Abstract
Objective: The objective of the present study is to contribute towards the validation of the SOC (Sense of Coherence) construct on the basis of data from psychosomatic patients.
Method: The study included a total of 1403 patients treated as out-patients or in consultations in the Clinic for Psychosomatic Medicine at the Charité University of Medicine, Berlin, between July 2002 and October 2005. Correlations were tested between the sense of coherence (SOC-L9), sociodemographic variables and the following psychometric instruments: Patient Health Questionnaire (PHQ), Brief COPE, Questionnaire on Self-Efficacy, Optimism and Pessimism (SWOP-K9) and Perceived Stress Questionnaire (PSQ-20).
Results: Associations were found between sense of coherence and age, but not with gender. In addition, high sense of coherence was correlated with high self-efficacy, optimism, subjective physical well-being and favourable coping strategies as well as with low perceived stress.
Conclusion: The results contribute to the validation of the SOC construct. Future investigations should include longitudinal studies of the precise association between sense of coherence and other psychological variables.
Keywords: Sense of coherence, salutogenesis, psychosomatic patients, construct validation
Abstract
Zielsetzung: Ziel der vorliegenden Studie ist es, anhand der Daten von psychosomatischen Patienten einen Beitrag zur Konstruktvalidität des SOC (Sense of Coherence) zu leisten.
Methode: In die Untersuchung wurden insgesamt n=1403 Patienten einbezogen, die in der Medizinischen Klinik mit Schwerpunkt Psychosomatik der Charité-Universitätsmedizin Berlin in der Zeit vom Juli 2002 bis Oktober 2005 poliklinisch oder konsiliarisch behandelt wurden. Es wurden Zusammenhänge zwischen dem Kohärenzempfinden (SOC-L9) und soziodemographischen Variablen sowie Korrelationen mit folgenden psychometrischen Instrumenten überprüft: Patient Health Questionnaire (PHQ), Brief-COPE, Fragebogen zu Selbstwirksamkeit, Optimismus und Pessimismus (SWOP-K9) und Perceived Stress Questionnaire (PSQ-20).
Ergebnisse: Es zeigten sich Zusammenhänge zwischen dem Kohärenzempfinden und Alter, nicht aber mit dem Geschlecht. Außerdem ist ein hohes Kohärenzempfinden mit höherer Selbstwirksamkeit, mehr Optimismus, günstigeren Copingstrategien, stärkerem subjektiven physischen Wohlbefinden und weniger subjektiv wahrgenommener Stressbelastung assoziiert.
Fazit: Die Ergebnisse leisten einen Beitrag zur Konstruktvalidität. In weiteren Studien sollten längsschnittlich die genauen Wirkungszusammenhänge von Kohärenzempfinden mit anderen psychologischen Variablen untersucht werden.
Introduction
Psychological and physical stress factors are regarded as risk factors for many psychosomatic diseases. It may, nevertheless, be questioned why not everyone exposed to this psychological or physical stress falls ill. What are the conditions responsible for the maintenance or recovery of health? Lazarus [1], [2] proposed the transactional stress model for the manner in which individuals cope with stress or stressful experiences. This model distinguishes between two evaluation processes. The primary evaluation is the evaluation of the situation as challenge, threat or irrelevance in relation to the well-being of the individual. The secondary evaluation covers the individual’s personal and social resources, i.e. his possibilities of coping with the stressful situation. According to this, stress only becomes damaging stress (“distress”), if the individual evaluates it as such on the basis of deficiencies in his psychosocial resources. “Coping” with stress is the term used for the attempt to deal with the demands of the surrounding world in such a way that negative consequences are avoided. A distinction is made between problem-orientated coping (dealing directly with the stressor by active problem solution) and emotional coping, meaning that no attempt is made to change the stress situation by defensive mechanisms, but rather an attempt for a search of emotional support, changes in thinking about stressors and changes in physical reactions [2].
Following Lazarus [1], Antonovsky [3], [4] formulated a stress concept, according to which stressors do not cause illness in principle, but only trigger a state of tension in an individual, which not necessarily must lead to distress. With his model of salutogenesis, Antonovsky presented an alternative way of viewing the development of disease or rather, the maintenance of health. He emphasised the importance of coping with stress and formulated the concept of “Sense of Coherence, SOC”. Sense of coherence reflects the manner in which the individual views the world and is expressed in a specific underlying attitude to his own person and to the environment [5], [6]. The sense of coherence is nevertheless, not a coping strategy, but permits the individual to make a decision between different coping strategies and to activate resources for coping with stress [7]. Sense of coherence is an overall orientation, expressing the extent to which an individual possesses a stable but dynamic feeling of confidence, penetrating all his attitudes, so that a) stimuli, events or developments are perceived as being structured, ordered and predictable (comprehensibility), b) the necessary resources are available to cope with both internal and external demands (manageability), and c) life is felt to be meaningful and demands are evaluated as challenges deserving investment and dedication [8].
Sense of coherence and sociodemographic variables
The results of empirical studies regarding the association between sense of coherence and gender are heterogenous. There are studies which found that the sense of coherence was lower in men than in women [9], [10], [11], [12], [13], but other studies suggest a lower sense of coherence in women [14], [15], [16] or no differences between genders [17], [18], [19]. Franke postulated that associations between gender and sense of coherence were most likely to be found in clinical studies [7], whereas Bengel et al. [6] found associations in non-clinical studies.
Sense of coherence may change with age. However, no generally valid statement can be made about increases or decreases in sense of coherence with increasing age, as results obtained from multiple studies are too heterogenous [10], [20], [21], [22], [23].
On the other hand, many studies have demonstrated that the sense of coherence increases with improvements in professional status [10], [11], [20], [21], [24], [25].
Sense of coherence and related concepts
Antonovsky developed a questionnaire with 29 items (SOC-29) for the measurement of the sense of coherence [5].There have hardly been any empirical studies on the validity of this SOC questionnaire [26].
Because of the overlap with other psychological variables, it has repeatedly been doubted whether the sense of coherence can be empirically demonstrated.
Antonovsky [3] postulated that there is a direct association between subjective physical health and sense of coherence. Empirical studies have yielded conflicting results: whereas some have found a direct association with subjectively evaluated physical health [18], [27], [28], [29], others have reported no direct [30], [31], [32] or unambiguous association [6], [10], [11], [25]. It has been demonstrated that high sense of coherence is associated with low anxiety and depression [12], [33], [34], [35], more optimism [9], [12], [30], [36], [37], more possibilities of positive coping [9], [12], [30], [36], [37] and less perceived stress [31], [38], [39], [40], [41].
There have been few studies on the significance of the sense of coherence in psychosomatics and psychotherapy [12]. It may be expected that a high sense of coherence would have a favourable effect on the course of psychotherapy. Moreover, a low SOC may be used as an indication for psychotherapeutic intervention.
The present study is intended as a contribution towards the investigation of the validity of the concept “Sense of Coherence“ in psychosomatic patients. In addition, associations were investigated between sense of coherence and sociodemographic variables.
We expect that:
There will be no association between sense of coherence and gender;
Younger patients will exhibit a lower sense of coherence than older patients;
Patients with the main diagnosis of “Depressive Syndrome” (“Depressive Episode” or “Recurrent Depressive Disorder”) will exhibit a lower sense of coherence than patients with anxiety disorders (“Phobic Disorders” or “Other Anxiety Disorder”), “Somatoform Disorders” or “Eating Disorders”.
On the basis of the results of previous studies [9], [12], [18], [27], [28], [29], [30], [31], [36], [37], [38], [39], [40], [41] and Lazarus’s transactional stress model, we expect that strong sense of coherence will be associated with:
Better subjective health and less perceived stress;
More active coping behaviour, more search for social support, more “focus on positive matters“ and less evasive coping behaviour;
More optimism and higher expectation of self-efficacy.
Patients and methods
Patients
The study was based on a population of 3932 patients treated as out-patients or in consultations in the Clinic for Psychosomatic Medicine at the Charité University of Medicine, Berlin, between July 2002 and October 2005, and who completed the questionnaire on sense of coherence for the first time during this period. At the time of enrollment, none of the patients was an in-patient for psychosomatic treatment.
Only those patients with the following ICD-10 diagnoses were enrolled in the study: Depressive Episode (F32), Recurrent Depressive Disorder (F33), Anxiety or Phobic Disorder (F40/41), Somatoform Disorder (F45) or Eating Disorders (F50). These diagnoses were made in the first clinical discussion by a doctor or psychologist. In addition, patients were excluded, if the complete test diagnosis was unavailable, because of language problems or if they were too old or refused to answer the questionnaire.
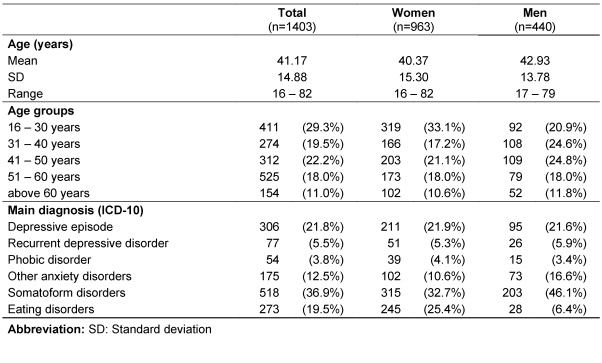
After considering these criteria, 1403 psychosomatic patients remained - 963 female (68.64%) and 440 male (31.36%). Table 1 includes additional information on the sample.
Table 1. Description of the sample.
Instruments
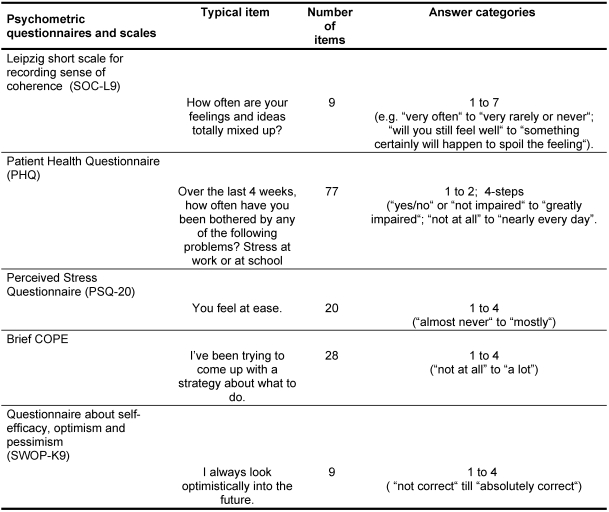
During the initial investigation - in the out-patient clinic or as a consultation - the patients completed the following psychometric questionnaires as part of their diagnosis (see Table 2). Consent for the evaluation of questionnaires for scientific purposes were generally obtained on entry to the clinic.
Table 2. Psychometric information on questionnaires and scales.
Leipzig Short Scale for Recording Sense of Coherence (SOC-L9)
The Leipzig Short Scale (SOC-L9) was used for recording the sense of coherence [18]. The SOC-L9 is a one dimensional measurement instrument. In contrast to the original 29-item version of Antonovsky [4], it consists of only 9 items, which cover the three subcomponents (comprehensibility, manageability and significance) of sense of coherence. The SOC-L9 is a reliable and valid measurement. It not only measures the content of the SOC-29 overall scale in a comparable manner, but is also economic [18].
Perceived Stress Questionnaire (PSQ-20)
The PSQ-20 records the subjective stress experienced and perceived. The 20 items in the short version may be summarised in the following four scales: worries, tension, joy and demands. The first three scales map the individual’s internal stress reactions. The scale “Demands“ records external stressors. The values of all PSQ items are also included in a total score. The reliability and validity of the PSQ-20 have been shown to be satisfactory [42].
Questionnaire on Self-Efficacy, Optimism and Pessimism (SWOP-K9)
Personal resources were recorded with the questionnaire “Self-Efficacy, Optimism and Pessimism“ (SWOP) [43]. The SWOP is composed of the questionnaire on general expectation of self-efficacy [44] and the Life Orientation Test (LOT) [45], which measures the outcome expectation. The 9 items in the SWOP-K9 may be summarised in 3 scales: self-efficacy, optimism and pessimism. The test quality criteria are satisfactory to good [43].
Patient Health Questionnaire (PHQ)
The Patient Health Questionnaire (PHQ) uses 77 items to record depressiveness, somatoform symptoms and psychosocial stress factors. The test quality criteria of the German version of the PHQ [46] are good to very good.
Brief COPE
Coping strategies were recorded with the German version of the Brief Cope [47]. This serves to measure the coping behaviour in past difficult or unpleasant situations. The 28 items may be summarised in 4 scales: search for support (emotional support, instrumental support, religion), focus on positive matters (humour, acceptance, positive re-evaluation), evasive coping behaviour (denial, self-accusation, experience of emotions) and active coping behaviour. The quality criteria are satisfactory [47].
Statistical Analyses
Statistical evaluation of the data was performed employing the Program SPSS, Version 11. Gender and age effects were analysed with the t-test for unpaired samples or with univariate analysis of variance.
For this purpose, age was split into categories. Associations between sense of coherence and other constructs (stress, coping strategies etc.) were tested by Pearson correlation analyses or partial correlations. Because of the large sample size, the selected level of significance was p<0.001.
Results
Gender and age effects
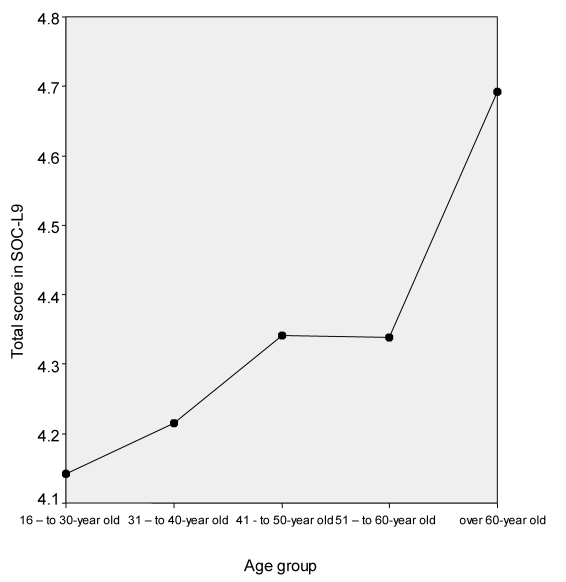
No differences between male and female psychosomatic patients with respect to sense of coherence (women: Mean=4.37, SD=1.07, Men: Mean=4.26, SD=1.12) were detected (see Figure 1).
Figure 1. Total score in the SOC-L9 for 16- to 30-year old, 31- to 40-year old, 41- to 50-year old, 51- to 60-year old and over 60-year old psychosomatic patients.
The patients were classified into the following age groups: 16-30 years (Mean=4.14, SD=1.08), 31-40 years (Mean=4.21, SD=1.08), 41-50 years (Mean=4.34, SD=1.13), 51-60 years (Mean=4.33, SD=1.08) and above 60 years (Mean=4.69, SD=1.11). Univariate analysis of variance found significant differences between the age groups (p<0.0001, η2=0.02).
Diagnosis groups
Univariate analysis of variance found significant differences between the diagnosis groups for the SOC total score (p<0.001; η2=0.07). The variable “Age” was controlled for in the analysis. Patients with depressive syndromes exhibited the lowest sense of coherence (recurrent depressive episodes Mean=3.71, SD=1.04; depressive episode Mean=3.93, SD=1.09). The highest values for sense of coherence were found in patients with somatoform disorders (Mean=4.62, SD=1.02) and for various (other) anxiety disorders (Mean=4.38, SD=1.09). The mean for patients with phobic disorder was 4.19 (SD=1.17) and for patients with eating disorders 4.23 (SD=1.09).
Construct validity
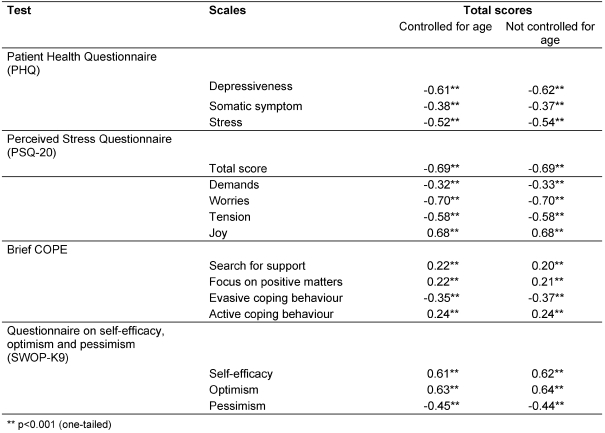
By controlling for the variable “age“,correlations were found between the SOC and other psychological constructs or questionnaires. High sense of coherence is associated with low depressiveness, high expectation of self-efficacy, more optimism, less pessimism and lower perceived stress (see Table 3).
Table 3. Correlation between SOC and subjective health, stress, coping and self-efficacy/optimism/pessimism.
The highest correlations were found between SOC and the scales “Worries“(r=-0.70) and “Joy” (r=0.68) in the PSQ-20. These scales record the patients’ feelings. Furthermore, we could detect high correlations between the SOC questionnaire and the scales “Self-Efficacy” (r=0.61) and “Optimism“(r=0.63) in the SWOP-K9, that record the general approach to life.
On the other hand, the correlation with external stressors, as recorded by the “Demands“ scale in the PSQ-20, was weaker (r=-0.32).
The weakest correlations were between the scales in the Brief COPE and the SOC total score (r=0.22 to 0.35).
Discussion
The objective of the present study was to investigate the association between sense of coherence and sociodemographic variables as well as ICD-10 diagnosis in a sample of psychosomatic patients. In addition, the work was intended to contribute towards the validation of the construct.
It turned out that the intensity of the sense of coherence was not associated with the gender of the psychosomatic patients. This is in accordance with the findings of Bengel et al. [6], who reported that sense of coherence was largely independent of gender in clinical studies.
It was also found that older patients reported higher values of sense of coherence than younger patients. In contrast to Gunzelmann et al. [48], we also found higher values of the sense of coherence in patients above 60 years as compared to younger patients. The significant differences in age-dependence of the sense of coherence may be due to the large size of our sample (n=1403).
The clinically defined ICD-10 diagnosis groups exhibited differences in the mean values of the sense of coherence. The lowest SOC values were exhibited by patients with a depressive episode or recurrent depressive disorders. There was also a very high correlation between the total SOC-L9 score and the PHQ scale depressiveness. Other studies have confirmed the conflation of sense of coherence with depression [23], [34]. Our studies support Geyer’s assumption that SOC is an inverse measure of depressiveness [35].
As in other studies, the present investigation found significant correlations between sense of coherence and subjectively evaluated physical health [30], [31], [49], [50], [51]. On the other hand, there are also numerous studies that could not establish a direct or an unambiguous correlation [6], [10], [11], [25], [30], [31], [32]. Because of the heterogeneity of the study results, the relationship between sense of coherence and physical health remains unclear. In our study, the correlation between the scale “Somatic Symptoms“ and the total SOC score was comparatively low (r=0.38). This may indicate that the specificity and areas of subjective evaluation of health could play an important role.
Patients with high sense of coherence reported more possibilities for more favourable coping, higher self-efficacy expectation, more optimism, less pessimism and less perceived stress. As in other studies, significant correlations were found between sense of coherence and other variables such as optimism, positive coping and less perceived stress [9], [12], [30], [36], [37], [38], [39], [40], [41]. Psychosocial resources seem to form the basis of SOC. The correlations support the concept of sense of coherence as formulated by Antonovsky, who postulated that there is a positive association between subjective physical health, possibilities of positive coping and optimism [3]. Our results support the validity of the SOC-L9 construct. However, the significance regarding the autonomy of SOC is limited as the high correlations obtained could also contain a reference to a general factor that may form the basis of SOC. Other studies have also reported high correlations and general factors of experience constructs [52], [53].
The correlations between all scales of the Brief SOC and the SOC total score were comparatively low (r=0.22 to 0.35). Antonovsky [54] suggested that it would be a mistake to regard the SOC as a coping strategy. Rather, high levels of SOC empowered individuals to decide between different coping strategies, thus activating specific resources which may be helpful in dealing with stressors [7].
The high correlations between sense of coherence and other psychological variables (subjective health, self-efficacy expectation, optimism, pessimism, perceived stress and coping) support the theoretical concept of sense of coherence, as formulated by Antonovsky. They also indicate that longitudinal studies should be performed to investigate exactly how and to what extent the SOC is predictive for well-being and quality of life.
Moreover, long-term studies on the stability of sense of coherence would be particularly desirable. How does the sense of coherence develop during a lifetime? How does a change in working life affect the sense of coherence? Is the degree of the sense of coherence a cause or a consequence of e.g. psychological or physical symptoms?
A longitudinal study investigating the effects of changes in social environment on the sense of coherence would be of particular significance, as Antonovsky [3] postulated that the social environment has a powerful influence on health maintenance.
In addition, longitudinal studies should be used to check the validity of the assumptions of the transactional stress model [1], in order to clarify associations between the sense of coherence and coping style or subjective well-being.
References
- 1.Lazarus RS. Psychological stress and the coping process. New York: McGraw; 1966. [Google Scholar]
- 2.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- 3.Antonovsky A. Health, stress, and coping: New perspectives on mental and physical well-being. San Fransisco: Jossey-Bass; 1979. [Google Scholar]
- 4.Antonovsky A. The sense of coherence: Development of a research instrument. Newsletter and Research Reports. 1983;1:1–11. [Google Scholar]
- 5.Antonovsky A. The structure properties of the sense of coherence scale. Soc Sci Med. 1993;36:725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 6.Bengel J, Strittmatter R, Willmann H. Was erhält den Menschen gesund? Antonovskys Modell der Salutogenese - Diskussionsstand und Stellenwert. Köln: Bundeszentrale für gesundheitliche Aufklärung (BZgA); 2001. (Forschung und Praxis der Gesundheitsförderung; 6). [Google Scholar]
- 7.Franke A, Broda M, editors. Psychosomatische Gesundheit. Versuch einer Abkehr vom Pathogenese-Konzept. Tübingen: dgvt; 1993. [Google Scholar]
- 8.Antonovsky A. Unraveling mystery of health. How people manage stress and stay well. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 9.Ghazinour M, Richter J, Eisemann M. Quality of life among Iranian refugees resettled in Sweden. J Immigr Health. 2004;6(2):71–81. doi: 10.1023/B:JOIH.0000019167.04252.58. [DOI] [PubMed] [Google Scholar]
- 10.Larsson G, Kallenberg KO. Sense of coherence, socioeconomic conditions and health. Eur J Public Health. 1996;6:175–180. [Google Scholar]
- 11.Poppius E, Tenkanen L, Kalimo R, Heinsalmi P. The sense of coherence, occupation and the risk of coronary heart disease in the Helsinki heart study. Soc Sci Med. 1999;49:109–120. doi: 10.1016/s0277-9536(99)00105-7. [DOI] [PubMed] [Google Scholar]
- 12.Sack M, Künsebeck H-W, Lamprecht F. Kohärenzgefühl und psychosomatischer Behandlungserfolg. Psychother Psychosom Med Psychol. 1997;47:149–155. [PubMed] [Google Scholar]
- 13.Broda M, Bürger W, Dinger-Broda A. Therapieerfolg und Kohärenzgefühl. Zusammenhänge zwei bis fünf Jahre nach stationär verhaltensmedizinischer Behandlung. In: Lutz R, Mark H, editors. Wie gesund sind Kranke? Göttingen: Hogrefe; 1995. pp. 113–122. [Google Scholar]
- 14.Bengtsson-Tops A, Brunt D, Rask M. The structure of Antonovsky's sense of coherence in patients with schizophrenia and its relationship to psychopathology. Scand J Caring Sci. 2005;19(3):280–287. doi: 10.1111/j.1471-6712.2005.00342.x. [DOI] [PubMed] [Google Scholar]
- 15.Raty LK, Larsson G, Soderfeldt BA, Larsson BM. Psychosocial aspects of health in adolescence: The influence of gender, and general self-concept. Adolesc Health Care. 2005;36(6):530. doi: 10.1016/j.jadohealth.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt-Ratjens C, Benz D, Van Damme D, Feldt K, Amelang M. Über zwiespältige Erfahrungen mit Fragbögen zum Kohärenzsinn sensu Antonovsky. Diagnostica. 1997;43(4):327–346. [Google Scholar]
- 17.Neuner B, Miller P, Maulhardt A, Weiss-Gerlach E, Neumann T, Brähler, Helmert, Haas, Müller J, Wernecke K, Spies Hazardous alcohol consumption and sense of coherence in emergency department patients with minor trauma. Drug Alcohol Depend. 2005;82(2):143–150. doi: 10.1016/j.drugalcdep.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Schumacher J, Wilz G, Gunzelmann T, Brähler E. The Antonovsky Sense of Coherence Scale: Test statistical evaluation of a representative population sample and construction of a brief scale. Psychother Psychosom Med Psychol. 2000;50(12):472–482. doi: 10.1055/s-2000-9207. [DOI] [PubMed] [Google Scholar]
- 19.von Bothmer MI, Fridlund B. Self-rated health among university students in relation to sense of coherence and other personality traits. Scand J Caring Sci. 2003;17:347–357. doi: 10.1046/j.0283-9318.2003.00234.x. [DOI] [PubMed] [Google Scholar]
- 20.Smith PM, Breslin FC, Beaton DE. Questioning the stability of sense of coherence: The impact of socio-economic status and working conditions in the Canadian population. Soc Psychiatry Psychiatr Epidemiol. 2003;38(9):475–484. doi: 10.1007/s00127-003-0654-z. [DOI] [PubMed] [Google Scholar]
- 21.Rimann M, Udris I. Kohärenzerleben (Sense of Coherence): Zentraler Bestandteil von Gesundheit oder Gesundheitsressource? In: Schüffel W, et al., editors. Handbuch der Salutogenese. Konzept und Praxis. 1998. pp. 351–373. [Google Scholar]
- 22.Karlsson I, Berglin E, Larsson PA. Sense of coherence: Quality of life before and after coronary artery bypass surgery - a longitudinal study. J Adv Nurs. 2000;31(6):1383–1392. doi: 10.1046/j.1365-2648.2000.01408.x. [DOI] [PubMed] [Google Scholar]
- 23.Frenz AW, Carey MP, Jorgensen RS. Psychometric evaluation of Antonovsky's sense of coherence scale. Psychol Assess. 1993;5:145–153. [Google Scholar]
- 24.Groholt E-K, Stigum H, Nordhagen R, Köhler L. Is parental sense of coherence associated with child health? Eur J Public Health. 2003;13(3):195–201. doi: 10.1093/eurpub/13.3.195. [DOI] [PubMed] [Google Scholar]
- 25.Lundberg O. Childhood conditions, sense of coherence, social class and adult ill health: Exploring their theoretical and empirical relations. Soc Sci Med. 1997;44(6):821–831. doi: 10.1016/s0277-9536(96)00184-0. [DOI] [PubMed] [Google Scholar]
- 26.Becker P. Die Salutogenesetheorie von Antonovsky: Eine wirklich neue, empirisch abgesicherte, zukunftsweisende Perspektive? In: Margraf J, Siegrist J, Neumer S, editors. Gesundheits- oder Krankheitstheorie? Saluto- versus pathogenetische Ansätze im Gesundheitswesen. Berlin: Springer; 1998. pp. 13–25. [Google Scholar]
- 27.Broda M, Dinger-Broda A, Bürger W. Selbstmanagement-Therapie und Gesundheitsressourcen - katamnestische Untersuchung zum Kohärenzgefühl bei verhaltensmedizinisch behandelten Patienten. In: Reinecker H, Schmelzer D, editors. Verhaltenstherapie, Selbstregulation, Selbstmanagement. Frederick H. Kanfer zum 70. Geburtstag. Göttingen: Hogrefe; 1996. pp. 257–248. [Google Scholar]
- 28.Geberth N, Broda M, Lauterbach W. Kohärenzgefühl und konstruktives Denken als Prädikatoren psychosomatischer Belastung. Praxis Klinische Verhaltensmedizin und Rehabilitation. 1997;10:70–75. [Google Scholar]
- 29.Stranzl G, Egger JW. Krankheitsverarbeitung und Wohlbefinden bei Nierentransplantierten und Dialysepatienten. Der Einfluss von dispositionellem und situationsspezifischem Coping auf das Wohlbefinden von Nierenkranken unter salutogenetischer Betrachtungsweise. Psychologie in der Medizin. 1997;8:17–24. [Google Scholar]
- 30.Becker P, Bös K, Woll A. Ein Anforderungs-Ressourcen-Modell der körperlichen Gesundheit: Pfandanalytische Überprüfungen mit latenten Variablen. Zeitschrift für Gesundheitspsychologie. 1994;2:25–48. [Google Scholar]
- 31.Buddeberg-Fischer B, Klaghofer R, Leuthold A, Buddeberg C. Unterrichtsklima und Symptombildung. Psychother Psychosom Med Psychol. 2000;50:222–229. doi: 10.1055/s-2000-13250. [DOI] [PubMed] [Google Scholar]
- 32.Hood SC, Beaudet MP, Catlin G. A healthy outlook. Health Rep. 1996;7:25–32. [PubMed] [Google Scholar]
- 33.Antonovsky H, Sagy S. The development of a sense of coherence and its impact on stress situations. J Soc Psychol. 1986;126(2):213–225. [PubMed] [Google Scholar]
- 34.Carmel S, Bernstein J. Trait anxiety, sense of coherence and medical school stressors: Observations at three stages. Anxiety Research. 1989;3:51–60. [Google Scholar]
- 35.Geyer S. Antonovsky's sense of coherence: Ein gut geprüftes und empirisch bestätigtes Konzept? In: Kolip P, Wydler H, Abel T, editors. Salutogenese und Kohärenzgefühl. Weinheim: 2000. pp. 209–221. [Google Scholar]
- 36.Chamberlain K, Petrie K, Azariah R. The role of optimism and sense of coherence in predicting recovery following surgery. Psychology and Health. 1992;7:301–310. [Google Scholar]
- 37.Fok SK, Chair SY, Lopez V. Sense of coherence, coping and quality of life following a critical illness. J Adv Nurs. 2003;49(2):173–181. doi: 10.1111/j.1365-2648.2004.03277.x. [DOI] [PubMed] [Google Scholar]
- 38.Hogh A, Mikkelsen EG. Is sense of coherence a mediator or moderator of relationships between violence at work and stress reactions? Scand J Psychol. 2005;46:429–437. doi: 10.1111/j.1467-9450.2005.00474.x. [DOI] [PubMed] [Google Scholar]
- 39.Richardson CG, Ratner PA. Sense of coherence as a moderator of the effects of stressful life events on health. J Epidemiol Community Health. 2005;59(11):979–984. doi: 10.1136/jech.2005.036756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flannery RB, Flannery GJ. Sense of coherence, life stress, and psychological distress: A prospective methodological inquiry. J Clin Psychol. 1990;46(4):415–420. doi: 10.1002/1097-4679(199007)46:4<415::aid-jclp2270460407>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 41.Black EK, White CA. Fear of recurrence, sense of coherence and posttraumatic stress disorder in haematological cancer survivors. Psycho-oncology. 2005;14(6):510–515. doi: 10.1002/pon.894. [DOI] [PubMed] [Google Scholar]
- 42.Fliege H, Rose M, Arck P, Levenstein S, Klapp BF. Validierung des "Perceived Stress Questionnaire" (PSQ) an einer deutschen Stichprobe. Diagnostica. 2001;47(3):142–152. [Google Scholar]
- 43.Scholler G, Fliege H, Klapp BF. Fragebogen zu Selbstwirksamkeit, Optimismus und Pessimismus. Psychother Psychosom Med Psychol. 1999;49:275–283. [PubMed] [Google Scholar]
- 44.Jerusalem M, Schwarzer R. Selbstwirksamkeit. In: Schwarzer R, editor. Skalen zur Befindlichkeit und Persönlichkeit. Institut für Psychologie, Freie Universität Berlin; 1986. pp. 15–28. [Google Scholar]
- 45.Scheier MF, Carver CS. Optimism, coping and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 46.Löwe B, Spitzerl L, Zipfel S, Herzog W. Gesundheitsfragebogen für Patienten. Testmappe mit Fragebögen, Manual, Schablonen, Kurzanleitung und Auswertungsbögen. 2. Auflage. Karlsruhe: Pfizer GmbH; 2002. [Google Scholar]
- 47.Knoll N. Stressbewältigung als Persönlichkeitsprozess: Ältere Menschen bewältigen eine Kataraktoperation. Fachbereich Erziehungswissenschaft und Psychologie, Freie Universität Berlin; 2002. [Google Scholar]
- 48.Gunzelmann T, Schumacher J, Brähler E. Das Kohärenzgefühl bei älteren Menschen: Zusammenhänge mit der subjektiven Gesundheit und körperlichen Beschwerden. Z Klin Psychol Psychiatr Psychother. 2000;48:145–165. [Google Scholar]
- 49.Straus F, Höfer R. Kohärenzgefühl, soziale Ressourcen und Gesundheit. In: Kolip P, Wydler H, Abel T, editors. Salutogenese und Kohärenzgefühl. Weinheim: 2000. pp. 115–128. [Google Scholar]
- 50.Strümpfer DJW. Sense of coherence, negative affectivity, and general health in farm supervisors. Psychol Rep. 1997;80:963–966. doi: 10.2466/pr0.1997.80.3.963. [DOI] [PubMed] [Google Scholar]
- 51.Schneider G, Driesch G, Kruse A, Wachter M, Nehen HG, Heuft G. What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence. Arch Gerontol Geriatr. 2004;39(3):227–237. doi: 10.1016/j.archger.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 52.Brown TA, Chorpita BFBDH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol. 1998;107(2):179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 53.Watson D, Clark AL. On traits and temperament: General and specific factors of emotional experience and their relation to the five-factor model. J Pers. 1991;60(2):441–476. doi: 10.1111/j.1467-6494.1992.tb00980.x. [DOI] [PubMed] [Google Scholar]
- 54.Antonovsky A. Salutogenese. Zur Entmystifizierung der Gesundheit. Tübingen: dgtv; 1997. [Google Scholar]