Abstract
Objective
Conventional pterional approach is a commonly used neurosurgical technique for the treatment of cerebral aneurysms. However, this technique requires more extensive brain exposure than other key hole approaches and is sometimes associated with surgical traumatization or cosmetic problems. The aim of this study was to compare the postoperative outcome between pterional and supraorbital keyhole approaches in the patients with anterior circulation aneurysms.
Methods
The authors reviewed patients with anterior circulation aneurysms who underwent aneurysm clipping via pterional or supraorbital keyhole approach at a single institute over a period of 2 years. Ninety-eight patients harboring 108 aneurysms were included in this study. Various outcomes were recorded, which included clinical grade, cosmetic problems, patients' satisfaction and complications such as chewing discomfort, frontal muscle weakness, hyposmia, infection.
Results
The supraorbital approach exhibited a shorter operation time compared with the pterional approach. Complications such as chewing discomfort occurred less frequently in the supraorbital approach group. Moreover, the cosmetic outcome was significantly better in the supraorbital group than in the pterional group.
Conclusion
The supraorbital keyhole approach reduced intra- and postoperative complications, including chewing discomfort and cosmetic disturbances, compared with the conventional pterional approach.
Keywords: Pterional approach, Supraorbital approach, Aneurysm, Clipping, Cosmetic outcome
INTRODUCTION
The pterional approach has been used in neurosurgery primarily for the treatment of a wide variety of neurosurgical disorders1-7,11,33). In vascular neurosurgery, in particular, pterional craniotomy exploits the advantages of naturally occurring planes and spaces that can be used to expose the base of the brain and the major structures of the circle of Willis, without significant brain retraction14,19,25). However, this traditional approach requires relatively extensive skin, bone, and brain exposure, possibly causing an increase in iatrogenic complication22,28,32).
In recent decades, however, the improvement of operating microscopes and refined instrumentation allowed the evolution of microneurosurgical techniques8,15,21,26-32). These techniques and the enormous development of diagnostic facilities permit the treatment of certain intracranial lesions using very small openings. Nowadays, increasing evidence shows that keyhole techniques, if applied properly, are appropriate for the obliteration of intracranial aneurysms9,10,13,18,21,26,31). Among the various keyhole procedures, the supraorbital approach is most frequently applied to the treatment of supratentorial aneurysms.
The supraorbital keyhole craniotomy via an eyebrow skin incision is well described by Perneczky et al.24,27,28). The successful management of supratentorial aneurysms by keyhole supraorbital craniotomy has recently been reported9,10,13,17,21,24,26-32). However, a remarkable controversy remains regarding the choice between the supraorbital keyhole approach9,32), and the pterional approach12,16), which is the traditional method for the surgical management of patients with anterior circulation aneurysms. Here, we describe our preliminary experience with the supraorbital keyhole approach for the clipping of anterior circulation aneurysms and compare it with the traditional pterional approach in terms of patient's subjective outcome assessment.
MATERIALS AND METHODS
Patient population
Between July 2006 and April 2008, we clipped 102 patients harboring 113 intracranial aneurysms of the anterior circulation. Among them, ninety-eight patients harboring 108 aneurysms were enrolled in this study. All operations were performed by the same surgeon at a single institute over a 2-year period. The clinical files and surgical reports of these patients were studied to assess the localization and management of the aneurysms, surgery-related complications, and intraoperative and postoperative problems. The patient's preoperative condition was assessed according to the Hunt-Hess and the Fisher grading scales. Exact diagnostic imaging was completed before surgery in every case, to provide an accurate definition of the variations in the anatomic and pathological structures. Three-dimensional (3D) angiographic computed tomography (CT) was performed preoperatively in all patients. The surgical approach was decided after the careful survey of the patient's anatomy of intracranial structures and aneurysm. Inferior direction aneurysms on the anterior communicating artery (ACOM) or middle cerebral artery (MCA) aneurysms with a long M1 were excluded from the supraorbital keyhole approach group. Two groups were analyzed for comparability of demographic and clinical variables, which included age, sex, aneurysm location, Hunt-Hess grade, and Fisher grade. Postoperative complications, outcome, and patient's satisfaction were recorded six months after surgery. Clinical outcome was assessed using the modified Rankin Scale (mRS) at six months after surgery. Poor outcome was defined as a mRS score of 4-6, which indicates severe disability or death. Scar tenderness and cosmetic satisfaction were evaluated using the patient's subjective sense as a score between 1 and 5. These descriptions were rated on a 5-cm visual analog scale (VAS), with "none" and "most severe imaginable" (scar tenderness, 1 = no pain, 5 = severe pain; cosmetic satisfaction, 1 = very satisfied, 5 = not satisfied). These values were compared between the pterional and supraorbital keyhole groups. The significance of observed differences between the variables was assessed by a Student's t-test and a Mann-Whitney U-test. A p value less than 0.05 was considered significant.
Operative technique
The supraorbital keyhole approach performed in this study was described in detail by Perneczky et al.28,32). The patient was placed in the supine position. The head was elevated above the level of the heart and turned between 15° and 60° to the contralateral side of the intended incision. The extent of head rotation depended on the location of the lesion. For ipsilateral MCA lesions, 15° of head rotation was used; for lesions of the communicating segment of the internal carotid artery (ICA), 20-30° of head rotation has been found to be sufficient. Surgery of the anterior communicating artery required a rotation of 40-60°. The neck of the patient was slightly retroflexed so that the zygomatic arch was the highest point. This position allows the gravity-related self-retraction of the frontal lobe. After sterilizing the eyebrow region, a standard skin incision was made in the superior edge of the eyebrow or on the forehead crease just above the eyebrow, starting from the midpupillary line and extending laterally to just behind the frontal process of the zygomatic bone. The supraorbital nerve and artery, the frontal branches of the facial nerve, and the superficial temporal artery were always preserved. Subcutaneous dissection was performed from the supraorbital foramen to the frontozygomatic suture. The temporalis fascia was incised a few millimeters before its insertion at the anterior temporal line. The keyhole was exposed via subperiosteal dissection of the temporalis muscle.
A burr hole was drilled on the superior temporal line, just above the frontal base. The craniotomy was performed using a high-speed drill. The medial-inferior edge of the craniotomy went around the level of the frontal base and the lateral edge to the sphenoid wing, at a width of 25-30 mm and a height of 15-25 mm. A large frontal sinus is a relative contraindication to this approach. If the frontal sinus was entered, it was exenterated by stripping and cauterizing its mucosa. The sinus was then covered with a periosteal flap. The dura was opened in a semicircular fashion. A conventional microsurgical technique was used with optimal illumination with a operative microscope. The arachnoid of the carotid cistern, the Sylvian fissure, and suprasellar cisterns were opened for CSF drainage, to create enough room for brain retraction and surgical manipulation. To increase CSF drainage, the membrane of the lamina terminalis was sometimes opened. At the end of the operation, a watertight dural closure was obtained using silk suture and fibrin glue. The temporalis muscle and fascia were sutured to the frontal pericranium. The skin was closed layer by layer.
RESULTS
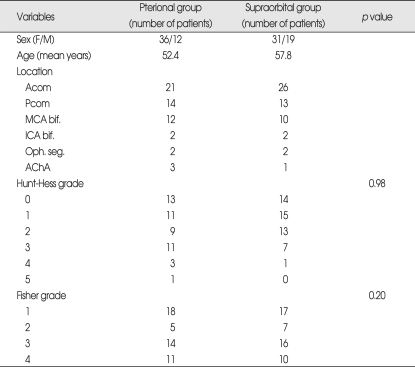
Nine of the 102 patients had two or more aneurysms. Four out of nine patients presenting with multiple aneurysms were excluded because of the need for multiple surgical approaches. Among the remaining 98 patients, 48 patients with 54 aneurysms were treated with the pterional approach, and 50 patients with 54 aneurysms were treated with the supraorbital keyhole approach. Three patients in the pterional group and two patients in the supraorbital keyhole group had two aneurysms that were treated via a single surgical approach. Sixty-seven patients were female, and thirty-one were male. The mean age was 55.7 ± 12.3 years. Pre-operative clinical data were presented (Table 1). The two groups showed a similar distribution of aneurysm location. ACOM was the most common lesion site, followed by the posterior communicating artery (PCOM) and MCA bifurcation. There was no significant difference in clinical grade between the two groups (Table 1).
Table 1.
Clinical data of patients
AChA : anterior choroidal artery, Acom : anterior communicating artery, bif. : bifurcation, Pcom : posterior communicating artery, Oph. seg. : ophthalmic segment of internal carotid artery
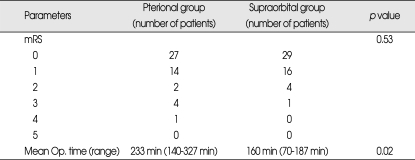
All of the aneurysms were clipped successfully. The overall outcome was good in both groups (Table 2). The mRS scores showed a similar distribution between the pterional and supraorbital groups; however, the operative time was markedly decreased in the supraorbital group (p = 0.02). Several complications were noted postoperatively (Table 3). We recorded these complications at two weeks and six months after surgery. Most complications were resolved six months later. Patients in the pterional group suffered complications twice as often as patients in the supraorbital group (85% vs. 42%; p < 0.01). The frequency of complications was high in the pterional group in most cases, especially regarding chewing discomfort or problem (65% vs. 10%; p < 0.01 at two weeks postoperatively; 40% vs. 6%; p < 0.01 at six months postoperatively). Although frontal numbness was elevated in the supraorbital group (2% vs. 18%; p < 0.01), this complication was resolved at the six-month follow-up in all cases.
Table 2.
Clinical outcome and operation time
Table 3.
Postoperative complications
CSF : cerebrospinal fluid
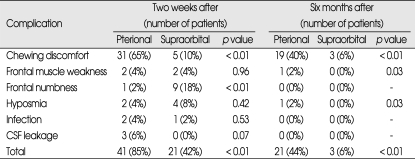
The supraorbital group also showed good results regarding cosmetic outcome (Table 4). Scar tenderness was significantly lower in the supraorbital group (2.1 ± 0.7 vs. 1.7 ± 0.7; p = 0.003). Cosmetic satisfaction was better in the pterional group, although this result was not significant (p = 0.093).
Table 4.
Cosmetic outcome
app. : approach; SD : standard deviation
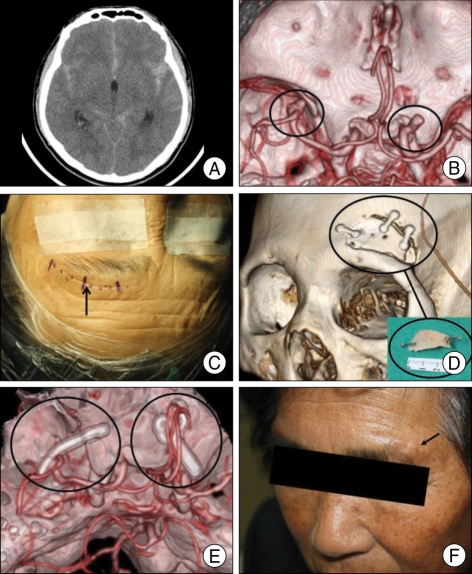
Illustrative case
Fig. 1 demonstrates a case of supraorbital keyhole approach. This 72-year-old woman presented with an aneurysmal subarachnoid hemorrhage. Hunt-Hess grade was II, and Fisher grade was III in this patient. Neuroimaging investigation revealed that she had two aneurysms, one on the left MCA bifurcation and another on the right ophthalmic segment. Based on CT data demonstrating a slight preponderance of blood in the left sylvian fissure, it was thought that the left-sided MCA bifurcation aneurysm was the cause of the subarachnoid hemorrhage. The ruptured MCA bifurcation aneurysm was clipped via supr-aorbital keyhole approach, and the contralateral ophthalmic segment aneurysm was clipped via the same corridor. A neurologically normal outcome was achieved (mRS score = 0). The patient complained of forehead numbness for about two months, which resolved spontaneously. She had an excellent cosmetic satisfaction (score = 1) and no scar tenderness (score = 1).
Fig. 1.
A : Computed tomography (CT) scan revealing a slight preponderance of blood in the left sylvian fissure in a 72-year-old female presented with a subarachnoid hemorrhage. B : CT angiography showing the presence of two aneurysms, one at the left middle cerebral artery bifurcation and another at the right ophthalmic segment of the internal cerebral artery. C : A photograph showing a skin incision marking on a forehead crease. D : Postoperative 3-dimensional CT image demonstrating the craniotomy site and the bone flap (small box). E : Postoperative CT angiography showing the aneurysms clipped via one corridor using the supraorbital approach. F : Photograph of the patient obtained six months after operation demonstrating a minute scar without depressed deformity.
DISCUSSION
Since Yasargil and Fox33) first described frontotemporal craniotomy with a pterional approach, this technique has replaced bifrontal and frontolateral craniotomies for access to aneurysms of the anterior circulation. However, the standard pterional approach requires a semicircular skin incision using either a musculocutaneous flap or an interfascial dissected temporal muscle flap and a conventional frontotemporal craniotomy33); this relatively wider exposure of the brain can cause an increase in surgical morbidity not related to the lesion. Patients sometimes complain of postoperative cosmetic impairments in the frontotemporal area resulting from the large skin incision scar, depression of the bone flap, inappropriate repair of burr holes, or temporal muscle atrophy.
Recently, the application of the minimally invasive concept to neurosurgical procedures has gained acceptance among neurosurgeons, with the understanding that keyhole surgery is not the miniaturization of any standard technique but rather the natural evolution into a more precise and refined act. Various modified and combined pterional approaches to skull-base lesions have been reported1-7). Perneczky and colleagues8,23,24,27,28,32) advocated the keyhole concept in neurosurgery and have used supraorbital minicraniotomy extensively to treat a variety of lesions. Eyebrow skin incision and supraorbital keyhole craniotomy were originally recommended for microsurgery of various cerebral aneurysms and tumors located in the supra- and parasellar regions27,28,32).
One of the most important goals of the supraorbital keyhole approach is the minimization of the brain exposure via limited and more specific craniotomies. Exposure of brain tissue for several hours during extended craniotomies always means an injury of the surface by nonphysiological surroundings, such as room air, irrigation media, and cover material. The supraorbital keyhole approach offers minimal brain exposure to air and accidental surgical trauma. Moreover, brain retraction is minimized or absent in this procedure. This significantly decreases approach-related surgical morbidity and shortens hospitalization. In terms of operative time, experienced surgeons need less time to perform the surgery using the pterional craniotomy. However, manipulation of the temporal muscle and performing a relatively larger size of the craniotomy may need more time.
The anatomy of the suprasellar area offers several advantages for keyhole approaches from the anterior32). The suprasellar area is bordered by the mesencephalon posteriorly and by the temporal lobes laterally. Therefore, approaches from these sides require retraction of brain tissue. Anteriorly, however, there are several windows into the suprasellar area that do not require brain retraction. Supraorbital craniotomy offers access to the circle of Willis, and dissection of the sylvian fissure can be performed easily. The burr hole in the frontal bone may be expanded backwardly or downwardly, if additional exposure of the middle fossa is desired. In addition, orbital rim osteotomy provides a direct view of the anterior cranial fossa, which includes the sellar and suprasellar regions, with even less brain retraction10,11,13,15). If the frontal process of the zygomatic bone is removed, the structures of the middle fossa can be well appreciated. This approach allows clipping of aneurysms located in the ipsilateral internal carotid artery, anterior communicating artery, and middle cerebral artery, and even in the contralateral internal carotid artery. According to van Lindert et al.32), there were no approach-related complications in 139 supraorbital keyhole craniotomies performed for aneurysms of the anterior circulation.
The most common cosmetic problem after pterional craniotomy is the presence of depressed deformities in the frontotemporal area which result from temporal muscle atrophy18,22). Conventional, large frontotemporal craniotomy uses multiple burr holes and needs rongeuring of the temporal squama. Depression of the bone flap or atrophy of the temporalis muscle results in a skin dent in the forehead. Patients sometimes complain of limited ability to open the mouth and pain during chewing resulting from temporal muscle resection, contracture after conventional fronto-temporal craniotomy. Small craniotomy, which is sealed with methyl methacrylate and other bone substitutes, is unlikely to cause cosmetic problems. Preservation of the superficial temporal artery, the frontal branches of the facial nerve, and the supraorbital nerve and artery minimizes the risk of wound healing problems. A short skin incision is later hidden by the eyebrow. Therefore, the postoperative cosmetic results observed in this approach were quite acceptable and, in most patients, were excellent. The length of the surgical procedure and hospitalization were significantly reduced compared with standard techniques.
However, supraorbital keyhole approach cannot be adopted as a standard approach. In our study, the patients with a mass effect on a CT scan were regarded not suitable for a supraorbital craniotomy. As described by Nathal and Gomez-Amador20), this approach has some limitations. In some cases of MCA bifurcation aneurysm, the M1 segment is too long, and the direction of the dome is lateral or caudal to the surgical view from this approach. This type of case requires an extensive amount of dissection, and the surgical view with a working space is limited in a very deep plane. In cases of posterior communicating artery segment aneurysm, the angle of vision is more rostral, and visualization of the neck area of the aneurysm is not good, especially if the dome has a caudal direction. In addition, small craniotomy offers a diminished opportunity for a change of plan if unexpected findings occur during surgery. This drawback can be overcome by the use of special keyhole-adapted microinstruments and of a neuroendoscope8,17,23,24). However, preoperative diagnostic imaging is of paramount importance in this procedure. Each individual patient should be evaluated for the possibility of proximal control, direction of the aneurysm, and application of the aneurysm clip32). Although transient loss of supraorbital sensation and paresis of the eyebrow can occur, this deficit appears to recover during postoperative healing10). Fortunately, in this study, there was no case who suffered from paresis of the eyebrow.
CONCLUSION
The careful choice of an adequate, less invasive surgical approach with minimal brain exploration may result in a significant reduction of traumatization to intracranial structures. In our experience, the limited supraorbital keyhole approach provides adequate visualization and safe surgical manipulation of anterior circulation aneurysms as others reported. The supraorbital keyhole approach improved postoperative results and resulted in shorter hospitalization times, as there was a reduction in the risk of complications, which included chewing discomfort, temporal muscle weakness, scarification, and cosmetic disturbances. The supraorbital keyhole approaches, which are based on improvements in diagnostic imaging, advanced surgical instruments, and microsurgical skills, constitute an effective and ideal craniotomy technique.
References
- 1.Alleyne CH, Jr, Barrow DL, Oyesiku NM. Combined transsphenoidal and pterional craniotomy approach to giant pituitary tumors. Surg Neurol. 2002;57:380–390. doi: 10.1016/s0090-3019(02)00705-x. discussion 390. [DOI] [PubMed] [Google Scholar]
- 2.Al-Mefty O. Supraorbital-pterional approach to skull base lesions. Neurosurgery. 1987;21:474–477. doi: 10.1227/00006123-198710000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Anson JA. Treatment strategies for intracranial fusiform aneurysms. Neurosurg Clin N Am. 1998;9:743. [PubMed] [Google Scholar]
- 4.Arnold H, Herrmann HD. Skull base chordoma with cavernous sinus involvement. Partial or radical tumour-removal? Acta Neurochir (Wien) 1986;83:31–37. doi: 10.1007/BF01420505. [DOI] [PubMed] [Google Scholar]
- 5.Backlund EO. Pterional approach for orbital decompression. Acta Ophthalmol (Copenh) 1968;46:535–540. doi: 10.1111/j.1755-3768.1968.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 6.Carmel PW, Antunes JL, Chang CH. Craniopharyngiomas in children. Neurosurgery. 1982;11:382–389. doi: 10.1227/00006123-198209000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Carrizo A, Basso A. Current surgical treatment for sphenoorbital meningiomas. Surg Neurol. 1998;50:574–578. doi: 10.1016/s0090-3019(97)00101-8. [DOI] [PubMed] [Google Scholar]
- 8.Cohen AR, Perneczky A, Rodziewicz GS, Gingold SI. Endoscope-assisted craniotomy : approach to the rostral brain stem. Neurosurgery. 1995;36:1128–1129. doi: 10.1227/00006123-199506000-00009. discussion 1129-1130. [DOI] [PubMed] [Google Scholar]
- 9.Czirják S, Nyáry I, Futó J, Szeifert GT. Bilateral supraorbital keyhole approach for multiple aneurysms via superciliary skin incisions. Surg Neurol. 2002;57:314–323. doi: 10.1016/s0090-3019(02)00698-5. discussion 323-324. [DOI] [PubMed] [Google Scholar]
- 10.Dare AO, Landi MK, Lopes DK, Grand W. Eyebrow incision for combined orbital osteotomy and supraorbital minicraniotomy : application to aneurysms of the anterior circulation. Technical note. J Neurosurg. 2001;95:714–718. doi: 10.3171/jns.2001.95.4.0714. [DOI] [PubMed] [Google Scholar]
- 11.Day AL. Aneurysms of the ophthalmic segment. A clinical and anatomical analysis. J Neurosurg. 1990;72:677–691. doi: 10.3171/jns.1990.72.5.0677. [DOI] [PubMed] [Google Scholar]
- 12.de Oliveira E, Tedeschi H, Siqueira MG, Ono M, Fretes C, Rhoton AL, Jr, et al. Anatomical and technical aspects of the contralateral approach for multiple aneurysms. Acta Neurochir (Wien) 1996;138:1–11. doi: 10.1007/BF01411716. discussion 11. [DOI] [PubMed] [Google Scholar]
- 13.Grand W, Landi MK, Daré AO. Transorbital keyhole approach to anterior communicating artery aneurysms. Neurosurgery. 2001;49:483–484. doi: 10.1097/00006123-200108000-00058. [DOI] [PubMed] [Google Scholar]
- 14.Hua SE, Gluckman TJ, Batjer HH. Middle cerebral artery occlusion after pterional approach to basilar bifurcation aneurysm : technical case report. Neurosurgery. 1996;39:1050–1053. doi: 10.1097/00006123-199611000-00038. discussion 1053-1054. [DOI] [PubMed] [Google Scholar]
- 15.Jho HD. Orbital roof craniotomy via an eyebrow incision : a simplified anterior skull base approach. Minim Invasive Neurosurg. 1997;40:91–97. doi: 10.1055/s-2008-1053424. [DOI] [PubMed] [Google Scholar]
- 16.Lynch JC, Andrade R. Unilateral pterional approach to bilateral cerebral aneurysms. Surg Neurol. 1993;39:120–127. doi: 10.1016/0090-3019(93)90089-j. [DOI] [PubMed] [Google Scholar]
- 17.Menovsky T, Grotenhuis JA, de Vries J, Bartels RH. Endoscope-assisted supraorbital craniotomy for lesions of the interpeduncular fossa. Neurosurgery. 1999;44:106–110. doi: 10.1097/00006123-199901000-00062. discussion 110-112. [DOI] [PubMed] [Google Scholar]
- 18.Moon SG, Huh SK, Shin MS, Lee KS, Jung N. Supraorbital approach to anterior skull base and intraorbital lesions. J Korean Neurosurg Soc. 1995;24:272–277. [Google Scholar]
- 19.Nagasawa S, Ohta T, Tsuda E. Surgical results and the related topographic anatomy in paraclinoid internal carotid artery aneurysms. Neurol Res. 1996;18:401–408. doi: 10.1080/01616412.1996.11740444. [DOI] [PubMed] [Google Scholar]
- 20.Nathal E, Gomez-Amador JL. Anatomic and surgical basis of the sphenoid ridge keyhole approach for cerebral aneurysms. Neurosurgery. 2005;56(1 Suppl):178–185. doi: 10.1227/01.neu.0000145967.66852.96. discussion 178-185. [DOI] [PubMed] [Google Scholar]
- 21.Paladino J, Pirker N, Stimac D, Stern-Padovan R. Eyebrow keyhole approach in vascular neurosurgery. Minim Invasive Neurosurg. 1998;41:200–203. doi: 10.1055/s-2008-1052042. [DOI] [PubMed] [Google Scholar]
- 22.Park J, Hamm IS. Cortical osteotomy technique for mobilizing the temporal muscle in pterional craniotomies. Technical note. J Neurosurg. 2005;102:174–178. doi: 10.3171/jns.2005.102.1.0174. [DOI] [PubMed] [Google Scholar]
- 23.Perneczky A, Fries G. Endoscope-assisted brain surgery : part 1--evolution, basic concept, and current technique. Neurosurgery. 1998;42:219–224. doi: 10.1097/00006123-199802000-00001. discussion 224-225. [DOI] [PubMed] [Google Scholar]
- 24.Perneczky A, Fries G. Use of a new aneurysm clip with an inverted-spring mechanism to facilitate visual control during clip application. Technical note. J Neurosurg. 1995;82:898–899. doi: 10.3171/jns.1995.82.5.0898. [DOI] [PubMed] [Google Scholar]
- 25.Pritz MB, Chandler WF. The transsylvian approach to middle cerebral artery bifurcation/trifurcation aneurysms. Surg Neurol. 1994;41:217–219. doi: 10.1016/0090-3019(94)90124-4. discussion 219-220. [DOI] [PubMed] [Google Scholar]
- 26.Ramos-Zúñiga R, Velázquez H, Barajas MA, López R, Sánchez E, Trejo S. Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery. 2002;51:125–130. doi: 10.1097/00006123-200207000-00019. discussion 130-131. [DOI] [PubMed] [Google Scholar]
- 27.Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57(4 Suppl):242–255. doi: 10.1227/01.neu.0000178353.42777.2c. discussion 242-255. [DOI] [PubMed] [Google Scholar]
- 28.Reisch R, Perneczky A, Filippi R. Surgical technique of the supraorbital key-hole craniotomy. Surg Neurol. 2003;59:223–227. doi: 10.1016/s0090-3019(02)01037-6. [DOI] [PubMed] [Google Scholar]
- 29.Sánchez-Vázquez MA, Barrera-Calatayud P, Mejia-Villela M, Palma-Silva JF, Juan-Carachure I, Gomez-Aguilar JM, et al. Transciliary subfrontal craniotomy for anterior skull base lesions. Technical note. J Neurosurg. 1999;91:892–896. doi: 10.3171/jns.1999.91.5.0892. [DOI] [PubMed] [Google Scholar]
- 30.Shanno G, Maus M, Bilyk J, Schwartz S, Savino P, Simeone F, et al. Image-guided transorbital roof craniotomy via a suprabrow approach : a surgical series of 72 patients. Neurosurgery. 2001;48:559–567. doi: 10.1097/00006123-200103000-00020. discussion 567-568. [DOI] [PubMed] [Google Scholar]
- 31.Steiger HJ, Schmid-Elsaesser R, Stummer W, Uhl E. Transorbital keyhole approach to anterior communicating artery aneurysms. Neurosurgery. 2001;48:347–351. doi: 10.1097/00006123-200102000-00021. discussion 351-352. [DOI] [PubMed] [Google Scholar]
- 32.van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol. 1998;49:481–489. doi: 10.1016/s0090-3019(96)00539-3. discussion 489-490. [DOI] [PubMed] [Google Scholar]
- 33.Yasargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol. 1975;3:7–14. [PubMed] [Google Scholar]