Abstract
Purpose
Tocopherols are lipophilic antioxidants present in vegetable oils. Although the antioxidant and anticancer activities of α-tocopherol (vitamin E) have been studied for decades, recent intervention studies with α-tocopherol have been negative for protection from cancer in humans. The tocopherols consist of 4 isoforms, α, β, γ, and δ variants, and recent attention is being made to other isoforms. In the present study, we investigated the inhibitory effect of a tocopherol mixture rich in γ- and δ-tocopherols against mammary tumorigenesis.
Experimental Design
Female Sprague Dawley rats were treated with N-methyl-N-nitrosourea (NMU), and then fed diets containing 0.1%, 0.3%, or 0.5% mixed tocopherols rich in γ- and δ-tocopherols for 9 weeks. Tumor burden and multiplicity were determined, and the levels of markers of inflammation, proliferation and apoptosis were evaluated in the serum and in mammary tumors. The regulation of nuclear receptor signaling by tocopherols was studied in mammary tumors and in breast cancer cells.
Results
Dietary administration of 0.1%, 0.3%, or 0.5% mixed tocopherols suppressed mammary tumor growth by 38%, 50%, or 80%, respectively. Tumor multiplicity was also significantly reduced in all three mixed tocopherol groups. Mixed tocopherols increased the expression of p21, p27, caspase-3 and peroxisome proliferator activated receptor-γ (PPAR-γ), and inhibited AKT and estrogen signaling in mammary tumors. Our mechanistic study found that γ- and δ-tocopherols, but not α-tocopherol, activated PPAR-γ and antagonized estrogen action in breast cancer.
Conclusion
The results suggest that γ- and δ-tocopherols may be effective agents for the prevention of breast cancer.
Keywords: breast cancer, γ-tocopherol, δ-tocopherol, estrogen receptor, PPAR-γ
INTRODUCTION
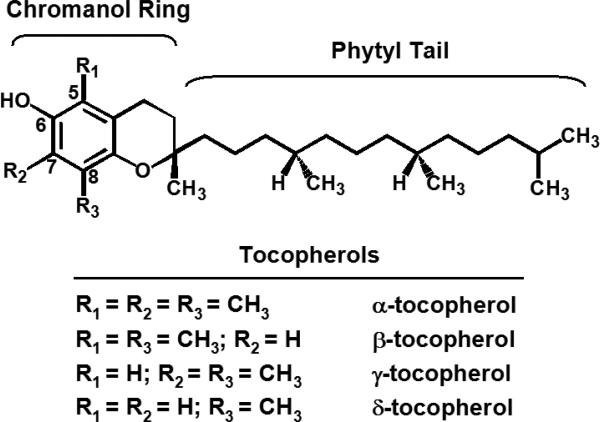
Vitamin E is a fat-soluble vitamin essential for humans (1). The vitamin E family is comprised of eight lipophilic, naturally occurring compounds that include four tocopherols (with a saturated phytyl tail) and four tocotrienols (with an unsaturated isoprenoid side chain) designated as α, β, γ, and δ (2). The prevalent tocopherols in foods are the α, γ, and δ variants, natural (RRR) tocopherols differing only in the number and location of the methyl groups in the chromanol ring system (Fig. 1). Tocopherols and tocotrienols are phenolic antioxidants present in many vegetable oils, and all their isomers are known to have strong antioxidant activities (3-5). In the U.S., α-tocopherol and γ-tocopherol are the most common dietary tocopherols due to their high amounts in commercially produced vegetable oils such as soybean, corn and cottonseed (3, 4, 6). Although γ-tocopherol is more abundant than α-tocopherol in the human diet, α-tocopherol has been considered the classic “vitamin E” because it is the major tocopherol found in plasma and tissues (3), and it has superior activity over other tocopherols in the fertility-restoration assay (7, 8).
Fig. 1.
Structures of tocopherol variants, α-, β-, γ-, and δ-tocopherol
Epidemiological evidence supporting a link between vitamin E and cancer is limited, and the results of a few completed studies with vitamin E are not consistent (2, 9). Similarly, the results of studies with pure α-tocopherol or its more stable acetate ester in different cancer models including colon, breast and prostate, are also not conclusive (2, 9, 10). A randomized, double-blind, placebo-controlled Alpha-Tocopherol, Beta-Carotene (ATBC) lung cancer prevention study conducted between 1985 and 1993 examined the effect of α-tocopherol and β-carotene daily supplements on the incidence of lung cancer and possibly other cancers (11). The study found that male smokers receiving 50 mg/day of synthetic DL-α-tocopherol acetate had a lower prostate cancer incidence and a significant reduction in prostate cancer deaths when compared with the control group (12).
Following the ATBC cancer prevention study, two large randomized trials assessing the effect of vitamin E supplementation on cancer incidence were established: The Heart Outcomes Prevention Evaluation (HOPE) trial (13) and the Women's Health Study (WHS) trial (14). These studies found no significant association between cancer incidence and vitamin E (α-tocopherol) ingestion (13), and there was no overall benefit for prevention of major adverse cardiovascular events or cancer (14). Interestingly, however, a nested case-control study with male residents in Washington County, MD, showed a statistically significant inverse association between γ-tocopherol and the risk of prostate cancer, whereas α-tocopherol showed no statistically significant benefit (15).
γ-Tocopherol, the most common form of vitamin E in the US diet and the second most common form in human tissues, has demonstrated anti-inflammatory and anti-cancer activity in numerous models of colon, breast, and prostate cancer (2, 16-19). Furthermore, γ-tocopherol effectively inhibited cyclooxygenase (20, 21), trapped reactive nitrogen species (22, 23), and showed stronger anti-inflammatory activity than α-tocopherol (21, 23). Our laboratory recently demonstrated cancer-preventive activity for mixed tocopherols in animal models of colon and mammary tumorigenesis (24, 25). We used a readily available mixed tocopherol preparation (containing over 50% γ-tocopherol) added at 0.1% to a standardized semi-purified laboratory diet. Administration of the tocopherol-containing diet resulted in a significant inhibition of azoxymethane (AOM)-induced aberrant crypt foci (ACF) in the colon of rats, a recognized early biomarker of colon cancer risk (24), and there was also a significant inhibition of N-methyl-N-nitrosourea (NMU)-induced mammary tumorigenesis (25). In addition, Ju et al. recently reported that the mixed tocopherols inhibit colon carcinogenesis by inducing apoptosis, inhibiting inflammation, and reducing the oxidative/nitrosative stress (26).
Tocopherols have been shown to bind to the estrogen receptor (ER) and to work as antagonists of estrogen signaling (27). This led us to study the mechanism of inhibition of mammary tumorigenesis by each tocopherol isoform. In addition to the anti-estrogenic action of tocopherols, they may activate a nuclear receptor, peroxisome proliferator activated receptor-γ (PPAR-γ), due to their structural similarity to thiazolidinedione PPAR-γ activator, troglitazone (28). Both α and γ-tocopherol have been shown to activate PPAR-γ expression and transactivation in colon cancer cells, and γ-tocopherol is a better modulator of PPAR-γ expression than α-tocopherol (16, 28).
In our earlier study, we showed that dietary administration of 0.1% mixed tocopherols inhibited NMU-induced mammary tumorigenesis and expression of proliferating cell nuclear antigen (PCNA) in tumor tissues (25). In the present study, we determined the efficacy of mixed tocopherols at three different doses on NMU-induced mammary tumorigenesis and also investigated the mechanisms of action of tocopherols in mammary tumors and in cultured MCF-7 and T47D human breast cancer cells. We investigated whether mixed tocopherols inhibit inflammatory markers or regulate nuclear receptor signaling, such as estrogen receptor or PPAR-γ, in mammary tumors, and whether these actions may contribute to the suppression of mammary tumor growth by tocopherols in experimental animals. We report here that mixed tocopherols may inhibit tumor growth through the regulation of nuclear receptor signaling during mammary tumorigenesis.
MATERIALS AND METHODS
Reagents and cell culture
α-Tocopherol, γ-tocopherol, and δ-tocopherol were purchased from Sigma (St. Louis, MO). The compounds were dissolved in DMSO. The human MCF-7 and T47D breast cancer cell lines were obtained from the American Type Culture Collection (Manassas, VA). The cells were maintained in Dulbecco's Modified Eagle's Medium (DMEM)/F-12 supplemented with 10% FBS and 1% penicillin /streptomycin at 37°C and 5% CO2, and passed every 3−4 days.
Measurement of cell proliferation by [3H]thymidine incorporation
MCF-7 and T47D cells were plated at a density of 8,000 cells/well in 24-well plates and treated with compounds in 10% charcoal stripped FBS/phenol red-free RPMI medium for 3 days. Before harvest, the cells were incubated with 1 μCi [3H]thymidine for 3 h at 37°C and were washed with phosphate buffered saline. The cells were precipitated with cold 10% trichloroacetic acid for 10 min and solubilized with 0.5 ml solubilization buffer (0.2 M NaOH, 40 μg/ml salmon sperm DNA) for 2 h at room temperature. The [3H]thymidine incorporated into the DNA of MCF-7 and T47D cells was determined using a scintillation spectrometer (Beckman Coulter, Fullerton, CA).
Transient transfection of PPAR-γ
pCMX-mPPAR-γ1, PPREx3-tk-Luc, pCMX-hRXR-α, and pCMV-β-gal vectors were kindly provided by Dr. David Mangelsdorf (University of Texas Southwestern Medical Center, Dallas, TX) and previously reported (29). For the transient transfection of PPAR-γ, PPRE-luc and RXR-α vectors, DNAs were mixed with FuGene6 Transfection Reagent (Invitrogen, Carlsbad, CA), and this mixture was directly added to MCF-7 and T47D cells in DMEM/F12 medium without serum. After incubation with the mixture for 4 h, the cells were treated with the compounds for an additional 36 h in 10% charcoal stripped FBS/phenol red free RPMI medium. Luciferase activity was measured with a luminometer (Turner Biosystems, Sunnyvale, CA) and normalized by β-galactosidase activity.
Diets for animal experiment
The mixed tocopherols were supplied by the Cognis Corporation (Kankakee, IL), and contained 57% γ-tocopherol, 24% δ-tocopherol, 13% α-tocopherol, and insignificant amount of β-tocopherol (about 0.5%). Semi-purified modified AIN-93M diet was obtained from Research Diets Laboratory (New Brunswick, NJ) and used as the control diet. The test diet was prepared by adding 0.1%, 0.3%, or 0.5% of mixed tocopherols to AIN-93M diet. The diets were stored in sealed containers at 4°C, and the food cups were replenished with fresh diets twice weekly.
Animals and experimental procedure
Female Sprague-Dawley rats were obtained from Taconic Farms (Germantown, NY). Rats (21 ± 1 days old) were treated with a single intraperitoneal injection of the carcinogen N-methyl-N-nitrosourea (NMU, 50 mg/kg body weight). One week after NMU injection, rats were fed AIN-93M control diet or AIN-93M diets containing mixed tocopherols (0.1, 0.3, or 0.5% of the diet). Tumors were palpated weekly. Nine weeks after NMU injection, the rats were sacrificed and tumors were weighed and counted at autopsy. The average tumor burden was the sum of tumor weights in the group/number of rats in the group. The average tumor multiplicity was the sum of the number of tumors in each group/number of rats per group. All animal studies were performed in accordance with an institutionally approved protocol.
Analysis of tocopherol levels in rat serum
Rat serum was collected at autopsy, and serum tocopherol levels (α-, δ-, or γ-tocopherol) were measured by a method modified from a previously described procedure (30). In brief, fat-soluble vitamins were extracted from 150 μl of plasma with ethanol and hexane, and then dissolved in a mixture of ethanol and acetonitrile. An HPLC system was developed using a Supelcosil LC18 column, 5 μm (4.6 ×150 mm; Bellefonte, PA) with ethanol:acetonitrile (45:55) as the mobile phase. A Waters 490 multiwavelength detector (Waters-Millipore, Milford, MA) was used to detect absorbance at 292 nm (α-, γ-, δ-tocopherol) and 325 nm (retinol). Reference samples of pure α-, γ- and δ-tocopherol as well as retinol were obtained from the Centers for Disease Control and Prevention (Atlanta, GA). The structures of α, β, γ and δ-tocopherol are shown in Fig. 1.
Histopathological analyses and immunohistochemistry
Mammary tumors from each group were harvested at autopsy and fixed in 10% formalin for 24 h. They were paraffin embedded, and cut into 4 μm thick tissue sections. Individual tumors were evaluated histopathologically in hematoxylin and eosin (H&E)-stained tumor sections. For immunohistochemistry, the slides were incubated overnight at room temperature with antibody against cleaved caspase-3 (1:200 diluted, Cell Signaling Technology Inc., Beverly, MA) and PPAR-γ (1:200, Santa Cruz Biotechnology, Santa Cruz, CA). The slides were incubated with biotinylated secondary antibody, and then with avidin/biotinylated peroxidase complex for 30 min at room temperature (Vector Labs, Burlingame, CA). The slides were then incubated with 3’-diaminobenzamine (DAB) substrate, and the sections were counterstained with Modified Harris Hematoxylin. The images were taken randomly using a Zeiss AxioCam HRc camera fitted to a Zeiss Axioskope 2 Plus microscope.
Western blot analysis
Tumor samples were homogenized in RIPA buffer (10 mM Tris-HCl, 5 mM EDTA, 150 mM NaCl, 1% Triton X-100, 1% sodium deoxycholate, 0.1% sodium dodecyl sulfate, 0.1mM Na3VO4, 1% PMSF, 1% aprotinin and 0.1% leupeptin) using a Dounce homogenizer (Wheaton, Millville, NJ), and the protein extracts were electrophoresed in 4−15% gradient gels (Biorad, Hercules, CA) and transferred to a PVDF membrane (PALL, Ann Arbor, MI). The primary antibodies against PARP, cleaved PARP, cleaved caspase-3, phospho-Akt, Akt (Cell Signaling Technology Inc., Beverly, MA), p21, p27, ER-α, and COX-2 (Santa Cruz Biotechnology, Santa Cruz, CA), actin (Sigma, St. Louis, MO), and secondary antibodies (Santa Cruz Biotechnology, Santa Cruz, CA) were used.
Quantitative RT-PCR analysis
These procedures have been previously reported (31). Labeled primers, including GAPDH, ER-α, and PPAR-γ, were obtained from Applied Biosystems (Foster City, CA).
Enzyme Immunoassay
Procedures for prostaglandin E2 (PGE2) and leukotriene B4 (LTB4) enzyme immunoassay (EIA) have been reported previously (26). For the determination of PGE2, LTB4, and 8-isoprostane levels, the tissue homogenates or serum samples were mixed with ethyl acetate, vortexed for 30 min, and then centrifuged at 10,000 × g for 20 min (Sorvall RT 6000B). The organic layer was collected and dried using a Speed Vacuum Evaporator (VWR International, INC., West Chester, PA). The dried samples were then reconstituted in EIA buffer (Cayman Chemical, Ann Arbor, Michigan), and levels of PGE2, LTB4, and 8-isoprostane were determined using EIA kits (Cayman Chemical, Ann Arbor, MI).
Statistical analysis
Statistical significance was evaluated using the Student's t-test.
RESULTS
The serum levels of γ-tocopherol and δ-tocopherol are significantly increased by the administration of mixed tocopherols in rats
We used AIN-93M control diet, 0.1%, 0.3%, or 0.5% mixed tocopherols in AIN-93M diet throughout the 9-week study. To determine the bioavailability of the diet tocopherol in experimental animals, we collected blood samples at autopsy and determined the serum levels of retinol, α-, γ- and δ-tocopherol (Table 1). Serum levels of retinol in rats fed with 0.1%, 0.3%, or 0.5% mixed tocopherols were comparable to those in rats fed with the control diet. However, rats fed with 0.1%, 0.3%, or 0.5% mixed tocopherols had much higher levels of γ- and δ-tocopherols than the control group (Table 1). Rats fed with 0.1%, 0.3%, or 0.5% mixed tocopherols had the levels of γ-tocopherol increased by 7.6, 19.1, or 23.5-fold, respectively. The level of δ-tocopherol was barely detectable in the control group fed the AIN-93M diet, but rats fed with 0.1%, 0.3%, or 0.5% mixed tocopherols had the levels of δ-tocopherol increased by 19.7, 56.3, or 80.7-fold, respectively. Mixed tocopherols contained only a negligible amount of β-tocopherol, and the serum level of β-tocopherol was not detectable.
Table 1.
Analysis of tocopherol levels in the serum of Sprague-Dawley rats fed a control diet or mixed tocopherol diets.
| Group# | Retinol (μM)§ | α-Tocopherol (μM)§ | γ-Tocopherol (μM)§ | δ-Tocopherol (μM)§ |
|---|---|---|---|---|
| AIN-93M control diet | 0.86 ± 0.37 | 20.8 ± 10.9 | 0.15 ± 0.09 | 0.03 ± 0.04 |
| 0.1% mixed tocopherols in AIN-93M diet | 0.69 ± 0.15 | 24.0 ± 9.2 (1.2 fold) | 1.14 ± 0.74** (7.6 fold) | 0.59 ± 0.41** (19.7 fold) |
| 0.3% mixed tocopherols in AIN-93M diet | 0.81 ± 0.22 | 29.4 ± 7.8 (1.4 fold) | 2.87 ± 0.73*** (19.1 fold) | 1.69 ± 0.44*** (56.3 fold) |
| 0.5% mixed tocopherols in AIN-93M diet | 0.81 ± 0.17 | 27.7 ± 4.3 (1.3 fold) | 3.53 ± 1.03*** (23.5 fold) | 2.42 ± 0.47*** (80.7 fold) |
All rats (21 ± 1 days old, n=12 per group) were given an i.p. injection of 50 mg N-methyl-N-nitrosourea per kilogram body weight 1 week before starting the feeding of mixed tocopherols. Rats were fed a control or mixed tocopherol-containing diets for 9 weeks. Serum samples were collected at autopsy and analyzed for the levels of retinol, α-tocopherol, γ-tocopherol and δ-tocopherol.
The data are expressed as the mean +/− S.E. (N=6).
*Significantly different from control by the Student's t-test, *p <0.05
p < 0.01
p< 0.001.
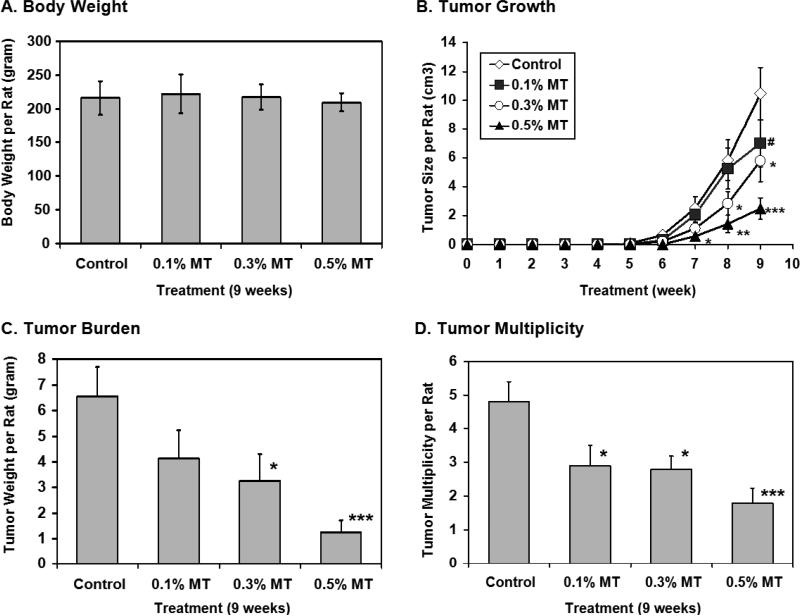
Mixed tocopherols inhibit NMU-induced mammary tumor growth and multiplicity without affecting the body weight
The body weight of rats fed the experimental diet containing 0.1%, 0.3%, or 0.5% mixed tocopherols was not significantly different from that of rats fed the control diet throughout the 9-week experimental period (Fig. 2A). Starting from 5 week after the carcinogen injection, mammary tumors became palpable, and the volume of mammary tumors was measured weekly (Fig. 2B). Mammary tumors continued to grow in the control group, whereas the tumor growth was inhibited in a dose-dependent fashion in groups fed with three different doses of mixed tocopherols (Fig. 2B). As shown in Fig. 2C and 2D, the tumor burden and tumor multiplicity at autopsy were also significantly reduced by the administration of mixed tocopherols. The percentage inhibition of the average tumor burden per rat for the groups fed 0.1%, 0.3%, or 0.5% mixed tocopherols was 38%, 50%, or 80%, respectively (Fig. 2C). The average tumor multiplicity from the control group was 4.8 ± 0.6 tumors per rat, whereas the average tumor multiplicity from the groups fed 0.1%, 0.3%, or 0.5% mixed tocopherols was 2.9 ± 0.6, 2.5 ± 0.4, or 1.8 ± 0.4 tumors per rat, respectively, which translated into reductions by 40%, 48%, or 63%, respectively (Fig. 2D).
Fig. 2.
Mixed tocopherols (MT) inhibit mammary tumor growth in a dose-dependent manner. All rats (21 ± 1 days old) were given an i.p. injection of 50 mg N-methyl-N-nitrosourea (NMU) per kilogram body weight 1 week before starting the feeding of 0.1%, 0.3%, and 0.5% mixed tocopherols. Rats were fed with control or mixed tocopherols containing diet for 9 weeks. Tumor volume and body weight were measured weekly. The data are expressed as mean +/− S.E. (N=12). A. Average body weight at autopsy was not affected up to 0.5% mixed tocopherols in the diet. B. Mixed tocopherols significantly inhibited the mammary tumor growth in a dose-dependent manner. C. Average tumor burden in the groups fed mixed tocopherols (0.1%, 0.3%, and 0.5% in the diet) was reduced by 37.9%, 50.0% and 80.3% respectively. D. Tumor multiplicity of the group fed 0.1%, 0.3%, and 0.5% mixed tocopherols in the diet was reduced by 39.6%, 47.9%, and 62.5% respectively. Significant difference between control and mixed tocopherols fed groups was determined by the Student's t-test (# p =0.05, *p <0.05, **p < 0.01, *** p< 0.001).
Treatment with mixed tocopherols does not affect the levels of markers of inflammation and oxidation in the serum
Since γ-tocopherol is known to inhibit the activity of the cyclooxygenase (COX) enzyme (20, 21), we next determined whether inflammatory markers are modulated by tocopherols in our animal model of mammary tumorigenesis. Pro-inflammatory eicosanoids, PGE2 and LTB4, are the enzymatic products of the arachidonic acid pathway, cyclooxygenase and lipooxygenase-5, respectively. Different from a previous report in the azoxymethane/dextran sulfate sodium (AOM/DSS)-induced colon cancer model in mice (26), the serum levels of PGE2 and LTB4 in the control group were not significantly different from those in the groups fed with mixed tocopherols (Table 2). The plasma level of 8-isoprostane, a marker of oxidative stress, was also measured to determine the anti-oxidant activity of the tocopherols during mammary carcinogenesis. As shown in Table 2, the plasma level of 8-isoprostane in the control group was also similar to that in the mixed tocopherol-fed groups.
Table 2.
Serum levels of PGE2, LTB4 and 8-isoprostane from control diet or mixed tocopherols diet fed Sprague-Dawley rats.
| Group# | PGE2 (pg/ml)§ | LTB4 (pg/ml)§ | 8-Isoprostane (pg/ml)§ |
|---|---|---|---|
| AIN-93M control diet | 7658.6 ± 1820.5 | 686.0 ± 78.1 | 287.5 ± 58.8 |
| 0.1% mixed tocopherols in AIN-93M diet | 8898.7 ± 1676.0 | 714.7 ± 47.9 | 290.4 ± 71.5 |
| 0.3% mixed tocopherols in AIN-93M diet | 8443.1 ± 1573.2 | 700.9 ± 49.0 | 248.4 ± 40.6 |
| 0.5% mixed tocopherols in AIN-93M diet | 8348.5 ± 1045.7 | 680.8 ± 30.6 | 255.1 ± 35.4 |
All rats (21 ± 1 days old, n=12 per group) were given an i.p. injection of 50 mg N-methyl-N-nitrosourea per kilogram body weight 1 week before starting the feeding of mixed tocopherols. Rats were fed with control or mixed tocopherol containing diet for 9 weeks. Serum samples were collected at autopsy and analyzed for the levels of PGE2, LTB4 and 8-isoprostane.
The data are expressed as mean +/− S.E. (N=6). There is no significant difference among groups by statistical analysis.
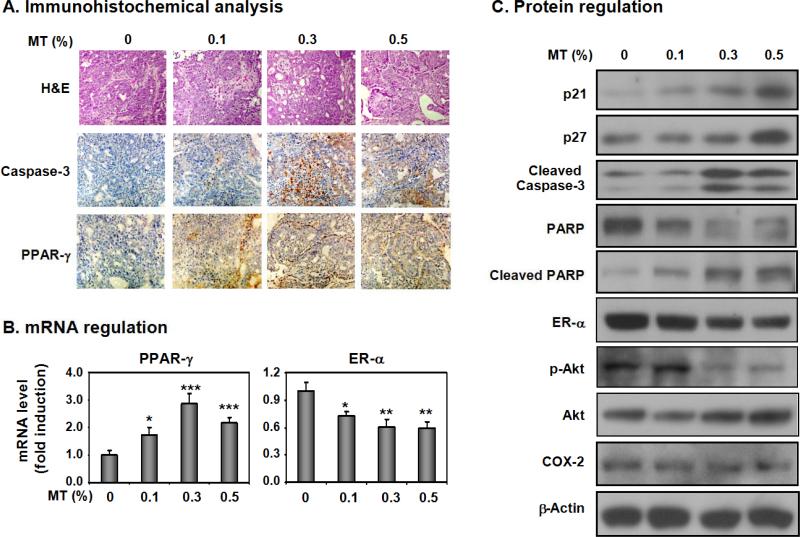
Mixed tocopherols regulate PPAR-γ and ER-α nuclear receptor signaling as well as cell proliferation and apoptosis in mammary tumors
To determine which factors may contribute to the inhibition of mammary tumorigenesis by tocopherols, we next analyzed the mammary tumors for various markers. Using H&E staining, we found that all tumors evaluated were adenocarcinomas, either papillary, cribriform or tubular adenocarcinoma type. The tumor grade among the control group and mixed tocopherol-treated groups was not different (Fig. 3A). However, immunohistochemical analyses determined that administration of mixed tocopherols increased the expression of an apoptosis marker, cleaved caspase-3, and a nuclear receptor, PPAR-γ, in mammary tumors (Fig. 3A). The mRNA levels of PPAR-γ and ER-α were also affected by mixed tocopherols. As shown in Fig. 3B, there was a significant induction of PPAR-γ mRNA level but a decrease of ER-α mRNA level. In western blot analysis, we found that dietary administration of mixed tocopherols upregulated the cyclin-dependent kinase (CDK) inhibitors, p21 and p27, and increased the level of apoptosis markers, cleaved PARP and cleaved caspase-3, in mammary tumors (Fig. 3C). Mixed tocopherols also down-regulated the protein levels of ERα and phospho-Akt in mammary tumor tissues (Fig. 3C). However, the expression of total Akt and COX-2 protein in NMU-induced mammary tumor tissues was not significantly changed by treatment with mixed tocopherols (Fig. 3C).
Fig. 3.
Mixed tocopherols (MT) regulate the markers of apoptosis and cell proliferation, as well as the expression of nuclear receptors, PPAR-γ and ER-α, in NMU-induced mammary tumors. A. Mammary tumor tissues were stained with H&E and immunostained with cleaved caspase-3 and PPAR-γ antibodies. Representative sections in mammary tumor tissues from the control group or mixed tocopherols-fed groups (0.1, 0.3, and 0.5%) are shown. B. mRNA level of PPAR-γ and ER-α in tumors from the control group and those from mixed tocopherols-fed groups (0.1, 0.3, and 0.5%) were determined by quantitative PCR. Five different tumors from each group were analyzed and the average value of mRNA expression levels was shown. Significant difference was determined by the Student's t-test (*p <0.05, **p < 0.01, *** p< 0.001). C. The expression levels of protein markers in mammary tumors were determined by Western blot analysis. Three tumor tissues from each group were randomly selected and pooled for protein analysis. The antibodies against p21, p27, cleaved caspase-3, and PARP were used to probe for the indicated proteins. The levels of ER-α, p-Akt, Akt and COX-2 were also determined as described in the Materials and Methods section.
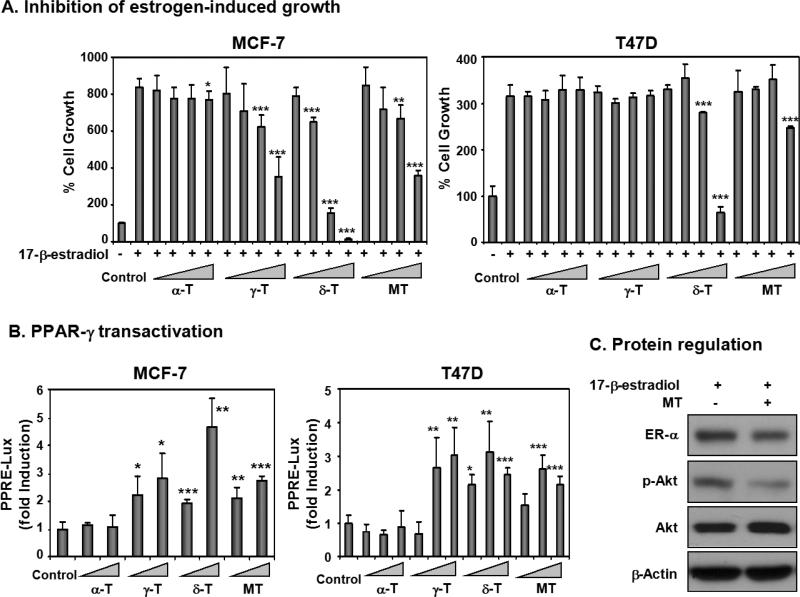
γ- and δ-Tocopherols inhibit estradiol-induced cell proliferation in ER-positive human breast cancer cells
We next investigated whether the tumor inhibitory effect of mixed tocopherols is due to the regulation of estrogen action in the breast. Since we found significant inhibitory effect of mixed tocopherols in ER-positive animal model of breast cancer in rats, we chose ER-positive human breast cancer cell lines, MCF-7 and T47D for further analysis in vitro (32). We used 10% charcoal stripped FBS/phenol red free RPMI medium to determine the possible anti-estrogenic action of the compounds. As shown in Fig. 4A, α-tocopherol (10, 30, 60, and 100 μM final concentration) did not significantly inhibit the growth of MCF-7 and T47D cells. Mixed tocopherols, γ-tocopherol and δ-tocopherol inhibited the estrogen-induced cell proliferation in MCF-7 cells. δ-Tocopherol markedly inhibited estrogen-induced cell proliferation in both MCF-7 and T47D cells in a dose-dependent manner.
Fig. 4.
Mixed tocopherols (MT), γ-tocopherol (γ-T) and δ-tocopherol (δ-T), exert anti-estrogenic activity and activate PPAR-γ in ER-positive human breast cancer cells. A. Inhibition of estrogen-induced growth of MCF-7 and T47D by mixed tocopherols and individual tocopherol isoforms. MCF-7 and T47D cells were treated with tocopherols (10, 30, 60, and 100 μM) in 10% charcoal stripped FBS/phenol red free RPMI medium for 3 days, together with 17-β-estradiol (10 pM), and the cell proliferation was compared using [3H]thymidine uptake assay. Statistical significance, *p < 0.05, **p < 0.01, ***p<0.001. B. PPAR-γ transactivation by mixed tocopherols and individual tocopherol isoforms. MCF-7 and T47D cells were transfected with DNA vectors (50 ng PPAR-γ, 40 ng PPRE-Luc, 50 ng, RXR-α, and 10 ng β-gal in 24-well plates) for 4 h in serum-free media. Then, cells were treated with compounds (50 and 100 μM in MCF-7 cells and 20, 50, and 100 μM in T47D cells) for additional 36 h in 10% charcoal stripped FBS in phenol red free RPMI. Luciferase activity was measured with a luminometer and normalized by β-galactosidase activity. Statistical significance, *p < 0.05, **p < 0.01, ***p<0.001. C. The effect of protein expression by mixed tocopherols (100 μM) in the presence of 17-β-estradiol (10 pM) in MCF-7 cells. After the incubation of 17-β-estradiol and mixed tocopherols for 24 h, the protein levels of ER-α, p-Akt, Akt, and β-actin were determined.
γ- and δ-Tocopherols, but not α-tocopherol, enhance the transactivation of PPAR-γ in ER-positive human breast cancer cells
PPAR-γ, which belongs to the nuclear receptor family, is known to be important for inhibition of experimental breast cancer (33-35). Since we found that mixed tocopherols inhibited mammary tumorigenesis and increased the expression of PPAR-γ mRNA and protein in mammary tumors, we investigated which individual isoforms activate PPAR-γ transcription in MCF-7 and T47D breast cancer cells. As shown in Fig. 4B, mixed tocopherols activated PPAR-γ transcription in MCF-7 and T47D cells. Among the tocopherol isoforms tested, α-tocopherol did not significantly activate PPAR-γ transcription, whereas γ-tocopherol, and more strongly δ-tocopherol, activated PPAR-γ transcription in MCF-7 and T47D cells (Fig. 4B).
Mixed tocopherols inhibit Akt phosphorylation and ER-α expression in MCF-7 human breast cancer cells
To determine whether the mixed tocopherols regulate the same molecular targets in vivo and in vitro, we tested the expression levels of ER-α and phospho-Akt in the presence of 17-β-estradiol in MCF-7 human breast cancer cells. As shown in Fig. 4C, mixed tocopherols down-regulated the expression of ER-α and inhibited the level of phospho-Akt without affecting total Akt.
DISCUSSION
Tocopherols are phenolic antioxidants present in a variety of vegetable oils, and the biological effects of the classic vitamin E (α-tocopherol) in cancer prevention have been investigated over many decades (3-5). However, the potential benefits of α-tocopherol in the prevention of cancer in preclinical and clinical studies were not conclusive (2, 9, 10, 36). Knowledge of the effect of other key tocopherol isomers on breast cancer formation is very limited, though recent studies suggest that γ- and δ-tocopherols have more potent anti-inflammatory and antioxidant properties than α-tocopherol (2, 16-21, 23).
Since γ-tocopherol as a pure isoform is not easily available for studying long-term dietary administration, we investigated cancer chemopreventive activity of dietary mixed tocopherols containing 57% γ-tocopherol and 24% δ-tocopherol in the NMU-induced mammary tumor model in rats. Oral administration of 500 mg of mixed tocopherols (containing 60% γ-tocopherol) daily to human subjects (37) resulted in levels of serum γ-tocopherol similar to what was observed with a 0.1% mixed tocopherol diet in rats (Table 1). The dose of mixed tocopherols used in humans (500 mg per day) is approximately 0.1% of a 2000 kcal daily diet, so a rough correlation of supplemented serum levels in humans and in rats in the present study seems reasonable. We found that mixed tocopherols significantly suppressed mammary tumor growth, tumor burden, and tumor multiplicity in a dose-dependent fashion without affecting body weight (Figs. 2A-2D). We further determined that administration of mixed tocopherols induced apoptosis, inhibited cell proliferation, and regulated the nuclear receptors, PPAR-γ and ER-α, in mammary tumors (Fig. 3).
Estrogen receptor (ER) is one of the most important markers involved in human breast carcinogenesis. Administration of selective estrogen receptor modulators (SERMs) such as tamoxifen and raloxifene have significantly reduced the risk of ER-positive breast cancer (38, 39). In our study, we found that mixed tocopherols down-regulated the expression of ER-α in mammary tumor tissues (Fig. 3B and 3C) and in ER-positive MCF-7 human breast cancer cells (Fig. 4C). Among the tocopherol isoforms tested, γ-tocopherol and more strikingly δ-tocopherol significantly inhibited estradiol-induced growth of ER-positive human breast cancer cells (Fig. 4A). α-Tocopherol is tri-methylated at the 5-, 7-, and 8-positions of the chromanol ring, whereas γ-tocopherol is dimethylated at the 7- and 8-positions and δ-tocopherol is monomethylated at the 8-position (Fig. 1). The difference in the chromanol ring structure may, in part, contribute to different anti-estrogenic activities of each isoform. Our studies suggest that δ- and/or γ-tocopherols may inhibit ER-positive tumor growth by altering the cellular response to estrogen.
Interestingly, the tocopherols may regulate another nuclear receptor, PPAR-γ, due to the structural similarity to a known PPAR-γ activator, troglitazone (28). The ligands for PPAR-γ have shown growth inhibitory effects on different tumor cell types such as colon (40, 41), lung (42) and breast cancer (33, 43), and nuclear expression of PPAR-γ was reported to be associated with a lower risk of recurrence of women's breast ductal carcinoma in-situ (DCIS) (44). Therefore, PPAR-γ has been considered as a molecular target for cancer chemoprevention (33, 34). Here, we demonstrated that mixed tocopherols markedly induced the mRNA and protein expression of PPAR-γ in mammary tumors (Fig. 3A and 3B). In addition, γ-, δ-, and mixed tocopherols (but not α-tocopherol) significantly increased the transactivation of PPAR-γ in ER-positive MCF-7 and T47D human breast cancer cells (Fig. 4B). Since ER-α has been shown to bind to PPAR response element and repress transactivation of the PPAR-γ (45), it is likely that activation of PPAR-γ may mediate the anti-estrogenic action of tocopherols, especially for γ- and δ-tocopherols.
Bonofiglio et al reported that the PPAR-γ and ER-α pathways have an opposite effect on the regulation of the PI3K/Akt transduction (45). Recently, the PPAR-γ agonist, rosiglitazone, was reported to inhibit the Akt phosphorylation induced by insulin-like growth factor-1 (IGF-1) in human adrenocortical carcinoma cells (46), suggesting a possible cross-talk between the PPAR-γ and Akt signaling pathways. Interestingly, γ-tocotrienol has been demonstrated to inhibit the proliferation of mammary epithelial cells by regulating ErbB3 phosphorylation and eventually reducing Akt signaling (47, 48). We found that mixed tocopherols down-regulated the phosphorylation of Akt in both tumor tissues and MCF-7 human breast cancer cells (Fig. 3C and Fig. 4C), which may contribute to the strong induction of apoptosis in tumor tissues. Further studies are necessary to determine whether there is interaction between activation of PPAR-γ and regulation of Akt signaling by mixed tocopherols.
Ju et al recently reported that mixed tocopherols inhibit inflammation and thus prevent colon carcinogenesis in azoxymethane/dextran sulfate sodium (AOM/DSS) treated CF-1 mice (26). In breast cancer, there was a significant association between a high expression level of COX-2 and a high risk of DCIS recurrence among women with DCIS in a case-control study (44). In addition, treatment with a COX-2 inhibitor together with a PPAR-γ agonist significantly delayed mammary tumorigenesis in the C3(1)-SV40 tumor antigen mouse model (49). These studies suggest that inflammation may play a role in breast cancer. However, in our NMU-induced breast cancer model, the serum levels of PGE2 and LTB4 in Sprague Dawley rats were not changed by NMU treatment (data not shown) compared to saline treated groups, and mixed tocopherols did not affect their levels in the serum (Table 2) or in mammary tumors (data not shown). Furthermore, the protein expression level of COX-2 in mammary tumors was not changed by administration of the mixed tocopherols (Fig. 3C). Taken together, our data indicate that inflammation may not be a key factor in NMU-induced mammary tumorigenesis.
PPAR-γ and ER-α are considered important molecular targets for cancer chemoprevention, and our data demonstrated that mixed tocopherols regulate ER-α and PPAR-γ nuclear receptor signaling which may, in part, contribute to their preventive effects in mammary tumorigenesis. In conclusion, mixed tocopherols, particularly γ- and/or δ-tocopherols, are safe and effective agents for the prevention of breast cancer in animals, suggesting that γ-and δ-tocopherols should be considered for studies in humans.
ACKNOWLEDGMENTS
This work was supported in part by NIH R03 CA112642, NIH R01 CA127645 to N.S. The authors thank Maria Hyra and Lamberto R. Navoa of the Animal Facility in the Department of Chemical Biology for their technical assistance in taking care of the animals. We thank Dr. Allan Conney for helpful advice on our work.
Footnotes
Statement of Translational Relevance
Epidemiological evidence supporting a link between vitamin E (α-tocopherol) and cancer is limited, and the results of a few completed human studies with α-tocopherol are not conclusive. γ-Tocopherol, the most common form of vitamin E in the diet in the United States, has demonstrated anti-inflammatory and anti-cancer activity. Our study found inhibition of mammary tumorigenesis by dietary tocopherols rich in γ- and/or δ-tocopherols. Mechanistic studies showed that the inhibitory activity was associated with activating PPAR-γ and antagonizing estrogen receptor signaling in mammary tumors. PPAR-γ and ER-α are considered important molecular targets for breast cancer prevention, and our data demonstrated that γ- and δ-tocopherols activate PPAR-γ transcription and inhibit estrogen action. We anticipate that γ- and δ-tocopherols may be major anti-tumorigenic agents, suggesting that γ- and δ-tocopherols should be considered for studies in humans.
REFERENCES
- 1.Wang X, Quinn PJ. Vitamin E and its function in membranes. Prog Lipid Res. 1999;38:309–36. doi: 10.1016/s0163-7827(99)00008-9. [DOI] [PubMed] [Google Scholar]
- 2.Constantinou C, Papas A, Constantinou AI. Vitamin E and cancer: An insight into the anticancer activities of vitamin E isomers and analogs. International journal of cancer. 2008;123:739–52. doi: 10.1002/ijc.23689. [DOI] [PubMed] [Google Scholar]
- 3.Traber MG. Vitamin E. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, editors. Modern Nutrition in Health and Disease. 10th ed. Lippincott Williams and Wilkins; Baltimore, MD: 2006. pp. 396–411. [Google Scholar]
- 4.Traber MG. Vitamin E regulatory mechanisms. Annual review of nutrition. 2007;27:347–62. doi: 10.1146/annurev.nutr.27.061406.093819. [DOI] [PubMed] [Google Scholar]
- 5.Traber MG, Atkinson J. Vitamin E, antioxidant and nothing more. Free radical biology & medicine. 2007;43:4–15. doi: 10.1016/j.freeradbiomed.2007.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dietary reference intakes for vitamin C, vitamin E, selenium and carotenoids. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 7.Brigelius-Flohe R, Traber MG. Vitamin E: function and metabolism. Faseb J. 1999;13:1145–55. [PubMed] [Google Scholar]
- 8.Hensley K, Benaksas EJ, Bolli R, et al. New perspectives on vitamin E: gamma-tocopherol and carboxyelthylhydroxychroman metabolites in biology and medicine. Free radical biology & medicine. 2004;36:1–15. doi: 10.1016/j.freeradbiomed.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Brigelius-Flohe R, Kelly FJ, Salonen JT, Neuzil J, Zingg JM, Azzi A. The European perspective on vitamin E: current knowledge and future research. The American journal of clinical nutrition. 2002;76:703–16. doi: 10.1093/ajcn/76.4.703. [DOI] [PubMed] [Google Scholar]
- 10.Kline K, Lawson KA, Yu W, Sanders BG. Vitamin E and cancer. Vitamins and hormones. 2007;76:435–61. doi: 10.1016/S0083-6729(07)76017-X. [DOI] [PubMed] [Google Scholar]
- 11.The ATBC Cancer Prevention Study Group The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. Ann Epidemiol. 1994;4:1–10. doi: 10.1016/1047-2797(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 12.Heinonen OP, Albanes D, Virtamo J, et al. Prostate cancer and supplementation with alpha-tocopherol and beta-carotene: incidence and mortality in a controlled trial. Journal of the National Cancer Institute. 1998;90:440–6. doi: 10.1093/jnci/90.6.440. [DOI] [PubMed] [Google Scholar]
- 13.Lonn E, Bosch J, Yusuf S, et al. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. Jama. 2005;293:1338–47. doi: 10.1001/jama.293.11.1338. [DOI] [PubMed] [Google Scholar]
- 14.Lee IM, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women's Health Study: a randomized controlled trial. Jama. 2005;294:56–65. doi: 10.1001/jama.294.1.56. [DOI] [PubMed] [Google Scholar]
- 15.Huang HY, Alberg AJ, Norkus EP, Hoffman SC, Comstock GW, Helzlsouer KJ. Prospective study of antioxidant micronutrients in the blood and the risk of developing prostate cancer. American journal of epidemiology. 2003;157:335–44. doi: 10.1093/aje/kwf210. [DOI] [PubMed] [Google Scholar]
- 16.Stone WL, Krishnan K, Campbell SE, Qui M, Whaley SG, Yang H. Tocopherols and the treatment of colon cancer. Annals of the New York Academy of Sciences. 2004;1031:223–33. doi: 10.1196/annals.1331.022. [DOI] [PubMed] [Google Scholar]
- 17.McIntyre BS, Briski KP, Gapor A, Sylvester PW. Antiproliferative and apoptotic effects of tocopherols and tocotrienols on preneoplastic and neoplastic mouse mammary epithelial cells. Proc Soc Exp Biol Med. 2000;224:292–301. doi: 10.1046/j.1525-1373.2000.22434.x. [DOI] [PubMed] [Google Scholar]
- 18.Jiang Q, Wong J, Fyrst H, Saba JD, Ames BN. gamma-Tocopherol or combinations of vitamin E forms induce cell death in human prostate cancer cells by interrupting sphingolipid synthesis. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:17825–30. doi: 10.1073/pnas.0408340102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dietrich M, Traber MG, Jacques PF, Cross CE, Hu Y, Block G. Does gamma-tocopherol play a role in the primary prevention of heart disease and cancer? A review. J Am Coll Nutr. 2006;25:292–9. doi: 10.1080/07315724.2006.10719538. [DOI] [PubMed] [Google Scholar]
- 20.Jiang Q, Elson-Schwab I, Courtemanche C, Ames BN. gamma-tocopherol and its major metabolite, in contrast to alpha-tocopherol, inhibit cyclooxygenase activity in macrophages and epithelial cells. Proceedings of the National Academy of Sciences of the United States of America. 2000;97:11494–9. doi: 10.1073/pnas.200357097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang Q, Ames BN. Gamma-tocopherol, but not alpha-tocopherol, decreases proinflammatory eicosanoids and inflammation damage in rats. Faseb J. 2003;17:816–22. doi: 10.1096/fj.02-0877com. [DOI] [PubMed] [Google Scholar]
- 22.Christen S, Woodall AA, Shigenaga MK, Southwell-Keely PT, Duncan MW, Ames BN. gamma-tocopherol traps mutagenic electrophiles such as NO(X) and complements alpha-tocopherol: physiological implications. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:3217–22. doi: 10.1073/pnas.94.7.3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jiang Q, Lykkesfeldt J, Shigenaga MK, Shigeno ET, Christen S, Ames BN. Gamma-tocopherol supplementation inhibits protein nitration and ascorbate oxidation in rats with inflammation. Free radical biology & medicine. 2002;33:1534–42. doi: 10.1016/s0891-5849(02)01091-2. [DOI] [PubMed] [Google Scholar]
- 24.Newmark HL, Huang MT, Reddy BS. Mixed tocopherols inhibit azoxymethane-induced aberrant crypt foci in rats. Nutr Cancer. 2006;56:82–5. doi: 10.1207/s15327914nc5601_11. [DOI] [PubMed] [Google Scholar]
- 25.Suh N, Paul S, Lee HJ, et al. Mixed Tocopherols Inhibit N-methyl-N-Nitrosourea-Induced Mammary Tumor Growth in Rats. Nutr Cancer. 2007;59:76–81. doi: 10.1080/01635580701419022. [DOI] [PubMed] [Google Scholar]
- 26.Ju J, Hao X, Lee MJ, et al. A gamma-tocopherol-rich mixture of tocopherols inhibits colon inflammation and carcinogenesis in azoxymethane and dextran sulfate sodium-treated mice. Cancer Prev Res. 2009;2:143–52. doi: 10.1158/1940-6207.CAPR-08-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamras H, Barsky SH, Ardashian A, Navasartian D, Heber D, Glaspy JA. Novel interactions of vitamin E and estrogen in breast cancer. Nutr Cancer. 2005;52:43–8. doi: 10.1207/s15327914nc5201_6. [DOI] [PubMed] [Google Scholar]
- 28.Campbell SE, Stone WL, Whaley SG, Qui M, Krishnan K. Gamma (gamma) tocopherol upregulates peroxisome proliferator activated receptor (PPAR) gamma (gamma) expression in SW 480 human colon cancer cell lines. BMC Cancer. 2003;3:25. doi: 10.1186/1471-2407-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y, Porter WW, Suh N, et al. A synthetic triterpenoid, 2-cyano-3,12-dioxooleana-1,9-dien-28-oic acid (CDDO), is a ligand for the peroxisome proliferator-activated receptor gamma. Molecular endocrinology (Baltimore, Md. 2000;14:1550–6. doi: 10.1210/mend.14.10.0545. [DOI] [PubMed] [Google Scholar]
- 30.Yang CS, Lee MJ. Methodology of plasma retinol, tocopherol, and carotenoid assays in cancer prevention studies. J Nutr Growth Cancer. 1987;4:19–27. [Google Scholar]
- 31.Lee HJ, Liu H, Goodman C, et al. Gene expression profiling changes induced by a novel Gemini Vitamin D derivative during the progression of breast cancer. Biochem Pharmacol. 2006;72:332–43. doi: 10.1016/j.bcp.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 32.Chan MM, Lu X, Merchant FM, Iglehart JD, Miron PL. Gene expression profiling of NMU-induced rat mammary tumors: cross species comparison with human breast cancer. Carcinogenesis. 2005;26:1343–53. doi: 10.1093/carcin/bgi100. [DOI] [PubMed] [Google Scholar]
- 33.Suh N, Wang Y, Williams CR, et al. A new ligand for the peroxisome proliferator-activated receptor-gamma (PPAR-gamma), GW7845, inhibits rat mammary carcinogenesis. Cancer research. 1999;59:5671–3. [PubMed] [Google Scholar]
- 34.Brown PH, Lippman SM. Chemoprevention of breast cancer. Breast Cancer Res Treat. 2000;62:1–17. doi: 10.1023/a:1006484604454. [DOI] [PubMed] [Google Scholar]
- 35.Fenner MH, Elstner E. Peroxisome proliferator-activated receptor-gamma ligands for the treatment of breast cancer. Expert Opin Investig Drugs. 2005;14:557–68. doi: 10.1517/13543784.14.6.557. [DOI] [PubMed] [Google Scholar]
- 36.Gould MN, Haag JD, Kennan WS, Tanner MA, Elson CE. A comparison of tocopherol and tocotrienol for the chemoprevention of chemically induced rat mammary tumors. The American journal of clinical nutrition. 1991;53:1068S–70S. doi: 10.1093/ajcn/53.4.1068S. [DOI] [PubMed] [Google Scholar]
- 37.Clarke MW, Ward NC, Wu JH, Hodgson JM, Puddey IB, Croft KD. Supplementation with mixed tocopherols increases serum and blood cell gamma-tocopherol but does not alter biomarkers of platelet activation in subjects with type 2 diabetes. Am J Clin Nutr. 2006;83:95–102. doi: 10.1093/ajcn/83.1.95. [DOI] [PubMed] [Google Scholar]
- 38.Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. Journal of the National Cancer Institute. 2005;97:1652–62. doi: 10.1093/jnci/dji372. [DOI] [PubMed] [Google Scholar]
- 39.Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. Jama. 2006;295:2727–41. doi: 10.1001/jama.295.23.joc60074. [DOI] [PubMed] [Google Scholar]
- 40.Tanaka T, Kohno H, Yoshitani S, et al. Ligands for peroxisome proliferator-activated receptors alpha and gamma inhibit chemically induced colitis and formation of aberrant crypt foci in rats. Cancer research. 2001;61:2424–8. [PubMed] [Google Scholar]
- 41.Osawa E, Nakajima A, Wada K, et al. Peroxisome proliferator-activated receptor gamma ligands suppress colon carcinogenesis induced by azoxymethane in mice. Gastroenterology. 2003;124:361–7. doi: 10.1053/gast.2003.50067. [DOI] [PubMed] [Google Scholar]
- 42.Keshamouni VG, Reddy RC, Arenberg DA, et al. Peroxisome proliferator-activated receptor-gamma activation inhibits tumor progression in non-small-cell lung cancer. Oncogene. 2004;23:100–8. doi: 10.1038/sj.onc.1206885. [DOI] [PubMed] [Google Scholar]
- 43.Yee LD, Williams N, Wen P, et al. Pilot study of rosiglitazone therapy in women with breast cancer: effects of short-term therapy on tumor tissue and serum markers. Clin Cancer Res. 2007;13:246–52. doi: 10.1158/1078-0432.CCR-06-1947. [DOI] [PubMed] [Google Scholar]
- 44.Kulkarni S, Patil DB, Diaz LK, Wiley EL, Morrow M, Khan SA. COX-2 and PPARgamma expression are potential markers of recurrence risk in mammary duct carcinoma in-situ. BMC cancer. 2008;8:36. doi: 10.1186/1471-2407-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bonofiglio D, Gabriele S, Aquila S, et al. Estrogen receptor alpha binds to peroxisome proliferator-activated receptor response element and negatively interferes with peroxisome proliferator-activated receptor gamma signaling in breast cancer cells. Clin Cancer Res. 2005;11:6139–47. doi: 10.1158/1078-0432.CCR-04-2453. [DOI] [PubMed] [Google Scholar]
- 46.Giulia C, Adriana L, Elisabetta P, et al. Rosiglitazone Inhibits Adrenocortical Cancer Cell Proliferation by Interfering with the IGF-IR Intracellular Signaling. PPAR research. 2008;2008:904041. doi: 10.1155/2008/904041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shah SJ, Sylvester PW. Gamma-tocotrienol inhibits neoplastic mammary epithelial cell proliferation by decreasing Akt and nuclear factor kappaB activity. Experimental biology and medicine (Maywood, NJ. 2005;230:235–41. doi: 10.1177/153537020523000402. [DOI] [PubMed] [Google Scholar]
- 48.Samant GV, Sylvester PW. gamma-Tocotrienol inhibits ErbB3-dependent PI3K/Akt mitogenic signalling in neoplastic mammary epithelial cells. Cell proliferation. 2006;39:563–74. doi: 10.1111/j.1365-2184.2006.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mustafa A, Kruger WD. Suppression of tumor formation by a cyclooxygenase-2 inhibitor and a peroxisome proliferator-activated receptor gamma agonist in an in vivo mouse model of spontaneous breast cancer. Clin Cancer Res. 2008;14:4935–42. doi: 10.1158/1078-0432.CCR-08-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]