maximum diameter. Third, the locations of the thyroid nodules were intraglandular and were relatively central in both lobes. Participants who agreed to participate in the study protocol were included. The exclusion criteria for study participants were as follows: i) patient refusal (a major reason for exclusion), ii) individuals who previously underwent US-FNAB of a thyroid nodule (excluded to rule out a possible bias related to pain or another recalled event that occurred during the previous biopsy), iii) participants who had a history of bleeding tendency and who had been taking aspirin or warfarin (coumadin), iv) patients with a purely cystic thyroid nodule or a calcified thyroid nodule.
All study patients underwent a diagnostic thyroid US examination using a high-resolution ultrasound unit (HDI 5000 or IU 22: Phillips Medical Systems, Bothell, WA) with a 12-15-MHz linear probe within a few weeks before, or just prior to, the US-FNAB. A high-resolution US unit (HDI 5000 or IU 22), with a 12-15-MHz linear probe was used for guidance during the entire US-FNAB procedure.
The order of local anesthesia administration was alternated in consecutive patients. The sequence was as follows. The first patient underwent an US-FNAB of a thyroid nodule with local anesthesia and then an US-FNAB of a thyroid nodule in the opposite lobe with no local anesthesia. The second patient then underwent an US-FNAB of a thyroid nodule with no local anesthesia and then an US-FNAB of a thyroid nodule in the opposite lobe with local anesthesia. This strategy was continued throughout the study. Therefore, half of all study patients underwent an US-FNAB of a thyroid nodule with the use of local anesthesia for the first nodule and half of all study patients underwent an US-FNAB of a thyroid nodule with the use of local anesthesia for the second nodule.
An experienced radiologist performed all US-FNAB procedures using a 10-ml plastic syringe attached to a conventional 23-gauge needle (called a 'syringe-needle unit'), under US guidance. Patients were placed in the supine position with their neck slightly extended and their hands comfortably crossed on their breasts or chest for privacy. The operator did not notify the patients of local anesthesia use during the procedures.
In cases where no local anesthesia was administered, the target nodule was placed in the center of the image by adjusting the US probe after skin sterilization. The tissue motion could then be clearly identified on the US monitor when the needle was gently oscillated back and forth on the skin surface. After appropriate aiming, the needle was vertically inserted into the target nodule in the center of the transverse US image, and the angle of the needle puncture was on a nearly coaxial plane to the axis of the transverse US image. After completion of the needle puncture of the target nodule under US guidance, sampling began using the 'mixed sampling technique.' This technique was performed as follows. After the accurate puncture of the target, the needle was moved up and down for a few seconds only by movement of the operator's wrist and without initial aspiration. When a small amount of material filled the well or hub of the needle, the syringe-needle unit could be rapidly withdrawn and the puncture site on the skin was compressed for several minutes. However, if no aspirates were obtained after a few seconds of capillary sampling, negative pressure was gradually applied using the first finger of the operator's right hand while observing the monitor and the well or hub of the needle in turn.
In cases where local anesthesia was applied, local anesthetic (2% lidocaine; Jeil, Daegu, Korea), stored at room temperature (20℃), was administered using a conventional 23-gauge needle as follows. After skin sterilization, the appropriate skin site for infiltration of local anesthesia over the target nodule was verified by gentle oscillation of the syringe-needle unit on the overlying skin and by observing the motion of the subcutaneous tissue on real time US. First, a small amount of lidocaine was instilled into the first puncture site that was mainly a subcutaneous fatty layer or dermis (after confirmation of non-intravascular puncture), and was then progressively instilled into a deeper layer of the anterior neck and around the thyroid capsule. Finally, an appropriate amount of lidocaine was instilled into the superficial subcutaneous layer or dermis that was unanesthetized while the operator retracted the syringe-needle unit. In all cases, local anesthesia was completed within one minute, and the total amount of infused lidocaine did not exceed 2 mL. US-FNAB of a thyroid nodule was performed as described above.
After completion of the US-FNAB, each patient was transferred to another room. A radiology nurse instructed the patient how to complete a pain survey form where the patient was asked to check his/her pain during the first and second US-FNABs, respectively. In this study, three pain scales were evaluated a four-category verbal rating scale (VRS), a horizontally depicted 11-point numeric rating scale (NRS) and a horizontal 100-mm visual analogue scale (VAS). For the VRS, a score of 0 represented 'no pain,' a score of 1 represented 'mild pain,' a score of 2 represented 'moderate pain' and a score of 3 represented 'severe pain.' Patients were asked to mark the items that applied. For the NRS, there was a range from 0 to 10, with a score of 0 representing 'no pain' and a score of 10 representing 'the worst pain.' Patients were asked to mark the number according to the pain degree that they felt during the US-FNAB. The VAS included a diagram that showed 'no pain' on the left side to 'the worst pain imaginable' on the right side. Patients were asked to place a mark along a 100-mm-long line in order to indicate the pain degree that they felt during the procedure. The VAS was then scored by measuring the distance from the left border.
Data were analyzed using SPSS software (SPSS, Version 14.0; SSPS, Chicago, IL). Differences in baseline characteristics between the use of local anesthesia and no local anesthesia were assessed by means of the Student's t-test for continuous variables. The Wilcoxon sign rank test was performed to determine whether there was a significant difference in pain scores with or without the use of local anesthesia. P-values less than 0.05 were considered as statistically significant.
RESULTS
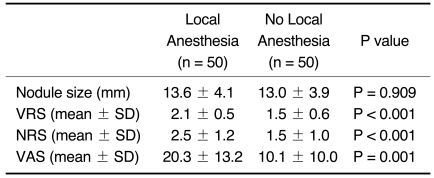
All patients (mean age, 49.3 ± 9.8 years; age range, 21-67 years) meeting the study criteria described in the materials and methods section had two thyroid nodules. These nodules were randomly assigned to undergo US-FNABs with or without local anesthesia and were comparable with respect to size and pain scores (Table 1). For each US-FNAB of a thyroid nodule, only one sampling through one puncture was performed. The mean maximum diameter of thyroid nodules assessed on US-FNABs with and without local anesthesia was 13.6 mm and 13.0 mm, respectively. There was no statistical difference for nodule size (Student's t test, p > 0.05).
Table 1.
Mean Nodule Size and Pain Scores of US-FNABs for Thyroid Nodules with and without Local Anesthesia
Note.-US-FNAB = ultrasound-guided fine-needle aspiration biopsy, VRS = verbal rating scale, NRS = numeric rating scale, VAS = visual analogue scale
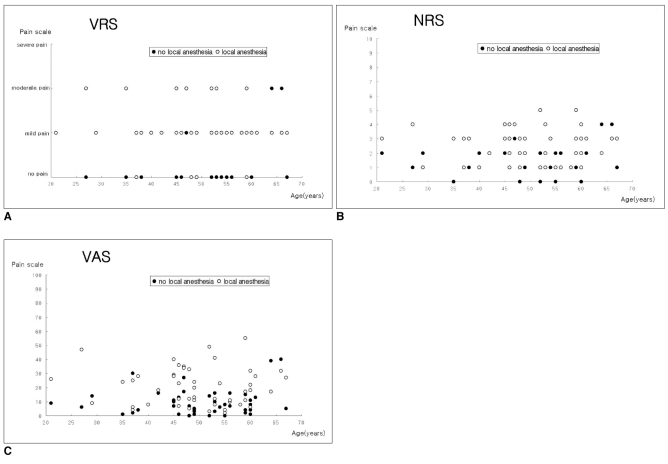
For the VRS, there were 27 patients with a higher pain score when local anesthesia was used, four patients with a higher pain score when no local anesthesia was administered and 19 patients with an equivalent pain score. The incidence of 'no pain,' 'mild pain,' 'moderate pain' and 'severe pain' was 5, 37, 8 and 0 when local anesthesia was used, and 26, 21, 3 and 0 when no local anesthesia was administered, respectively. These differences were statistically significant (Wilcoxon sign rank test, p < 0.001) (Fig. 1A). For NRS, there were 33 patients with a higher pain score when local anesthesia was used, 10 patients with a higher pain score where no local anesthesia was administered and seven patients with an equivalent pain score. The mean value of the pain scores was 2.5 with the use of local anesthesia and 1.5 when no local anesthesia was used. This difference was statistically significant (Wilcoxon sign rank test, p < 0.001) (Fig. 1B). For VAS, 35 patients indicated a higher pain score when local anesthesia was used, 11 patients had a higher pain score where no local anesthesia was administered and four patients had an equivalent pain score. The mean value of the pain score was 20.3 and 10.1 with and without the use of local anesthesia, respectively. This difference was also statistically significant (Wilcoxon sign rank test, p = 0.001) (Fig. 1C). There was no statistical difference in the three pain scales between females and males (Mann-Whitney test, p < 0.001), even though there were only a small number of study participants. In addition, many of the participants could not discriminate between a procedure that used local anesthesia and a procedure where no local anesthesia was administered following completion of the US-FNAB.
Fig. 1.
Patient pain scores for three pain scales (A. VRS, B. NRS, C. VAS). VRS = verbal rating scale, NRS = 11 point numeric rating scale, VAS = 100 mm visual analogue scale.
The rate of sampling adequacy on US-FNABs of thyroid nodules was 94% (47 of 50) with the use of local anesthesia and 96% (48 of 50) where no local anesthesia was administered. Based on the cytology, nodules collected following local anesthesia were identified as 'benign' (n = 40, 80%), 'suspicious for papillary thyroid carcinoma (PTC)' (n = 1, 2%), 'suggestive of PTC' (n = 3, 6%), 'indeterminate for malignancy' (n = 1, 2%) and 'inadequate' (n = 5, 10%). Those nodules collected without local anesthesia were identified as 'benign' (n = 38, 76%), 'suspicious for PTC' (n = 0, 0%), 'suggestive of PTC' (n = 5, 10%), 'indeterminate for malignancy' (n = 3, 6%) and 'inadequate' (n = 4, 8%). There were no significant patient complications.
DISCUSSION
Local anesthesia has been commonly used to control patient pain during US-FNABs of thyroid nodules (3, 4). The advantages of using local anesthesia include the ability to obtain multiple aspirates without patient discomfort and that patient fear of procedures using needles can be controlled. Some operators, however, prefer to use no local anesthesia when only one needle puncture is needed for an US-FNAB of a thyroid nodule (1, 2).
Lidocaine is a widely used local anesthetic agent in the form of a topical compound or infiltrate. The anesthetic mechanism of lidocaine is as follows. The agent alters depolarization in neurons by blocking the fast voltage-gated sodium channels in the cell membrane, and with sufficient blockage, the membrane of the presynaptic neuron will not depolarize and thus fail to transmit an action potential, thus leading to anesthetic effects (5). Local injection of lidocaine solution, however, is a possible cause of drug toxicity; in particular, when lidocaine solution is inappropriately injected into a vessel or is infused in an over-estimated dose in an infant or child, significant systemic toxicity can occur, although the possibility is very low (6).
Although we used unbuffered lidocaine in the present study, the local injection of unbuffered lidocaine can induce various degrees of the pain or discomfort in the injection site (7-11). The pH of an anesthetic solution is known to be the main factor determining the amount of patient pain experienced during injection, and buffer solutions used to create near physiological pH have been demonstrated to reduce pain (7-9). Interestingly, Porter and Frizelle (11) have insisted that the main factor related to patient pain during local anesthesia is not the pH but the actual local anesthetic agent, local injection technique or the patient. A reduction in pain experienced following injection is reported when the local anesthetic is warmed (12-14), but Allen et al. (15) have insisted that the practice of warming a local anesthetic prior to performing a sub-Tenon's block did not significantly reduce the amount of pain experienced by patients.
Pain is a subjective sensation, and is therefore difficult to measure. Pain assessment scales are useful to elicit responses from patients regarding pain or discomfort. The relative merits of the three pain scales, the VAS, NRS and VRS, all of which are often used to assess pain, have been studied extensively and several investigators have validated the usefulness of the scales (5, 16). The present study showed that the same patients felt greater pain during an US-FNAB when local anesthesia was used as compared to a procedure where no local anesthesia was administered. Based on our experience performing US-FNABs of thyroid nodules using no local anesthesia, many patients seem to easily tolerate the pain or discomfort related to the procedure. At the Busan Paik Hospital, US-FNABs of thyroid or neck masses have been routinely performed for approximately the past five years using one needle puncture, one sampling and no local anesthesia. However, we prefer administering local anesthesia for an US-FNAB of thyroid or neck masses if cellulitis is combined around the target, if multiple sampling is required or if a patient prefers the use of local anesthesia.
Our biopsy technique for performing an US-FNAB has two important parts: 'mixed sampling technique' and only one sampling with one needle puncture, and we think it is simple and effective. Recently, we have reported a high rate of diagnostic efficacy and no significant complications for US-FNABs of thyroid nodules when using this biopsy technique (17).
The present study has several limitations. First, the study included a relatively small number of participants and there were far fewer male participants than females. Second, the US-FNAB technique included one sampling and one puncture. Accordingly, this study result should be applied for an US-FNAB where only one sample is obtained. We recommend the use of local anesthesia when two or more samples on an US-FNAB for a thyroid nodule are obtained. Third, we used a 23G needle attached to a 10-mL syringe for lidocaine infusion. Use of a smaller caliber needle, such as a 25G or 26G needle, may potentially reduce the pain scale for a patient as compared to the use of a 23G needle. Fourth, we used 2% lidocaine for local anesthesia although 1% lidocaine or a buffered lidocaine with bicarbonate may cause less discomfort than 2% lidocaine. Finally, delayed patient pain was not assessed; however, no participants complained of newly developed pain or aggravated pain after an US-FNAB while they waited for compression of puncture sites and while completing the pain scale forms.
In conclusion, we found that there was significantly less pain in patients undergoing US-FNAB of thyroid nodules when no local anesthesia was administered compared to when local anesthesia was used. Therefore, we believe that US-FNAB with no local anesthesia seems to be preferable to perform for one needle puncture and one sampling.
Acknowledgements
This work was supported by the Busan Paik Hospital Imaging Research Institute.
References
- 1.Yokozawa T, Miyauchi A, Kuma K, Sugawara M. Accurate and simple method of diagnosing thyroid nodules the modified technique of ultrasound-guided fine needle aspiration biopsy. Thyroid. 1995;5:141–145. doi: 10.1089/thy.1995.5.141. [DOI] [PubMed] [Google Scholar]
- 2.Danese D, Sciacchitano S, Farsetti A, Andreoli M, Pontecorvi A. Diagnostic accuracy of conventional versus sonography-guided fine-needle aspiration biopsy of thyroid nodules. Thyroid. 1998;8:15–21. doi: 10.1089/thy.1998.8.15. [DOI] [PubMed] [Google Scholar]
- 3.Rausch P, Nowels K, Jeffrey RB., Jr Ultrasonographically guided thyroid biopsy: a review with emphasis on technique. J Ultrasound Med. 2001;20:79–85. doi: 10.7863/jum.2001.20.1.79. [DOI] [PubMed] [Google Scholar]
- 4.O'Malley ME, Weir MM, Hahn PF, Misdraji J, Wood BJ, Mueller PR. US-guided fine-needle aspiration biopsy of thyroid nodules: adequacy of cytologic material and procedure time with and without immediate cytologic analysis. Radiology. 2002;222:383–387. doi: 10.1148/radiol.2222010201. [DOI] [PubMed] [Google Scholar]
- 5.Brau ME, Nau C, Hempelmann G, Vogel W. Local anesthetics potently block a potential insensitive potassium channel in myelinated nerve. J Gen Physiol. 1995;105:485–505. doi: 10.1085/jgp.105.4.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donald MJ, Derbyshire S. Lignocaine toxicity; a complication of local anaesthesia administered in the community. Emerg Med J. 2004;21:249–250. doi: 10.1136/emj.2003.008730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesth Analg. 1987;66:572–574. [PubMed] [Google Scholar]
- 8.Christoph RA, Buchanan L, Begalla K, Schwartz S. Pain reduction in local anaesthetic administration through pH buffering. Ann Emerg Med. 1988;17:117–120. doi: 10.1016/s0196-0644(88)80293-2. [DOI] [PubMed] [Google Scholar]
- 9.Dire DJ, Hogan DE. Double-blinded comparison of diphenhydramine versus lidocaine as a local anesthetic. Ann Emerg Med. 1993;22:1419–1422. doi: 10.1016/s0196-0644(05)81989-4. [DOI] [PubMed] [Google Scholar]
- 10.Xia Y, Chen E, Tibbits DL, Reilley TE, McSweeney TD. Comparison of effects of lidocaine hydrochloride, buffered lidocaine, diphenhydramine, and normal saline after intradermal injection. J Clin Anesth. 2002;14:339–343. doi: 10.1016/s0952-8180(02)00369-0. [DOI] [PubMed] [Google Scholar]
- 11.Porter JC, Frizelle FA. Use of local anesthetic agents among New Zealand plastic surgeons - their practices and philosophies. Med Sci Monit. 2000;6:194–197. [PubMed] [Google Scholar]
- 12.Bainbridge LC. Comparison of room temperature and body temperature local anaesthetic solutions. Br J Plast Surg. 1991;44:147–148. doi: 10.1016/0007-1226(91)90050-t. [DOI] [PubMed] [Google Scholar]
- 13.Davidson JA, Boom SJ. Warming lignocaine to reduce pain associated with injection. BMJ. 1992;305:617–618. doi: 10.1136/bmj.305.6854.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bell RW, Butt ZA. Warming lignocaine reduces the pain of injection during peribulbar local anaesthesis for cataract surgery. Br J Ophthalmol. 1995;79:1015–1017. doi: 10.1136/bjo.79.11.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allen MJ, Bunce C, Presland AH. The effect of warming local anaesthetic on the pain of injection during sub-Tenon's anaesthesia for cataract surgery. Anaesthesia. 2008;63:276–278. doi: 10.1111/j.1365-2044.2007.05351.x. [DOI] [PubMed] [Google Scholar]
- 16.Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4:407–414. doi: 10.1016/s1526-5900(03)00716-8. [DOI] [PubMed] [Google Scholar]
- 17.Kim DW, Lee EJ, Kim SH, Kim TH, Lee SH, Kim DH, et al. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules: comparison in efficacy according to nodule size. Thyroid. 2009;19:27–31. doi: 10.1089/thy.2008.0106. [DOI] [PubMed] [Google Scholar]