Abstract
Atherosclerosis is a complex pathologic process in which chemokine-mediated leukocyte accumulation in arterial walls is thought to be an important mechanism of pathogenesis. An interesting exception to this paradigm is the chemokine CXCL16, also known as the scavenger receptor for phosphatidylserine and oxidized low density lipoprotein (SR-PSOX), which is highly expressed in mouse and human atherosclerotic lesions, yet appears to be atheroprotective. Here we address potential mechanisms responsible for this activity. Consistent with its presence in atherosclerotic plaque, we found that atherogenic lipids upregulated CXCL16 in primary human monocyte-derived macrophages. However, the same lipids downregulated the CXCL16-targeted protease ADAM10, resulting in preferential expression of CXCL16 as the transmembrane form, not the shed form. Although transmembrane CXCL16 is known to mediate cell-cell adhesion by binding its receptor CXCR6, and atherogenic lipids are known to stimulate macrophage adhesion to coronary artery smooth muscle cells, we found that heterotypic adhesion of these cell types occurred in a CXCL16-independent manner. Instead we found that in macrophages CXCL16 promoted internalization of both oxidized low density lipoprotein and high density lipoprotein, as well as release of cholesterol. Moreover, CXCL16 deficiency in macrophages interfered with oxidized low density lipoprotein-induced upregulation of atheroprotective genes: adenosine triphosphate binding cassette transporter A1 and G1 as well as apolipoprotein E. Thus, our findings support the hypothesis that CXCL16 mediates atheroprotection through its scavenger role in macrophages and not by cell-cell adhesion.
Keywords: chemokines, monocytes/macrophages, inflammation
Introduction
Atherogenesis is thought to involve inflammatory responses to oxidized low density lipoproteins (oxLDL) and its free oxidized lipid constituents, which accumulate in the arterial intima (1). These responses include local release of chemoattractants that collaborate with cytokines, Toll-like receptors and adhesion molecules to promote infiltration of leukocytes into vascular sub-endothelium (2,3). Chemokines are a family of leukocyte chemoattractants that includes several well-characterized atherogenic factors (4–6). Family members are divided into four major subfamilies--C, CC, CXC, CX3C--based on the number and spacing of conserved cysteines. Most chemokines are secreted proteins that subserve many immunologic functions, most notably regulation of leukocyte trafficking to and activation at sites of infection and inflammation through interactions with cognate seven-transmembrane domain G protein-coupled receptors (7). In atherosclerosis, it is thought that chemokines coordinate communication of blood leukocytes with endothelium, thereby regulating leukocyte influx and accumulation in the vessel wall (4–6). In contrast to this paradigm, genetic evidence has suggested that the chemokine CXCL16 functions as an atheroprotective factor (8), through unknown mechanisms.
CXCL16 is atypical owing to the presence of a mucin-like stalk, and transmembrane and cytoplasmic domains not present in other CXC chemokines (9,10). It is expressed on the plasma membrane where it directly mediates adhesion to cells expressing its specific receptor CXCR6 (11). Upon cleavage of the mucin-like stalk, the chemokine domain is able to chemoattract CXCR6+ T, NK, NKT, B and dendritic cells (9,10,12,13). Cleavage is mediated by ADAM10, a member of the disintegrin and metalloproteinase domain (ADAM) family of enzymes (14,15). CXCL16 was first identified on the basis of its ability to scavenge phosphatidylserine and oxLDL (16), and thus was originally named SR-PSOX (17). Because CXCL16 functions as a chemokine, a scavenger receptor and an adhesion molecule, it may be involved in several phases of the immune response from antigen recognition to migration of immune cells into inflammatory foci, including atherosclerotic plaque.
CXCL16 is undetectable in normal aorta, but is expressed in mouse and human coronary and carotid atherosclerotic lesions, co-localizing with lipid-laden intimal macrophages (Mϕ) and smooth muscle cells (SMCs) (17,18). Studies evaluating soluble CXCL16 as a potential biomarker of coronary artery disease have been inconsistent (19,20). A polymorphic variant of CXCL16 named CXCL16-A181V has been reported to be associated with increased coronary artery stenosis in post-infarction patients (21), suggesting that wild type CXCL16 may be atheroprotective. Consistent with this, genetic inactivation of cxcl16 in hyperlipidemic low density lipoprotein receptor knockout mice (ldlr−/−) results in accelerated atherosclerosis due to enhanced Mϕ recruitment to the aortic arch (8). Although the CXCL16-CXCR6 relationship is considered monogamous, cxcr6 inactivation in atherosclerosis-prone apolipoprotein E (ApoE) knockout mice (apoE−/−) decreased susceptibility to atherosclerosis, and was accompanied by reduced homing of lymphocytes into the aorta. These data suggest that cxcr6 is a pro-atherogenic chemokine receptor (22).
To investigate how CXCL16 may oppose atherosclerosis, we tested how lipid components of the atheromatous microenvironment affect CXCL16 expression and function on primary monocyte-derived Mϕ. We focused on oxLDL and its lipid derivatives--including 9-hydroxy-10E,12Z-octa decadienoic acid ester (9-HODE) and 13-hydroxy-9Z,11E-octadecadienoic acid ester (13-HODE), the two major bioactive oxidized linoleic acid metabolite components of LDL (23,24), and arachidonic acid-containing phospholipids 1-palmitoyl-2-glutaroyl-sn-glycero-3-phosphocholine (PGPC) and 1-palmitoyl-2-(5-oxo valeroyl)-sn-glycero-3-phosphocholine (POV-PC) (25), all of which are present in high amounts in human atherosclerotic lesions (23–25).
Materials and Methods
Materials
LDL, oxLDL, HDL, acetyl LDL (acLDL), 1,1'-dioctadecyl-3,3,3',3'-tetramethylin docarbocyaninet (Dil)-oxLDL and Dil-HDL were purchased from Intracel (Frederick, MD). 9-HODE, 13-HODE, PGPC and POV-PC were from Cayman Europe (Tallinn, Estonia). Monoclonal antibodies (mAbs) included: rat anti-human CX3CR1 (Caltag-MedSystems Ltd, Buckingham, UK), rat anti-human CXCL16 (R&D Systems Europe Ltd, Abingdon, UK), mouse anti-human CD14, CD36, CD68 (BD Biosciences, Oxford, UK) and SR-A (CosmoBio, Tokyo, Japan). Isotype-matched control Abs used for flow cytometry and scavenger receptor blocking studies were from BD Biosciences. Real-time PCR reagents, including validated 6-carboxyfluorescein-tagged human ApoE, ABCA1, ABCG1 and GAPDH probes were from Applied Biosystems (Austin, TX). Primary human coronary artery smooth muscle cells (CASMCs) and SmGM-2 medium were from Lonza (Slough, UK). RPMI 1640 and Vybrant cell adhesion assay kit were from Invitrogen Ltd (Paisley, UK).
Cell Culture
Mo were isolated from peripheral blood of healthy donors using NycoPrep 1.068 according to the manufacturer’s instructions (Axis-Shield, Kimbolton, UK) and resuspended in RPMI 1640 medium supplemented with 20 vol % of autologous serum. Blood was collected in accordance with protocols # 07/Q0404/42 and # 09-04 approved by the institutional review board. CD14+ cells represented 84±4% of the prep. Cells were plated at a density of 2.5 × 106/well in a 6-well dish, incubated at 37°C for 1 h, then stimulated with LDL (50 µg/ml), oxLDL (50 µg/ml), or oxidized arachidonic acid-or oxidized linoleic acid-containing lipids (10 µg/ml) for 6, 12 or 24 h. CASMCs were cultured and stimulated as reported previously (26).
Characterization of a Model of Foamy Macrophage in vitro
To study potential mechanisms by which human CXCL16 may regulate atheroprotection at the cellular and molecular levels, we first used atherogenic lipids to establish a foamy macrophage model in vitro from cultured human peripheral blood monocytes. Mo were cultured in the presence of atherogenic or control lipids (LDL (50 µg/ml), oxLDL (50 µg/ml), or oxidized arachidonic acid- or oxidized linoleic acid-containing lipids (10 µg/ml)), and assayed 6, 12 and 24 h after lipid addition for the following parameters: 1.) intracellular lipid accumulation measured by staining with Oil Red O; 2.) expression of macrophage-specific surface marker CD68 and scavenger receptors, including expression of CD36 and SR-A; and 3.) adhesion, as described previously (26,27). Incubation of Mo with 50 µg/ml of oxLDL or 10 µg/ml of 9-HODE and 13-HODE resulted in time-dependent upregulation of CD68, CD36 and SR-A, as well as in markedly increased Oil Red O staining, which are all properties of foam cells in atherosclerotic plaques. Since maximal induction of these foamy macrophage characteristics occurred when Mo were treated for 24 h with atherogenic lipids, we used cells treated for this duration for all experiments shown and refer to them in the manuscript as Mϕ. For all functional assays we have used either Mo or Mϕ. We have not included in our functional assays cells cultured in the presence of atherogenic lipids for 6 or 12 h as these cells are immunophenotyically no longer monocytes, but do not display a foam cell-like immunophenotype.
Analysis of Cellular Lipid Accumulation
Cells were fixed in Cytofix buffer (BD Biosciences, San Jose, CA) for 30 min at room temperature, washed twice with PBS and stained with 0.5% Oil Red O (Sigma-Aldrich, St. Louis, MO). Quantification of lipid accumulation was performed by extracting Oil Red O from stained cells with isopropanol and measuring absorbance of cell extracts at 510 nm. Results were normalized to total cell protein concentration.
Flow Cytometry
Cells (106) were fixed (Cytofix buffer, BD Biosciences) and then stained with mAbs at 4°C for 30 min in labeling buffer (Hanks’ balanced salt solution with 0.1% BSA and 0.1% sodium azide) containing anti-Fc reagent (Miltenyi Biotech, Bisley, UK). Flow cytometry was performed in duplicate using a FacsCalibur and then analyzed with CellQuest (Becton-Dickinson, San Jose, CA), correcting for nonspecific staining with isotype Ab controls.
mRNA Quantification
RNA was extracted by RNeasy kit (Qiagen, Valencia, CA) and reverse transcribed with RETROscript (Applied Biosystems/Ambion, Austin, TX). cDNA was serially diluted and amplified in triplicate for standard curves for each primer/probe set. Relative target quantification was calculated with the 2−ΔΔCT method (28) and normalized to GAPDH.
CXCL16 Knockdown
Seven CXCL16-specific sRNAi were designed using BLOCK-iT RNAi Designer Program from Invitrogen and sRNAi with a sequence 5'-CCGGAAACA CCTGAGAGCTTACCAT-3', which silenced CXCL16 expression by ≥ 80%, was used for all knockdown experiments. The negative control sRNAi had medium GC content (-Cmed) that matched CXCL16-specific sRNAi GC composition. Fluorescein-labeled dsRNA oligomer (F), used to estimate transfection efficiency, had the same length as CXCL16-specific sRNAi. Mo (5×106) were nucleofected (Amaxa, Cologne, Germany) with 50, 150 or 300 nM of fluorescein-labeled dsRNA, negative control or CXCL16-specific sRNAi, resuspended in 2 ml of prewarmed RPMI 1640 supplemented with 20 vol % of autologous serum, and then cultured with or without lipids for 24 h.
Soluble CXCL16 and ApoE quantitation using ELISA
Soluble CXCL16 in the supernatants of unstimulated or stimulated Mo was measured using the Quantikine colorimetric ELISA (R&D Europe) as recommended by the manufacturer. Soluble ApoE in the supernatants of sRNAi-transfected or untransfected Mo was measured using ApoE4/Pan-ApoE ELISA kit from MBL Co. (Woburn, MA).
Adhesion Assay
Mo (5×106/ml), either untransfected or transfected with negative control or CXCL16-specific sRNAi, were cultured with or without lipids for 24 h. Some untransfected cells were incubated for 45 min prior to the adhesion assay with anti-CX3CR1 or anti-CXCL16 mAbs or isotype controls. Cells were washed with prewarmed RPMI 1640, loaded for 30 min with 5 µM calcein AM at 37°C, resuspended at 0.5×106/100 µl and incubated at 37°C for 60 min with primary human CASMCs cultured with oxLDL for 24 h. Nonadherent cells were removed by washing, and end-point fluorescence (in units per millilitre (U/ml)) was measured with a fluorescein filter set (absorbance 494 nm; emission 517 nm) using the multifunctional microplate reader FLUOstar Galaxy (BMG Labtech Ltd, Aylesbury, UK).
Cholesterol Efflux Assay
Mo (5×106) were incubated with or without 50 µg/ml oxLDL for 24 h, lipid-loaded and labeled for 24 h in the presence of 50 µg/ml acLDL and 2 µCi/ml [1α,2α(n)-3H]-Cholesterol (PerkinElmer, Waltham, MA) in 1 ml of 0.2% BSA in RPMI 1640 and then equilibrated for 4 h in 0.2% BSA-RPMI 1640. After the labelling and equilibration procedures, cells were washed twice with PBS (pH=7.4), incubated for 6, 12 or 24 h at 37°C in 1 ml of 0.2% BSA-RPMI 1640 containing 50 µg/ml human high density lipoprotein (HDL) (density 1.063-1.21 g/ml) or 50 µg/ml purified human apolipoprotein A1 (ApoA-1) (BioVision, Mountain View, CA) as cholesterol-poor acceptors. At different time points, 100 µl of medium were harvested, and after precipitation at 6000 × g for 10 min to remove cell debris, radioactivity in the supernatant was measured by liquid scintillation counting. The cells were lysed in 0.5 ml of 0.1 M NaOH and 0.1% SDS, and cell-associated radioactivity was determined. Cholesterol efflux was expressed as % of radioactivity released from cells into the medium relative to the total radioactivity in cells plus medium.
Dil-oxLDL/Dil-HDL Internalization
Mo (2.5×106) were differentiated into Mϕ in the presence of oxLDL (50 µg/ml) for 24 h. For the Dil-oxLDL internalization assay, cells were pre-treated with isotype control or mAbs recognizing CD36, SR-A, CXCL16 or CD68, then incubated for 2 h at 37°C with 5 µg/ml of Dil-oxLDL. For the Dil-HDL internalization assay, cells were pre-treated with isotype control rat IgG2a or anti-CXCL16 mAb then incubated for 2 h at 37°C with 5 µg/ml of Dil-HDL. The efficiency of Dil-HDL uptake in cells was also measured in the presence of a 40-fold excess of unlabeled LDL, HDL or oxLDL. After incubation, Dil-oxLDL or Dil-HDL accumulation in cells was determined by isopropanol extraction of Dil, and fluorescence was measured at absorbance 520 nm and emission 564 nm. Results were normalized to total cell protein concentration. Dil-HDL uptake was also measured as described above in Mo that were either untransfected or transfected with the negative control or CXCL16-specific sRNAi.
Statistical Analysis
All conditions were performed in duplicate or triplicate, and each experiment was performed using cells from 3 to 8 different Mo or CASMC donors. Values for each condition were averaged, and data are presented as mean ± SEM. The statistical significance of differences among matched groups was tested by the nonparametric Friedman 2-way ANOVA by ranks, followed by Dunn’s post-test, using the GraphPad Prism 3.0 program (GraphPad Software). Values of P <0.05 were considered statistically significant.
Results
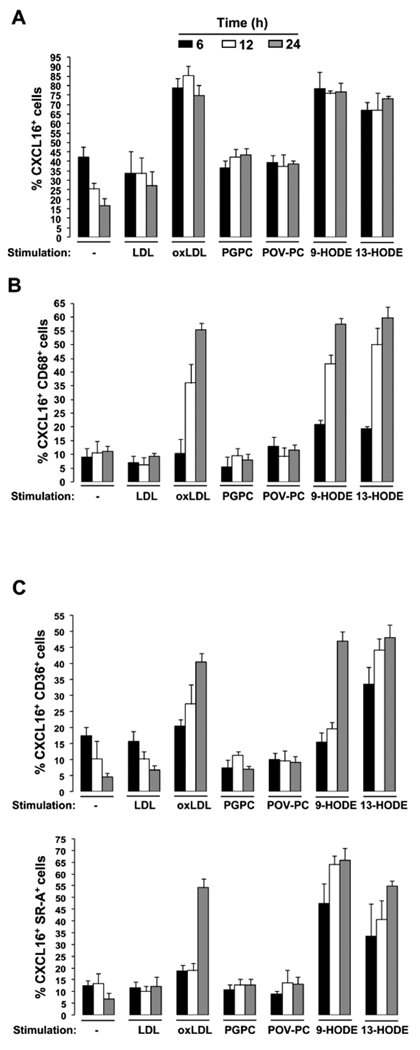
To determine how CXCL16 may protect against atherosclerosis, we first investigated how atherogenic lipids regulate CXCL16 expression on Mϕ, the main CXCL16+ cell type in atherosclerotic lesions (17,18). Although standard in vitro Mo-to-Mϕ differentiation protocols employ extended culturing of Mo in various growth factors including GM-CSF and M-CSF, we utilized and optimized previously described protocols that support rapid differentiation of Mo to Mϕ as determined by the immunophenotype of cultured cells (29–33). As expected, freshly isolated human peripheral blood Mo were ~85% CD14+, but expressed very low levels of the classical macrophage scavenger receptors CD68, SR-A and CD36 (data not shown). Consistent with this, the cells stained very poorly with lipid-specific Oil Red O (Suppl. Fig 1). In contrast, freshly isolated Mo expressed high levels of CXCL16, a non-classical scavenger receptor for oxLDL and a chemokine (~43%, data not shown). CXCL16 expression on Mo remained constant for 6 hours ex vivo (Fig. 1A and Suppl. Fig. 2A), but declined thereafter in the absence of atherogenic lipid stimulation to 25% and 18% by 12 and 24 hours, respectively. Compared with these benchmarks, stimulation of cells with the atherogenic lipids oxLDL, 9-HODE or 13-HODE for 6, 12 or 24 hours, markedly increased CXCL16+ cell frequency (Fig. 1A and Suppl. Figs. 2C, F and G), which strongly correlated with induction of the macrophage differentiation marker CD68 (Fig. 1B). CXCL16 expression was also associated with expression of two scavenger receptor subtypes crucial for foam cell formation: CD36 (Fig. 1C, top panel and Suppl. Figs. 2C, F and G) and SR-A (Fig. 1C, bottom panel and Suppl. Figs. 2C, F and G), as well as with a significant increase in Oil Red O uptake (Suppl. Fig. 1). The effect was atherogenic lipid-specific, since unmodified LDL, PGPC or POV-PC had no significant effect on CXCL16 expression (Fig. 1A and Suppl. Figs. 2B, D and E).
FIGURE 1. OxLDL and oxidized linoleic acid components of LDL specifically promote CXCL16 up-regulation on human blood monocyte-derived Mϕ.
Mo were isolated, cultured and stimulated as described in Materials and Methods. A–C, Summary data of the percent of total cells with the indicated immunophenotype as a function of cell stimulus and incubation time. Donors were the same in A through C. Data are from 4 independent experiments using 8 different donors and are presented as the mean ± SEM.
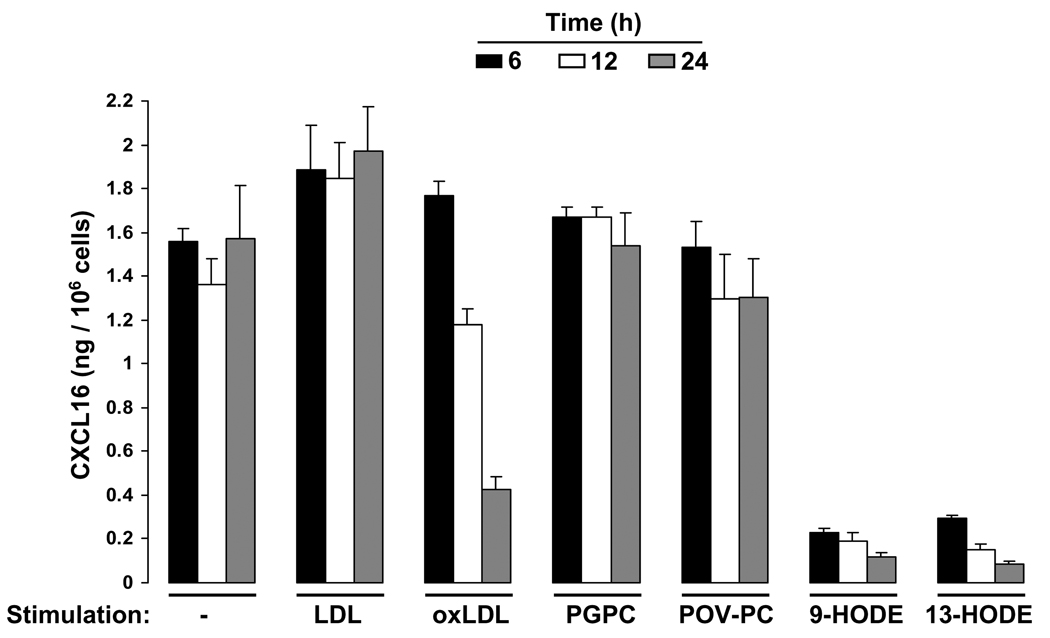
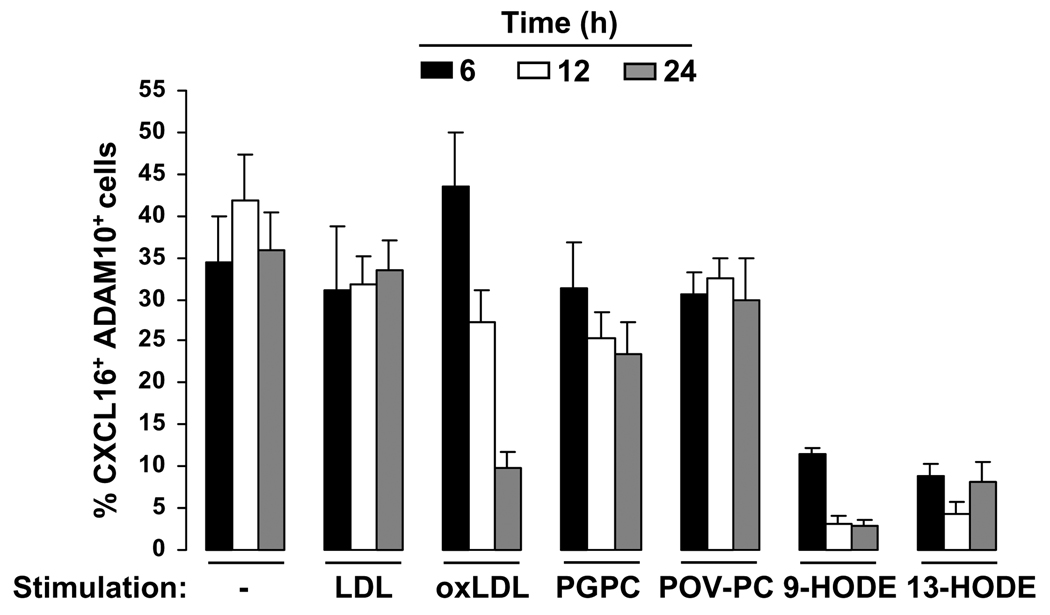
CXCL16 is a multimodular chemokine, which may be either membrane-anchored or soluble (9,10); therefore, we tested whether atherogenic lipids that specifically upregulated membrane-bound CXCL16 (Fig. 1) may also regulate release of the CXCL16 chemokine domain. Stimulation of Mo with LDL or arachidonic acid derivatives for 6, 12 or 24 hours promoted release of CXCL16. In contrast, oxLDL, 9-HODE or 13-HODE promoted a rapid and time-dependent decrease of shed CXCL16 compared to the amount of soluble CXCL16 detected in the supernatant of unstimulated cells (Fig. 2). Atherogenic lipid-dependent blockage of CXCL16 shedding coincided with a rapid and time-dependent decrease of ADAM10 surface expression on CXCL16+ Mϕ (Fig. 3 and Suppl. Fig. 3). Thus, atherogenic lipid-induced upregulation of CXCL16 on human Mϕ favors transmembrane localization over release due to concomitant downregulation of the CXCL16-specific protease ADAM10.
FIGURE 2. Oxidized lipids inhibit release of the CXCL16 chemokine domain from monocytes.
Mo were cultured with or without the stimuli listed on the x-axis (concentrations as in Figure 1). Cell culture supernatants were collected at indicated time points and analyzed for the presence of CXCL16 by enzyme-linked immunosorbent assay (ELISA). Data represent the mean ± SEM from 3 independent experiments using 3 different donors with each condition tested in triplicate.
FIGURE 3. Atherogenic lipids downregulate ADAM10 surface expression on CXCL16+ cells.
Mo were cultured with or without the indicated stimuli. Summary data are shown for the percent of CXCL16+ADAM10+ cells as a function of cell stimulus. Data are from 3 independent experiments using 3 different donors and are presented as the mean ± SEM.
Since CXCR6 and CXCL16 mediate cell-cell adhesion (11), we next tested whether they mediate adhesion of Mϕ to CASMCs, the two cell types known to be in close proximity in atherosclerotic lesions (34). Neither CXCR6 nor CXCL16 have been detected in healthy coronary arteries (17,18). However, we observed low constitutive expression of CXCR6 on the surface of CASMCs cultured in vitro and this increased 4.6 fold if CASMCs were stimulated for 24 hours with oxLDL or atherogenic lipids (Suppl. Fig. 4).
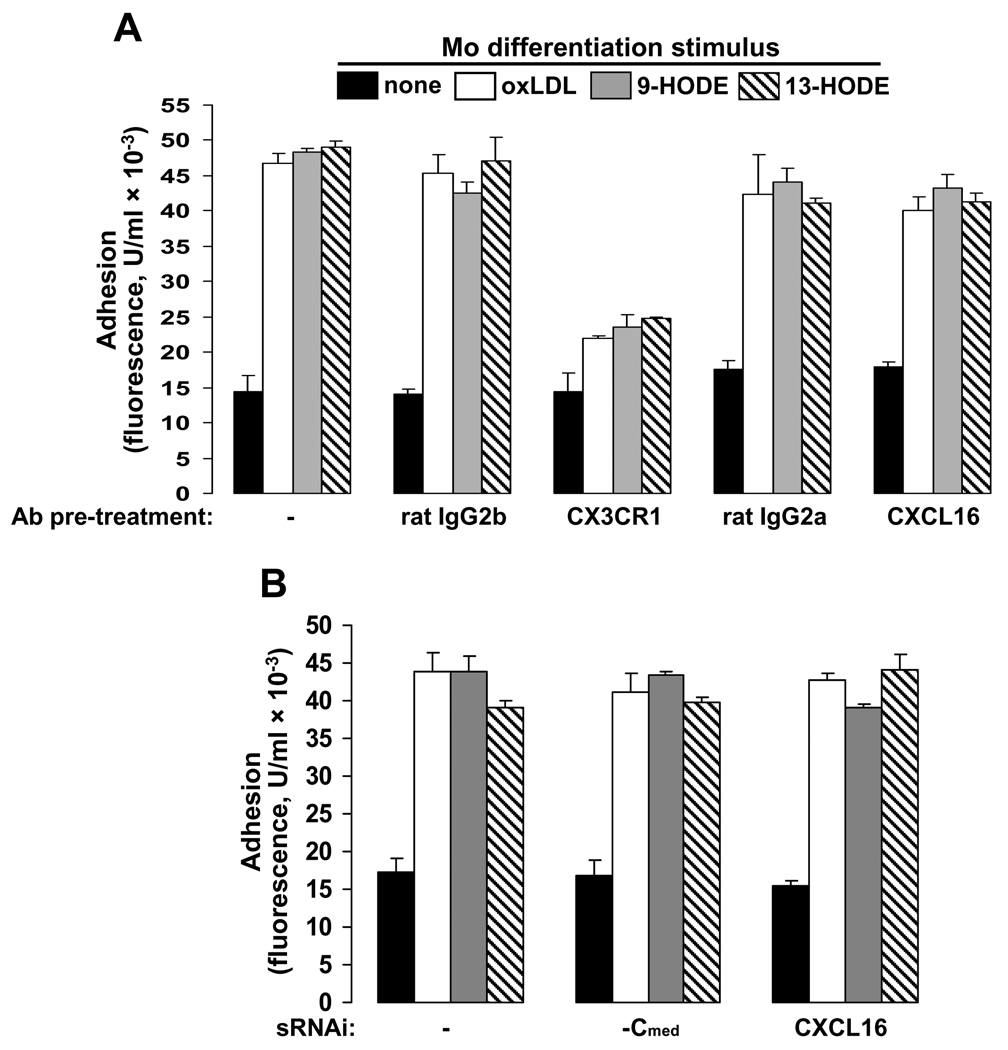
As we have shown previously (26,27), when both Mo and CASMCs were stimulated with oxLDL or oxidized linoleic acid-containing lipids before assay, heterotypic adhesion increased dramatically (Fig. 4). Preincubation of Mϕ with anti-CX3CR1 mAb specifically reduced adhesion (Fig. 4A), indicating as previously shown (26,27) that Mϕ -SMC interaction is in part dependent upon CX3CL1-CX3CR1 interaction. Surprisingly, neither pretreatment of Mϕ with CXCL16-directed mAb (Fig. 4A) nor silencing endogenous CXCL16 with specific sRNAi (Suppl. Fig. 5) affected adhesion of Mϕto CASMCs (Fig. 4B).
FIGURE 4. CXCL16-CXCR6 axis does not promote adhesion of Mϕ to coronary artery smooth muscle cells (CASMCs).
Static adhesion of Mϕ to CASMCs, which were cultured with 25 µg/ml oxLDL for 24 h. The adhesion assay was performed as described in Materials and Methods. A, Prior to the adhesion assay, Mo or Mϕ were blocked for 45 min at 37°C with the following agents: 5 µg/ml isotype control rat IgG2b or CX3CR1 mAb or 4 µg/ml rat IgG2a or CXCL16 mAb. B, Mo were nucleofected with 150 nM of the indicated CXCL16-specific (CXCL16) or negative control (-Cmed) sRNAi and then cultured for 24 h in the presence or absence of atherogenic lipids. Data in A are from 3 independent experiments using Mo from 3 different donors with each condition tested in duplicate. Results in B are from 4 independent experiments using 4 different donors, each condition tested in triplicate. Data are expressed as the mean ± SEM.
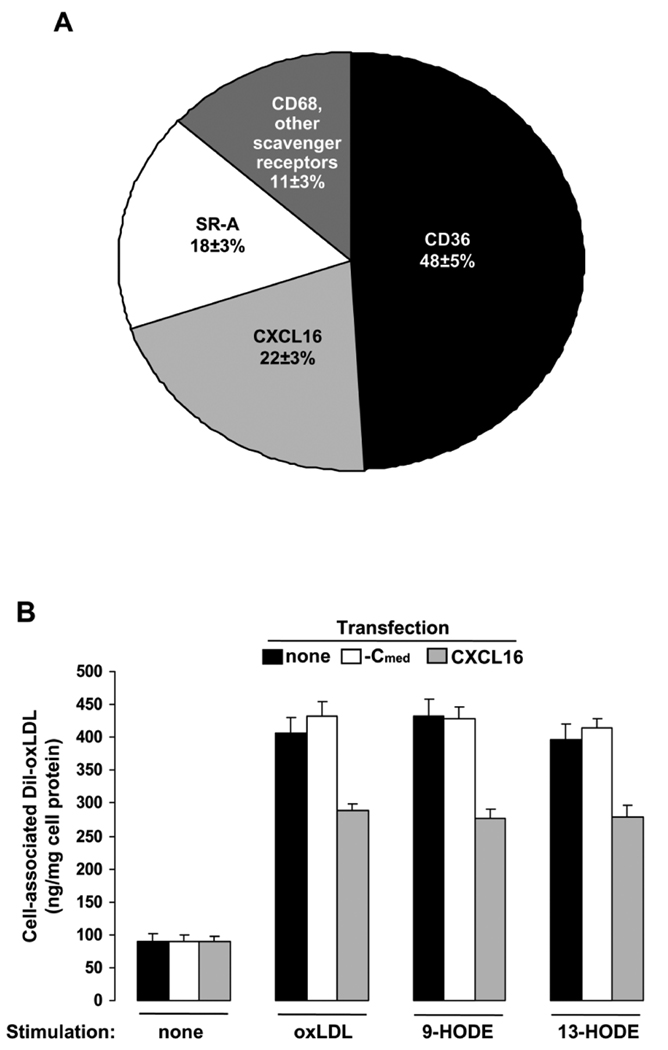
CXCL16 is the only known chemokine that functions as a scavenger receptor for phosphatidylserine and oxLDL (16–18,35). In this regard, Mϕ from cxcl16−/− mice internalize significantly less oxLDL (~34%) than wild-type controls (8), suggesting that CXCL16 may mediate a significant portion of oxLDL uptake in vivo. These results are supported by our study in which we measured the contribution of known scavenger receptors towards oxLDL uptake in human Mϕ. Blockage of CD36 resulted in the greatest decrease (~50%) in Dil-oxLDL internalization (Fig. 5A), which confirms that CD36 is the main scavenger receptor for oxLDL on foam cell Mϕ (36). Although SR-A is the major scavenger receptor for acLDL (37), this receptor also internalizes oxLDL (36). We were able to confirm this because blockage of SR-A decreased Dil-oxLDL internalization by ~20% (Fig. 5A). While the contribution of CD68 towards Dil-oxLDL internalization was minor, blockage of CXCL16 resulted in a strong decrease of Dil-oxLDL scavenging (Fig. 5A). Furthermore, silencing of endogenous CXCL16 in Mϕ decreased the amount of cell associated Dil-oxLDL by ~25% (Fig. 5B), confirming our data shown in Fig. 5A. These results imply that CXCL16 is the second major scavenger receptor for oxLDL on human Mϕ ex vivo.
FIGURE 5. CXCL16 promotes oxLDL internalization in Mϕ.
Uptake of Dil-oxLDL was performed as detailed in Materials and Methods. Cell-associated fluorescence was expressed as nanograms of Dil-oxLDL per milligram of total cellular protein. A, Prior to Dil-oxLDL internalization assay, Mϕ were incubated for 45 min at 37°C with 4 µg/ml of isotype control or mAbs recognizing CD36, SR-A, CXCL16 or CD68. B, Mo were nucleofected with 150 nM of the indicated CXCL16-specific (CXCL16) or negative control (-Cmed) sRNAi and then cultured for 24 h with or without 50 µg/ml oxLDL, 10 µg/ml 9-HODE or 10 µg/ml 13-HODE. Values shown are the mean (±SEM) of n=4 donors for each condition.
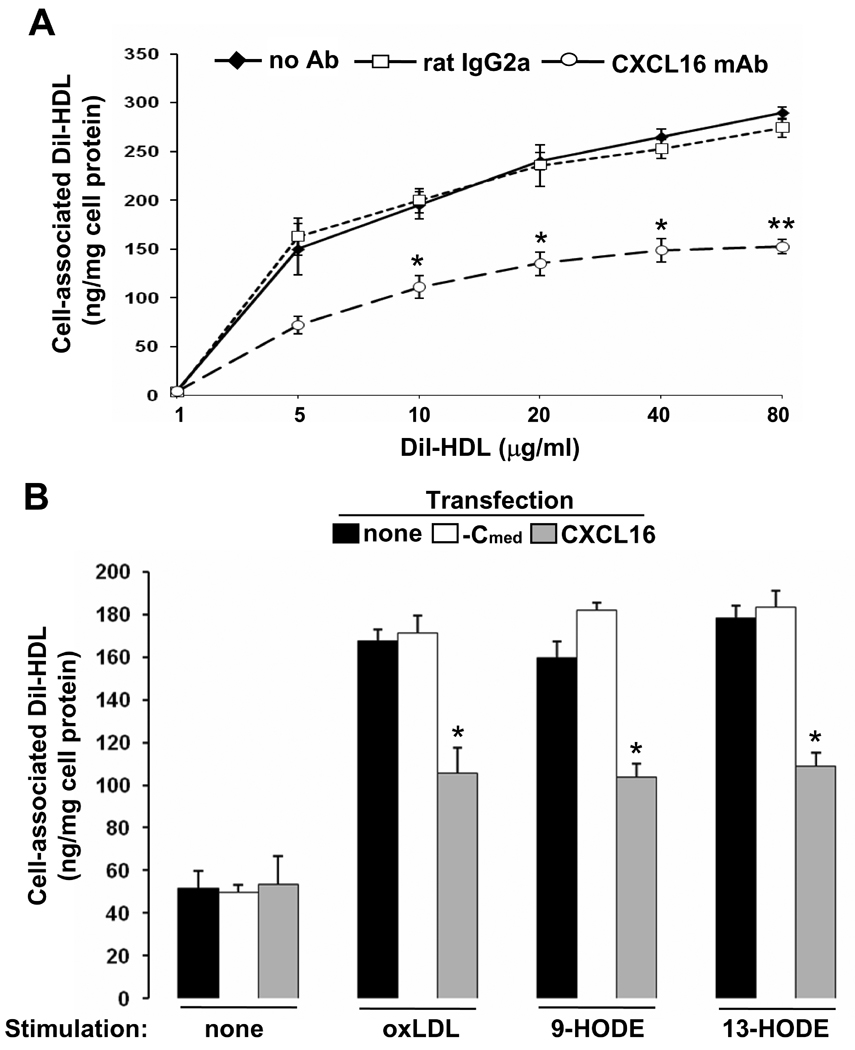
Exacerbation of atherosclerosis in ldlr−/− mice by inactivation of cxcl16 was unexpected and suggested that CXCL16 is atheroprotective, even though cxcl16−/−– Mϕ exhibited marked reductions in uptake of oxidized lipids in vitro (8). This prompted us to analyze CXCL16 scavenger functions further; thus, we examined whether CXCL16 may promote uptake of HDL in Mϕ. Internalization of Dil-HDL in Mϕ was dose-dependent (Fig. 6A). Neutralization of CXCL16’s scavenger function resulted in reduced Dil-HDL uptake in Mϕ (Fig. 6A). Furthermore, CXCL16-silenced Mϕ internalized significantly less Dil-HDL compared to untransfected or negative control CXCL16 sRNAi-transfected cells (Fig. 6B). We confirmed a role for CXCL16 in HDL uptake by incubating cells in excess amounts of unlabeled LDL, HDL or oxLDL. Internalization of Dil-HDL by Mϕ was greatly reduced in the presence of unlabeled HDL or oxLDL but not LDL (Suppl. Fig. 6A), indicating that HDL and oxLDL may be internalized through the same set of macrophage scavenger receptors. This pattern of Dil-HDL uptake remained unchanged if Mϕ were treated with isotype control rat IgG2a Ab prior to the assay; however, Dil-HDL internalization in Mϕ decreased by 36% if cells were pretreated with anti-CXCL16 mAb (Suppl. Fig. 6B). While our data do not identify CXCL16 as a physiologic HDL receptor, they demonstrate that CXCL16 expression is important in the process of HDL internalization in Mϕ.
FIGURE 6. CXCL16 promotes HDL uptake in Mϕ.
Uptake of Dil-HDL was performed as described in Materials and Methods. Cell-associated fluorescence was expressed as nanograms of Dil-HDL per milligram of total cellular protein. A, Mϕ, which were differentiated in presence of 50 µg/ml oxLDL for 24 h, were incubated with 4 µg/ml rat IgG2a or CXCL16 mAb before Dil-HDL internalization assay. B, Mo were nucleofected with 150 nM of CXCL16-specific (CXCL16) or negative control (-Cmed) sRNAi and then cultured for 24 h with or without 50 µg/ml oxLDL, 10 µg/ml 9-HODE or 10 µg/ml 13-HODE. Data represent the mean ± SEM from 4 donors. *p < 0.05 and **p < 0.01 vs the corresponding unblocked control value in A.
*p < 0.05 for the indicated values vs the corresponding lipid-stimulated negative control sRNAi (-Cmed) value in B.
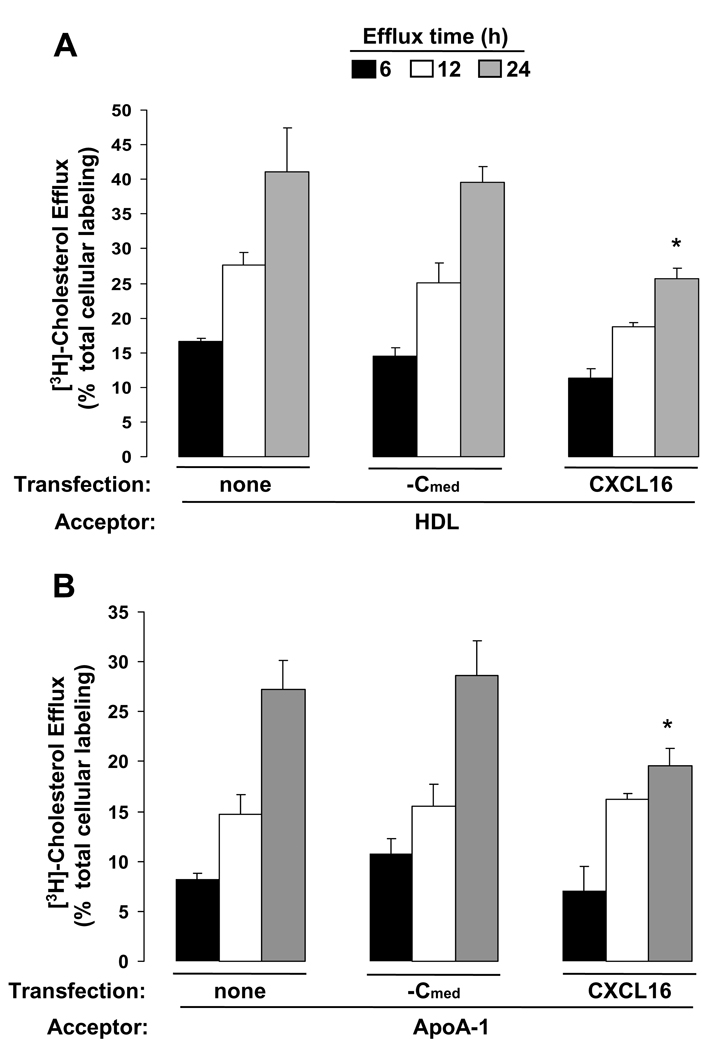
Through a process known as reverse cholesterol transport (RCT), excess cholesterol may be released from extrahepatic lipid-loaded cells, such as foam cells in the arterial wall, to lipid-poor acceptors such as HDL and Apo-A1, and this in turn promotes formation of mature HDL-cholesterol particles which transport the excess cholesterol to the liver and intestine for excretion. By reducing accumulation of cholesterol in the arterial wall, cholesterol efflux and RCT may interfere with atherogenesis (38). Because genetic evidence suggests that CXCL16 is atheroprotective (8,21), we investigated CXCL16’s role in macrophage cholesterol efflux. 3H-cholesterol egress to lipid-poor acceptors was time dependent (Fig. 7). Transfection with CXCL16-specific sRNAi specifically knocked-down expression of CXCL16 and significantly decreased the rate of 3H-cholesterol efflux to HDL (Fig. 7A) and Apo-A1 (Fig. 7B) 24 hours after addition of lipid-poor acceptors.
FIGURE 7. CXCL16 expression increases 3H-Cholesterol release from Mϕ.
Mo were nucleofected with 150 nM of CXCL16-specific (CXCL16) or negative control (-Cmed) sRNAi and then cultured for 24 h with 50 µg/ml acLDL in the presence of radioactive cholesterol. Cells were equilibrated, washed and efflux was stimulated by incubating Mϕ in media containing lipid-poor acceptors for 6, 12 or 24 h. A, Macrophage 3H-Cholesterol efflux to human HDL. B, The release of 3H-Cholesterol to purified human ApoA-1. Results represent the mean ± SEM and are from 3 independent experiments using 3 different donors with each condition tested in triplicate. *p < 0.05, comparing the indicated value to the corresponding negative control sRNAi (-Cmed) value for the same time point.
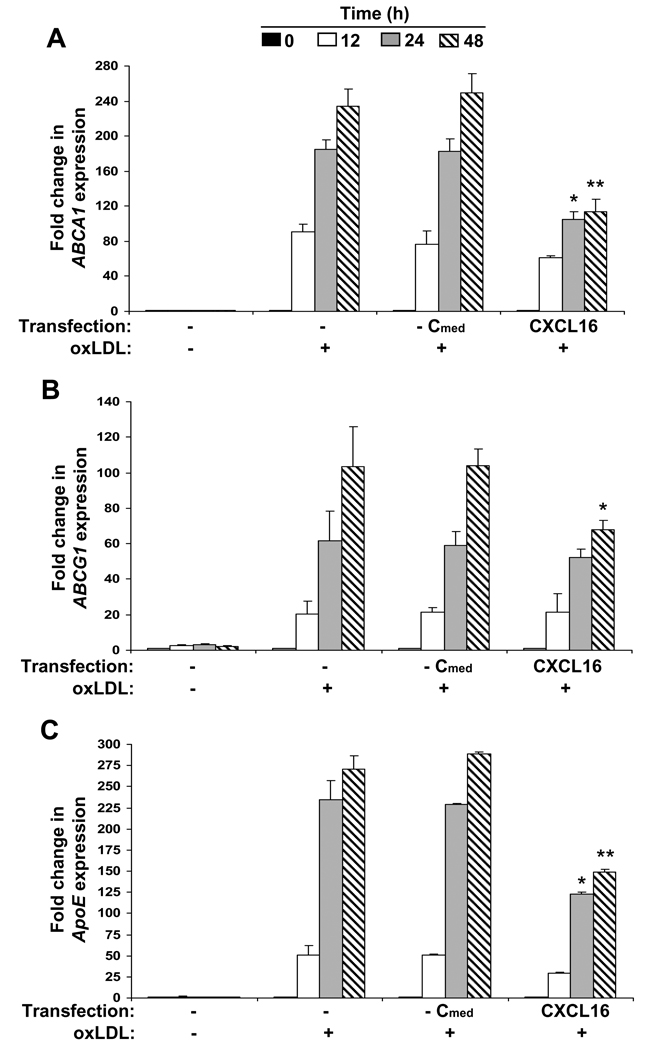
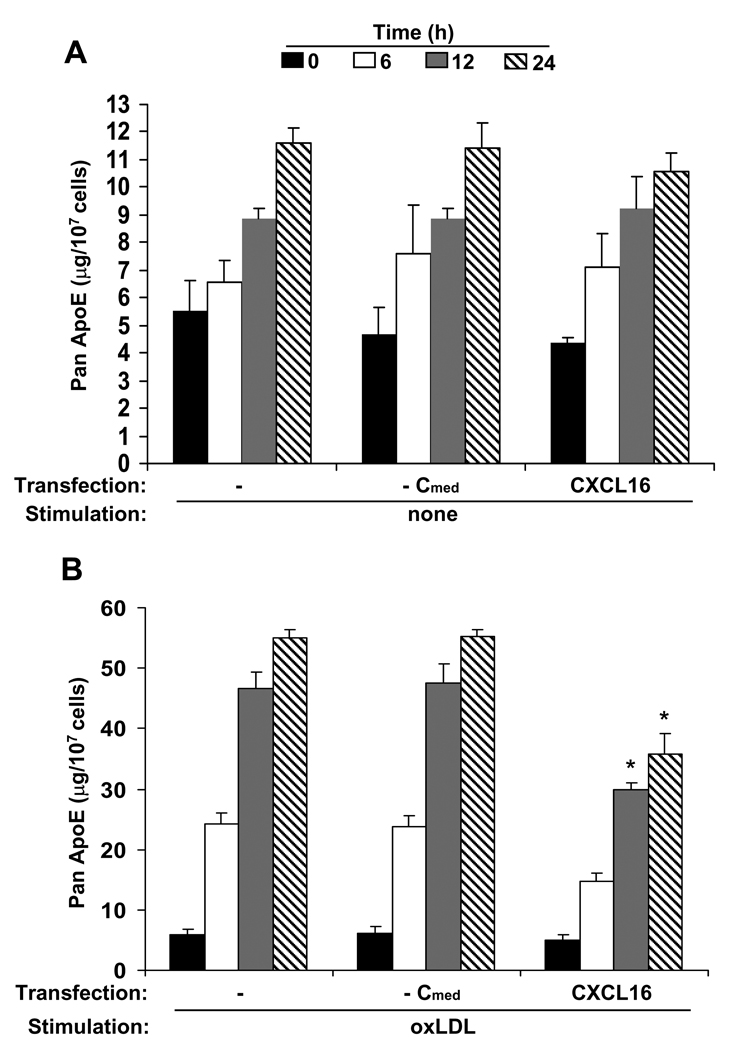
Macrophage uptake of oxLDL leads to profound changes in gene expression and lipid metabolism that collectively influence the development of atherosclerotic lesions. In this regard, cholesterol-enriched Mϕ show marked induction of anti-inflammatory and antiatherogenic ApoE as well as the adenosine triphosphate (ATP) binding cassette transporter A1 (ABCA1) and ATP binding cassette transporter G1 (ABCG1), two principal molecules involved in cholesterol efflux from foam cells. Effects of oxLDL on Mϕ gene expression are in part scavenger receptor-dependent and mediated by transcriptional activation of nuclear receptors (39). While oxLDL-induced activation of nuclear receptors results in foam cell formation which is detrimental if unopposed, it also provides a mechanism for lipid clearance from the arterial wall if coupled to RCT (39,40). As CXCL16 is a receptor for oxLDL (17,18), CXCL16 could, like other scavenger receptors, regulate nuclear receptor activity and thus control macrophage cholesterol efflux and RCT as well as the severity of atherogenic inflammation through the coordinate regulation of apoE, ABCA1, and ABCG1 expression (39–41). We tested this hypothesis and as shown in Fig. 8, lack of macrophage CXCL16 significantly decreased oxLDL-induced upregulation of ABCA1 (Fig. 8A), ABCG1 (Fig. 8B) and apoE (Fig. 8C) mRNA. Furthermore, CXCL16 deficiency affected ABCA1 and ApoE expression immediately whereas ABCG1 expression was affected at later time points (Fig. 8) Moreover, silencing of endogenous CXCL16 significantly reduced expression of macrophage (Fig. 9B), but not monocyte ApoE (Fig. 9A). These data correlate with a decrease in ApoE mRNA accumulation (Fig. 8C). Thus, our data suggest that at least one possible mechanism by which CXCL16 opposes atherosclerosis is by mediating the uptake of oxLDL, which in turn affects expression of atheroprotective molecules at the transcriptional level.
FIGURE 8. CXCL16-dependent uptake of oxLDL affects expression of atheroprotective genes.
Mo were nucleofected with 150 nM of CXCL16-specific (CXCL16) or negative control (-Cmed) sRNAi and then cultured for 12, 24 or 48 h with or without 50 µg/ml oxLDL. Cells were harvested at indicated times, RNA isolated as described in Materials and Methods, and accumulation of mRNA for ABCA1 (A), ABCG1(B) and ApoE(C) was examined. Results represent the mean ± SEM and are from 5 independent experiments with each condition tested in triplicate. Donors were the same in A–C. *p < 0.05 and **p < 0.01 vs the corresponding negative control sRNAi (-Cmed) value for the same time point.
FIGURE 9. Silencing of endogenous CXCL16 decreases production of macrophage ApoE.
Mo were transfected with sRNAi listed on the x-axis and then cultured for 6, 12 or 24 h with or without 50 µg/ml oxLDL. Cell culture supernatants were collected at indicated time points and analyzed for the presence of panApoE by ELISA. Data represent the mean ± SEM from 3 different donors with each condition tested in triplicate.*p < 0.05 vs the corresponding negative control sRNAi (-Cmed) value for the same time point.
Discussion
Within ten years cardiovascular disease will be the major cause of mortality worldwide (42), underscoring the intensified need to precisely identify and characterize mechanisms of atherogenesis. Recent investigations suggest that atherosclerosis may be mediated in part by the balance of atherogenic and atheroprotective chemokines. Currently, the sole example of an atheroprotective chemokine is CXCL16, supported by genetic data in mouse and man (8,21); however, underlying mechanisms have not been delineated. We have addressed this gap at the cellular and molecular level using a model cell system involving primary human Mϕ treated with pro-atherogenic lipids. We found that oxLDL and oxidized linoleic acid derivatives of LDL found in large amounts in atherosclerotic plaque specifically upregulated expression of CXCL16. CXCL16, one of only two known transmembrane and adhesive chemokines, was expressed in this system preferentially in the transmembrane form, not the shed form, yet did not function as an adhesion molecule promoting interaction between CXCR6+ human CASMCs and human Mϕ s, but rather as a scavenger receptor for oxLDL. It also contributed significantly towards the uptake of HDL in Mϕ. Our results also show that CXCL16 expression in Mϕ increased the rate of cholesterol efflux to lipid-poor extracellular HDL and ApoA-1 acceptors, which implies that CXCL16 is involved in macrophage RCT, a fundamental mechanism protecting against atherosclerosis (43).
Zhang et al. previously reported that oxLDL at very high concentrations could increase CXCL16 expression using a cultured human macrophage cell line (THP-1) (44). Our results extend this finding to primary human peripheral blood monocyte-derived Mϕ under lipid conditions simulating the atherogenic microenvironment. In this system, atherogenic lipids upregulate CXCL16 on Mϕ, which are the predominant inflammatory cell type expressing this chemokine in atherosclerotic lesions (17,18). The observation that CXCL16 expression accompanies the process of foam cell development in vitro (44) suggested to us that it is not functioning in this context as a classic chemokine, mediating either cell-cell adhesion or chemotaxis, since those functions would be expected to be atherogenic, not atheroprotective. In this regard, our finding that macrophage CXCL16 expression is important in the process of HDL internalization as well as in macrophage cholesterol efflux identifies a mechanism by which CXCL16 may oppose atherogenesis in atheromatous conditions and provides a potential mechanism of how CXCL16 supports the atheroprotective role of HDL.
Numerous epidemiological studies show an inverse correlation between HDL plasma level and the risk of coronary heart disease. The central anti-atherogenic activity of HDL is its ability to remove cholesterol from foam cells, SMCs and endothelial cells in the arterial wall by cholesterol efflux (38). Experimental evidence obtained in vitro and in vivo suggests that cholesterol release from foam cells is predominantly receptor-mediated and fractional. Scavenger Receptor-BI (SR-BI), the only known physiological HDL receptor, which facilitates the bidirectional flux of free cholesterol between cells and lipoprotein, stimulates ~7% of total cholesterol efflux (45). ABCA1 and ABCG1 together account for ~65% of the net cholesterol efflux to HDL or serum from cholesterol-loaded Mϕ, as revealed in studies of Abca1−/−Abcg1−/− Mϕ (46,47). Taken together, our results indicating that CXCL16 increases cholesterol egress to lipid-poor acceptors by ~34% (Fig. 7) complement genetic knockdown studies (46,47) and suggest the new hypothesis that CXCL16 negatively regulates atherogenesis in vivo by facilitating RCT.
We have shown that oxLDL induces macrophage expression of ABCA1, ABCG1 (Fig. 8) and ApoE in a CXCL16-dependent manner (Fig. 8 and Fig 9). All these molecules are involved in cholesterol efflux, the initial step in RCT (48). While the critical role of ABCA1 and ABCG1 in promoting cholesterol release from foam cells has been clearly demonstrated in vivo (46,47) and in vitro (49), bone marrow transplantation studies indicate that macrophage-derived ApoE may also be anti-atherogenic as it promotes cholesterol efflux from lipid-loaded macrophages in the artery wall by three distinct processes: ABC-independent, and ABCA1- and ABCG1-dependent. Macrophage synthesis of ApoE stimulates cholesterol efflux from cells not loaded with cholesterol but this process is ABC-independent (50). In cholesterol loaded cells, stimulation of lipid efflux by macrophage ApoE is primarily ABCA1-dependent. This is likely the predominant pathway in the artery wall that generates lipidated ApoE (51). In contrast to ABCA1, which promotes efflux to lipid-poor acceptors, ABCG1 stimulates efflux to mature HDL particles, which contain ApoE (48). The ApoE-HDL containing particles can be cleared from the plasma via SR-BI (45). As the uptake of these particles is impaired in the liver and adrenal glands of apoE−/− mice, it has been suggested that ApoE may facilitate HDL presentation to SR-BI (52). Because CXCL16-dependent oxLDL internalization affects ApoE, ABCG1 and ABCA1 expression, CXCL16 may oppose atherogenesis by increasing ABC-dependent cholesterol efflux in the vessel wall and by stimulating the SR-BI-dependent uptake of mature HDL particles in the liver. This conclusion is supported by experimental evidence demonstrating that targeted disruption of cxcl16 (8) or SR-BI (53,54) exacerbates atherosclerosis. Thus, effects of CXCL16 and SR-BI may be additive and cooperative, and expression and function of both scavenger receptors may be necessary for sustained protection against atherosclerosis.
While ABCA1 and ABCG1 are predominantly involved in cholesterol efflux (46,47), ApoE, which is produced by several tissues and cells including foamy macrophages, is a multifunctional protein that in addition to facilitating cholesterol release from foamy macrophages in atherosclerotic lesions may also inhibit SMC migration and proliferation, directly modifies lymphocyte-mediated immunity in atherosclerotic lesions and decreases vascular inflammation by suppressing production of pro-inflammatory and pro-atherogenic cytokines TNFα, IL-6 and IFNγ (55). Thus, CXCL16 may interfere with atherogenesis on multiple levels by regulating expression of this multifunctional protein.
Our results also demonstrate that CXCL16’s scavenger role in our system is supported through lipid-induced downregulation of surface ADAM10. While the mechanism through which atherogenic lipids downregulate ADAM10 remains unclear, our data suggest that these lipids shift the balance between soluble and transmembrane CXCL16 in an ADAM10-dependent manner in favor of a membrane-bound form of CXCL16. Thus, these data suggest a concept that although CXCL16 is a multimodular chemokine which exists in two different forms, soluble and membrane-bound (9,10), the atherogenic environment may dictate preference of a single configuration which may determine the role of CXCL16 in atherosclerotic lesions.
When expressed in a membrane-tethered form, CXCL16 could conceivably support cell-cell adhesion (11), which could play a role in plaque evolution. Consistent with this, transmembrane CXCL16 was shown to function as a pro-adhesive chemokine promoting adhesion of primary cells, predominantly T cells to fibroblastic reticular cells in the lymph node (56), to the follicle-associated epithelial cells covering Peyer's patches (57) and to the vascular endothelium (58), suggesting that the CXCR6-CXCL16 axis may contribute critically in the formation of primary and secondary T cell responses. Contrary to these investigations, our results show that while CXCR6 and CXCL16 are expressed in atherosclerotic lesions and in our model system, this axis does not mediate adhesion in our model system and thus may not be critical for capture, retention and organization of inflammatory cells in plaques, at least not in early atherosclerotic lesions in which the two major cell types involved in intercellular interactions are foam cell Mϕ and SMCs (34).
Cellular cholesterol efflux and RCT constitute a potent physiological protective system against atherosclerosis (38,43); however, the involvement of many players in the metabolic pathway of HDL makes this system a difficult therapeutic target. Our investigation establishes a link between CXCL16, HDL and macrophage cholesterol efflux, and provides the first experimental support at the molecular and cellular level using primary human cells relevant to atherosclerotic plaque for the scavenger mechanism of atheroprotection mediated by CXCL16 proposed originally by Aslanian et al. (8). Our work has identified important new questions for future investigation, such as how CXCL16 mediates selective uptake of lipoproteins and cholesterol efflux from Mϕ, how atherogenic lipids turn on CXCL16 expression while turning off ADAM10, and how CXCR6 can promote atherogenesis while its ligand restricts it.
Supplementary Material
Acknowledgments
Sources of Funding
This work was funded by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health (Bethesda, MD), and in part by a Wellcome Trust Career Development Award in Basic Biomedical Sciences ref. # 081169 (to J Barlic).
Footnotes
Disclosures
None.
References
- 1.Witztum JL. The oxidation hypothesis of atherosclerosis. The Lancet. 1994;344:793–795. doi: 10.1016/s0140-6736(94)92346-9. [DOI] [PubMed] [Google Scholar]
- 2.Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- 3.Hansson GK, Robertson AK, Soderberg-Naucler C. Inflammation and Atherosclerosis. Annu Rev Pathol: Mechanisms of Disease. 2006;1:297–329. doi: 10.1146/annurev.pathol.1.110304.100100. [DOI] [PubMed] [Google Scholar]
- 4.Barlic J, Murphy PM. Chemokine regulation of atherosclerosis. J Leukoc Biol. 2007;82:226–236. doi: 10.1189/jlb.1206761. [DOI] [PubMed] [Google Scholar]
- 5.Charo IF, Taubman MB. Chemokines in the Pathogenesis of Vascular Disease. Circ Res. 2004;95:858–866. doi: 10.1161/01.RES.0000146672.10582.17. [DOI] [PubMed] [Google Scholar]
- 6.Zernecke A, Shagdarsuren E, Weber C. Chemokines in Atherosclerosis: An Update. Arterioscler Thromb Vasc Biol. 2008;28:1897–1908. doi: 10.1161/ATVBAHA.107.161174. [DOI] [PubMed] [Google Scholar]
- 7.Murphy PM, Baggiolini M, Charo IF, Hebert CA, Horuk R, Matsushima K, Miller LH, Oppenheim JJ, Power CA. International Union of Pharmacology. XXII. Nomenclature for Chemokine Receptors. Pharmacol Rev. 2000;52:145–176. [PubMed] [Google Scholar]
- 8.Aslanian AM, Charo IF. Targeted Disruption of the Scavenger Receptor and Chemokine CXCL16 Accelerates Atherosclerosis. Circulation. 2006;114:583–590. doi: 10.1161/CIRCULATIONAHA.105.540583. [DOI] [PubMed] [Google Scholar]
- 9.Matloubian M, David A, Engel S, Ryan JE, Cyster JG. A transmembrane CXC chemokine is a ligand for HIV-coreceptor Bonzo. Nat Immunol. 2000;1:298–304. doi: 10.1038/79738. [DOI] [PubMed] [Google Scholar]
- 10.Wilbanks A, Zondlo SC, Murphy K, Mak S, Soler D, Langdon P, Andrew DP, Wu L, Briskin M. Expression Cloning of the STRL33/BONZO/TYMSTR Ligand Reveals Elements of CC, CXC, and CX3C Chemokines. J Immunol. 2001;166:5145–5154. doi: 10.4049/jimmunol.166.8.5145. [DOI] [PubMed] [Google Scholar]
- 11.Shimaoka T, Nakayama T, Fukumoto N, Kume N, Takahashi S, Yamaguchi J, Minami M, Hayashida K, Kita T, Ohsumi J, Yoshie O, Yonehara S. Cell surface-anchored SR-PSOX/CXC chemokine ligand 16 mediates firm adhesion of CXC chemokine receptor 6-expressing cells. J Leukoc Biol. 2004;75:267–274. doi: 10.1189/jlb.1003465. [DOI] [PubMed] [Google Scholar]
- 12.Tabata S, Kadowaki N, Kitawaki T, Shimaoka T, Yonehara S, Yoshie O, Uchiyama T. Distribution and kinetics of SR-PSOX/CXCL16 and CXCR6 expression on human dendritic cell subsets and CD4+ T cells. J Leukoc Biol. 2005;77:777–786. doi: 10.1189/jlb.1204733. [DOI] [PubMed] [Google Scholar]
- 13.Wagsater D, Olofsson PS, Norgren L, Stenberg B, Sirsjo A. The chemokine and scavenger receptor CXCL16/SR-PSOX is expressed in human vascular smooth muscle cells and is induced by interferon gamma. Biochem Biophys Res Commun. 2004;325:1187–1193. doi: 10.1016/j.bbrc.2004.10.160. [DOI] [PubMed] [Google Scholar]
- 14.Abel S, Hundhausen C, Mentlein R, Schulte A, Berkhout TA, Broadway N, Hartmann D, Sedlacek R, Dietrich S, Muetze B, Schuster B, Kallen KJ, Saftig P, Rose-John S, Ludwig A. The Transmembrane CXC-Chemokine Ligand 16 Is Induced by IFN-{gamma} and TNF-{alpha} and Shed by the Activity of the Disintegrin-Like Metalloproteinase ADAM10. J Immunol. 2004;172:6362–6372. doi: 10.4049/jimmunol.172.10.6362. [DOI] [PubMed] [Google Scholar]
- 15.Gough PJ, Garton KJ, Wille PT, Rychlewski M, Dempsey PJ, Raines EW. A Disintegrin and Metalloproteinase 10-Mediated Cleavage and Shedding Regulates the Cell Surface Expression of CXC Chemokine Ligand 16. J Immunol. 2004;172:3678–3685. doi: 10.4049/jimmunol.172.6.3678. [DOI] [PubMed] [Google Scholar]
- 16.Shimaoka T, Kume N, Minami M, Hayashida K, Kataoka H, Kita T, Yonehara S. Molecular Cloning of a Novel Scavenger Receptor for Oxidized Low Density Lipoprotein, SR-PSOX, on Macrophages. J Biol Chem. 2000;275:40663–40666. doi: 10.1074/jbc.C000761200. [DOI] [PubMed] [Google Scholar]
- 17.Minami M, Kume N, Shimaoka T, Kataoka H, Hayashida K, Akiyama Y, Nagata I, Ando K, Nobuyoshi M, Hanyuu M, Komeda M, Yonehara S, Kita T. Expression of SR-PSOX, a Novel Cell-Surface Scavenger Receptor for Phosphatidylserine and Oxidized LDL in Human Atherosclerotic Lesions. Arterioscler Thromb Vasc Biol. 2001;21:1796–1800. doi: 10.1161/hq1001.096652. [DOI] [PubMed] [Google Scholar]
- 18.Minami M, Kume N, Shimaoka T, Kataoka H, Hayashida K, Yonehara S, Kita T. Expression of Scavenger Receptor for Phosphatidylserine and Oxidized Lipoprotein (SR-PSOX) in Human Atheroma. Ann NY Acad Sci. 2001;947:373–376. doi: 10.1111/j.1749-6632.2001.tb03966.x. [DOI] [PubMed] [Google Scholar]
- 19.Smith C, Halvorsen B, Otterdal K, Waehre T, Yndestad A, Fevang B, Sandberg WJ, Breland UM, Froland SS, Oie E, Gullestad L, Damas JK, Aukrust P. High levels and inflammatory effects of soluble CXC ligand 16 (CXCL16) in coronary artery disease: down-regulatory effects of statins. Cardiovasc Res. 2008;79:195–203. doi: 10.1093/cvr/cvn071. [DOI] [PubMed] [Google Scholar]
- 20.Sheikine Y, Bang CS, Nilsson L, Samnegard A, Hamsten A, Jonasson L, Eriksson P, Sirsjo A. Decreased plasma CXCL16/SR-PSOX concentration is associated with coronary artery disease. Atherosclerosis. 2006;188:462–466. doi: 10.1016/j.atherosclerosis.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 21.Lundberg GA, Kellin A, Samnegard A, Lundman P, Tornvall P, Dimmeler S, Zeiher AM, Hamsten A, Hansson GK, Eriksson P. Severity of coronary artery stenosis is associated with a polymorphism in the CXCL16/SR-PSOX gene. J Intern Med. 2005;257:415–422. doi: 10.1111/j.1365-2796.2005.01469.x. [DOI] [PubMed] [Google Scholar]
- 22.Galkina E, Harry BL, Ludwig A, Liehn EA, Sanders JM, Bruce A, Weber C, Ley K. CXCR6 Promotes Atherosclerosis by Supporting T-Cell Homing, Interferon-{gamma} Production, and Macrophage Accumulation in the Aortic Wall. Circulation. 2007;116:1801–1811. doi: 10.1161/CIRCULATIONAHA.106.678474. [DOI] [PubMed] [Google Scholar]
- 23.Harland WWA, Gilbert JJD, Brooks CCJ. Lipids of human atheroma. 8. Oxidised derivatives of cholesteryl linoleate. Biochim Biophys Acta. 1973;316:378–385. [PubMed] [Google Scholar]
- 24.Jira W, Spiteller G, Carson W, Schramm A. Strong increase in hydroxy fatty acids derived from linoleic acid in human low density lipoproteins of atherosclerotic patients. Chem Phys Lipids. 1998;91:1–11. doi: 10.1016/s0009-3084(97)00095-9. [DOI] [PubMed] [Google Scholar]
- 25.Berliner JA, Subbanagounder G, Leitinger N, Watson AD, Vora D. Evidence for a Role of Phospholipid Oxidation Products in Atherogenesis. Trends Cardiovasc Med. 2001;11:142–147. doi: 10.1016/s1050-1738(01)00098-6. [DOI] [PubMed] [Google Scholar]
- 26.Barlic J, Zhang Y, Foley JF, Murphy PM. Oxidized Lipid-Driven Chemokine Receptor Switch, CCR2 to CX3CR1, Mediates Adhesion of Human Macrophages to Coronary Artery Smooth Muscle Cells Through a Peroxisome Proliferator-Activated Receptor {gamma}-Dependent Pathway. Circulation. 2006;114:807–819. doi: 10.1161/CIRCULATIONAHA.105.602359. [DOI] [PubMed] [Google Scholar]
- 27.Barlic J, Zhang Y, Murphy PM. Atherogenic Lipids Induce Adhesion of Human Coronary Artery Smooth Muscle Cells to Macrophages by Up-regulating Chemokine CX3CL1 on Smooth Muscle Cells in a TNF{alpha}-NF{kappa}B-dependent Manner. J Biol Chem. 2007;282:19167–19176. doi: 10.1074/jbc.M701642200. [DOI] [PubMed] [Google Scholar]
- 28.Livak KJ, Schmittgen TD. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2-[Delta][Delta]CT Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 29.Frostegard J, Nilsson J, Haegerstrand A, Hamsten A, Wigzell H, Gidlund M. Oxidized low density lipoprotein induces differentiation and adhesion of human monocytes and the monocytic cell line U937. Proc Natl Acad Sci U S A. 1990;87:904–908. doi: 10.1073/pnas.87.3.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geng Y, Kodama T, Hansson GK. Differential expression of scavenger receptor isoforms during monocyte-macrophage differentiation and foam cell formation. Arterioscler Thromb. 1994;14:798–806. doi: 10.1161/01.atv.14.5.798. [DOI] [PubMed] [Google Scholar]
- 31.Inoue M, Itoh H, Tanaka T, Chun TH, Doi K, Fukunaga Y, Sawada N, Yamshita J, Masatsugu K, Saito T, Sakaguchi S, Sone M, Yamahara Ki, Yurugi T, Nakao K. Oxidized LDL Regulates Vascular Endothelial Growth Factor Expression in Human Macrophages and Endothelial Cells Through Activation of Peroxisome Proliferator-Activated Receptor-{gamma} Arterioscler Thromb Vasc Biol. 2001;21:560–566. doi: 10.1161/01.atv.21.4.560. [DOI] [PubMed] [Google Scholar]
- 32.Maxeiner H, Husemann J, Thomas CA, Loike JD, Khoury JE, Silverstein SC. Complementary Roles for Scavenger Receptor A and CD36 of Human Monocyte-derived Macrophages in Adhesion to Surfaces Coated with Oxidized Low-Density Lipoproteins and in Secretion of H2O2. J Exp Med. 1998;188:2257–2265. doi: 10.1084/jem.188.12.2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore KJ, Rosen ED, Fitzgerald ML, Randow F, Andersson LP, Altshuler D, Milstone DS, Mortensen RM, Spiegelman BM, Freeman MW. The role of PPAR-{gamma} in macrophage differentiation and cholesterol uptake. Nat Med. 2001;7:41–47. doi: 10.1038/83328. [DOI] [PubMed] [Google Scholar]
- 34.Stary HC, Chandler AB, Glagov S, Guyton JR, Insull W, Jr, Rosenfeld ME, Schaffer SA, Schwartz CJ, Wagner WD, Wissler RW. A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1994;89:2462–2478. doi: 10.1161/01.cir.89.5.2462. [DOI] [PubMed] [Google Scholar]
- 35.Ludwig A, Weber C. Transmembrane chemokines: versatile 'special agents' in vascular inflammation. Thromb Haemost. 2007;97:694–703. [PubMed] [Google Scholar]
- 36.Kunjathoor VV, Febbraio M, Podrez EA, Moore KJ, Andersson L, Koehn S, Rhee JS, Silverstein R, Hoff HF, Freeman MW. Scavenger Receptors Class A-I/II and CD36 Are the Principal Receptors Responsible for the Uptake of Modified Low Density Lipoprotein Leading to Lipid Loading in Macrophages. J Biol Chem. 2002;277:49982–49988. doi: 10.1074/jbc.M209649200. [DOI] [PubMed] [Google Scholar]
- 37.Goldstein JL, Ho YK, Basu SK, Brown MS. Binding Site on Macrophages that Mediates Uptake and Degradation of Acetylated Low Density Lipoprotein, Producing Massive Cholesterol Deposition. Proc Natl Acad Sci U S A. 1979;76:333–337. doi: 10.1073/pnas.76.1.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohashi R, Mu H, Wang X, Yao Q, Chen C. Reverse cholesterol transport and cholesterol efflux in atherosclerosis. QJM. 2005;98:845–856. doi: 10.1093/qjmed/hci136. [DOI] [PubMed] [Google Scholar]
- 39.Chawla A, Boisvert WA, Lee CH, Laffitte BA, Barak Y, Joseph SB, Liao D, Nagy L, Edwards PA, Curtiss LK, Evans RM, Tontonoz P. A PPAR[gamma]-LXR-ABCA1 Pathway in Macrophages Is Involved in Cholesterol Efflux and Atherogenesis. Mol Cell. 2001;7:161–171. doi: 10.1016/s1097-2765(01)00164-2. [DOI] [PubMed] [Google Scholar]
- 40.Laffitte BA, Repa JJ, Joseph SB, Wilpitz DC, Kast HR, Mangelsdorf DJ, Tontonoz P. LXRs control lipid-inducible expression of the apolipoprotein E gene in macrophages and adipocytes. Proc Natl Acad Sci U S A. 2001;8:507–512. doi: 10.1073/pnas.021488798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naik SU, Wang X, Da Silva JS, Jaye M, Macphee CH, Reilly MP, Billheimer JT, Rothblat GH, Rader DJ. Pharmacological Activation of Liver X Receptors Promotes Reverse Cholesterol Transport In Vivo. Circulation. 2006;113:90–97. doi: 10.1161/CIRCULATIONAHA.105.560177. [DOI] [PubMed] [Google Scholar]
- 42.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, Haase N, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O'Donnell CJ, Roger V, Rumsfeld J, Sorlie P, Steinberger J, Thom T, Wasserthiel-Smoller S, Hong Y, C for the American Heart Association Statistics, and S. Stroke Statistics. Heart Disease and Stroke Statistics--2007 Update: A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 43.Tall AR. Cholesterol efflux pathways and other potential mechanisms involved in the athero-protective effect of high density lipoproteins. J Intern Med. 2008;263:256–273. doi: 10.1111/j.1365-2796.2007.01898.x. [DOI] [PubMed] [Google Scholar]
- 44.Zhang L, Liu HJ, Li TJ, Yang Y, Guo XL, Wu MC, Rui YC, Wei LX. Lentiviral vector-mediated siRNA knockdown of SR-PSOX inhibits foam cell formation in vitro. Acta Pharmacol Sin. 2008;29:847–852. doi: 10.1111/j.1745-7254.2008.00823.x. [DOI] [PubMed] [Google Scholar]
- 45.Huby T, Doucet C, Dachet C, Ouzilleau B, Ueda Y, Afzal V, Rubin E, Chapman MJ, Lesnik P. Knockdown expression and hepatic deficiency reveal an atheroprotective role for SR-BI in liver and peripheral tissues. J Clin Invest. 2006;116:2767–2776. doi: 10.1172/JCI26893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Out R, Hoekstra M, Habets K, Meurs I, de Waard V, Hildebrand RB, Wang Y, Chimini G, Kuiper J, Van Berkel TJC, Van Eck M. Combined Deletion of Macrophage ABCA1 and ABCG1 Leads to Massive Lipid Accumulation in Tissue Macrophages and Distinct Atherosclerosis at Relatively Low Plasma Cholesterol Levels. Arterioscler Thromb Vasc Biol. 2008;28:258–264. doi: 10.1161/ATVBAHA.107.156935. [DOI] [PubMed] [Google Scholar]
- 47.Yvan-Charvet L, Ranalletta M, Wang N, Han S, Terasaka N, Li R, Welch C, Tall AR. Combined deficiency of ABCA1 and ABCG1 promotes foam cell accumulation and accelerates atherosclerosis in mice. J Clin Invest. 2007;117:3900–3908. doi: 10.1172/JCI33372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tall AR, Yvan-Charvet L, Terasaka N, Pagler T, Wang N. HDL, ABC Transporters, and Cholesterol Efflux: Implications for the Treatment of Atherosclerosis. Cell Metab. 2008;7:365–375. doi: 10.1016/j.cmet.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 49.Liu L, Bortnick AE, Nickel M, Dhanasekaran P, Subbaiah PV, Lund-Katz S, Rothblat GH, Phillips MC. Effects of Apolipoprotein A-I on ATP-binding Cassette Transporter A1-mediated Efflux of Macrophage Phospholipid and Cholesterol: Formation of Nascent High Density Lipoprotein Particles. J Biol Chem. 2003;278:42976–42984. doi: 10.1074/jbc.M308420200. [DOI] [PubMed] [Google Scholar]
- 50.Huang ZH, Fitzgerald ML, Mazzone T. Distinct Cellular Loci for the ABCA1-Dependent and ABCA1-Independent Lipid Efflux Mediated by Endogenous Apolipoprotein E Expression. Arterioscler Thromb Vasc Biol. 2006;26:157–162. doi: 10.1161/01.ATV.0000193627.12516.1d. [DOI] [PubMed] [Google Scholar]
- 51.Yancey PG, Yu H, Linton MF, Fazio S. A Pathway-Dependent on ApoE, ApoAI, and ABCA1 Determines Formation of Buoyant High-Density Lipoprotein by Macrophage Foam Cells. Arterioscler Thromb Vasc Biol. 2007;27:1123–1131. doi: 10.1161/ATVBAHA.107.139592. [DOI] [PubMed] [Google Scholar]
- 52.Arai T, Rinninger F, Varban L, Fairchild-Huntress V, Liang CP, Chen W, Seo T, Deckelbaum R, Huszar D, Tall AR. Decreased selective uptake of high density lipoprotein cholesteryl esters in apolipoprotein E knock-out mice. Proc Natl Acad Sci U S A. 1999;96:12050–12055. doi: 10.1073/pnas.96.21.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang W, Yancey PG, Su YR, Babaev VR, Zhang Y, Fazio S, Linton MF. Inactivation of Macrophage Scavenger Receptor Class B Type I Promotes Atherosclerotic Lesion Development in Apolipoprotein E-Deficient Mice. Circulation. 2003;108:2258–2263. doi: 10.1161/01.CIR.0000093189.97429.9D. [DOI] [PubMed] [Google Scholar]
- 54.Van Eck M, Bos IS, Hildebrand RB, Van Rij BT, Van Berkel TJC. Dual Role for Scavenger Receptor Class B, Type I on Bone Marrow-Derived Cells in Atherosclerotic Lesion Development. Am J Pathol. 2004;165:785–794. doi: 10.1016/S0002-9440(10)63341-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Curtiss LK. ApoE in Atherosclerosis: A Protein With Multiple Hats. Arterioscler Thromb Vasc Biol. 2000;20:1852–1853. doi: 10.1161/01.atv.20.8.1852. [DOI] [PubMed] [Google Scholar]
- 56.Hara T, Katakai T, Lee JH, Nambu Y, Nakajima-Nagata N, Gonda H, Sugai M, Shimizu A. A transmembrane chemokine, CXC chemokine ligand 16, expressed by lymph node fibroblastic reticular cells has the potential to regulate T cell migration and adhesion. Int Immunol. 2006;18:301–311. doi: 10.1093/intimm/dxh369. [DOI] [PubMed] [Google Scholar]
- 57.Hase K, Murakami T, Takatsu H, Shimaoka T, Iimura M, Hamura K, Kawano K, Ohshima S, Chihara R, Itoh K, Yonehara S, Ohno H. The Membrane-Bound Chemokine CXCL16 Expressed on Follicle-Associated Epithelium and M Cells Mediates Lympho-Epithelial Interaction in GALT. J Immunol. 2006;176:43–51. doi: 10.4049/jimmunol.176.1.43. [DOI] [PubMed] [Google Scholar]
- 58.Postea O, Koenen RR, Hristov M, Weber C, Ludwig A. Homocysteine Upregulates Vascular Transmembrane Chemokine CXCL16 and Induces CXCR6+ Lymphocyte Recruitment in vitro and in vivo. J Cell Mol Med. 2008;12:1700–1709. doi: 10.1111/j.1582-4934.2008.00223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.