Abstract
In this study, we compare self-perceived unmet need across Canadian provinces and assess how the reasons for unmet need – problems with availability, accessibility and acceptability – vary. This cross-sectional study uses data from the Canadian Community Health Survey (2.1) conducted in 2003. Overall, 11.7% perceived having had unmet healthcare needs in the previous 12 months. The adjusted provincial rates varied from 13.3% in Manitoba to 7.8% in Prince Edward Island. Among those reporting unmet health service needs, the leading reason was problems of availability of services (54.9%), followed by acceptability (42.8%) and accessibility related to cost or transportation (12.7%). Unmet need due to problems of availability was most likely in Quebec, Newfoundland and Manitoba, while Alberta and British Columbia had the highest likelihood of unmet need due to accessibility problems. Those in British Columbia, Saskatchewan and Manitoba were more likely to report problems of acceptability. The reasons for unmet need vary across provinces, with each reason having different policy implications.
Abstract
Cette étude compare la perception de la population face aux besoins non comblés et évalue la variation des raisons qui mènent à cette perception (raisons liées à des problèmes de disponibilité, d'accessibilité et d'acceptabilité), entre les provinces canadiennes. Cette étude transversale s'appuie sur les données de l'Enquête sur la santé dans les collectivités canadiennes (2.1) effectuée en 2003. En général, 11,7 pour cent des répondants perçoivent avoir eu des besoins non comblés au cours des 12 mois précédents l'enquête. Les taux provinciaux ajustés varient entre 13,3 pour cent au Manitoba et 7,8 pour cent à l'Île-du-Prince-Édouard. Parmi les besoins non comblés déclarés, les raisons principalement invoquées sont liées aux problèmes de disponibilité des services (54,9 pour cent), suivi de l'acceptabilité (42,8 pour cent) et de l'accessibilité en raison des coûts de transport (12,7 pour cent). Les besoins non comblés attribués à la disponibilité sont plus susceptibles d'avoir lieu au Québec, à Terre-Neuve et au Manitoba tandis que pour l'Alberta et la Colombie-Britannique, ce sont les besoins non comblés attribués à l'accessibilité qui sont le plus invoqués. Les résidents de la Colombie-Britannique, de la Saskatchewan et du Manitoba sont plus susceptibles d'invoquer des problèmes liés à l'acceptabilité. Les raisons invoquées pour signaler des besoins non comblés varient entre les provinces, et chacune d'entre elles a ses propres répercussions sur les politiques.
Canadian policy makers have long struggled with how best to provide access to high-quality healthcare to all Canadians. Access to care is of great concern to the general public, who expect equitable distribution of access across the population, regardless of socio-demographic factors and region or province of residence (Hutchison 2007). Often, access to healthcare services is evaluated based on measures of utilization. These measures do not provide information about those who do not use healthcare services, or the adequacy of access of those who do. Self-perceived unmet healthcare need is a commonly used indicator of access to care. This measure is derived from surveys and does not rely on respondents' use of healthcare services, as is the case with utilization-based access measures.
Research using data from the Canadian Community Health Survey (CCHS 1.1) and the National Population Health Survey (NPHS) has shown that the proportion of people reporting unmet healthcare needs rose from 4.2% in 1994/95 to three times that in 2000/01 (12.5%) (Sanmartin et al. 2002). In order to address this potential worsening in access to care, greater understanding is needed about the reasons healthcare needs are not being met and how these reasons vary by region and segment of the population.
Reasons for unmet need can be classified into three categories: availability of services, accessibility and acceptability of available services (Table 1) (Chen and Hou 2002). Unmet need due to problems of availability includes too-lengthy wait times, services not available when required and services not available in area. This category of reasons has the strongest policy implications because these factors could potentially be altered by governments and health authorities/regions. Unmet need due to problems of accessibility includes reasons related to cost and transportation – both of which also have policy implications. The final category, acceptability of available services, is related to personal preferences or circumstances of individuals. Because these reasons are not related to characteristics of healthcare services (with the possible exception of language), their implication for healthcare planning is unclear.
TABLE 1.
Reasons for self-perceived unmet need
| % | Availability | % | Acceptability | % | Accessibility |
|---|---|---|---|---|---|
| 35.6 | Waiting time too long | 9.9 | Felt it would be inadequate | 11.5 | Cost |
| 16.5 | Not available when required | 8.5 | Other | 1.6 | Transportation |
| 11.0 | Not available in area | 8.4 | Didn't get around to it | ||
| 7.9 | Decided not to seek care | ||||
| 7.1 | Too busy | ||||
| 3.7 | Didn't know where to go | ||||
| 1.7 | Dislike doctors/Afraid | ||||
| 1.3 | Personal/Family responsibilities | ||||
| 0.6 | Language problems | ||||
Because healthcare delivery and planning occur largely at the provincial level, it is useful to evaluate the reasons for unmet need by province. Based on data from the 1998/99 NPHS, rates of perceived unmet need ranged from 4.5% in Newfoundland to 8.3% in Manitoba (Wilson and Rosenberg 2002). Differences in reasons for unmet need among some provinces have also been reported; however, these results did not adjust for other determinants of healthcare utilization (Chen and Hou 2002).
The purpose of this study was to assess provincial variation in unmet need in general and across the three categories of reasons: availability, accessibility and acceptability. This study also explored the contribution to unmet need of other determinants, including demographic factors, health status and socio-economic variables.
Methods
This was a cross-sectional study of the population of the 10 Canadian provinces, using data from the Canadian Community Health Survey (CCHS 2.1) conducted in 2003. Self-perceived unmet need was compared across the provinces while taking into account known determinants of access according to Anderson's Health Behaviour Model (Andersen 1995).
The CCHS is a national population health survey aimed at describing the health and health services experiences of Canadians. The survey sample for this study included 111,258 non-proxy survey respondents aged 20 or older who lived in one of the 10 Canadian provinces in 2003. After applying the weights that adjust for the multistaged cluster sampling design and the distribution of responses, the survey represents approximately 22.6 million people, or 69.5% of the Canadian population. The CCHS excluded residents of Indian reserves, Crown lands, certain remote areas, institutions and full-time members of the Canadian Forces (Statistics Canada 2005).
The outcome variable, self-perceived unmet need, is the response to the survey question, “During the past 12 months, was there ever a time when you felt that you needed healthcare but didn't receive it?” The reasons for unmet need are the response to the question, “Thinking of the most recent time, why didn't you get care?” The reported reasons were categorized into the three categories of availability, accessibility and acceptability as reported by Chen and Hou (Table 1) (Chen and Hou 2002).
The independent predictor variables were selected based on Andersen's Health Behaviour Model (HBM). The HBM is a framework that is designed to assist in the understanding of the determinants of health services use and patient satisfaction (Andersen 1995). These predictors were identified as components of contextual characteristics, need, predisposing characteristics and enabling resources. Contextual characteristics were indicated as the province of residence and Statistical Area Classification (SAC), which indicates the rural–urban status of the respondents' municipality of residence (du Plessis et al. 2001).
Two measures of need are used in this study: the presence of chronic conditions and self-rated health status. The measure of chronic conditions indicates whether subjects have zero, one or two or more chronic conditions (Table 2). Self-rated health status has been shown to be strongly related to utilization of healthcare services (Eyles et al. 1991). This measure has the five categories excellent, very good, good, fair and poor, which are rated by survey respondents in response to the question, “In general, would you say your health is…?”
TABLE 2.
Chronic conditions
| Asthma | Cataracts |
| Fibromyalgia | Glaucoma |
| Arthritis or rheumatism | Thyroid condition |
| High blood pressure | Chronic fatigue syndrome |
| Migraine headaches | Multiple chemical sensitivities |
| Diabetes | Schizophrenia |
| Epilepsy | Mood disorder |
| Heart disease | Anxiety disorder |
| Cancer | Other developmental disorder |
| Stomach or intestinal ulcers | Eating disorder |
| Effects of stroke | Chronic bronchitis |
| Bowel disorder/Crohn's or colitis | Emphysema of COPD |
| Alzheimer's disease or other dementia | Other long-term health conditions |
Predisposing characteristics describe an individual's propensity to use healthcare services and are generally demographic factors that are related to utilization and are not easily altered. The predisposing variables used in this study were sex, age, marital status, educational attainment and ethnic or cultural origin. Enabling resources are the means that individuals have available to them for the use of healthcare services. The more enabling resources that exist, the greater the likelihood that health services will be used (given that there is a need). Enabling resources include having a regular medical doctor, adequate household income and pharmaceutical insurance, and occupational class.
The analytical approach for this study consisted of constructing multivariate logistic regression models following the steps outlined by Hosmer and Lemeshow (2000) and calculating least squared means to determine an adjusted percentage for each province. The CCHS used a probability sample – that is, each subject was assigned a weight indicating the number of individuals in the population that they are meant to represent. Because of the complex nature of the survey design, a bootstrap re-sampling technique was used to estimate the adjusted variances and confidence intervals.
Results
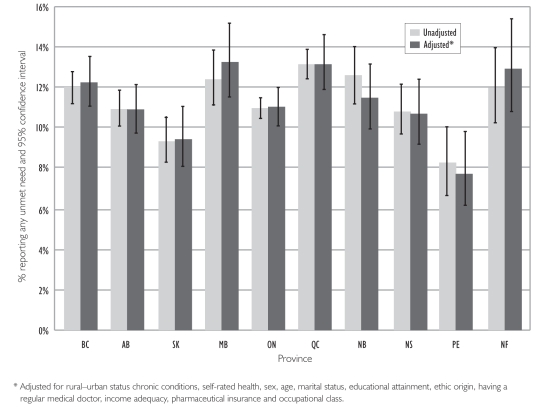
Overall, 11.7% reported having had unmet healthcare needs in the previous 12 months. Table 3 gives the demographic distribution of the study population and those reporting self-perceived unmet need. Unmet need was more common among women, younger people, those with higher educational attainment and those with lower household income. Figure 1 shows the unadjusted and adjusted rate of self-perceived unmet need by province. The unadjusted provincial rates for overall unmet need varied from 13.1% in Quebec to 8.2% in Prince Edward Island. Adjusting for other factors associated with unmet need resulted in slight changes in the rank order, with the highest rate in Manitoba (13.3%) and the lowest in Prince Edward Island (7.8%).
TABLE 3.
Distribution of study population and self-perceived unmet need
| Variable | Study population (%) | Reported unmet need (%) |
|---|---|---|
| Sex | ||
| Female | 51.3 | 13.1 |
| Male | 48.7 | 10.1 |
| Age | ||
| 20 to 29 years | 18.4 | 15.2 |
| 30 to 39 years | 19.9 | 13.5 |
| 40 to 49 years | 22.5 | 12.2 |
| 50 to 59 years | 17.6 | 10.6 |
| 60 to 69 years | 11.1 | 7.9 |
| 70 to 79 years | 7.6 | 7.1 |
| 80+ years | 3.1 | 4.7 |
| Educational Attainment | ||
| < Secondary school graduation | 18.5 | 9.9 |
| Secondary school graduation | 19.3 | 10.3 |
| Some post-secondary | 7.7 | 14.4 |
| Post-secondary graduation | 54.5 | 12.4 |
| Income Adequacy | ||
| Low income | 7.6 | 16.0 |
| Middle or high income | 80.2 | 11.4 |
| Not stated | 12.3 | 10.8 |
| Province | ||
| British Columbia | 13.4 | 12.0 |
| Alberta | 9.7 | 10.9 |
| Saskatchewan | 3.0 | 9.3 |
| Manitoba | 3.4 | 12.4 |
| Ontario | 38.7 | 11.0 |
| Quebec | 24.2 | 13.1 |
| New Brunswick | 2.4 | 12.5 |
| Nova Scotia | 3.0 | 10.9 |
| Prince Edward Island | 0.4 | 8.2 |
| Newfoundland | 1.7 | 12.0 |
FIGURE 1.
Self-perceived unmet need by province
Among those reporting unmet health services needs, the leading reason was problems with availability of services (54.9%), followed by acceptability (42.8%) and accessibility (12.7%), respectively. (Because respondents could select more than one reason, the percentages do not total 100%.) Table 1 shows the breakdown by reasons within each category.
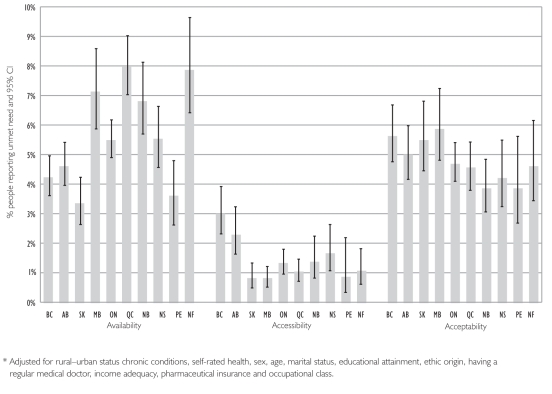
The adjusted percentages of self-perceived unmet need by reason are illustrated by province in Figure 2. Unmet healthcare need due to problems of availability was most likely in Quebec, Newfoundland and Manitoba and least likely in Saskatchewan, Prince Edward Island, British Columbia and Alberta. Alberta and British Columbia had the highest likelihood of unmet need due to problems of accessibility, with little variation among the other provinces. There was less variation in unmet need due to problems of acceptability, with British Columbia, Saskatchewan and Manitoba more likely to report problems and New Brunswick, Nova Scotia and Prince Edward Island less likely.
FIGURE 2.
Unmet need by reported reason*
The placement of each province within the rank order varies depending on the stated reason (Table 4). Only two provinces had a constant ranking for all three causes: Ontario, with mid-range rankings, and Prince Edward Island, with low levels of unmet need for all reasons. Manitoba showed the most notable differences, with the highest rate of unmet need due to acceptability problems and the lowest rate for problems of accessibility. British Columbia and Alberta, the two most western provinces, had the highest percentage of unmet need due to problems of accessibility, with moderately high levels of acceptability-related unmet need and low levels of availability-related unmet need. Quebec and Newfoundland, two of the most eastern provinces, both had moderate to low levels of unmet need due to acceptability and accessibility, and the highest level of need due to availability. Because problems of availability were most common, they were most closely aligned with all-cause unmet need.
TABLE 4.
Rank order of provinces by adjusted* rates of self-perceived unmet need, overall and by reason
| Province | Overall unmet need | Reason for unmet need | ||
|---|---|---|---|---|
| Availability | Accessibility | Acceptability | ||
| BC | 4 | 8 | 1 | 2 |
| AB | 7 | 7 | 2 | 4 |
| SK | 9 | 10 | 9 | 3 |
| MB | 1 | 3 | 10 | 1 |
| ON | 6 | 6 | 5 | 5 |
| QC | 2 | 1 | 7 | 7 |
| NB | 5 | 4 | 4 | 10 |
| NS | 8 | 5 | 3 | 8 |
| PE | 10 | 9 | 8 | 9 |
| NF | 3 | 2 | 6 | 6 |
1 = highest/most unmet need; 10 = lowest/least unmet need
Adjusted for rural–urban status chronic conditions, self-rated health, sex, age, marital status, educational attainment, ethnic origin, having a regular medical doctor, income adequacy, pharmaceutical insurance and occupation class.
Table 5 shows the adjusted odds ratios for all factors associated with unmet need that were controlled for in this analysis. Residents of rural communities were less likely to report unmet need overall or due to problems of availability or accessibility. Although they follow the same trend, differences across the rural–urban spectrum in unmet need due to problems of acceptability were small (to view Table 5 go to: http://www.longwoods.com/product.php?productid=20934).
TABLE 5.
Multivariate logistic regression models for overall unmet need and each reason
| Variable | Overall | Availability | Accessibility | Acceptability |
|---|---|---|---|---|
| Place of Residence | ||||
| Province | ||||
| British Columbia† | 1.00 | 1.00 | 1.00 | 1.00 |
| Alberta | 0.87 (0.77, 0.99)* | 1.10 (0.93, 1.31) | 0.75 (0.62, 0.90)** | 0.88 (0.74, 1.05) |
| Saskatchewan | 0.75 (0.63, 0.89)** | 0.79 (0.61, 1.01) | 0.27 (0.19, 0.38)** | 0.97 (0.77, 1.22) |
| Manitoba | 1.09 (0.93, 1.28) | 1.73 (1.38, 2.16)** | 0.26 (0.17, 0.40)** | 1.05 (0.83, 1.32) |
| Ontario | 0.88 (0.80, 0.97)* | 1.31 (1.14, 1.51)** | 0.43 (0.34, 0.54)** | 0.83 (0.71, 0.96)* |
| Quebec | 1.09 (0.98, 1.21) | 1.95 (1.69, 2.26)** | 0.34 (0.25, 0.46)** | 0.80 (0.68, 0.94)** |
| New Brunswick | 0.93 (0.80, 1.08) | 1.65 (1.34, 2.03)** | 0.45 (0.31, 0.65)** | 0.67 (0.53, 0.85)** |
| Nova Scotia | 0.86 (0.73, 1.01) | 1.32 (1.08, 1.61)* | 0.55 (0.40, 0.75)** | 0.74 (0.57, 0.96)* |
| Prince Edward Island | 0.60 (0.47, 0.78)** | 0.83 (0.61, 1.13) | 0.29 (0.14, 0.59)** | 0.68 (0.45, 1.01) |
| Newfoundland | 1.06 (0.87, 1.30) | 1.93 (1.53, 2.43)** | 0.35 (0.19, 0.64)** | 0.81 (0.59, 1.11) |
| Statistical Area Classification‡ | ||||
| Urban – CMA | 0.89 (0.82, 0.96)** | 0.80 (0.73, 0.89)** | 1.02 (0.79, 1.31) | 0.98 (0.87, 1.10) |
| Urban – CA† | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural – Strong MIZ | 0.85 (0.73, 0.98)* | 0.82 (0.68, 0.99)* | 0.56 (0.40, 0.80)** | 0.94 (0.76, 1.17) |
| Rural – Moderate MIZ | 0.80 (0.72, 0.90)** | 0.75 (0.65, 0.87)** | 0.81 (0.55, 1.17) | 0.87 (0.72, 1.06) |
| Weak or No MIZ | 0.84 (0.75, 0.93)** | 0.91 (0.79, 1.03) | 0.80 (0.65, 0.99)* | 0.86 (0.73, 1.00) |
| Need | ||||
| Chronic Conditions | ||||
| None | 0.74 (0.67, 0.83)** | 0.81 (0.71, 0.92)** | 0.50 (0.40, 0.63)** | 0.74 (0.64, 0.87)** |
| 1 chronic condition† | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 or more conditions | 1.67 (1.52, 1.84)** | 1.79 (1.59, 2.02)** | 1.49 (1.20, 1.85)** | 1.44 (1.26, 1.64)** |
| Self-rated Health | ||||
| Excellent | 0.45 (0.41, 0.50)** | 0.45 (0.40, 0.52)** | 0.55 (0.41, 0.74)** | 0.45 (0.38, 0.52)** |
| Very good | 0.67 (0.62, 0.73)** | 0.67 (0.60, 0.74)** | 0.65 (0.54, 0.79)** | 0.71 (0.63, 0.80)** |
| Good† | 1.00 | 1.00 | 1.00 | 1.00 |
| Fair | 1.60 (1.45, 1.76)** | 1.43 (1.26, 1.62)** | 1.54 (1.19, 1.99)** | 1.66 (1.44, 1.92)** |
| Poor | 3.36 (2.87, 3.94)** | 2.94 (2.44, 3.54)** | 3.04 (2.16, 4.27)** | 3.09 (2.52, 3.78)** |
| Predisposing Characteristics | ||||
| Sex | ||||
| Female† | 1.00 | 1.00 | 1.00 | 1.00 |
| Male | 0.72 (0.68, 0.78)** | 0.67 (0.61, 0.73)** | 0.73 (0.60, 0.89)** | 0.82 (0.74, 0.91)** |
| Age | ||||
| 20 to 29 years | 1.13 (1.01, 1.27)* | 0.90 (0.77, 1.05) | 0.94 (0.65, 1.35) | 1.59 (1.34, 1.89)** |
| 30 to 39 years | 1.79 (1.62, 1.99)** | 1.53 (1.34, 1.75)** | 1.48 (1.19, 1.84)** | 2.10 (1.80, 2.44)** |
| 40 to 49 years | 1.42 (1.29, 1.57)** | 1.29 (1.12, 1.48)** | 1.35 (1.01, 1.82)* | 1.63 (1.42, 1.88)** |
| 50 to 59 years† | 1.00 | 1.00 | 1.00 | 1.00 |
| 60 to 69 years | 0.67 (0.59, 0.67)** | 0.75 (0.64, 0.88)** | 0.61 (0.44, 0.83)** | 0.64 (0.53, 0.77)** |
| 70 to 79 years | 0.52 (0.45, 0.60)** | 0.57 (0.47, 0.70)** | 0.48 (0.30, 0.79)** | 0.59 (0.46, 0.74)** |
| 80+ years | 0.30 (0.25, 0.36)** | 0.29 (0.23, 0.37)** | 0.24 (0.15, 0.40)** | 0.44 (0.33, 0.57)** |
| Marital Status | ||||
| Married or equivalent† | 1.00 | 1.00 | 1.00 | 1.00 |
| Single/divorced/widowed | 1.03 (0.96, 1.10) | 0.94 (0.86, 1.02) | 1.31 (1.07, 1.61)** | 1.06 (0.96, 1.17) |
| Educational Attainment | ||||
| < Secondary graduation | 0.97 (0.86, 1.09) | 0.85 (0.74, 0.99)* | 1.26 (1.02, 1.56)* | 1.07 (0.91, 1.27) |
| Secondary graduation† | 1.00 | 1.00 | 1.00 | 1.00 |
| Other post-secondary | 1.39 (1.22, 1.58)** | 1.33 (1.13, 1.56)** | 1.69 (1.29, 2.21)** | 1.30 (1.07, 1.57)** |
| Post-secondary graduation | 1.29 (1.18, 1.42)** | 1.40 (1.26, 1.55)** | 1.40 (1.15, 1.70)** | 1.10 (0.95, 1.26) |
| Ethnic or Cultural Origin | ||||
| White† | 1.00 | 1.00 | 1.00 | 1.00 |
| Not White | 0.90 (0.81, 1.01) | 0.96 (0.83, 1.12) | 1.22 (1.00, 1.50)* | 0.83 (0.71, 0.97)* |
| Enabling Resources | ||||
| Has a Regular Medical Doctor | ||||
| Yes† | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 1.69 (1.54, 1.85)** | 1.55 (1.49, 1.85)** | 1.40 (1.07, 1.83)** | 1.78 (1.56, 2.03)** |
| Income Adequacy (2 cats) | ||||
| Low income | 1.19 (1.06, 1.33)** | 1.03 (0.88, 1.21) | 1.51 (1.26, 1.80)** | 1.26 (1.08, 1.48)** |
| Middle or high income† | 1.00 | 1.00 | 1.00 | 1.00 |
| Unknown, NA or not stated | 0.92 (0.81, 1.04) | 1.00 (0.86, 1.17) | 0.98 (0.76, 1.26) | 0.84 (0.70, 1.01) |
| Has Pharmaceuticals Insurance | ||||
| Yes† | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 1.20 (1.11, 1.29)** | 1.05 (0.95, 1.15) | 2.56 (2.17, 3.01)** | 1.01 (0.90, 1.13) |
| Occupation Class | ||||
| Business/social services/healthcare † | 1.00 | 1.00 | 1.00 | 1.00 |
| Sales and service | 0.96 (0.88, 1.05) | 0.86 (0.76, 0.97)* | 1.39 (1.09, 1.78)** | 0.99 (0.87, 1.12) |
| Trades/transport/primary | 1.01 (0.91, 1.11) | 0.87 (0.76, 0.99) | 1.31 (1.01, 1.71)* | 1.08 (0.93, 1.25) |
| Not employed | 0.85 (0.76, 0.94)** | 0.82 (0.72, 0.94)** | 1.16 (0.91,1.47) | 0.84 (0.72, 0.99)* |
Odds ratio (95% CI). Higher numbers indicate a greater odds of the outcome.
p< 0.05, ** p< 0.01
Reference category
CMA = Census Metropolitan Area; CA = Census Amalgamation; MIZ = Metropolitan Influence Zone
Higher need was associated with increased odds of reporting unmet need overall and for each of the three reasons. There were some differences among the predisposing characteristics. Women were more likely to report unmet need for each reason. Age was negatively associated with reporting unmet need overall and for each of the three reasons. Level of educational attainment had a strong association; those with the highest level of education were most likely to report unmet need overall and need due to problems of availability or accessibility. Some differences were observed among the enabling resources. People without a regular medical doctor were more likely to report unmet healthcare need for each of the three reasons. People in the lowest income quintile were more likely to report unmet need due to problems of accessibility. People without pharmaceutical insurance were much more likely to report unmet need related to problems of accessibility.
Discussion
We found provincial variations in unmet need overall, and large variations in reasons for unmet need among some provinces. Overall rates of unmet need reported in 2003 did not increase from the 2000/01 cycle of the CCHS (Sanmartin et al. 2002). The overall rate for Canada (11.7%) was lower than the rate reported for the United States population (18%) but higher than the estimated rate for the insured population of the United States (6.8%) (Pagan and Pauly 2006).
The 2003 data used in this study show Quebec having the highest unadjusted rate of unmet need; this figure is more than double that found in the 1998/99 NPHS (Wilson and Rosenberg 2002). Whether organizational factors might have contributed to this change in self-reported unmet need is unknown; however, over the time in question (1999 to 2003), the Chaoulli case was working its way through the courts in Quebec (Flood and Xavier 2008; Pinker 1999). The media attention that was given to this claim – that unduly long wait times for necessary healthcare violated the Quebec Charter of Human Rights and Freedoms – may have altered the Quebec public's perception of the availability and accessibility of healthcare services and thus influenced their responses to this survey question.
The province with the lowest level of unmet need in 2003 was Prince Edward Island. Although its level was higher than that reported in 1998/99, the province did not change substantially in rank, moving from the second lowest to lowest (Wilson and Rosenberg 2002). Manitoba had the second highest unadjusted rate and the highest adjusted rate – not a change in rank from 1998/99, when it had the highest unadjusted rate (Wilson and Rosenberg 2002). Adjusted provincial comparisons of self-reported unmet need have not previously been reported. Because of the smaller sample sizes in the NPHS, statistically significant relationships among many of the factors associated with the reasons for unmet need could not be identified (Chen and Hou 2002; Wilson and Rosenberg 2002).
This study shows availability to be the most common category of reasons for unmet need, while previous research based on 1998/99 data showed availability as the second most common reason (Chen and Hou 2002). The most common single reason related to availability was long waiting times; this was also the most common single reason in 1998/99 and 2000/01 (Sanmartin et al. 2002). The residents of the provinces of Quebec, Newfoundland and Manitoba were most likely to report unmet need due to problems of availability. This finding does not correlate directly with the supply of family physicians in these provinces in the survey year, 2003. At that time, Quebec had 104 family physicians per 100,000 population, a figure higher than the national average of 96, while Manitoba had less than the national average, with 92 per 100,000, and Newfoundland had about average (CIHI 2007). These findings also do not correlate with reported wait times for specialists or surgery in that period (Esmail and Walker 2003).
The second most common category of reasons for unmet need is acceptability; in 1998/99, this was the most common reason (Chen and Hou 2002). These reasons are related to personal preferences or circumstances of individuals and are mostly unrelated to characteristics of healthcare services.
The least common reasons for unmet need were those related to accessibility, reported at the same rate as in 1998/99. Residents of British Columbia and Alberta were most likely to have unmet need due to problems of accessibility. This finding may be related to population distribution in these provinces, with the majority of tertiary services centralized at a few locations, although this analysis does control for rural– urban status. The majority of people who reported problems of accessibility cited cost as the primary barrier. Health insurance premiums account for the largest proportion of out-of-pocket healthcare costs in Canada. In 2002, British Columbia, Alberta and Quebec were the only provinces that had public healthcare premiums in place (Luffman 2005); however, because these premiums are collected by the government (often as a payroll deduction) and not at the point of care, this factor is unlikely to account for higher rates of unmet need due to cost in British Columbia and Alberta. There is no evidence that higher private insurance premiums are charged in these two provinces. The third most common category of out-of-pocket costs is eye care goods and services; in 2002, routine eye care for those between the ages of 18 and 65 was delisted from the BC health insurance plan. However, many other provinces had not covered routine eye care prior to that – Alberta, Saskatchewan, Manitoba, Quebec, Nova Scotia, Prince Edward Island and Newfoundland (Stabile and Ward 2006). There is no evidence that residents of British Columbia or Alberta pay higher out-of-pocket costs for the other common categories of dental services, prescription drugs or other drugs (Luffman 2005).
Unmet need due to problems of availability is the most common and most variable reason across provinces; it also has the greatest potential for policy intervention. Barriers to availability include too-lengthy waiting time, lack of services when required and lack of services in a particular area – all factors that governments and health authorities/regions could potentially alter. Strategies to address these potential barriers to access include increasing available services through the use of primary care teams, non-physician care providers such as physician assistants or nurse practitioners, and telephone advisory services. Some areas of Canada have successfully implemented telemedicine programs that expand the delivery of services in dermatology, radiology, cardiology and diabetes (Cheung et al. 1998; Dunscombe and Roberts 2001; Jin et al. 2003; Reid et al. 1998). Decentralized service delivery can also be implemented to reduce travel time from patients' homes to healthcare services and associated out-of-pocket costs (Roberts et al. 2002; Seto 2008). Given that a too-lengthy wait time is the most common reason for reporting unmet need, particular attention should be focused on this barrier. Little is known about waiting times for primary care; international comparisons show that Canada has a great deal of room to improve in access to primary care (Schoen et al. 2005; Walberg et al. 2008), and that enhanced access is possible through better scheduling practices, without increasing costs or healthcare personnel (Murray and Berwick 2003). There is also evidence that surgical wait times can be reduced by centralizing wait lists and wait list management (Priest et al. 2007).
While unmet need due to availability has increased since 1998/99 (Chen and Hou 2002), it is unclear whether actual availability, or just public perception, has changed. Either way, the problem of availability is important to policy makers and healthcare providers particularly in Quebec, Newfoundland and Manitoba, where the lack is greatest. Also important is the higher rates of perception of unmet need due to accessibility in British Columbia and Alberta, where the additional travel time and related costs may be preventing people from getting needed healthcare services. Unmet need due to problems of acceptability presents a quandary, as it generally results from individual patient perceptions and not necessarily from factors that can be addressed by health policy. Further research to understand acceptability would help with the interpretation of this variable.
Limitations
The limitations of this study are largely related to the design and conduct of the Canadian Community Health Survey (CCHS). Because the study is based on survey data, there is a risk of recall bias; respondents were asked about unmet need and the reason for it in only the previous 12 months, an approach that could potentially lead to an underestimation of problems with unmet needs. There are also limitations related to the sample selection for the survey, the most notable being the exclusion of a large number of Aboriginal Canadians, an omission that may result in overestimating the level of access in rural areas. While this study describes some characteristics of unmet need and the variation across provinces, it is unable to elucidate causes for this variation.
Conclusion
This study found that after controlling for other factors, higher rates of unmet need were reported among people who resided in urban communities, had poorer health status, had physician-diagnosed chronic conditions, were female, were of younger age, had more education, had lower income, did not have a regular medical doctor and did not have pharmaceutical insurance. These are similar to the findings of Kasman and Badley (2004), based on data from the 2001 CCHS. The odds ratios for most determinants of unmet need except province were similar across the categories of reasons.
Future research on self-perceived unmet need should focus on distinguishing between unmet need that is related to public and personal perceptions versus that which is directly mutable by government and health policy makers. These further analyses could help identify factors that are associated with provincial variation, such as the supply of physicians and services, and the location and distribution of services within provinces.
Acknowledgements
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Lyn Sibley was supported by a postdoctoral fellowship from the Canadian Institute of Health Research and the Institute for Health Services and Policy Research (CIHR–IHSPR).
Contributor Information
Lyn M. Sibley, Postdoctoral Fellow, Institute for Clinical Evaluative Sciences, Health System Performance Research Network, Department of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Richard H. Glazier, Senior Scientist, Institute for Clinical Evaluative Sciences, Scientist, Centre for Research on Inner City Health, St. Michael's Hospital; Associate Professor, Department of Family and Community Medicine, University of Toronto, Toronto, ON.
References
- Andersen R.M. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI) Supply, Distribution and Migration of Canadian Physicians, 2006. 2007 Retrieved May 27, 2009. < http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=PG_870_E&cw_topic=870&cw_rel=AR_14_E#full>.
- Chen J., Hou F. Unmet Needs for Health Care. Health Reports. 2002;13(2):23–34. [PubMed] [Google Scholar]
- Cheung S.T., Davies R.F., Smith K., Marsh R., Sherrard H., Keon W.J. The Ottawa Telehealth Project. Telemedicine Journal. 1998;4(3):259–66. doi: 10.1089/tmj.1.1998.4.259. [DOI] [PubMed] [Google Scholar]
- du Plessis V., Beshiri R., Bollman R.D., Clemenson H. Rural and Small Town Canada Analysis Bulletin 3(3). Cat. No. 21-006-XIE2001003. Ottawa: Statistics Canada; 2001. Definitions of Rural. Retrieved May 27, 2009. < http://www.statcan.gc.ca/bsolc/olc-cel/olc-cel?catno=21-006-XIE2001003&lang=eng>. [Google Scholar]
- Dunscombe P., Roberts G. Radiotherapy Service Delivery Models for a Dispersed Patient Population. Clinical Oncology (Royal College of Radiologists) 2001;13(1):29–37. doi: 10.1053/clon.2001.9211. [DOI] [PubMed] [Google Scholar]
- Esmail N., Walker M. Waiting Your Turn: Hospital Waiting Lists in Canada. 13th ed. Vancouver: The Fraser Institute; 2003. [Google Scholar]
- Eyles J., Birch S., Chambers S., Hurley J., Hutchison B. A Needs-Based Methodology for Allocating Health Care Resources in Ontario, Canada: Development and an Application. Social Science and Medicine. 1991;33(4):489–500. doi: 10.1016/0277-9536(91)90331-6. [DOI] [PubMed] [Google Scholar]
- Flood C.M., Xavier S. Health Care Rights in Canada: The Chaoulli Legacy. Medicine and Law. 2008;27(3):617–44. [PubMed] [Google Scholar]
- Hosmer D.W., Lemeshow S. Applied Logistic Regression. New York: John Wiley & Sons; 2000. [Google Scholar]
- Hutchison B. Disparities in Healthcare Access and Use: Yackety-Yack, Yackety-Yack. Healthcare Policy. 2007;3(2):10–13. [PMC free article] [PubMed] [Google Scholar]
- Jin A., Martin D., Maberley D., Dawson K., Seccombe D., Beattie J. Evaluation of a Mobile Diabetes Care Telemedicine Clinic Serving Aboriginal Communities in Northern British Columbia, Canada. Circumpolar Health. 2003;62(2):124–28. doi: 10.3402/ijch.v63i0.17871. [DOI] [PubMed] [Google Scholar]
- Kasman N.M., Badley E.M. Beyond Access: Who Reports That Health Care Is Not Being Received When Needed in a Publicly Funded Health Care System? Canadian Journal of Public Health. 2004;95(4):304–8. doi: 10.1007/BF03405137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luffman J. Out-of-Pocket Spending on Prescription Drugs. Perspectives on Labour and Income. 2005;6(9):5–13. [Google Scholar]
- Murray M., Berwick D.M. Advanced Access: Reducing Waiting and Delays in Primary Care. Journal of the American Medical Association. 2003;289(8):1035–40. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- Pagan J.A., Pauly M.V. Community-Level Uninsurance and the Unmet Medical Needs of Insured and Uninsured Adults. Health Services Research. 2006;41(3 Pt. 1):788–803. doi: 10.1111/j.1475-6773.2006.00506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinker S. The Chaoulli Case: One-Tier Medicine Goes on Trial in Quebec. Canadian Medical Association Journal. 1999;161(10):1305–6. [PMC free article] [PubMed] [Google Scholar]
- Priest A., Rachlis A., Cohen M. Vancouver: Canadian Centre for Policy Alternatives and the BC Health Coalition; 2007. Why Wait? Public Solutions to Cure Surgical Waitlists. [Google Scholar]
- Reid D.S., Weaver L.E., Sargeant J.M., Allen M.J., Mason W.F., Klotz P.J., Langille D.B. Telemedicine in Nova Scotia: Report of a Pilot Study. Telemedicine Journal. 1998;4(3):249–58. doi: 10.1089/tmj.1.1998.4.249. [DOI] [PubMed] [Google Scholar]
- Roberts G.H., Dunscombe P.B., Samant R.S. Geographic Delivery Models for Radiotherapy Services. Australasian Radiology. 2002;46(3):290–94. doi: 10.1046/j.1440-1673.2002.01062.x. [DOI] [PubMed] [Google Scholar]
- Sanmartin C., Houle C., Tremblay S., Berthelot J.M. Changes in Unmet Health Care Needs. Health Reports. 2002;13(3):15–21. [PubMed] [Google Scholar]
- Schoen C., Osborn R., Huynh P.T., Doty M., Zapert K., Peugh J., Davis K. Taking the Pulse of Health Care Systems: Experiences of Patients with Health Problems in Six Countries. Health Affairs (Millwood) Web Exclusives: W5–25. 2005 Nov 3; doi: 10.1377/hlthaff.w5.509. Retrieved May 27, 2009.< http://content.healthaffairs.org/cgi/content/abstract/hlthaff.w5.509>. [DOI] [PubMed] [Google Scholar]
- Seto E. Cost Comparison between Telemonitoring and Usual Care of Heart Failure: A Systematic Review. Telemedicine Journal and E-Health. 2008;14(7):679–86. doi: 10.1089/tmj.2007.0114. [DOI] [PubMed] [Google Scholar]
- Stabile M., Ward C. The Effects of Listing Public Health Care Services. In: Beach C., Chaykowski R., Shortt S., St-Hilaire F., Sweetman A., editors. Health Services Restructuring: New Evidence and New Directions. Kingston, ON: McGill-Queen's University Press; 2006. [Google Scholar]
- Statistics Canada. Canadian Community Health Survey 2003: User Guide for the Public Use Microdata File. Ottawa: Author; 2005. Cat. No. 82M0013XCB. [Google Scholar]
- Walberg M., Björnberg A., Nagy R. Euro-Canada Health Consumer Index 2008. Health Consumer Powerhouse AB and Frontier Centre for Public Policy. 2008 Retrieved may 27, 2009. < http://www.fcpp.org/pdf/ECHCI2008finalJanuary202008.pdf>. [Google Scholar]
- Wilson K., Rosenberg M.W. The Geographies of Crisis: Exploring Accessibility to Health Care in Canada. Canadian Geographer. 2002;46(3):223–34. [Google Scholar]