Abstract
Acute myocardial infarction (AMI) is rare in patients with idiopathic thrombocytopenic purpura (ITP). We describe a case of an AMI during thrombocytopenia in a patient with chronic ITP. A 47-yr-old woman presented with anterior chest pain and a low platelet count (21,000/µL) at admission. Urgent coronary angiography revealed total occlusion of proximal right coronary artery and primary percutaneous coronary intervention (PCI) was performed successfully. This case suggests that primary PCI may be a therapeutic option for an AMI in patients with ITP, even though the patient had severe thrombocytopenia.
Keywords: Myocardial Infarction; Percutaneous Coronary Intervention; Purpura, Thrombocytopenic, Idiopathic
INTRODUCTION
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder characterized by a low platelet count and mucocutaneous bleeding (1). The incidences of atherosclerosis and myocardial infarction in patients with congenital coagulation disorders and chronic thrombocytopenia are very low (2). Even though thrombotic events occur in patients with chronic ITP, most cases were reported during or shortly after intravenous immunoglobulin (IVIG) administration, when platelet counts began to rise (3, 4).
Thrombolytic therapy is contraindicated for a patient with ITP even with acute myocardial infarction (AMI) (5). Few cases of primary percutaneous coronary intervention (PCI) for AMI in patients with ITP have been reported (6, 7).
This report describes a case of AMI that occurred during thrombocytopenia in a patient with ITP and managed successfully by PCI without major bleeding complications.
CASE REPORT
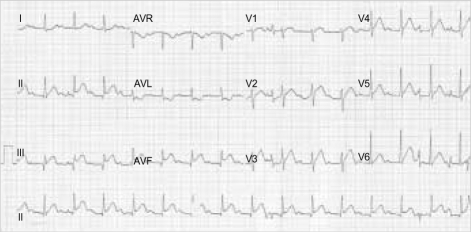
A 47-yr-old woman was transferred to the emergency room with anterior chest pain. Three years ago, she was diagnosed as chronic ITP. The patient has taken steroids for ITP and an antidiabetic drug for type 2 diabetes mellitus (DM). Because the patient was diagnosed as type 2 DM only after she took steroids, probably, it was regarded as drug-induced DM. Chest pain had developed 6 hr before an arrival at emergency room, and she had already been treated with nitroglycerin and beta blocker at other hospital. Electrocardiogram (ECG) showed ST segment elevation in the leads of II, III, and aVF, which was consistent with an inferior wall AMI (Fig. 1). The patient was alert, her blood pressure was 140/90 mmHg with a pulse rate of 78 beats per minute, and respiration at the rate of 21 per minute. Heart sounds were normal without gallop sound or significant murmur. The cardiac enzymes were elevated: the level of CK was 520 U/L (normal range: 20-180 U/L) and CK-MB 109 U/L (normal range: 0-6 U/L). Platelet count was 21,000/µL. Blood coagulation tests showed prothrombin time (PT) of 9.75 sec (international normalized ratio [INR]; 0.76) and activated partial thromboplastin time (aPTT) of 30.6 sec. Chest radiography showed no pulmonary congestion with cardiothoracic ratio of 50%.
Fig. 1.
Electrocardiogram shows the first degree atrioventricular block and ST segment elevation in leads of II, III, and aVF.
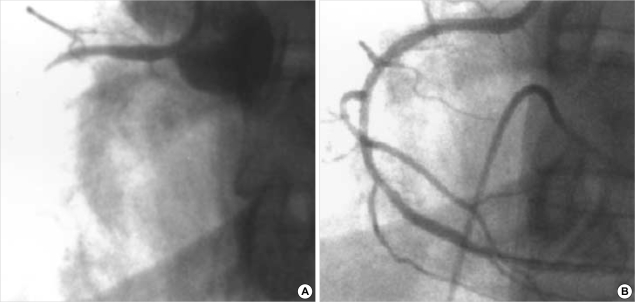
Urgent diagnostic coronary angiography revealed total occlusion in the proximal right coronary artery (RCA) (Fig. 2A), and normal left coronary artery (LCA). Loading dose of clopidogrel (300 mg) was administered and then PCI was performed using a balloon and a stent for the proximal RCA lesion successfully (Fig. 2B). During the PCI, temporary pacemaker was inserted due to sinus arrest.
Fig. 2.
Coronary angiography of the right coronary artery on left anterior oblique view. (A) Total obstruction in the proximal right coronary artery before percutaneous coronary intervention (PCI). (B) After the PCI with the aid of temporary pacemaker, successful reperfusion was obtained without residual stenosis.
Bolus injection of 2,000 units heparin was done at the beginning of the coronary angiography and then additional 6,000 units during the PCI. Activated partial thromboplastin time was within normal range (42.8 sec). On the next day, platelet count was 18,000/µL and ecchymoses were found around the puncture site of the right femoral artery. Heparin was not administered any more in the intensive care unit after the PCI, but combined anti-platelet therapy (aspirin 200 mg and clopidogrel 75 mg) was performed as usual. IVIG administration was started to prevent hemorrhagic complications. After the removal of the sheath introducers from the right femoral artery, we compressed the puncture sites for more than 30 min to achieve complete hemostasis. No other bleeding complications occurred. The patient was discharged asymptomatically at ten days after PCI.
DISCUSSION
Atherosclerosis and myocardial infarction are rare in patients with chronic thrombocytopenia. In other words, high platelet count has been correlated with high incidence of ischemic heart disease, as well as elevated hemostatic factors (8). If a patient with chronic thrombocytopenia has a coronary artery disease, concomitance of known coronary risk factors such as family history for cardiovascular disease, hypertension, diabetes, dyslipidemia, or cigarette smoking, should be considered. In this case, the patient was obese and had diabetes after steroid treatment for ITP. Steroids are known to induce metabolic changes as well as a hypercoagulable state, each of which may promote atherosclerosis, thus steroids may play a possible role in precipitating the clinical events in this patient (8).
IVIG therapy for ITP has been associated with a very rare occurrence of thrombotic events, such as myocardial infarction and stroke. Paolini et al. (3) suggested that the rapid rise in platelet counts in response to IVIG therapy in ITP may aggravate the potentially adverse effect of increased plasma viscosity leading to increased susceptibility to fatal thrombotic events. When a patient with ITP needs IVIG therapy for thrombocytopenia, careful attention must be paid to a rapid rise in the platelet count, which may induce myocardial infarction or stroke, particularly in the elderly and in patients with coronary risk factors. In this case, AMI occurred before the patient was treated with IVIG.
Because there is an antigenic mimicry between platelets and endothelial cells, the pathogenesis of AMI in thrombocytopenic patients with chronic ITP may stem from endothelial damage induced by autoantibodies directed against antigens presented on both platelets and coronary endothelial cells (9). In this case, the result of platelet associated antigen was weakly positive. Further studies about the relationship between coronary endothelial cell and platelet associated antigen are needed to confirm this hypothesis.
This case reminds us of several precautions in managing a patient with ITP who had AMI during thrombocytopenia. First of all, when puncturing the vessels to insert a sheath introducer, it is important not to injure the vessels and be sure to compress the puncture site for longer than usual after removing the sheath introducer. Percutaneous closing device can be used after PCI, especially in patients with coagulation disorders. Second, there is no recommended dose of heparin in managing an AMI in a patient with ITP, because of extremely rare occurrences of AMI in ITP. We used cautiously small amount of heparin before and during the procedure and IVIG to prevent bleeding complications. Fortunately, there was no specific bleeding complications related to the procedure. Although we did not use conventional dose of heparin, it was enough to manage the patient with AMI during thrombocytopenia. Maybe, small dose of heparin with IVIG therapy can be recommended to treat AMI during thrombocytopenia. Large investigational study should be needed in patients with ITP to find out the optimal dose of heparin. Consequently, the current case suggests that primary PCI can be a useful therapeutic strategy in acute ST elevation myocardial infarction.
References
- 1.Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med. 2002;346:995–1008. doi: 10.1056/NEJMra010501. [DOI] [PubMed] [Google Scholar]
- 2.Juhan-Vague I. Haemostatic parameters and vascular risk. Atherosclerosis. 1996;124(Suppl):49–55. doi: 10.1016/0021-9150(96)05857-1. [DOI] [PubMed] [Google Scholar]
- 3.Paolini R, Fabris F, Cella G. Acute myocardial infarction during treatment with intravenous immunoglobulin for idiopathic thrombocytopenic purpura. Am J Hematol. 2000;65:177–178. doi: 10.1002/1096-8652(200010)65:2<177::aid-ajh17>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 4.Elkayam O, Paran D, Milo R, Davidovitz Y, Almoznino-Sarafian D, Zeltser D, Yaron M, Caspi D. Acute myocardial infarction associated with high dose intravenous immunoglobulin infusion for autoimmune disorders. A study of four cases. Ann Rheum Dis. 2000;59:77–80. doi: 10.1136/ard.59.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antman EM. ST-elevation myocardial infarction: Management. In: Zipes Douglas P., Peter Libby, Bonow Robert O., Braunwald E., editors. Heart Disease: Textbook of Cardiovascular Medicine. 7th ed. Vol 2. Philadelphia: Saunders; 2005. pp. 1167–1226. [Google Scholar]
- 6.Fuchi T, Kondo T, Sase K, Takahashi M. Primary percutaneous transluminal coronary angioplasty performed for acute myocardial infarction in a patient with idiopathic thrombocytopenic purpura. Jpn Circ J. 1999;63:133–136. doi: 10.1253/jcj.63.133. [DOI] [PubMed] [Google Scholar]
- 7.Kikuchi S, Hayashi Y, Fujioka S, Kukita H, Ochi N. A case of intracoronary stent implanted for acute myocardial infarction in an elderly patient with idiopathic thrombocytopenic purpura. Nippon Ronen Igakkai Zasshi. 2002;39:88–93. doi: 10.3143/geriatrics.39.88. [DOI] [PubMed] [Google Scholar]
- 8.Paolini R, Zamboni S, Ramazzina E, Zampieri P, Cella G. Idiopathic thrombocytopenic purpura treated with steroid therapy does not prevent acute myocardial infarction: a case report. Blood Coagul Fibrinolysis. 1999;10:439–442. doi: 10.1097/00001721-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Fruchter O, Blich M, Jacob G. Fatal acute myocardial infarction during severe thrombocytopenia in a patient with idiopathic thrombocytopenic purpura. Am J Med Sci. 2002;323:279–280. doi: 10.1097/00000441-200205000-00010. [DOI] [PubMed] [Google Scholar]