Abstract
The successful use of transcriptional targeting for cancer therapy depends on the activity of a given promoter inside the malignant cell. Because solid human tumors evolve as a “cross-talk” between the different cell types within the tumor, we hypothesized that targeting the entire tumor mass might have better therapeutic effect. Secreted protein acidic and rich in cysteine (SPARC) is a matricellular protein overexpressed in different human cancers malignant melanomas both in the malignant cells compartment as in the stromal one (fibroblasts and endothelial cells). We have shown that expression of the herpes simplex virus-thymidine kinase (TK) gene driven by the SPARC promoter in combination with ganciclovir inhibited human melanoma cell growth in monolayer as well as in multicellular spheroids. This inhibitory effect was observed both in homotypic spheroids composed of melanoma cells alone as well as in spheroids made of melanoma cells and stromal cells. Expression of the TK gene was also efficient to inhibit the in vivo tumor growth of established melanomas when TK was expressed either by the malignant cells themselves or by coadministered endothelial cells. Our data suggest that the use of therapeutic genes driven by SPARC promoter could be a valuable strategy for cancer therapy aiming to target all the cellular components of the tumor mass.
Introduction
In the past several decades, the incidence of malignant melanoma has increased more than any other cancer. More than 50,000 cases of invasive melanoma (4% of all cancer cases) were diagnosed only in the United States in 2004 (1, 2). Although early, localized disease is effectively treated with wide excision, the metastatic disease is universally fatal (3, 4). Transcriptional targeting consists in the use of tumor-specific gene promoters (TSP) to direct the expression of therapeutic genes specifically to a tumor (5). The effectiveness of this strategy depends on the precise characterization of the tumor-associated gene activity from which the TSP derives. In human melanoma, the tyrosinase enhancer/promoter and the tyrosine and human melanoma inhibitory activity promoters have been used for tissue-specific expression of therapeutic genes (6-8). Additional promoters corresponding to genes expressed in different human cancers, such as the survivin and cyclooxygenase-2, were also used for targeting malignant melanoma cell lines and tumors (9, 10). One of the main features of solid human tumors is their high heterogeneity in terms of cellular composition and gene expression (11). Thus, using a TSP whose activity is restricted only to a subset of malignant cells where the selected TSP is active might allow remaining malignant cells to escape this specific therapy and stromal cells to continue supporting malignant cell growth. Thus, selecting a TSP for cotargeting the tumor and stromal compartments of the tumor mass seems as a plausible strategy for achieving a better therapeutic effect.
Secreted protein acidic and rich in cysteine (SPARC) is a secreted protein involved in cell-extracellular matrix interactions (12). Different groups including ours have shown that SPARC overexpression is associated with increased aggressiveness and worse prognosis of malignant melanoma and other human cancers as well (13-16). SPARC was found to be overexpressed not only in malignant melanoma cells but also in tumor-associated fibroblasts and endothelial cells, whereas moderate or no expression was observed in benign nevi and normal melanocytes, respectively (13). In other human cancers, such as breast, lung, pancreatic adenocarcinoma, and sarcomatoid renal carcinoma, SPARC expression is mainly overexpressed by intermingled fibroblasts and endothelial cells, although in human breast cancer, it is also overexpressed by epithelial cells corresponding to the most aggressive cancer types (17-20). Thus, conditional targeting of cancer cells using the SPARC gene promoter seems as a plausible strategy to target all the cellular components of a tumor mass.
To develop a strategy for cotargeting the different cell components of a tumor mass, we investigated the characteristics and activity of different variants of the human SPARC promoter. We prepared plasmid-based vectors carrying the thymidine kinase (TK) gene driven by two variants of the SPARC promoter and evaluated their efficacy in vitro, in cell culture spheroids, and in vivo after xenograft transplantation in nude mice. For the first time, we show the antitumor efficacy of this type of construct when expressed either by the malignant cells themselves or by neighboring fibroblasts or endothelial cells, suggesting that the use of therapeutic genes driven by SPARC promoter could be a valuable strategy for cancer therapy.
Materials and Methods
Plasmids Construction
A 1.2-kb fragment corresponding to the 5′ region of the human SPARC gene (−1,175 to +71 bp relative to the transcription start site) was amplified from human lymphocyte genomic DNA with SPfse and SPfas primers (Supplementary Table S1).5 This PCR product, hSPPr, was cloned in pGEM-T-easy vector (Promega Corp., Madison, WI) to obtain pGEM-hSPPr. This plasmid was used as a template to obtain the promoter variants −1,175/+28 (using primers SPfse and R28; Supplementary Table S1),5 −120/+28 (using primers F120 and R28; Supplementary Table S1),5 −120/+71 (using primers F120 and Spfas; Supplementary Table S1),5 and hSPPrΔ10. The hSPPrΔ10 promoter variant (1,236 bp) corresponds to the promoter lacking the inter-GGA box region and was generated by a two-step amplification procedure. First, a 1,084-bp fragment upstream to the inter-GGA region was amplified using primers SPse and Δ10r (Supplementary Table S1).5 A second fragment (208 bp) downstream to the inter-GGA region was amplified with primers Δ10f and SPas (Supplementary Table S1).5 Both products were mixed and used as templates for a second PCR round with SPse and SPas primers to obtain the hSPPrΔ10 promoter lacking the 10-bp inter-GGA region. The four promoter variants were cloned in pCR4-TOPO (Invitrogen, Carlsbad, CA) and subcloned in the promoterless firefly luciferase gene reporter vector pGL3-Basic (Promega) to obtain pGL3-hSPPr, pGL3-120/+71, pGL3-120/+28, and pGL3-hSPPrΔ10.
The HSVtk gene was amplified from the plasmid Pago (21) with TKF1 and TKR1 primers (Supplementary Table S1).5 A 1,131-bp fragment was cloned in place of the luciferase gene in pGL3-hSPPr and pGL3-hSPPrΔ10 followed by subcloning of the MluI/BamHI hSPPr-TK and hSPPrΔ10-TK cassettes into the MluI and BamHI sites of pcDNA3.1(+) (Invitrogen) in place of the cytomegalovirus promoter. The final vectors were named phSPPr-TK and phSPPrΔ10-TK. The plasmid pcEGFP was constructed by cloning the EcoRI/NotI enhanced green fluorescent protein (EGFP) entire coding sequence obtained from pEGFP-1 (Clontech, Mountain View, CA) into the EcoRI/NotI sites of pcDNA3.1(+). All the constructs were confirmed by restriction pattern and automatic DNA sequencing (ABI Prism 377 DNA Sequencer, Applied Biosystems, Foster City, CA).
In vivo Studies
Female athymic N:NIH(S)-nu mice (8-10 weeks old; obtained from the animal facility of the Faculty of Veterinary, University of La Plata, La Plata, Argentina) were s.c. injected in both flanks either with 2.5 × 106 malignant cells alone or in combination with a similar amount of bovine aortic endothelial cells (BAEC). When the average tumor volume reached 100 mm3, mice were randomly separated in different cages. The corresponding groups received i.p. administrations of 30 mg/kg body weight of ganciclovir or saline every day during 4 weeks. Tumor volumes were estimated from caliper measurements twice weekly [volume = 0.52 × (width)2 × length]. None of the mice showed signs of wasting or other visible indications of toxicity. Experiments were done following institution guidelines. In vivo external imaging was followed with a Leica (Wetzlar, Germany) Stereo Fluorescence System (model MZFLIII). The animals were kept under ethylic ether anesthesia during this process.
Statistical Analysis
Statistical analyses of luciferase studies, spheroid, and in vivo experiment were determined by ANOVA followed by Tukey’s test or Bonferroni’s multiple comparison test. A P < 0.05 was considered significant.
Results
Transcriptional Activity of Different SPARC Promoter Variants
SPARC expression was examined in different human cell lines by real-time PCR. Compared with A375N, MEL-J-N and MEL-Les melanoma cells expressed moderate and low SPARC mRNA levels, respectively, whereas HeLa cervix carcinoma cells and T-47D breast cancer cells showed negligible SPARC mRNA expression (Table 1). WI-38 fetal fibroblasts and a transformed variant WI-38 VA expressed moderate SPARC mRNA levels, whereas BAEC expressed higher SPARC mRNA levels than A375N melanoma cells (Table 1).
Table 1. Relative expression of SPARC mRNA levels in different malignant and nonmalignant cell lines.
| Cell line | Origin | Relative expression* |
|---|---|---|
| A375N | Melanoma | 100 |
| MEL-J-N | Melanoma | 24.29 ± 7.11 |
| MEL-Les | Melanoma | 7.29 ± 0.70 |
| HeLa | Cervix carcinoma | 0.08 ± 0.02 |
| T-47D | Breast carcinoma | 0.11 ± 0.03 |
| WI-38 | Fibroblast | 18.21 ± 2.68 |
| WI-38 VA | Fibroblast | 12.68 ± 5.05 |
| BAEC | Endothelium | 205.19 ± 12.35 |
Data were obtained by real-time PCR and expressed as the relative expression with respect to the levels observed in the A375N cell line. The numbers correspond to the mean ± SD.
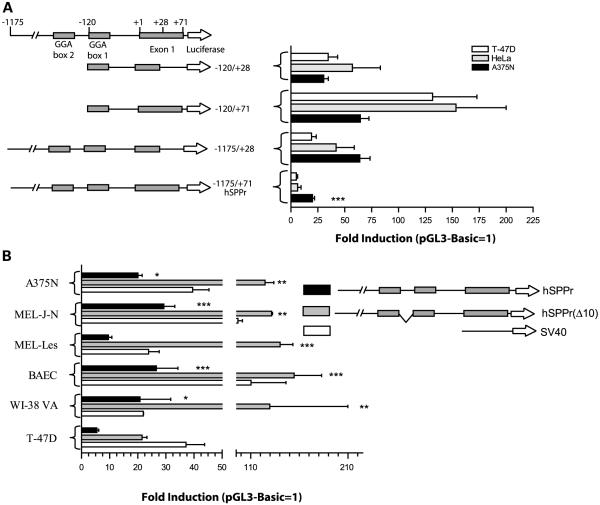
We next assessed the strength and specificity of the different SPARC promoter fragments by comparing their ability with direct the expression of the luciferase reporter gene in the different cell types (Fig. 1). The −1,175 to +71 SPARC promoter fragment (termed hSPPr) includes the entire nontranslated first exon that was shown to contain positive regulatory elements in the bovine SPARC promoter (22). This construct was compared with a variant extending from −1,175 to +28 that was shown to display high activity (23), a shorter variant extending from −120 to +28 that was also shown to drive gene activity (23), and to a variant extending from −120 to +71 that includes the first exon. All the promoter fragments were active in A375N melanoma cells; however, hSPPr displayed the highest specificity being 4-and 3-fold more active in A375N cells than in T-47D and HeLa cells, respectively (Fig. 1A). The rest of the promoter fragments showed similar or even higher activity than hSPPr in A375N cells but their activity did not correlate with SPARC expression levels in the different cell types (Fig. 1A).
Figure 1.
Luciferase activity driven by different variants of SPARC promoter. A, activity of different variants of SPARC promoter in different cell lines B, activity of hSPPr and hSPPr(Δ10) in different cell types. Statistical analysis of hSPPr and hSPPr(Δ10) activity in the different cell lines was made in comparison to T-47D cells. ***, P < 0.001; **, P < 0.01; *, P < 0.05. Data include the activity in the different cell types of an SV40 promoter.
We pursued the characterization of hSPPr activity by deleting a 10-bp spacer between the GGA-1 and GGA-2 boxes [termed hSPPr(Δ10)] that has been shown previously to inhibit promoter activity (23). hSPPr(Δ10) activity was 4- to 15-fold higher than hSPPr in melanoma cells, WI-38 cells, and BAEC, although it also showed 4-fold increased activity in T-47D cells (Fig. 1B). As a comparison, we show the levels of activity of an SV40 promoter that was highly variable depending on the cell type (Fig. 1B).
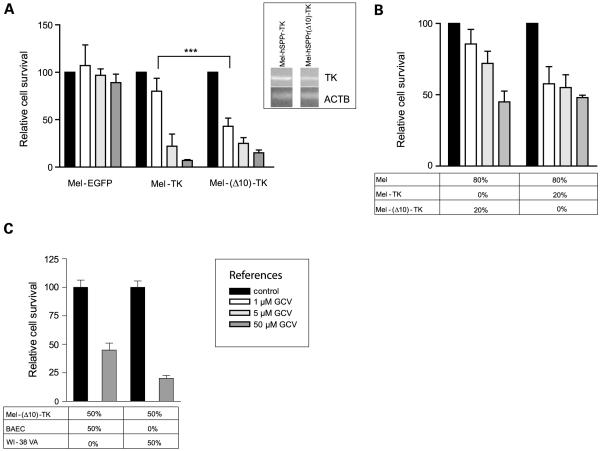
TK Expression Driven by SPARC Promoter followed by Exposure to Ganciclovir-Induced Human Melanoma Cell Killing In vitro
We constructed two plasmids carrying the TK gene under the control of either hSPPr or hSPPr(Δ10) promoters. A375N cells were transfected with both constructs and at least 10 G418-resistant clones were selected and tested for their sensitivity to different concentrations of ganciclovir (1, 5, and 50 μmol/L). All the isolated clones were highly sensitive to ganciclovir, regardless of whether TK was driven by hSPPr or hSPPr(Δ10) promoters (data not shown). One stable clone was selected and further characterized in each case and named Mel-TK and Mel-(Δ10)-TK, respectively. Mel-(Δ10)-TK cells were slightly more sensitive than Mel-TK cells to the lowest ganciclovir concentration, although at higher ganciclovir concentrations, both promoters were equally effective in inhibiting melanoma cell growth in vitro (Fig. 2A). Semiquantitative reverse transcription-PCR analysis showed 2-fold higher TK activity in the Mel-TK than in the Mel-(Δ10)-TK selected cell clone (Fig. 2A, inset); this difference might account for the fact that both cell clones were almost equally sensitive to ganciclovir both in vitro and in vivo (see Fig. 5 below) despite the fact that hSPPr(Δ10) activity was higher than hSPPr in melanoma cells according to luciferase assays.
Figure 2.
In vitro sensitivity to ganciclovir (GCV) of different cell types expressing TK. A, ganciclovir sensitivity of A375N-derived cell clones expressing TK driven by hSPPr and hSPPr(Δ10). Inset, TK and actin (ACTB) bands after semiquantitative reverse transcription-PCR. B, bystander effect induced by melanoma cells expressing TK driven by the two versions of SPARC promoter. C, ganciclovir sensitivity of a cell culture mix composed of Mel-(Δ10)-TK and either BAEC or WI-38 VA cells (1:1 cell ratio). ***, P < 0.001.
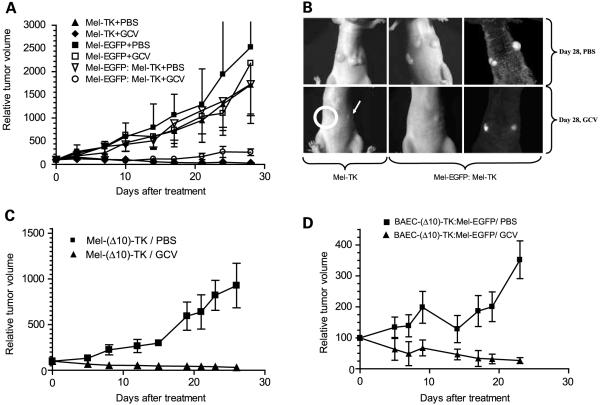
Figure 5.
In vivo inhibition of established melanomas expressing TK and treated with ganciclovir. A, the different cell types were injected as described and treated with PBS (n = 4) or ganciclovir (n = 6). B, external visualization of the in vivo tumor growth (bright field and fluorescence). C, mice carrying Mel-(Δ10)-TK tumors were treated with ganciclovir (n = 6) or PBS (n = 4) as described. D, mice carryingchimeric BAEC-(Δ10)-TK:A375N tumors were treated with ganciclovir (n = 6) or PBS (n = 4) as described.
Additional studies showed that 20% of Mel-TK or Mel-(Δ10)-TK cells mixed with 80% of parental A375N cells were sufficient to eliminate >50% of total cells in both cases in the presence of 50 μmol/L ganciclovir, indicating that SPARC promoter was able to drive TK bystander effect efficiently (Fig. 2B). Moreover, TK expression in melanoma cells induced 55 ± 3.6% and 81 ± 2.5% inhibition in total cell growth when a coculture of Mel-(Δ10)-TK either with BAEC or WI-38 VA cells (1:1 ratio) was exposed to 50 μmol/L ganciclovir, suggesting that TK expression in melanoma cells induced killing of adjacent nonmelanoma cells (Fig. 2C).
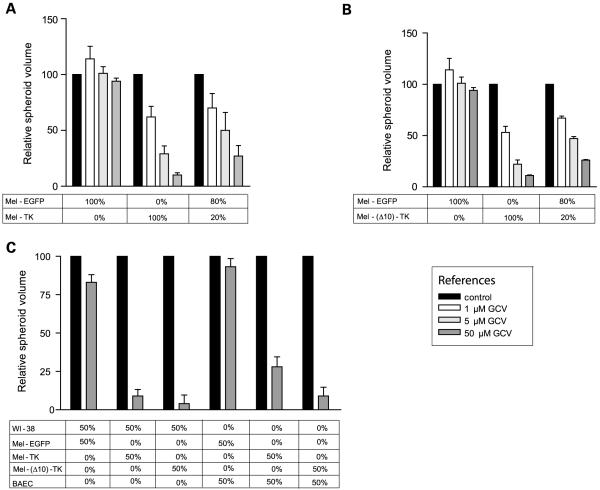
TK Expression Driven by SPARC Promoter followed by Exposure to Ganciclovir-Inhibited Melanoma Cell Growth in Homotypic and Heterotypic Spheroids
We next did in vitro assays using a three-dimensional model system of multicellular spheroids (24). Spheroids were grown for 3 days followed by the addition of ganciclovir and sized 7 days later. Homotypic spheroids made of 100% of either Mel-TK or Mel-(Δ10)-TK cells were growth inhibited at the three ganciclovir concentrations tested (Fig. 3A and B). Interestingly, when TK-expressing A375N cells accounted for only 20% of total A375N cells, spheroid growth was inhibited close to 80% in the presence of 50 μmol/L ganciclovir, confirming that TK expression driven by SPARC promoter can promote a bystander effect also when cells were grown in spheroids (Fig. 3A and B). In addition, both Mel-TK and Mel-(Δ10)-TK cells led to a strong growth inhibition of heterotypic spheroids composed of either of the two cell clones mixed with WI-38 cells or BAEC, confirming that TK expression in melanoma cells led to the elimination of neighbor stromal cells (Fig. 3C). In the entire set of experiments, ganciclovir had only minimal effect on spheroid growth in the absence of TK expression (data not shown).
Figure 3.
In vitro sensitivity to ganciclovir of homotypic and heterotypic spheroids. A, ganciclovir sensitivity of spheroids made of Mel-TK cells alone or mixed with Mel-EGFP cells. B, ganciclovir sensitivity of spheroids made of Mel-(Δ10)-TK alone or mixed with Mel-EGFP cells. C, ganciclovir sensitivity of spheroids made of melanoma cells expressing TK mixed with WI-38 fibroblasts. or BAEC.
TK Activity Expressed in Endothelial Cells Led to Cell Growth Inhibition in the Presence of Ganciclovir
As an initial step to establish whether TK expression in nonmelanoma cells driven by SPARC promoter might affect melanoma cell growth, we stably transfected WI-38 VA cells and BAEC with plasmids expressing TK. WI-38 cells were not used due to their low levels of transfectability (data not shown). Stable transfection of WI-38 VA cells and BAEC with hSPPr(Δ10)-TK plasmid led to the elimination of almost 70% of cells in both cases in the presence of 50 μmol/L ganciclovir (Fig. 4A).
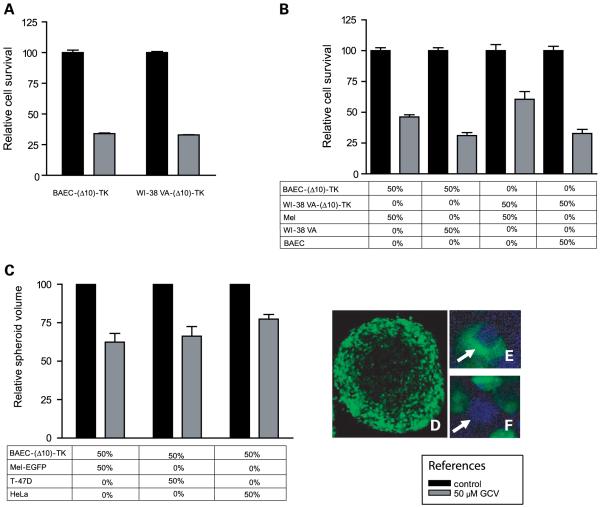
Figure 4.
In vitro sensitivity to ganciclovir of heterotypic cell cultures and spheroids containing stromal cells expressing TK. A, ganciclovir sensitivity of BAEC and WI-38 VA cells expressing TK. In all cases, ganciclovir was added for 5 d, the day after cells were seeded on the plates; data were obtained by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay. B, ganciclovir sensitivity of cells monolayers containing BAEC-(Δ10)-TK or WI-38 VA-(Δ10)-TK cells mixed with A375N cells. C, ganciclovir sensitivity of heterotypic spheroids made of BAEC-(Δ10)-TK cells mixed with different malignant cell types. D, immunofluorescence of a heterotypic spheroid made of Mel-EGFP and BAEC-(Δ10)-TK cells showingthe presence of Mel-EGFP green fluorescent cells at the outer part. E, combined immunofluorescence of EGFP and proliferatingcell nuclear antigen on a spheroid made of Mel-EGFP and BAEC-(Δ10)-TK cells. A representative Mel-EGFP cell (arrow) showing a blue nucleus (corresponding to positive proliferating cell nuclear antigen staining) and green cytoplasm. F, similar to E but showinga potential BAEC-(Δ10)-TK cell (arrow) with a blue nucleus and no green fluorescence in the cytoplasm.
Next, we established whether TK expression by WI-38 VA cells and BAEC might affect growth of adjacent cells lacking TK expression. A heterotypic cell culture mix of BAEC-(Δ10)-TK and A375N cells (1:1 ratio) was growth inhibited by 54 ± 1.8% in the presence of ganciclovir (Fig. 4B). In comparison, an heterotypic cell culture mix of WI-38 VA-(Δ10)-TK and A375N cells (1:1 ratio) was growth inhibited only by 40 ± 6.2% (Fig. 4B), suggesting that TK expression was more effective in driving elimination of melanoma cells when expressed by endothelial cells. In addition, BAEC-(Δ10)-TK inhibited by 68.9 ± 2.3% the in vitro growth of a 1:1 cell culture mix containing WI-38 VA cells (Fig. 4B), whereas WI-38 VA-(Δ10)-TK cells inhibited by 68 ± 3.4% a 1:1 cell culture mix containing BAEC (Fig. 4B).
Next, we try to establish whether TK expression in BAEC could be also effective in achieving elimination of malignant cells lacking TK expression in heterotypic spheroids. BAEC and BAEC-(Δ10)-TK cells were unable to form homotypic spheroids (data not shown); however, BAEC-(Δ10)-TK cells readily formed spheroids when mixed at 1:1 ratio with malignant cells. Exposure of these heterotypic spheroids to ganciclovir led to a growth inhibition of 37.6 ± 5.6%, 33.7 ± 6.2%, and 22.6 ± 3% when spheroids contained MEL-EGFP, T-47D, or HeLa cells, respectively (Fig. 4C). WI-38-(Δ10)-TK cells were slightly less effective than BAEC-(Δ10)-TK cells in the inhibition of heterotypic spheroids containing the malignant cells described above (data not shown). We hypothesized that the weaker inhibitory growth effect of stromal cells expressing TK in heterotypic spheroids compared with cell culture mixes could be due to the way the cells arranged in the spheroid. Interestingly, Mel-EGFP cells located in the outer part of the spheroid, whereas BAEC-(Δ10)-TK cells concentrated in the inner part and were then less accessible to ganciclovir (Fig. 4D). Immunohistochemical detection of proliferating cell nuclear antigen in combination with EGFP expression also showed that both Mel-EGFP and BAEC-(Δ10)-TK cells were cycling (Fig. 4E and F). Very similar results were obtained with heterotypic spheroids made of WI-38 VA-(Δ10)-TK and Mel-EGFP cells (data not shown).
Expression of TK Driven by SPARC Promoters followed by Ganciclovir Administration Led to the In vivo Growth Inhibition of Human Melanomas in Nude Mice
As a first approach to establish the feasibility of using SPARC promoter-TK combination in cancer therapy, we established in vivo models, in which Mel-TK cells were s.c. xenografted bilaterally in nude mice. Ten days later, mice harboring established melanoma tumors were split in two and given daily with either ganciclovir or PBS for 28 days. No tumor regression was observed in the groups of mice that received PBS (Fig. 5A). However, tumor regression was observed in all mice treated with ganciclovir (Fig. 5A). Average tumor size at the end of the experiment was below the size observed at the initiation of ganciclovir administration and in most cases tumors were not visible (Fig. 5A).
Mel-EGFP tumors also grew rapidly regardless of ganciclovir administration, whereas the in vivo growth of tumors composed of 1:1 mix of Mel-TK and Mel-EGFP cells was strongly inhibited following ganciclovir administration compared with control Mel-TK/Mel-EGFP tumors treated with PBS (Fig. 5A). Twenty-eight days after the initiation of the experiments, a decrease in the amount of EGFP-expressing cells was observed by external visualization of EGFP fluorescence in the group of mice treated with ganciclovir (Fig. 5B). As expected, mice injected with a mix of Mel-TK and Mel-EGFP cells and treated with PBS showed large tumors (Fig. 5B). Similar studies done with melanoma cells expressing TK driven by the hSPPr(Δ10) promoter also showed inhibition of tumor growth following ganciclovir administration, indicating that both variants of SPARC promoter were useful in driving TK expression leading to tumor growth inhibition (Fig. 5C).
TK Expression Driven by Endothelial Cells followed by Ganciclovir Administration Led to the In vivo Growth Inhibition of Established Tumors Composed of Melanoma and Endothelial Cells
To establish whether expression of TK by adjacent endothelial cells might induce tumor growth inhibition in vivo, we injected mice s.c. with a mix of BAEC-(Δ10)-TK cells and Mel-EGFP melanoma cells. Although these heterotypic tumors were smaller than those observed with melanoma cells alone, they grew uniformly and reached an average size of 200 mm3 (Fig. 5D; data not shown). Expression of TK by coadministered BAEC inhibited tumor growth in vivo in xenograft models following ganciclovir administration (Fig. 5D). Tumor regression was observed in all mice and average tumor size at the end of the experiment was below the size observed at the initiation of ganciclovir administration and in most cases tumors were not visible (Fig. 5D; data not shown).
Discussion
Conditional expression of therapeutic genes in tumor cells driven by TSP is a promising approach for cancer treatment. Promoters are currently selected for their capacity of being expressed mainly by the malignant tumor cells themselves (5-7). Because tumor progression occurs as a result of an active cross-talk between malignant and tumor-associated stromal cells, we hypothesized that expression of therapeutic genes driven by promoters corresponding to genes activated in the different cell types that compose the tumor mass would provide a greater advantage to achieve cancer remission. Here, we show for the first time that expression of a suicidal gene in nontumorigenic endothelial cells or fibroblasts driven by the SPARC promoter was able to inhibit melanoma cell growth both in vitro and in vivo in xenogeneic models.
Different promoter variants of the SPARC gene were evaluated to establish their degree of activity and specificity. We observed that the largest fragment (hSPPr) showed the better ratio of specificity versus activity, being more active in cells expressing the highest SPARC mRNA levels. Interestingly, a certain threshold of endogenous SPARC mRNA expression was necessary to establish a clear difference in hSPPr activity between cells that expressed SPARC mRNA compared with cells lacking SPARC mRNA expression. Indeed, MEL-Les cells that expressed only 7% of SPARC mRNA levels expressed by A375N cells showed only 1.8-fold higher hSPPr activity than T-47D cells, whereas MEL-J-N cells that expressed 24% of SPARC mRNA levels expressed by A375N cells showed 5.5-fold higher hSPPr activity than T-47D cells. In addition, we found no strict correlation between endogenous SPARC mRNA levels and promoter activity. Indeed, A375N, MEL-J-N, and WI-38 VA cells and BAEC that expressed different SPARC mRNA levels showed essentially similar levels of hSPPr activity. By searching the literature, we found no reports assessing the correlation between endogenous expression levels of a given gene and the activity of the corresponding promoter which is of relevance when selecting a promoter for conditional targeting (7, 9, 25, 26). We can hypothesize that additional regulatory elements important in the regulation of endogenous SPARC mRNA levels, including post-transcriptional regulation and intra-cellular stability of the mRNA, are absent in hSPPr and may give origin to the lack of strict correlation between SPARC mRNA levels and promoter activity.
In close agreement with a previous report (23), deletion of the 10-bp inter-GGA spacer element has an up-regulatory effect on SPARC promoter activity. However, the promoter fragment lacking the inter-GGA 10 bp was still more active in cells expressing SPARC. Despite the differences in activity between the two large promoter fragments in luciferase studies, both were able to drive TK expression and induce tumor cells elimination, both in vitro and in vivo.
The present studies that compared SPARC promoter capacity with drive TK expression in vitro in cell culture and multicellular spheroids and in vivo allowed drawing interesting conclusions: both SPARC promoter variants were effective in driving TK expression inducing growth inhibition of homotypic melanoma spheroids and tumors in the presence of ganciclovir. SPARC promoter-driven TK expression in melanoma cells was able to inhibit heterotypic spheroids containing, in addition, fibroblasts or endothelial cells. Rather than the phagocytosis of melanoma apoptotic bodies by neighbor fibroblasts or endothelial cells, which is not an intrinsic feature of these cells, this result suggests that tight junctions can be formed between malignant and stromal cells that allow exchange of phosphorylated ganciclovir (27-29). Vasculogenic mimicry, a process by which cancer cells can adopt the functionality of endothelial cells, has been characterized in human melanoma cells showing their intrinsic plasticity and potential capacity for tight interaction with neighbor endothelium (30).
Most importantly, the in vivo growth inhibition of mixed tumors composed of melanoma and endothelial cells was also attained when TK was expressed by the coadministered endothelial cells. A previous study has shown that expression of TK in pluripotent bone stromal cells driven by the osteocalcin promoter was effective in inhibiting the in vivo growth of chimeric tumors made of bone stromal cells and prostate cancer cells expressing osteocalcin (28). However, this previous work did not provide evidence about the efficacy of the approach on the complete set of animals, the extent of the in vivo growth inhibition, and the potential tumorigenic capacity of the pluripotent bone stromal cells that contributed a bone component to the chimeric tumors. The larger efficacy of BAEC-(Δ10)-TK in vivo and in monolayer cell culture compared with multicellular spheroids was probably the result of BAEC-(Δ10)-TK cells accessibility to ganciclovir due to spheroid architecture. Previous studies showed that binding of cytostatic drugs at the spheroid periphery delayed or prevented drug penetration to the inner part of the spheroids (31). It can be hypothesized that TK was more effective in vivo than in spheroids when expressed by BAEC, most probably due to tumor accessibility to ganciclovir through tumor-associated vasculature. Overall, the evidence that the in vivo melanoma growth was inhibited even when TK was expressed by neighbor endothelial cells suggests that targeting the endothelial cell compartment with a therapeutic vector whose activity is driven by SPARC promoter might achieve tumor elimination even if the malignant cell compartment of the tumor mass showed no SPARC activity.
Acknowledgments
We thank Fabio Fraga for technical support.
Grant support: Welcome Trust, United Kingdom, the René Barón and Amigos de la Fundación Leloir para la Investigación contra el Cáncer Foundations, The National Ministry of Health and the National Agency for Promotion of Science and Technology, Argentina, and the Arthritis Research Campaign, United Kingdom.
Footnotes
Supplementary material for this article is available at Molecular Cancer Therapeutics Online (http://mct.aacrjournals.org/).
References
- 1.Jemal A, Tiwari RC, Murray T, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8–29. doi: 10.3322/canjclin.54.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Clegg LX, Ward E, et al. Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 3.Clausen SP, Brady MS. Surgical margins in patients with cutaneous melanoma—assessing the adequacy of excision. Melanoma Res. 2005;15:539–42. doi: 10.1097/00008390-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Tsutsumida A, Furukawa H, Yamamoto Y, Sugihara T. Treatment strategy for cutaneous malignant melanoma. Int J Clin Oncol. 2005;10:311–7. doi: 10.1007/s10147-005-0522-9. [DOI] [PubMed] [Google Scholar]
- 5.Toniatti C, Bujard H, Cortese R, Ciliberto G. Gene therapy progress and prospects: transcription regulatory systems. Gene Ther. 2004;11:649–57. doi: 10.1038/sj.gt.3302251. [DOI] [PubMed] [Google Scholar]
- 6.Fecker LF, Geilen CC, Hossini AM, et al. Selective induction of apoptosis in melanoma cells by tyrosinase promoter-controlled CD95 ligand overexpression. J Invest Dermatol. 2005;124:221–8. doi: 10.1111/j.0022-202X.2004.23572.x. [DOI] [PubMed] [Google Scholar]
- 7.Schoensiegel F, Paschen A, Sieger S, et al. MIA (melanoma inhibitory activity) promoter mediated tissue-specific suicide gene therapy of malignant melanoma. Cancer Gene Ther. 2004;11:408–18. doi: 10.1038/sj.cgt.7700721. [DOI] [PubMed] [Google Scholar]
- 8.Rothfels H, Paschen A, Schadendorf D. Evaluation of combined gene regulatory elements for transcriptional targeting of suicide gene expression to malignant melanoma. Exp Dermatol. 2003;12:799–810. doi: 10.1111/j.0906-6705.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- 9.Zhu ZB, Makhija SK, Lu B, et al. Transcriptional targeting of tumors with a novel tumor-specific survivin promoter. Cancer Gene Ther. 2004;11:256–62. doi: 10.1038/sj.cgt.7700679. [DOI] [PubMed] [Google Scholar]
- 10.Nettelbeck DM, Rivera AA, Davydova J, et al. Cyclooxygenase-2 promoter for tumour-specific targeting of adenoviral vectors to melanoma. Melanoma Res. 2003;13:287–92. doi: 10.1097/00008390-200306000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Hanash S. Integrated global profiling of cancer. Nat Rev Cancer. 2004;4:638–44. doi: 10.1038/nrc1414. [DOI] [PubMed] [Google Scholar]
- 12.Vial E, Castellazzi M. Down-regulation of the extracellular matrix protein SPARC in vSrc- and vJun-transformed chick embryo fibroblasts contributes to tumor formation in vivo. Oncogene. 2000;19:1772–82. doi: 10.1038/sj.onc.1203493. [DOI] [PubMed] [Google Scholar]
- 13.Ledda F, Bravo AI, Adris S, et al. The expression of the secreted protein acidic and rich in cysteine (SPARC) is associated with the neoplastic progression of human melanoma. J Invest Dermatol. 1997;108:210–4. doi: 10.1111/1523-1747.ep12334263. [DOI] [PubMed] [Google Scholar]
- 14.Rumpler G, Becker B, Hafner C, et al. Identification of differentially expressed genes in models of melanoma progression by cDNA array analysis: SPARC, MIF, and a novel cathepsin protease characterize aggressive phenotypes. Exp Dermatol. 2003;12:761–71. doi: 10.1111/j.0906-6705.2003.00082.x. [DOI] [PubMed] [Google Scholar]
- 15.Massi D, Franchi A, Borgognoni L, Reali UM, Santucci M. Osteonectin expression correlates with clinical outcome in thin cutaneous malignant melanomas. Hum Pathol. 1999;30:339–44. doi: 10.1016/s0046-8177(99)90014-x. [DOI] [PubMed] [Google Scholar]
- 16.Framson PE, Sage EH. SPARC and tumor growth: where the seed meets the soil? J Cell Biochem. 2004;92:679–90. doi: 10.1002/jcb.20091. [DOI] [PubMed] [Google Scholar]
- 17.Podhajcer OL, Wolf C, Lefebvre O, et al. Comparative expression of the SPARC and stromelysin-3 genes in mammary tumours. Breast. 1996;5:13–20. [Google Scholar]
- 18.Sakai N, Baba M, Nagasima Y, et al. SPARC expression in primary human renal cell carcinoma: upregulation of SPARC in sarcomatoid renal carcinoma. Hum Pathol. 2001;32:1064–70. doi: 10.1053/hupa.2001.28244. [DOI] [PubMed] [Google Scholar]
- 19.Sato N, Fukushima N, Maehara N, et al. SPARC/osteonectin is a frequent target for aberrant methylation in pancreatic adenocarcinoma and a mediator of tumor-stromal interactions. Oncogene. 2003;22:5021–30. doi: 10.1038/sj.onc.1206807. [DOI] [PubMed] [Google Scholar]
- 20.Koukourakis MI, Giatromanolaki A, Brekken RA, et al. Enhanced expression of SPARC/osteonectin in the tumor-associated stroma of non-small cell lung cancer is correlated with markers of hypoxia/acidity and with poor prognosis of patients. Cancer Res. 2003;63:5376–80. [PubMed] [Google Scholar]
- 21.Berenstein M, Adris S, Ledda F, et al. Different efficacy of in vivo herpes simplex virus thymidine kinase gene transduction and ganciclovir treatment on the inhibition of tumor growth of murine and human melanoma cells and rat glioblastoma cells. Cancer Gene Ther. 1999;6:358–66. doi: 10.1038/sj.cgt.7700056. [DOI] [PubMed] [Google Scholar]
- 22.Young MF, Findlay DM, Dominguez P, et al. Osteonectin promoter. DNA sequence analysis and S1 endonuclease site potentially associated with transcriptional control in bone cells. J Biol Chem. 1989;264:450–6. [PubMed] [Google Scholar]
- 23.Hafner M, Zimmermann K, Pottgiesser J, Krieg T, Nischt R. A purine-rich sequence in the human BM-40 gene promoter region is a prerequisite for maximum transcription. Matrix Biol. 1995;14:733–41. doi: 10.1016/s0945-053x(05)80016-2. [DOI] [PubMed] [Google Scholar]
- 24.Sutherland RM. Cell and environment interactions in tumor micro-regions: the multicell spheroid model. Science. 1988;240:177–84. doi: 10.1126/science.2451290. [DOI] [PubMed] [Google Scholar]
- 25.Wesseling JG, Bosma PJ, Krasnykh V, et al. Improved gene transfer efficiency to primary and established human pancreatic carcinoma target cells via epidermal growth factor receptor and integrin-targeted adenoviral vectors. Gene Ther. 2001;8:969–76. doi: 10.1038/sj.gt.3301473. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Bezdek T, Chang J, et al. A glial-specific, repressible, adenovirus vector for brain tumor gene therapy. Cancer Res. 1998;58:3504–7. [PubMed] [Google Scholar]
- 27.Kapoor P, Saunders MM, Li Z, et al. Breast cancer metastatic potential: correlation with increased heterotypic gap junctional intercellular communication between breast cancer cells and osteoblastic cells. Int J Cancer. 2004;111:693–7. doi: 10.1002/ijc.20318. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh CL, Gardner TA, Miao L, Balian G, Chung LW. Cotargeting tumor and stroma in a novel chimeric tumor model involving the growth of both human prostate cancer and bone stromal cells. Cancer Gene Ther. 2004;11:148–55. doi: 10.1038/sj.cgt.7700665. [DOI] [PubMed] [Google Scholar]
- 29.Miekus K, Czernik M, Sroka J, Czyz J, Madeja Z. Contact stimulation of prostate cancer cell migration: the role of gap junctional coupling and migration stimulated by heterotypic cell-to-cell contacts in determination of the metastatic phenotype of Dunning rat prostate cancer cells. Biol Cell. 2005;97:893–903. doi: 10.1042/BC20040129. [DOI] [PubMed] [Google Scholar]
- 30.Hendrix MJ, Seftor EA, Hess AR, Seftor RE. Vasculogenic mimicry and tumour-cell plasticity: lessons from melanoma. Nat Rev Cancer. 2003;3:411–21. doi: 10.1038/nrc1092. [DOI] [PubMed] [Google Scholar]
- 31.Erlanson M, Daniel-Szolgay E, Carlsson J. Relations between the penetration, binding, and average concentration of cytostatic drugs in human tumour spheroids. Cancer Chemother Pharmacol. 1992;29:343–53. doi: 10.1007/BF00686002. [DOI] [PubMed] [Google Scholar]