Abstract
Background
Research on the long-term course of major depressive disorder (MDD) is hindered by the absence of established course criteria and by idiosyncratic definitions of chronicity. The aims of this study were to derive an empirical index of MDD course, to examine its predictive validity, and to identify the adulthood outcomes associated with a chronic course.
Method
Indicators for a MDD course factor were rationally selected and subjected to principal components (PCA) and confirmatory factor analyses (CFA) among 426 subjects with a lifetime history of MDD by age 30. Scores on the index prior to age 19 were examined as predictors of course from age 19 to 30. Associations between the index and outcomes of interest at age 30 were examined.
Results
Three indicators loaded highly on a chronic course index and displayed adequate internal consistency: early onset age, number of episodes, and duration of ill time. Predictive validity of the index was supported. A more chronic course was associated with greater symptom severity, greater likelihood of treatment utilization, and greater psychosocial impairment in multiple domains. Treatment utilization interacted with chronicity to predict relatively few outcomes and did not reduce the negative impact of a chronic course.
Conclusions
The course of MDD through early adulthood is best represented by a composite of early onset age, number of episodes, and duration of ill time. A chronic course through early adulthood is associated with numerous indicators of psychosocial impairment. Mental health treatment utilization in a naturalistic setting does not appear to reduce the negative impact of chronic MDD.
Keywords: Chronic, course, depression, early onset, outcomes, recurrence
Introduction
The chronic course of major depressive disorder (MDD) has received much attention, particularly in the past 10–15 years (e.g. Merikangas et al. 1994; Birmaher et al. 2002; Zalsman et al. 2006). Evidence suggests that features related to the course of MDD, including onset age, episode length, and recurrence, overlap considerably and are associated with a positive family history of the disorder (Klein et al. 2002, 2004; Zisook et al. 2004; Mondimore et al. 2006, 2007). Nevertheless, prior research on the long-term course of MDD is limited in at least two ways. First, heterogeneous approaches to operationalizing chronicity and limitations of DSM-IV criteria that address lifetime course have made it difficult to compare findings across investigations (Mondimore et al. 2006, 2007). MDD course specifiers were introduced in the DSM-III-R, and included chronic depressive episode, recurrent episodes, and a ‘partial remission’ specifier. The DSM-IV added a ‘with or without antecedent dysthymia’ specifier and a ‘with or without full inter-episode recovery’ specifier for recurrent episodes. As noted by Klein (in press), the addition of specifiers improved coverage and descriptive validity of MDD course, but also increased the complexity of the classification system, established artificial distinctions between continuous phenomena, and obscured the distinction between chronic and non-chronic courses.
Second, prior research has frequently examined indicators of MDD course in isolation, which fails to capture different manifestations of a chronic course. For example, previous studies of MDD recurrence (e.g. Solomon et al. 2004; Dunn & Goodyer, 2006; Pettit et al. 2006) include individuals who display one manifestation of a chronic course, but may exclude individuals who experience a single, lengthy episode of many years. Conversely, studies that examine MDD duration as the primary outcome (e.g. Spijker et al. 2004) may exclude individuals who experience relatively brief but recurrent episodes.
One solution to the problem of incomplete coverage is to examine multiple course indicators in the same study. Although this approach has been used, it is not without limitation. Simultaneous examination of multiple course indicators neglects the substantial overlap between indicators and may produce biased results. As an example, parental history of MDD has been found to predict both MDD recurrence and MDD duration in offspring (Rohde et al. 2005). Given the relationship between recurrence and duration, however, it is unclear whether the predictive effects of parental MDD are unique to either course indicator or whether they are an artifact of overlap in group membership (i.e. a subgroup of individuals who have both recurrence and lengthy duration). Moreover, the stability, utility, and etiological relevance of different indicators have been questioned, and cogent arguments have been made for collapsing them into a single dimension (McCullough et al. 2003; Klein et al. 2004, in press).
What is needed, therefore, is a systematic approach to measuring MDD course that provides adequate coverage of the construct and takes into account the overlap between indicators of the construct. Mondimore et al. (2006) used a rational approach to address this need and defined chronicity as (a) early onset MDD, (b) either at least two lifetime episodes or a single episode of at least 3 years' duration, and (c) substantial mood symptoms most or all of the time. That definition provides comprehensive coverage and integration of course indicators but is limited by the absence of an empirical basis and the dichotomization of what is probably a dimensional phenomenon. The primary purpose of this study, consistent with the recommendation of Klein (in press) and the spirit of Mondimore et al. (2006), was to develop an empirical index of MDD course comprising a unified set of indicators. Given previous findings that features reflecting the course of MDD overlap, we sought to determine whether a single factor or factors may provide a more parsimonious representation of MDD course. If evidence for such a factor is obtained, it might provide the basis for a chronic depression phenotype. Importantly, the use of quantitative procedures to develop an index is likely to lead to a more reliable characterization of MDD course. After developing an empirical index of MDD course, a second aim of this investigation was to examine the predictive validity of the index. If the index provides an adequate characterization of a chronic course, then earlier scores (e.g. through adolescence) should predict subsequent course (e.g. through early adulthood).
A final aim of this study was to identify the outcomes associated with a chronic course at age 30. Prior research suggests that chronic courses of depression are accompanied by psychosocial impairment in multiple domains, including economic standing, occupational performance, physical health status, social adjustment, and greater health-care costs (e.g. Hays et al. 1997; Berndt et al. 2000; Judd et al. 2000; Crown et al. 2002; Gilmer et al. 2005). Past research also indicates that the prevalence rates of co-morbid psychiatric disorders are higher among individuals with protracted courses of depression (e.g. Markowitz et al. 1992; Hasin et al. 1996; Garyfallos et al. 1999; Crown et al. 2002; Shankman & Klein, 2002; Gilmer et al. 2005; Dalrymple & Zimmerman, 2007). However, such findings are limited by the absence of a systematic approach to measuring course (Mondimore et al. 2006, 2007). The present study aimed to address that limitation by using an empirically derived index of MDD course and examining its adulthood correlates. Outcomes investigated included status variables, co-morbid psychiatric disorders, severity of MDD, and numerous indicators of psychosocial functioning. Based on prior research (e.g. Markowitz et al. 1992; Berndt et al. 2000; McCullough et al. 2003), we anticipated that a more chronic MDD course would be associated with lower income, a higher number of episodes of co-morbid disorders, more severe depressive symptoms, and poorer interpersonal functioning in early adulthood.
We also examined mental health treatment utilization as a potential correlate of MDD course, and whether treatment utilization moderated the impact of MDD course on outcomes of interest. Understanding the outcomes associated with a chronic course in young adulthood, as well as the potential impact of treatment utilization on such outcomes, may alert clinicians to problem areas in need of additional assessment and intervention.
Method
Sampling strategy
Probands
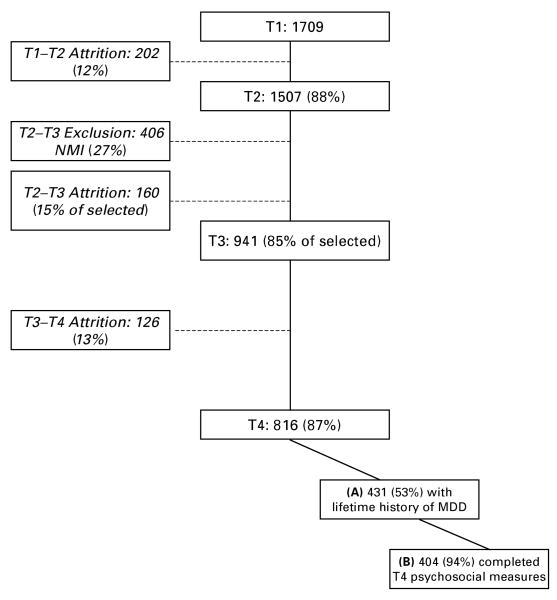
A diagram of the assessment points, sample size, and attrition rates is displayed in Fig. 1. Oregon Adolescent Depression Project (OADP) probands were randomly selected from nine high schools in western Oregon. A total of 1709 adolescents (mean=16.6, s.d.=1.2) completed an initial (T1) assessment. Approximately 1 year later, 1507 (88%) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined to participate or dropped out of the study before T2, were small (Lewinsohn et al. 1993).
Fig. 1.
Sample selection and participation at each assessment point.
At age 24, all probands with a history of MDD (n=360), or a history of non-mood disorders (n=284) by T2, and a random sample with no history of psychiatric disorder (n=457) were invited to participate in a third (T3) evaluation. Of the 1101 T2 participants selected for a T3 interview, 941 (85%) completed the age-24 evaluation. The T2 diagnostic groups did not differ on the rate of participation at T3.
At age 30, all T3 participants were invited to participate in a T4 evaluation. Of the 941 T3 participants, 816 (87%) completed the T4 diagnostic interview. The 816 T4 participants included 484 (59%) women. Among those invited to T3 and T4 assessments, women were more likely than men to complete evaluations (χ2 >5.99, p's <0.05); participation did not differ as a function of other demographic variables or previous diagnoses.
Parents
Lifetime psychiatric disorders in the biological parents of probands were assessed near the time of the T3 evaluation. When parents could not be interviewed directly, informant data were obtained from the probands and, if possible, from a second informant. Diagnostic information on at least one parent was available for 730 probands (89.5%).
Diagnostic interviews
At T1, probands were interviewed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Orvaschel et al. 1982), which included additional items to derive DSM-III-R diagnoses. At the following assessment waves, probands were interviewed using the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al. 1987), which elicited detailed information about the onset and course of psychiatric disorders since the previous evaluation. Diagnostic interviews were supplemented with the Hamilton Depression Rating Scale (HAMD; Hamilton, 1960) to rate the severity of current and worst point depressive symptoms. Proband interviews at T3 and T4 and interviews with relatives were conducted by telephone, which generally yields comparable results to face-to-face interviews (Sobin et al. 1993; Rohde et al. 1997). Independent review of randomly selected T1 cases revealed excellent inter-rater reliability for MDD diagnosis, onset age, number of episodes, and duration (κ and intra-class correlation coefficients >0.85).
If probands met criteria for a disorder at any interview, information was obtained regarding mental health treatment utilization, which was dichotomously scored and defined as receiving psychotherapy, medications, or hospitalization for the disorder. An overlapping dichotomous variable was created to reflect the presence versus absence of medication treatment.
At the time of the T4 assessment, probands were asked to complete a mailed questionnaire that elicited demographic information and included a number of measures with established reliability and validity (described in greater detail in previous publications; Andrews et al. 1993; Lewinsohn et al. 1994): Coping (Parker & Brown, 1979; Folkman & Lazarus, 1980); Daily Hassles (Unpleasant Events Schedule; Lewinsohn et al. 1985); Depressive Symptoms (Center for Epidemiological Studies Depression Scale, CES-D; Radloff, 1977); Major Life Events (Holmes & Rahe, 1967; Sandler & Block, 1979); Optimism (Life Orientation Test – Revised; Scheier et al. 1994); Perceived Social Support from Family and Friends (Procidano & Heller, 1983); Self-Esteem (Rosenberg, 1965); the Social Adjustment Scale (Weissman & Bothwell, 1976); and Social Competence (Lewinsohn et al. 1980; Harter, 1982).
Selection of sample for the current report
Probands who completed T4, met criteria for at least one lifetime MDD episode, and had data available from at least one parent were selected for the current report (n=431; box A in Fig. 1). Five probands were subsequently deemed to be outliers and excluded (to be described later). Characteristics of the remaining 426 are listed in Table 1. At T4, the majority of the sample was female, married, and had at least some college education. Mean MDD onset age was 18 years, mean number of episodes was two, and mean total MDD ill time was just over 1 year. Approximately half had experienced at least one substance use disorder episode, slightly more than one-third had experienced at least one anxiety disorder episode, and less than 10% had experienced dysthymia. Over 40% had received some form of mental health treatment, including 26% who had received psychotropic medications. Although the entire sample had a lifetime history of MDD, few met current diagnostic criteria at T4 and mean HAMD and CES-D scores were in the mild range.
Table 1. Descriptives on status and psychiatric variables assessed at T4.
| Status variables | |
| Female sex, n (%) | 303 (71.1) |
| Education, n (%) | |
| High school or less | 60 (14.0) |
| Some college | 181 (42.5) |
| College or professional | 184 (43.2) |
| Income, n (%) | |
| <US$20000 | 75 (17.6) |
| US$20000–29999 | 74 (17.4) |
| US$30000–39999 | 65 (15.3) |
| US$40000–49999 | 49 (11.5) |
| ≥ US$50000 | 138 (32.4) |
| Marital status, n (%) | |
| Married | 235 (55.2) |
| Not married | 191 (44.8) |
| Psychiatric variables | |
| Presence of current MDD, n (%) | 29 (6.8) |
| Lifetime presence of DSM-IV chronic MDD, n (%) | 51 (11.9) |
| Lifetime number of minor depression episodes, n (%) | |
| 1 | 57 (13.4) |
| >1 | 15 (3.5) |
| Lifetime number of ANX episodes, n (%) | |
| 1 | 95 (22.3) |
| >1 | 37 (12.9) |
| Lifetime number of DYSTH episodes, n (%) | |
| 1 | 34 (8.0) |
| Lifetime number of SBS episodes, n (%) | |
| 1 | 90 (21.1) |
| >1 | 112 (29.7) |
| History of any treatment, n (%) | 183 (43.0) |
| History of medication, n (%) | 111 (26.1) |
| Positive history of suicide attempt, n (%) | 18 (4.2) |
| Lifetime presence of parental MDD, n (%) | 228 (53.5) |
| MDD onset age in years, mean (s.d.) | 18.6 (5.3) |
| Number of MDD episodes, mean (s.d.) | 2.1 (1.3) |
| Total MDD duration in weeks, mean (s.d.) | 60.0 (97.8) |
| HAMD – Worst, mean (s.d.) | 8.4 (8.4) |
| HAMD – Current, mean (s.d.) | 2.4 (5.3) |
| Current CES-Da, mean (s.d.) | 12.8 (10.5) |
MDD, Major depressive disorder; ANX, anxiety disorder; DYSTH, dysthymic disorder; SBS, substance use disorder; HAMD, Hamilton Depression Rating Scale; CES-D, Center for Epidemiological Studies Depression Scale; S.D., standard deviation.
Total n=426.
n=404.
Statistical analyses were performed with the sample displayed in box A of Fig. 1. Analyses that included T4 psychosocial outcomes were performed with the sample displayed in box B.
Results
Development of a chronic course index
Possible indicators for a chronic course index during T4 were rationally selected based on prior research and included duration of MDD ill time, number of MDD episodes, MDD first-onset age, duration of minor depression ill time, number of minor depressive episodes, and lifetime history of dysthymia. Preliminary analysis revealed five univariate outliers on measured variables [i.e. z scores outside of ±3 standard deviations from the mean; Cohen & Cohen (1983), p. 128]; these five cases were excluded from analyses. Additional analysis revealed substantial skew and kurtosis for duration and number of episodes of MDD and minor depression respectively. Log-based and square root transformations were performed to bring skew and kurtosis within acceptable ranges.
Approximately 50% of the 426 probands with a lifetime history of MDD by T4 were randomly selected and scores on these five variables were subjected to a PCA with varimax rotation within this subsample. The results suggested a two-component solution in which MDD duration, MDD number of episodes, and MDD onset age each loaded (>0.70) on one component, and minor depression duration and minor depression number of episodes loaded (>0.90) on a second component. Dysthymia did not load on either component (highest loading=0.28). Given preliminary evidence that the three MDD indicators loaded on one component, the PCA was repeated including only MDD duration, number of MDD episodes, and MDD onset age. Each of the three variables loaded on one component (eigenvalue=1.95) that accounted for 64.97% of the variance. Component loadings were as follows: number of MDD episodes (0.84); MDD duration (0.85); and MDD onset age (0.73). Internal consistency of the three items was adequate (standardized α=0.73).
Based on the results of the PCA, a CFA was used to test model fit in the other half of the sample. A one-factor model was specified with each of the three indicators loading onto the factor. The model provided an adequate-good fit [root mean square error of approximation (RMSEA)=0.07, comparative fit index (CFI)=0.99, Tucker–Lewis fit index (TLI)=0.97]. The standardized loadings of the indicators on the latent factor were as follows: number of MDD episodes (0.85); MDD duration (0.59); MDD onset age (0.48).
The results from the PCA and CFA therefore support the presence of a unidimensional MDD course factor characterized by early onset age, lengthy duration, and recurrent episodes. A unit-weighted factor index was created from the three indicators (a regression-weighted factor score was also created and examined in analyses; the results were almost identical with both approaches). Median scores on the indicators for each quartile of the index are presented in Table 2. For clinical utility, we also list median scores on duration of the longest episode. As is evident in the table, the bottom three quartiles reflect a non-chronic MDD course, with median onset ages over 17 years, median number of episodes <2, and median total duration <9 months (and longest single episode <6 months). Conversely, the top quartile displays evidence of a chronic course, with median onset under age 15, median number of episodes at 4, and median total duration of almost 2 years (longest single episode >1 year). Based on these results, the shared presence of the following index criteria reflects a ‘definite’ chronic course: (a) onset by age 16 years; (b) >3 episodes; and (c) total duration >1 year. Using those criteria, 47 (11.0%) of our depressed sample would be considered to have a definite chronic course. In recognition of the heterogeneity of MDD, a relaxation to two of three index criteria would allow for a designation of a ‘probable’ chronic course up to age 30. Using this decision rule, an additional 77 (18.1%) of our depressed sample would be considered to have a probable chronic course.
Table 2. Median scores by quartile on indicators of the chronic course index.
| Indicator | First quartile (n=107) | Second quartile (n=106) | Third quartile (n=107) | Fourth quartile (n=106) |
|---|---|---|---|---|
| Onset age (years) | 24.25 | 19.25 | 17.33 | 14.91 |
| Number of episodes | 1.0 | 1.0 | 2.0 | 4.0 |
| Total duration (weeks) | 4.0 | 14.00 | 34.00 | 97.00 |
| Longest episode (weeks) | 4.0 | 13.00 | 22.00 | 58.50 |
Total n=426.
Predictive validity of the index
To test the predictive validity of the chronic course index, we examined the prospective associations between the index score in adolescence and subsequent course indicators in adulthood. An adolescent course index score was computed based on the three indicators up to age 18 years for the 248 (58.2%) probands with a lifetime history of MDD by that age. A regression equation was then constructed in which the adolescent course score predicted a composite score of MDD duration plus number of episodes from ages 19–30 (onset age could not be included as an outcome because it would create a dependency between predictor and outcome scores). In support of the predictive validity of the index, adolescent scores significantly predicted greater MDD duration and number of episodes during the 11-year interval from age 19 to age 30 [F(1, 247)=13.51, B=0.25, s.e.=0.07, p<0.001].
Adult outcomes associated with a chronic course of MDD
Frequencies and mean scores on outcome variables at T4 are presented in Tables 1 and 3 respectively. Consistent with the mean mild depressive symptom scores discussed above, measures of psychosocial functioning indicated minor levels of impairment on average (Table 3).
Table 3. Descriptives on psychosocial variables assessed at T4.
| Psychosocial variables | Mean | s.d. |
|---|---|---|
| Coping | 48.1 | 7.13 |
| Daily hassles | 44.4 | 11.56 |
| Family support | 9.1 | 1.99 |
| Friend support | 9.2 | 1.91 |
| Major events | 3.4 | 2.97 |
| Optimism | 15.5 | 4.07 |
| Self-esteem | 31.9 | 5.66 |
| Social competence | 14.2 | 4.41 |
| SAS Work | 1.9 | 0.54 |
| SAS Social/leisure | 1.9 | 0.49 |
| SAS Family relations | 1.8 | 0.65 |
SAS, Social Adjustment Scale; s.d., standard deviation.
Total n=404.
Status and psychiatric correlates of a chronic course
Univariate associations between the index and outcome variables of interest at T4 are displayed in Table 4 (see unadjusted estimates). Higher index scores corresponded to a decreased likelihood of being married and lower household income. The association between MDD course and lower household income remained significant while controlling for marital status (B=−0.13, s.e.=0.06, p<0.05), but the reverse was not true (B=−0.27, s.e.=0.26, p=n.s.). MDD course was not associated with educational attainment.
Table 4. Associations between chronic course index scores, T4 status variables, T4 psychiatric outcomes, and T4 psychosocial functioning.
| T4 outcomes | Unadjusted B (s.e.) | AdjustedaB (s.e.) |
|---|---|---|
| Status variables | ||
| Education | 0.02 (0.07) | 0.03 (0.07) |
| Household income | −0.15 (0.06)** | −0.15 (0.06)* |
| Marital status | −0.48 (0.23)* | −0.50 (0.22)* |
| Psychiatric | ||
| ANX episodes | 0.60 (0.11)*** | 0.57 (0.11)*** |
| ANX duration | 0.002 (0.001)*** | 0.002 (0.001)** |
| DYSTH episodes | 1.14 (0.41)** | 1.08 (0.41)** |
| DYSTH duration | 0.002 (0.001) | 0.002 (0.001) |
| SBS episodes | 0.24 (0.05)*** | 0.23 (0.05)*** |
| SBS duration | 0.001 (0.001) | 0.001 (0.001) |
| Suicide attempt | 0.008 (0.02) | 0.008 (0.02) |
| HAMD | ||
| Worst | 0.06 (0.01)*** | 0.06 (0.01)*** |
| Current | 0.09 (0.02)*** | 0.11 (0.03)*** |
| Current CES-Dc | 0.03 (0.01)** | 0.02 (0.01)* |
| Current MDD | 1.11 (0.44)* | – |
| Parental MDD | 0.74 (0.22)*** | 0.73 (0.22)*** |
| Parental onset age | 0.001 (0.001) | 0.001 (0.001) |
| Parental recurrent MDDb | 0.45 (0.32) | 0.38 (0.31) |
| Psychosocialc | ||
| Coping | −0.06 (0.02)*** | −0.05 (0.02)** |
| Daily hassles | 0.02 (0.01) | 0.02 (0.01) |
| Family support | −0.20 (0.06)*** | −0.19 (0.06)** |
| Friend support | −0.03 (0.06) | −0.03 (0.06) |
| Major events | 0.11 (0.04)** | 0.11 (0.04)** |
| Optimism | −0.12 (0.03)*** | −0.11 (0.03)*** |
| Self-esteem | −0.07 (0.02)*** | 0.06 (0.02)** |
| Social competence | 0.06 (0.03)* | 0.05 (0.03) |
| SAS Work | 0.83 (0.22)*** | 0.79 (0.22)*** |
| SAS Social/leisure | 0.44 (0.23) | 0.35 (0.24) |
| SAS Family relations | 0.95 (0.28)*** | 0.90 (0.29)** |
ANX, Anxiety disorder; DYSTH, dysthymic disorder; SBS, substance use disorder; HAMD, Hamilton Depression Rating Scale; CES-D, Center for Epidemiological Studies Depression Scale; MDD, major depressive disorder; SAS, Social Adjustment Scale; s.e., standard error.
Total n=426.
Adjusted for T4 current MDD.
n=227;
n=404.
p<0.001,
p<0.01,
p<0.05.
With regard to psychiatric disorders, a more chronic MDD course was associated with a higher number of lifetime episodes of substance use disorders, anxiety disorders, and dysthymic disorder. Among probands with at least one episode of co-morbid psychiatric disorders, we examined the association between the index and the total lifetime duration of the respective disorder. MDD course was significantly associated with a longer duration of anxiety disorders but not substance use disorders or dysthymia. The index was also associated with the severity of worst-point major depressive episodes and current T4 MDD and depressive symptoms. When examined by quartile on the course index, the prevalence rate of current T4 MDD was 6.5% for the bottom quartile, 2.3% for the second quartile, 3.7% for the third quartile, and 14.2% for the upper quartile. MDD course was not associated with a history of suicide attempt.
Given the possibility that current depression at T4 may have biased responses, analyses were repeated controlling for current MDD (see adjusted estimates in Table 4). As displayed in the adjusted estimates in Table 4, all significant univariate associations were robust to controlling for current MDD. We repeated analyses controlling for T4 CES-D scores rather than current MDD; no outcome differed in terms of statistical significance.
Psychosocial correlates of a chronic course
Univariate associations between the index and psychosocial variables assessed at T4 are displayed in the lower section of Table 4 (unadjusted estimates). MDD course was associated with an array of psychosocial variables indicative of poorer general functioning. When controlling for T4 current MDD (see adjusted estimates in Table 4), all significant univariate associations remained significant except for social competence [B=0.05, s.e.=0.03, p>0.10]. Over and above the effects of current depressive symptoms, probands with a more chronic course endorsed more impaired family social support and familial relationships, more impaired work functioning, a higher number of major life events, and poorer coping, optimism, and self-esteem. By contrast, daily hassles and friend social support did not differ as a function of MDD course. Once again, we repeated analyses controlling for T4 CES-D scores rather than current MDD and no outcome changed meaningfully.
Relationship between mental health treatment utilization and MDD course
Individuals with a more chronic course were more likely to have received mental health treatment for MDD by T4 (B=1.38, s.e.=0.22, p<0.001), including psychotropic medication (B=1.29, s.e.=0.25, p< 0.001). To determine whether MDD course was associated uniquely with treatment utilization, we examined the association between course and treatment while controlling for worst-point MDD severity and all co-morbid psychiatric disorders. MDD course continued to be associated with treatment utilization after controls (p's<0.001).
We next sought to determine whether mental health treatment utilization moderated the impact of MDD course on T4 psychiatric and psychosocial outcomes. Regression analyses were run with course scores, history of any treatment and their interaction term as predictors. T4 outcomes were placed as dependent variables. Treatment utilization did not moderate the associations between MDD course and status variables, worst-point severity, or number or duration of substance use or dysthymic episodes. Treatment did, however, moderate the association between course and the number of anxiety episodes from T1 to T4, such that course was significantly and positively associated with the number of anxiety episodes among those who received treatment (n=182; B=0.14, s.e.=0.03, p<0.001) but not among those who did not receive treatment (n=232; B=−0.04, s.e.=0.17, p=n.s.). Treatment utilization also moderated the links between course and current HAMD scores and multiple psychosocial variables at T4, including coping skills, social skills, self-esteem, and optimism. The nature of these interactions was such that course significantly predicted poorer functioning among those who received treatment (all p's<0.01) but not among those who did not receive treatment (all p's >0.10). None of these associations changed meaningfully when controlling for current MDD or worst-point severity of MDD.
Discussion
A chronic course of MDD in early adulthood is best characterized by a composite index of early onset age, recurrent episodes, and lengthy duration of ill time. The chronic course index provides thorough coverage of MDD course while also reflecting the overlap between course indicators. Predictive validity of the index from adolescence through early adulthood was supported. Based on these findings, the index may provide the basis for a systematic approach to operationalizing MDD course and assisting in integrating findings across future investigations.
MDD recurrence and duration have been examined frequently as indicators of a chronic course. The present findings suggest that early onset represents another integral feature of chronicity. It should be noted that an earlier onset allows for a greater amount of time in which recurrences or lengthy episodes may occur. Nevertheless, the long prospective follow-up of this study (approximately 15 years) lends support to the notion that early onset is indeed a feature of a chronic course, not simply an artifact of a short follow-up.
It is somewhat surprising that dysthymia and minor depression course indicators did not load on the course factor. This may have resulted in part from the relatively low lifetime prevalence rates of dysthymia (8.0%) and minor depression (16.9%), or perhaps because we restricted our sample to probands with a positive lifetime history of MDD. Alternatively, it may suggest that the presence and/or course of less severe manifestations of depression are unrelated to the course of syndromal MDD, at least in early adulthood. It is also possible that they may be more strongly linked to MDD course among individuals with a later onset or as depressed individuals progress through adulthood.
Using the three course indicators in our sample, recommended criteria for ‘definite’ and ‘probable’ chronic courses of MDD up to age 30 were presented. Of note, our empirical, bottom-up approach to developing an index led to similar designations as others' rational, top-down approach. Our definition of a probable chronic MDD course roughly corresponds to the subtype described in the Genetics of Recurrent Early Onset Depression project (GenRED; Mondimore et al. 2006), in that individuals display early onset and either recurrent episodes or a single lengthy episode. Moreover, the prevalence (29%) of definite or probable chronic depression in the present sample was similar to the prevalence (35%) of the early onset recurrent subtype in GenRED. We encourage future research to cross-validate indicators of the chronic course index and to explore whether the suggested criteria are appropriate in diverse samples. It may be that the three indicators consistently reflect a chronic course, but that the suggested cut-points need to be modified based on sample-specific characteristics (e.g. raising onset age criterion for depressed older adults).
An additional aim of the present study was to identify early adulthood outcomes associated with of a chronic course of MDD while addressing course measurement limitations of prior studies. The findings suggest that, among individuals with a positive history of MDD, a chronic course predicts greater impairment in young adulthood in multiple domains. Consistent with past research (e.g. Markowitz et al. 1992; Berndt et al. 2000; Gilmer et al. 2005), individuals with a chronic course were likely to experience depressive episodes of greater severity, more episodes or a longer total duration of co-morbid psychiatric disorders, more severe current depressive symptoms, parental history of MDD, and to have lower incomes. They were also more likely to report impaired relationships with family members, impaired work performance, poorer coping skills, negative cognitive styles such as low optimism and low self-esteem, and to experience a higher number of stressful life events.
It is unsurprising that individuals with a chronic MDD course were more likely to undergo treatment. The findings of an association with treatment utilization, even controlling for greater MDD severity and co-morbid psychiatric disorders, suggest that the course of MDD contributed uniquely to individuals' decisions to seek treatment. Even among those who sought treatment, however, a chronic course continued to predict poorer functioning. It is likely that basic treatment approaches will not suffice for individuals with chronic MDD courses. Intensive, evidence-based approaches specifically tailored for chronic MDD (e.g. Keller et al. 2000; Schatzberg et al. 2005) may hold more promise in reducing its course and attendant psychosocial impairments. Given the overlap between MDD course and substance use disorder episodes and anxiety disorder duration respectively, treatment providers may also assess and intervene for these co-occurring disorders (Watkins et al. 2006; Zimmerman et al. 2006).
The strengths of this study include the prospective, longitudinal design with repeated assessments over approximately 15 years, the large sample of depressed persons, and the application of empirical procedures to developing an internally consistent course index. Despite these strengths, several limitations deserve mention. First, probands were oversampled on the basis of early onset depression and were only 30 years old at the final assessment point. These methodological aspects restrict our findings to relatively early onset MDD chronicity. Many probands will be likely to experience future, possibly lengthy episodes. It is unclear whether the features and outcomes of MDD course up to age 30 remain the same through adulthood. Second, data were not available on the course of subthreshold, inter-episode or residual depressive symptoms, as were included in a previous measure of chronicity (Mondimore et al. 2006). As such, the chronic course index is limited to syndromal MDD. Consideration of other course features in the refinement of the empirical index represents a worthwhile endeavor for future research. Third, retrospective bias in reporting the number and duration of episodes between assessment waves is a concern given the 6-year intervals from T2 to T3 and T3 to T4. Fourth, we separately examined number of episodes and duration of co-morbid psychiatric disorders, rather than creating empirical indices of the chronicity of those disorders. Fifth, limited data were available regarding the modalities, timing, and duration of mental health treatment utilization. This prevents conclusions regarding the efficacy of treatment in modifying the impact of chronic MDD, but does present a naturalistic view of mental health treatment utilization in a community setting. Additional research with older samples and with more detailed information on treatment utilization is encouraged.
In summary, this report has provided the empirical basis for an index of the long-term course of MDD. Using the index, a more chronic course up to early adulthood is associated with outcomes such as more severe and co-morbid psychopathology, parental MDD history, and psychosocial impairment. In addition to refining understanding of the phenomenology and outcomes of a chronic course, we hope the index will provide a common metric for research on the long-term course of MDD.
Acknowledgments
This research was supported by NIMH awards MH40501, MH50522 and MH52858 to P.M.L. and MH75744 to J.W.P.
Footnotes
Declaration of Interest: None.
References
- Andrews JA, Lewinsohn PM, Hops H, Roberts RE. Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychological Reports. 1993;73:1019–1046. doi: 10.2466/pr0.1993.73.3.1019. [DOI] [PubMed] [Google Scholar]
- Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Kornstein SG, Miller IM, Thase ME, Trapp GA, Keller MB. Lost human capital from early-onset chronic depression. American Journal of Psychiatry. 2000;157:940–947. doi: 10.1176/appi.ajp.157.6.940. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child and Adolescent Psychiatric Clinics of North America. 2002;11:619–637. doi: 10.1016/s1056-4993(02)00011-1. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 2nd. Lawrence Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Crown W, Finkelstein S, Brendt E, Ling D, Poret AW, Rush J, Russell JM. The impact of treatment-resistant depression in health care utilization and costs. Journal of Clinical Psychiatry. 2002;63:963–971. doi: 10.4088/jcp.v63n1102. [DOI] [PubMed] [Google Scholar]
- Dalrymple KL, Zimmerman M. Does comorbid social anxiety disorder impact the clinical presentation of principal major depressive disorder? Journal of Affective Disorders. 2007;100:241–247. doi: 10.1016/j.jad.2006.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn V, Goodyer IM. Longitudinal investigation into childhood and adolescent onset depression: psychiatric outcome in early adulthood. British Journal of Psychiatry. 2006;188:216–222. doi: 10.1192/bjp.188.3.216. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21:219–239. [PubMed] [Google Scholar]
- Garyfallos G, Adamopoulou A, Karastergiou A, Voikli M, Sotiropoulou A, Donias S, Giouzepas J, Paraschos A. Personality disorders in dysthymia and major depression. Acta Psychiatrica Scandinavica. 1999;99:332–340. doi: 10.1111/j.1600-0447.1999.tb07238.x. [DOI] [PubMed] [Google Scholar]
- Gilmer WS, Trivedi MH, Rush AJ, Wisniewski SR, Luther J, Howland RH, Yohanna D, Khan A, Alpert J. Factors associated with chronic depressive episodes: a preliminary report from the STAR*D project. Acta Psychiatrica Scandinavica. 2005;112:425–433. doi: 10.1111/j.1600-0447.2005.00633.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgery. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harter S. The Perceived Competence Scale for Children. Child Development. 1982;53:87–97. [PubMed] [Google Scholar]
- Hasin DS, Tsai WY, Endicott J, Mueller TI, Coryell W, Keller M. Five-year course of major depression: effects of comorbid alcoholism. Journal of Affective Disorders. 1996;41:63–70. doi: 10.1016/0165-0327(96)00068-7. [DOI] [PubMed] [Google Scholar]
- Hays JC, Krishnan KR, George LK, Pieper CF, Flint EP, Blazer DG. Psychosocial and physical correlates of chronic depression. Psychiatry Research. 1997;72:149–159. doi: 10.1016/s0165-1781(97)00105-4. [DOI] [PubMed] [Google Scholar]
- Holmes TH, Rahe RH. The social readjustment rating scale. Journal of Psychosomatic Research. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ, Paulus M, Leon AC, Maser JD, Endicott J, Corvell W, Kunovac JL, Mueller TI, Rice JP, Keller MB. Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow BL, Duner DL, Gelenberg AJ, Markowitz JC, Nemeroff CB, Russell JM, Thase ME, Trivedi MH, Zajecka J. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Klein DN. Classification of depressive disorders in DSM-V: proposal for a two-dimension system. Journal of Abnormal Psychology. doi: 10.1037/0021-843X.117.3.552. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Durbin CE. Clinical features of major depressive disorder in adolescents and their relatives: impact on familial aggregation, implications for phenotype definition and specificity of transmission. Journal of Abnormal Psychology. 2002;111:98–106. [PubMed] [Google Scholar]
- Klein DN, Shankman AS, Lewinsohn PM, Rohde P, Seeley JR. Family study of chronic depression in a community sample of young adults. American Journal of Psychiatry. 2004;161:646–653. doi: 10.1176/appi.ajp.161.4.646. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Mermelstein RM, Alexander C, MacPhillamy D. The Unpleasant Events Schedule: a scale for the measurement of aversive events. Journal of Clinical Psychology. 1985;41:483–498. doi: 10.1002/1097-4679(198507)41:4<483::aid-jclp2270410407>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Mischel W, Chaplin W, Barton R. Social competence and depression: the role of illusory self-perceptions. Journal of Abnormal Psychology. 1980;89:203–212. doi: 10.1037//0021-843x.89.2.203. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Moran ME, Kocsis JH, Frances AJ. Prevalence and comorbidity of dysthymic disorder. Journal of Affective Disorders. 1992;24:63–71. doi: 10.1016/0165-0327(92)90020-7. [DOI] [PubMed] [Google Scholar]
- McCullough JP, Klein DN, Borian FE, Howland RH, Riso LP, Keller MB, Banks PLC. Group comparisons of DSM–IV subtypes of chronic depression: validity of the distinctions, Part 2. Journal of Abnormal Psychology. 2003;112:614–622. doi: 10.1037/0021-843X.112.4.614. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Wicki W, Angst J. Heterogeneity of depression. Classification of depressive subtypes by longitudinal course. British Journal of Psychiatry. 1994;164:342–348. doi: 10.1192/bjp.164.3.342. [DOI] [PubMed] [Google Scholar]
- Mondimore FM, Zandi PP, MacKinnon DF, McInnis MG, Miller EB, Crowe RP, Scheftner WA, Marta DH, Weissman MM, Levinson DF, Murphy-Ebenez KP, DePaulo JR, Potash JB. Familial aggregation of illness chronicity in recurrent, early-onset major depression pedigrees. American Journal of Psychiatry. 2006;163:1554–1560. doi: 10.1176/ajp.2006.163.9.1554. [DOI] [PubMed] [Google Scholar]
- Mondimore FM, Zandi PP, MacKinnon DF, McInnis MG, Miller EB, Schweizer B, Crowe RP, Scheftner WA, Weissman MM, Levinson DF, DePaulo JR, Potash JB. A comparison of the familiality of chronic depression in recurrent early-onset depression pedigrees using different definitions of chronicity. Journal of Affective Disorders. 2007;100:171–177. doi: 10.1016/j.jad.2006.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MR, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child and Adolescent Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Parker GB, Brown LB. Repertoires of response to potential precipitants of depression. Australian and New Zealand Journal of Psychiatry. 1979;13:327–333. doi: 10.3109/00048677909159155. [DOI] [PubMed] [Google Scholar]
- Pettit JW, Lewinsohn PM, Joiner TE., Jr Propagation of major depressive disorder: relationship between first episode symptoms and recurrence. Psychiatry Research. 2006;141:271–278. doi: 10.1016/j.psychres.2005.07.022. [DOI] [PubMed] [Google Scholar]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. American Journal of Community Psychology. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR. Association of parental depression with psychiatric course from adolescence to young adulthood among formerly depressed individuals. Journal of Abnormal Psychology. 2005;114:409–420. doi: 10.1037/0021-843X.114.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews assessing Axis I and II disorders. American Journal of Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the Adolescent Self-Image. Princeton University Press; Princeton, NJ: 1965. [Google Scholar]
- Sandler IN, Block M. Life stress and maladaption of children. American Journal of Community Psychology. 1979;7:425–439. doi: 10.1007/BF00894384. [DOI] [PubMed] [Google Scholar]
- Schatzberg AF, Rush AJ, Arnow BA, Banks PL, Blalock JA, Borian FE, Howland R, Klein DN, Kocsis JH, Kornstein SG, Manber R, Markowitz JC, Miller I, Ninan PT, Rothbaum BO, Thase ME, Trivedi MH, Keller MB. Chronic depression: medication (nefazodone) or psychotherapy (CBASP) is effective when the other is not. Archives of General Psychiatry. 2005;62:513–520. doi: 10.1001/archpsyc.62.5.513. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a re-evaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Shankman S, Klein D. The impact of comorbid anxiety disorders on the course of dysthymic disorder: a 5-year prospective longitudinal study. Journal of Affective Disorders. 2002;70:211–217. doi: 10.1016/s0165-0327(01)00302-0. [DOI] [PubMed] [Google Scholar]
- Sobin E, Weissman MM, Goldstein RB, Adams P, Wickramaratne P, Warner V, Lish JD. Diagnostic interviewing for family studies: comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric disorders. Psychiatric Genetics. 1993;3:227–233. [Google Scholar]
- Solomon DA, Leon AC, Endicott J, Mueller TI, Coryell W, Shea MT, Keller MB. Psychosocial impairment and recurrence of major depression. Comprehensive Psychiatry. 2004;45:423–430. doi: 10.1016/j.comppsych.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Spijker J, De Graaf R, Bijl RV, Beekman ATF, Ormel J, Nolen WA. Determinants of persistence of major depressive episodes in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Journal of Affective Disorders. 2004;81:231–240. doi: 10.1016/j.jad.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Watkins KE, Paddock SM, Zhang L, Wells KB. Improving care for depression in patients with comorbid substance misuse. American Journal of Psychiatry. 2006;163:125–132. doi: 10.1176/appi.ajp.163.1.125. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: an overview. Epidemiology, clinical manifestation and risk factors. Child and Adolescent Psychiatric Clinics of North America. 2006;15:827–841. doi: 10.1016/j.chc.2006.05.002. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, Zisook S, Ginsberg DL. Recognition and treatment of depression with or without comorbid anxiety disorders. Primary Psychiatry. 2006;13:1–13. [Google Scholar]
- Zisook S, Rush AJ, Albala A, Alpert J, Balasubramani GK, Fava M, Husain M, Sackeim H, Trivedi M, Wisniewski S. Factors that differentiate early vs. later onset of major depression disorder. Psychiatry Research. 2004;129:127–140. doi: 10.1016/j.psychres.2004.07.004. [DOI] [PubMed] [Google Scholar]