Abstract
The objective of our study was to investigate whether life satisfaction and depressive symptoms are independent predictors of mortality in a non-Western sample of adults. The sample included 5,131 adults (aged 50 – 95 at baseline) in Taiwan who participated in the Survey of Health and Living Status of the Near Elderly and Elderly. There were 1,815 deaths recorded over a 10-year period. Higher life satisfaction significantly predicted lower risk of mortality after controlling for age, sex, education, marital status and health status. Depressive symptoms significantly predicted higher risk of mortality. A significant interaction with age revealed that the protective effect of life satisfaction weakened with age. The results suggest that life satisfaction and depressive symptoms independently predict mortality risk in adults.
Keywords: life satisfaction, depressive symptoms, mortality, Taiwan
Introduction
Prospective studies have shown that positive well-being influences risk of adverse medical events and mortality. In the present study, we focus on the association between mortality risk and two psychological variables that are frequently measured in demographic and health surveys—life satisfaction and depressive symptoms—during a ten year follow-up of adults in Taiwan.
Many studies demonstrate that depressive symptoms increase the risk of mortality in adults (Blazer, 2003). In the U.S., the effect appears to be similar among Whites, African Americans and Hispanics, but may be stronger for men compared to women (Schulz, Drayer, & Rollman, 2002). Researchers are increasingly attentive to the mechanisms through which depressive symptoms impact health and mortality. For example, there is a strong relationship between depressive symptoms and cardiovascular disease and mortality, suggesting that the physiological consequences of psychological distress may lead to higher risk for mortality. (Schulz et al., 2002).
Other studies have focused on the role of positive mental well-being in health and mortality (Koivumaa-Honkanen et al., 2000; Lyyra, Törmäkangas, Read, & Taina Berg, 2006; Maier & Smith, 1999). Positive well-being is not simply the absence of negative well-being (Diener, Scollon & Lucas, 2003). Studies suggest that positive and negative well-being involve distinct activation of physiological and neurobiological systems.(Hamer, 1996; Panksepp & Miller, 1996; Pressman & Cohen, 2005; Ryff et al., 2006) and operate in parallel rather than being bi-polar opposites (Cacioppo & Bernston, 1999; Cacioppo, Garnder, & Bernston, 1999). It is generally accepted that there are three independent facets of positive well-being: positive affect, negative affect and life satisfaction (Diener et al., 2003). Although there have been studies examining the connections between all of these facets and health, we focus on life satisfaction because it reflects current quality of life judgments that are based on individuals’ own criteria for success and happiness (Okun & Stock, 1987) and may be more stable than measures of affect (Schimmack & Oishi, 2005). Life satisfaction measures vary in their composition, but generally, they tap trait levels of positive affect as well as cognitive assessments of the extent to which a person’s life matches his or her expectations (Okun & Stock, 1987).
Life satisfaction has been shown to predict mortality risk in Western populations (Lyyra, Tormakangas, Read, & Taina Berg, 2006; Maier & Smith, 1999). Lyyra et al. (2006) found that lower life satisfaction increased risk of dying in a community based sample of octogenarians (N=320). In a sample of adults from the Berlin Aging Study (N=516), satisfaction with aging predicted lower mortality risk of adults over a three-year period (Maier & Smith, 1999). Studies using population representative samples have shown associations between life satisfaction and fatal injury and all-cause mortality. Koivumaa-Honkanen et al. (2000) found that life dissatisfaction was a predictor of fatal injury during a 20-year follow-up (Koivumaa-Honkanen, Honkanen, Koskenvuo, Viinamaki, & Kaprio, 2002). Life satisfaction exerted a significant protective effect on all-cause mortality in a 20-year prospective cohort study of Finnish adults, although the relationship was significant only for men and was partially mediated by health related behaviors (Koivumaa-Honkanen et al., 2000).
Theoretical models of successful aging identify the pathways through which having higher life satisfaction over the lifespan may be beneficial to health. For example, life satisfaction may reveal how well one has adapted to the cumulative losses associated with aging (Brandstadter & Greve, 1994; Folkman, 1997; Rothbaum, Weisz & Snyder, 1982). Studies of coping in adulthood suggest that individuals use “assimilative” and “accommodative” actions to stabilize and protect their mental well-being from the biological, psychological and social changes inherent in the aging process (Brandstadter & Greve, 1994). In the context of health, assimilative activities can involve efforts to make positive lifestyle changes such as implementing and maintaining health regimens or fitness, and may also include compensatory behaviors, such as using external aids to improve physical functioning. Accommodative behaviors involve negotiating desired goals and expectations. Higher life satisfaction and a positive view of self is an indication of an individual’s flexibility in disengaging from or adjusting goals that are no longer attainable (Brandstadter & Renner, 1992; Rasmussen, Wrosch, Scheier & Carver, 2006). For example, Cheng (2004) found that while the gap between individuals’ desired and actual selves in the domain of health increases with age, the psychological impact of this discrepancy is compensated for by fewer discrepancies in other domains (e.g., relational). Life satisfaction does not appear to be greatly affected by aging related deficits in health because of individuals’ behavioral and psychological adjustment. Thus, higher life satisfaction may be an indication of how well individuals have coped with increased discrepancies in health as they age.
Several studies have shown that psychological variables may matter less to health at older ages (Schulz, et al., 1996), while others have found that the relationship strengthens with age (Duberstein, Sorensen, Lyness, King, Conwell, et al., 2003). The former outcome suggests that psychological variables become less important in the face of age-related health decline while the latter indicates that physical vulnerability amplifies the effects of negative well-being (e.g. high neuroticism) (Duberstein et al., 2003). We address the possibility that the relationship between psychological variables and mortality changes with age by including both life satisfaction and depressive symptoms as well as interactions between age and the psychological variables in our models. We also include extensive controls for health status in order to reduce the possibility that poorer health drives the relationship between life satisfaction and mortality.
Another important feature of the present study is its focus on the relationship between life satisfaction and health in a non-Western sample. A previous study of the Survey of Health and Living Status found that life satisfaction was a significant predictor of the survival of adults in Taiwan even with controls for SES and several measures of objective health status (Mete, 2005). However, Mete (2005) found that the relationship was largely accounted for by self-evaluated health. We build on Mete’s (2005) study by analyzing three additional years of follow-up survey data. We also include depressive symptoms as well as interactions between the psychological variables and age. Given the previous literature demonstrating associations between both life satisfaction and depressive symptoms and mortality, we tested whether life satisfaction and depressive symptoms independently predicted mortality in a Chinese sample over a ten year follow-up period (1996 – 2006).
Method
Study Participants
The data come from a nationally-representative random sample of adults (aged 50 – 95) in Taiwan who participated in the Survey of Health and Living Status of the Near Elderly and Elderly. The oldest cohort comprises 4,049 respondents (aged 60 and up) who were first interviewed in 1989; in 1996, a cohort of 2,462 respondents (aged 50 – 66) was added. Follow-up interviews were conducted with both cohorts in 1999 (n = 4,440; 90% of survivors) and 2003 (n = 3,778; 92% of survivors) (Chang & Hermalin, 1998a; Chang & Hermalin, 1998b; Hermalin, Liang, & Chang, 1989). Survival status (as of December 31, 2006) and date of death were verified by linking the survey data to the Death Certificate file maintained by the Taiwan Department of Health and to the Household Registration file constructed by the Taiwanese Ministry of the Interior. In the current analysis, we use interview data from 1996, 1999 and 2003 and survival status through 2006. The available sample comprises 5,131 survivors at the time of the 1996 survey, 1,815 of whom died by December 31, 2006 (1,102 men and 714 women). Decedents were observed an average of 5.1 years (range 0.01 – 10.6) prior to their death, whereas those who survived to 2006 were followed for an average of 10.2 years (range 2.9 – 10.7). The average number of years between the date of the last interview and death was 1.75 years for those under age 63, 1.79 years for those between the ages of 63 and 77, and 1.65 years for those over age 78.
Respondents who were lost-to-follow-up (LFU) during the observation period included individuals who were alive but not interviewed, those who were missing data on the variables in the analysis, individuals who had unknown vital status, and individuals who had emigrated before December 31, 2006. Four hundred sixteen respondents had no valid data in 1996, 1999 and 2003, and thus were excluded from the analysis. There were 3,668 respondents with complete data. The remaining 1,365 respondents had valid data for at least one wave but were LFU for one or two waves; these respondents did not contribute data for periods in which they were LFU. For example, if a respondent was interviewed in 1996, LFU in 1999, and interviewed in 2003, s/he would contribute data for 1996-1998 and 2003-2006 (but not 1999-2002). Persons who had unknown vital status or who emigrated were censored at their last date of interview.
We compared the sociodemographic characteristics of respondents who were LFU for one or more waves to those with complete data (n = 3,668). Respondents who had no valid data for any of the three waves (n = 416) were significantly (p < .001) older at baseline (M = 74.46, SD = 9.06) and had fewer years of education (M = 3.52, SD = 4.71) compared to those with complete data (M = 65.53, SD = 8.95 and M = 4.82, SD = 4.55, respectively). Similarly, those who were LFU for one or two waves (n = 1,365) were significantly (p < .001) older at baseline (M = 68.87, SD = 10.00) and had fewer years of education (M = 4.27, SD = 4.71) compared to those with complete data.
Measures
Life Satisfaction
Life satisfaction was measured using items adapted from the 20-item Life Satisfaction Index (LSIA) (Neugarten, Havighurst, & Tobin, 1961) and modified for use with Taiwanese respondents. Subscales of the LSIA are comparable to other measures of life satisfaction that are typically used (Nezlek, Richardson, Green & Schatten-Jones, 2002; Stock, Okun, & Benin, 1986). Still, the LSIA has been shown to encompass other aspects of subjective well-being compared to more recent measures of life satisfaction, such as Diener’s Satisfaction with Life Scale (Diener, Emmons, Larsen & Griffin, 1985). For example, the LSIA captures mood tone, zest versus apathy, congruence between desired and achieved goals, and self-concept (Okun & Stock, 1987; Neugarten et al., 1961).
We originally used eight items adapted from the LSIA. We removed two items because we found that they cross-loaded with the CES-D. We removed one additional item because we discovered an inconsistency in respondents’ answers to the question. The remaining five items loaded highly on one factor (eigenvalues were 3.83 in 1996, 2.56 in 1999 and 2.30 in 2003). We calculated Cronbach’s alpha for three age groups: up to age 62, age 63-77 and age 78 and up. Cronbach’s alpha for these five items ranged from .78 to .85 across the three waves for all age groups, with values being highest for the oldest group (.84 in 1996, .85 in 1999 and .83 in 2003). The five items loaded on one factor for all age groups. The interviewers made the following statement to the respondents before asking questions about their life (in Mandarin): “I’d like to ask for your current views or feelings about your life. Please tell me whether you agree with the sentences I am about to read.” We used the following five items from the scale to represent life satisfaction, each of which required a Yes/No response (0 = No; 1 = Yes):
Has your life been better than most people’s lives?
Are you satisfied with your life?
Do you find what you do interesting?
Have these few years been the best in your life?
Would you say your life has matched your hopes?
Summing across the items produced a score with a potential range of 0 (low) to 5 (high life satisfaction).
Depressive Symptoms
Depressive Symptoms were measured using a subset of eight items from the 20-item Center for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977). Shorter forms of the CES-D have demonstrated reliability in Western populations (Andresen, Carter, Malmgren & Patrick, 1994; Kohout, Berkman, Evans & Cornoni-Huntley, 1993), as well as in elderly Chinese (Boey, 1999) and other Chinese populations (Krause et al., 1992; Ofstedal et al., 1999).
Respondents reported whether they had experienced a number of different situations or feelings in the past week (0 = no) and how often they experienced these feelings (1 = rarely or one day; 2 = sometimes or 2 to 3 days; and 3 = often/chronically or 4 or more days). We originally used ten items from the CES-D but removed two items because they cross-loaded with the LSIA. The eight remaining items include questions about poor appetite, exhaustion, poor sleep, bad mood, loneliness, unfriendliness of others, anguish, unable to get oneself going. All items were scored in the same direction and summed to create the depressive symptom scale. The scale ranges from 0 to 24, with higher scores indicating more frequent depressive symptoms. We calculated Cronbach’s alpha for three age groups across the three waves: up to age 62, age 63-77 and age 78 and up. Cronbach’s alpha for these eight items ranged from .82 to .86 across the three waves for all age groups, with values being highest for the oldest age group in all three waves (.86 in 1996, .86 in 1999 and .84 in 2003).
Control variables
We added sociodemographic and health variables that are related to both psychological well-being and mortality. The variables included sex and educational attainment (as of 1996), age, marital status, self-assessed health, chronic conditions, cognitive function, mobility limitations, smoking status and alcohol consumption. Self-assessed health (SAH) was measured using one question that asks respondents to rate their overall health in one of five categories (1 = excellent, 2=good, 3=average, 5=not so good, or 5=poor). Measures of SAH are widely used and have been shown to be powerful predictors of survival and functional decline, regardless of how the questions are phrased (Benyamini & Idler, 1999; Goldman & Glei, 2004; Haga, Shibata, Suyama, Suzuki, Iwasaki, Suzuki & Yasumura, 1995; Idler & Benyamini, 1997; Idler & Kasl, 1995; Kaplan, Strawbridge, Camacho & Cohen, 1993; Mossey & Shapiro, 1982). Based on the respondent’s report of current chronic conditions, we include separate count measures for six “serious” conditions (high blood pressure, diabetes, heart disease, cancer, liver disease, kidney disease --all of which are among the top ten leading causes of death in Taiwan) and six “other” conditions (respiratory ailment, arthritis/rheumatism, ulcer/gastrointenstinal disorder, cataracts, gout, spinal spurs). Cognitive function was based on items from the modified Rey Auditory Verbal Learning Test (Lezak, 1983) and a modification of the Digits Backward Test (Wechsler, 1981). Respondents received one point for every word they correctly recalled out of a possible ten. They were then asked to recall a list of five numbers in reverse order. If they recalled all five numbers correctly in reverse order (in one trial), they received one point. The number of words correctly recalled from the Rey Auditory Verbal Learning Test was summed with the 0 or 1 point received for the Digits Backward Test. The measure was reverse scored so that a higher number of points indicated poorer cognitive function in order to be consistent with the other health measures (potential range was 0 to 11). Mobility limitations included the number of mobility activities for which the respondent had any difficulty (potential range was 0 to 8). These activities include standing for 15 minutes, squatting, reaching over one’s head, grasping with fingers, lifting/carrying 11-12 kilograms, running 20-30 meters, walking 200-300 meters, and climbing 2-3 flights of stairs (Nagi, 1969; 1976). We also included smoking status and whether or not respondents drank alcohol. Respondents were asked (in Mandarin), “Do you currently smoke?” (0 = No; 1 = Yes) and “Do you drink alcohol?” (0 = No; 1 = Yes).
Data Analysis
Three separate models were estimated in order to examine the effects of life satisfaction and depressive symptoms individually and then simultaneously. Both life satisfaction and the CES-D were time-varying. Control variables were fixed variables (sex and educational attainment as of 1996) as well as the time-varying measures of age, marital status, self-assessed health, chronic conditions, cognitive function, mobility limitations, smoking status and alcohol consumption. For each year of age, we evaluated whether death occurred and the length of exposure length of exposure (i.e., proportion of the age year from the beginning of observation until death or the end of observation). For time-varying measures other than age, the values at a given observation year (1996, 1999, 2003) were used to predict mortality between that wave and the next wave.
We used a piecewise exponential hazards model to predict age-specific mortality in the period 1996-2006. Although we use age as the primary clock, we also control for period effects using calendar year as a continuous variable (i.e., year in which the respondent attained the specified age, which is equivalent to year of birth plus age); this variable captures the trend in mortality decline over time. This model assumes that each additional year of age is associated with an exponential increase in the risk of mortality (although the hazard is treated as constant within a given year of age). Thus, the model is similar to a Gompertz model, which assumes that the log-hazard is linear across age and has been used widely to model adult age mortality (Finch & Pike, 1996; Olshansky & Carnes, 1997; Zimmer, Martin, & Hui-Sheng, 2005).
In order to allow for non-proportional hazards, we included interactions between age (as well as calendar year) and the two variables of interest—life satisfaction and depressive symptoms. In addition, we explored interactions between the two psychological variables and measures of health status in 1996 (e.g., whether the respondent had at least one mobility limitation and whether the respondent had at least one chronic condition) because of previous work suggesting that psychological well-being may be a stronger predictor of future health status for persons who are healthier at baseline (Ostir, Ottenbacher, & Markides, 2004). We also included interactions between the psychological variables and sex. Interaction terms that were statistically significant (p < .05) were retained in the final model.
Because the distribution of the CES-D is skewed, we ran an additional model (not shown) using the log of the CES-D measure (instead of the CES-D measure itself) to explore whether outliers are exerting undue influence on the results; the results were substantively unchanged. To ease comparability of the coefficients, we used standardized versions of the life satisfaction and the CES-D measures in the models. All analyses were performed using Stata 10.0 (StataCorp, 2005).
Results
The sociodemographic characteristics and health status of the study population are shown in Table 1. At the baseline interview, the mean life satisfaction score of the sample (n = 4,627) was 3.15 (SD = 1.77). The mean CES-D score was 3.63 (SD = 4.85). The correlation between life satisfaction and the CES-D was -.48, -.47 and -.48 in 1996, 1999 and 2003, respectively.
Table 1.
Sociodemographic Characteristics and Health Status of the Study Population.
| 1996 | 1999 | 2003 | ||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Fixed Baseline Characteristics | ||||||
| Female, % | 46.1 | |||||
| Education, years | 4.72 | 4.55 | ||||
| Time Varying Covariates | ||||||
| Age, years | 65.71 | 9.14 | 68.19 | 8.88 | 70.87 | 8.30 |
| Married, % | 71.8 | 69.4 | 67.0 | |||
| Poor Self-assessed Health (1-5) | 2.80 | 1.11 | 2.85 | 1.08 | 2.92 | 1.07 |
| Serious Conditions (0-6) | .68 | .91 | .84 | .98 | 1.00 | 1.04 |
| Other Conditions (0-6) | .82 | 1.02 | 1.00 | 1.10 | 1.16 | 1.18 |
| Poor Cognitive function (0-11) | 6.66 | 2.57 | 6.79 | 2.60 | 7.44 | 2.37 |
| Mobility limitations (0-8) | 1.10 | 1.97 | 1.47 | 2.21 | 1.76 | 2.30 |
| Currently Smoking, % | 27.3 | 24.8 | 20.4 | |||
| Currently Drinking Alcohol, % | 21.6 | 25.1 | 25.0 | |||
| Life Satisfaction (0-5) | 3.15 | 1.77 | 3.16 | 1.85 | 3.26 | 1.77 |
| Depressive Symptoms (0-24) | 3.63 | 4.85 | 5.51 | 4.90 | 3.32 | 4.55 |
| Number of respondents observed | 4627 | 4224 | 3438 | |||
Table 2 presents relative risk ratios relating fixed and time-varying factors, including life satisfaction and the CES-D, to mortality during the ten year follow-up period. The first two models included either life satisfaction or depressive symptoms with controls. Both measures were included in the final model. Not surprisingly, being female, married and having better health were associated with lower mortality. After accounting for sociodemographic and health risk factors, we found that both life satisfaction and depressive symptoms had significant associations with mortality.
Table 2.
Relative Risk Ratios from Piecewise Exponential Hazard Models Relating Life Satisfaction and Depressive Symptoms to Mortality.
| Life Satisfaction | CES-D | Full Model | ||||
|---|---|---|---|---|---|---|
| Predictors | RR | SE | RR | SE | RR | SE |
| Fixed Baseline Characteristics | ||||||
| Female | 0.465 | 0.073** | 0.461 | 0.073** | 0.456 | 0.074** |
| Education | 1.001 | 0.007 | 1.001 | 0.007 | 1.000 | 0.007 |
| Time Varying Covariates | ||||||
| Control Variables | ||||||
| Age | 1.070 | 0.004** | 1.072 | 0.004** | 1.069 | 0.004** |
| Married | 0.885 | 0.064* | 0.891 | 0.064 | 0.892 | 0.065 |
| Poor Self-assessed Health | 1.251 | 0.035** | 1.226 | 0.036** | 1.227 | 0.035** |
| Serious Conditions | 1.139 | 0.029** | 1.141 | 0.029** | 1.137 | 0.029** |
| Other Conditions | 0.928 | 0.026* | 0.923 | 0.026* | 0.925 | 0.026* |
| Poor Cognitive Function | 1.045 | 0.013* | 1.044 | 0.013* | 1.043 | 0.013* |
| Mobility limitations | 1.172 | 0.013** | 1.161 | 0.014** | 1.164 | 0.014** |
| Currently Smoking | 1.270 | 0.071* | 1.162 | 0.013** | 1.271 | 0.072* |
| Currently Drinks Alcohol | 0.840 | 0.079* | 0.841 | 0.079* | 0.840 | 0.079* |
| Psychological Variables | ||||||
| Life Satisfactiona | 0.451 | 0.246* | 0.462 | 0.246* | ||
| Life Satisfactiona × Age | 1.011 | 0.003* | 1.011 | 0.003* | ||
| CES-Da | 1.829 | 0.214* | 1.083 | 0.030* | ||
| CES-D × Age | 0.993 | 0.003* | ||||
Note. We also included a control for period effects (i.e., a continuous variable indicating the calendar year in which the respondent completed a given age) in all three models; Interaction terms that were statistically significant (p < .05) were retained in the final model;
p < .05,
p < .001.
Measures of Life Satisfaction and CES-D have been standardized (M=0, SD=1).
The effects of life satisfaction and depressive symptoms change little in the full model, implying that the effects are independent. Results from the full model suggest that a one SD increase in depressive symptoms was associated with an 8.3% increase in mortality risk (RR = 1.083). The effect of life satisfaction on mortality is complicated by a significant interaction with age. At younger ages, higher levels of life satisfaction predicted lower risk of mortality, but this protective effect weakens with age. For example, a one SD increase in life satisfaction was associated with a 24% reduction in the risk of mortality for a person aged 50 (RR=.462*1.0150=0.76), but by age 78 the effect is virtually zero. Figure 1 shows how the predicted risk ratio associated with a one SD increase in life satisfaction changes with age. In fact, the results suggest that the relationship reverses after age 78— higher life satisfaction predicts higher mortality. In contrast to the significant interaction between life satisfaction and age, the interaction between depressive symptoms and age was not significant, suggesting that higher values of the depressive symptoms score continue to predict increases in mortality at the oldest ages. Interactions between the psychological variables and health and sex were not significant. In order to examine further the role that health may play in the interaction between life satisfaction and age, we re-estimated our model on a “healthy” sample (N = 2,666) that included only those respondents with no “serious” conditions and no limitations with respect to six activities of daily living. The results were consistent with those presented here. However, we found the effects were somewhat weaker among the “healthy” sample: the main effect of life satisfaction and the interaction between life satisfaction and age were attenuated and were no longer statistically significant (p = .06 and .06, respectively), in part because of the loss of statistical power when more than 40% of observations were excluded from analysis.
Figure 1.
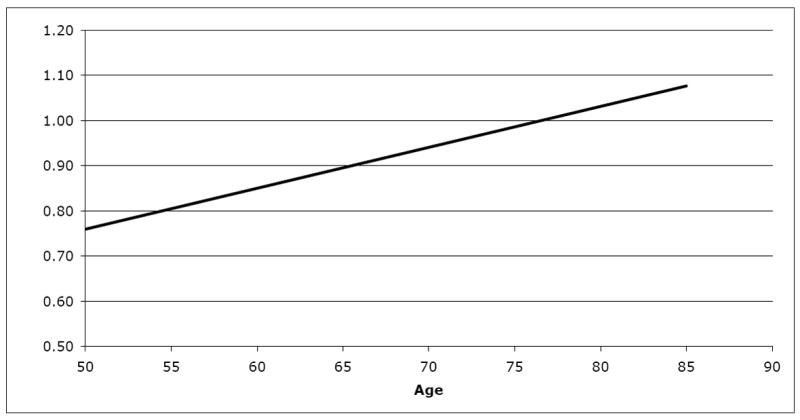
Predicted Mortality Risk Ratio for a One SD Increase in Life Satisfaction, by Age.
Discussion
The purpose of our study was to investigate whether life satisfaction and depressive symptoms are significantly related to mortality risk in a Chinese sample of adults. We build on a previous study of the Survey of Health and Living Status (Mete, 2005) by including both life satisfaction and depressive symptoms as well as interactions between the psychological variables and age. We demonstrate that both variables independently predict mortality risk. In the presence of controls for sociodemographic and health variables, life satisfaction significantly predicted lower risk of mortality (among younger persons) whereas depressive symptoms significantly predicted higher risk of mortality (at all ages).
Our study also reveals that the relationship between psychological variables and health may change with age The negative effect of life satisfaction on mortality weakened with age by age—78 the effect was virtually nil and at even older ages the association reversed whereby higher life satisfaction predicted higher mortality. This unexpected result raises an important question— why would the protective effect of life satisfaction weaken (or even reverse) with age? Using the framework given by Brandstadter & Greve (1994), we know that as adults age they tend to use fewer assimilative strategies (e.g., behavior modification) and more accommodative strategies (e.g., lowering expectations). Adults at the youngest ages are making lifestyle changes in order to reduce the discrepancy between their actual and desired selves by improving adherence to medical regimens and behaviors (e.g., better sleep, diet, exercise). In contrast, adults at the oldest ages are experiencing cumulative and irreversible deficits in health. They rely more on accommodative strategies, which are psychological adjustments that protect well-being (Brandstadter & Greve, 1994).
There are two psychological avenues one might take in the face of irreversible damage to health: denial or acceptance. Both of these coping strategies may enhance life satisfaction but may also be a health risk. For example, there is some evidence to support the idea that individuals expressing denial in the face of poor health have a higher risk of mortality (Brown et al., 2000; Derogatis, Abeloff, & Melisaratos, 1979; Devins et al., 1990). Alternatively, those who have accepted their deteriorating health may be less likely to pursue behaviors and interventions that may prolong their lives. In either case, higher life satisfaction as a result of denial or acceptance of one’s health state may indicate a higher risk of mortality. Future research should seek to validate this hypothesis by investigating the pathways through which higher life satisfaction may lead to higher risk of mortality at the oldest ages.
We should note several limitations in this study. One concern is the validity of our life satisfaction measure in a non-Western culture. Studies of life satisfaction in Chinese populations have primarily used measures that were developed in the US (Lu & Shih, 1997; Oishi, Diener, Lucas, & Suh, 1999). Measures that tap psychological traits or judgments about the self may not be meaningful in cultures that view personal characteristics as embedded in the social context, e.g., positive feelings or expectancies as a mother, as an employee, or as a citizen (Markus & Kitayama, 1998). Chinese respondents may be confused by measures that require them to assess personal traits that are removed from social context (Markus & Kitayama, 1998). Thus, it is possible that a more culturally appropriate measure would reveal a negative relationship between life satisfaction and mortality risk (i.e., higher life satisfaction predicts lower mortality) that persists with age. Second, we were limited by the availability of objective health measures over multiple survey waves. We do include data on current alcohol consumption, but the “yes” or “no” responses provide minimal information. Thus, it is possible that our results would have been different if data were available to control for additional objective measures of health. A final limitation is that we cannot eliminate the problem of loss-to-followup. Adults who remained in the study were likely a high functioning group–both physically and psychologically–compared to those who dropped out of the study.
Many prospective studies reveal that depressive symptoms are associated with mortality risk. The current study demonstrates that lower mortality risk is related to the presence of life satisfaction as well as the absence of depressive symptoms. Life satisfaction may be especially important for resilience in adulthood, when the cumulative effects of aging contribute to higher risk of mortality. However, the effect appears to reverse at the oldest ages, suggesting that a positive disposition at the oldest ages may not be sufficient to counteract existing health deterioration at this stage of life and may reflect psychological states before death (i.e., denial or acceptance). Future research should examine further the role that life satisfaction and similar constructs play in health at different points in the lifespan.
Acknowledgments
Support for this project came from the Demography and Epidemiology Unit of the Behavioral and Social Research Program of the National Institute of Aging (R01AG16790 and R01AG16661) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24HD047879). We thank German Rodriguez for helpful comments on the manuscript.
Footnotes
An earlier version of this paper was presented at the 2008 Population Association of America Annual Meeting in New Orleans, Louisiana.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/pag.
Contributor Information
Amy Love Collins, Princeton University.
Dana A. Glei, University of California, Berkeley
Noreen Goldman, Princeton University.
References
- Andresen EM, Carter WB, Malmgren JA, Patrick DL. Screen for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1999;10(20):77–84. [PubMed] [Google Scholar]
- Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality. Research on Aging. 1999;21(3):392–401. [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. Journals of Gerontology. 2003;58A(3):249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. International Journal of Geriatric Psychiatry. 1999;14(8):608–617. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Brandstadter J, Greve W. The aging self: Stabilizing and protective processes. Developmental Review. 1994;14:52–80. [Google Scholar]
- Brandstadter J, Renner G. Tenacious goal pursuit and flexible goal adjustment: Explication and age-related analysis of assimilative and accommodative strategies in coping. Psychology and Aging. 1990;5:58–67. doi: 10.1037//0882-7974.5.1.58. [DOI] [PubMed] [Google Scholar]
- Brown JE, Butow PN, Culjak G, Coates AS, Dunn SM. Psychosocial predictors of outcome: Time to relapse and survival in patients with early stage melanoma. British Journal of Cancer. 2000;83(11):1448–1453. doi: 10.1054/bjoc.2000.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Bernston GG. The affect system: Architecture and operating characteristics. Current Directions in Psychological Science. 1999;8(5):133. [Google Scholar]
- Cacioppo JT, Garnder WL, Bernston GG. The affect system has parallel and integrative processing components: Form follows function. Journal of Personality and Social Psychology. 1999;76(5):839. [Google Scholar]
- Chang MC, Hermalin AI. 1996 Survey of health and living status of the middle aged and elderly in Taiwan (A) Survey of those over 50–66 years of age (No 98–49) Ann Arbor, MI: PSC Publications, University of Michigan; 1998a. [Google Scholar]
- Chang MC, Hermalin AI. 1996 Survey of health and living status of the middle aged and elderly in Taiwan (B) Survey of those over 67 years of age (No 98–50) Ann Arbor, MI: PSC Publications, University of Michigan; 1998b. [Google Scholar]
- Cheng S. Age and subjective well-being revisited: A discrepancy perspective. Psychology & Aging. 2004;19(3):409–415. doi: 10.1037/0882-7974.19.3.409. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Abeloff MD, Melisaratos N. Psychological coping mechanisms and survival time in metastatic breast cancer. Journal of the American Medical Association. 1979;242(14):1504–1508. [PubMed] [Google Scholar]
- Devins GM, Mann J, Mandin H, Paul LC, Hons RB, Burgess ED, Taub K, Schorr S, Letourneau PK, Buckle S. Psychosocial predictors of survival in end-stage renal disease. Journal of Nervous Mental Disorders. 1990;178(2):127–133. doi: 10.1097/00005053-199002000-00008. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annual Review of Psychology. 2003;54:403–425. doi: 10.1146/annurev.psych.54.101601.145056. [DOI] [PubMed] [Google Scholar]
- Diener E, Scollon CN, Lucas RE. The evolving concept of subjective well-being: The multi-faceted nature of SWB. In: Costa PT, Siegler IC, editors. Advances in Cell Aging and Gerontology. Vol. 15. New York: Elsevier Science; 2003. pp. 187–219. [Google Scholar]
- Duberstein PR, Sörensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, et al. Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging. 2003;18(1):25–37. doi: 10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Finch CE, Pike MC. Maximum life span predictions from the Gompert mortality model. Journals of Gerontology: Biological Sciences and Medical Sciences. 1996;51(3):183–194. doi: 10.1093/gerona/51a.3.b183. [DOI] [PubMed] [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social Science & Medicine. 1997;45(8):1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Goldman N, Glei D, Cheng M. The role of clinical risk factors in understanding self-rated health. Annals of Epidemiology. 2004;14:49–57. doi: 10.1016/s1047-2797(03)00077-2. [DOI] [PubMed] [Google Scholar]
- Haga H, Shibata H, Suyama Y, Suzuki K, Iwasaki K, Suzuki T, Yasumura S. Self-rated health as a predictor of active life in the community elderly. Japanese Journal of Epidemiology. 1995;5:11–15. [Google Scholar]
- Hamer DH. The heritability of happiness. Nature Genetics. 1996;14(2):125–126. doi: 10.1038/ng1096-125. [DOI] [PubMed] [Google Scholar]
- Hermalin AI, Liang J, Chang MC. 1989 Survey of health and living status of the elderly in Taiwan: Questionnaire and survey design Comparative study of the elderly in Asia (No 89-1) Ann Arbor, MI: PSC Publications, University of Michigan; 1989. [Google Scholar]
- Idler E, Benyamini Y. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler EL, Kasl S. Self-ratings of health: do they also predict change in functional ability? Journals of Gerontology: Psychological Sciences and Social Sciences. 1995;50(6):S344–53. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Strawbridge WJ, Camacho T, Cohen RD. Factors associated with change in physical functioning in the elderly: A six-year prospective study. Journal o f Aging and Health. 1993;5:40–53. doi: 10.1093/geront/33.5.603. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of th CES-D (Center for Epidemiologic Studies Depression) depression symptoms index. Journal of Aging & Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Honkanen R, Koskenvuo M, Viinamaki H, Kaprio J. Life dissatisfaction as a predictor of fatal injury in a 20-year follow-up. Acta Psychiatrica Scandinavica. 2002;105(6):444–450. doi: 10.1034/j.1600-0447.2002.01287.x. [DOI] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Honkanen R, Viinamaki H, Heikkila K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. American Journal of Epidemiology. 2000;152(10):983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- Krause N, Liang J. Cross-cultural variations in depressive symptoms in later life. International Psychogeriatrics. 1992;4(2):185–202. [PubMed] [Google Scholar]
- Lezak MD. Neuropsychological assessment. 2. New York: Oxford University Press; 1983. [Google Scholar]
- Lyyra T, Törmäkangas TM, Read SR, Taina Berg S. Satisfaction with present life predicts survival in octogenarians. The Journals of Gerontology: Psychological Sciences and Social Sciences. 2006;61(6):319–326. doi: 10.1093/geronb/61.6.p319. [DOI] [PubMed] [Google Scholar]
- Maier H, Smith J. Psychological predictors of mortality in old age. The Journals of Gerontology. Psychological Sciences and Social Sciences. 1999;54(1):44–54. doi: 10.1093/geronb/54b.1.p44. [DOI] [PubMed] [Google Scholar]
- Markus HR, Kitayama S. The cultural psychology of personality. Journal of Cross Cultural Psychology. 1998;29(1):63–87. [Google Scholar]
- Mete C. Predictors of elderly mortality: health status, socioeconomic status, and social determinants of health. Health Economics. 2005;14:135–148. doi: 10.1002/hec.892. [DOI] [PubMed] [Google Scholar]
- Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. American Journal of Public Health. 1982;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagi SZ. Disability and Rehabilitation: Legal, Clinical, and Self Concepts and Measurement. Columbus: The Ohio State University Press; 1969. [Google Scholar]
- Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Memorial Fund Quarterly. 1976;54(4):439–68. [PubMed] [Google Scholar]
- Neugarten BL, Havighurst RJ, Tobin SS. The measurement of life satisfaction. Journal of Gerontology. 1961;16:134–143. doi: 10.1093/geronj/16.2.134. [DOI] [PubMed] [Google Scholar]
- Nezlek JB, Richardson DS, Green LR, Schatten-Jones EC. Psychological well being and day-to-day social interaction among older adults. Personal Relationships. 2002;9:57–71. [Google Scholar]
- Ofstedal MB, Zimmer ZS, Lin HS. A comparison of correlates of cognitive functioning in older persons in Taiwan and the United States. The Journals of Gerontology Series B: Psychological and Social Sciences. 1999;54(5):S291–301. doi: 10.1093/geronb/54b.5.s291. [DOI] [PubMed] [Google Scholar]
- Oishi S, Diener EF, Lucas RE, Suh EM. Cross-cultural variations in predictors of life satisfaction: Perspectives from needs and values. Personality & Social Psychology Bulletin. 1999;25(8):980–990. [Google Scholar]
- Okun MA, Stock WA. The construct validity of subjective well-being measures: An assessment via quantitative research syntheses. Journal of Community Psychology. 1987;15(4):481–492. [Google Scholar]
- Olshansky SJ, Carnes BA. Ever since Gompertz. Demography. 1997;34(1):1–15. [PubMed] [Google Scholar]
- Ostir GV, Ottenbacher KJ, Markides KS. Onset of frailty in older adults and the protective role of positive affect. Psychology and Aging. 2004;19(3):402–408. doi: 10.1037/0882-7974.19.3.402. [DOI] [PubMed] [Google Scholar]
- Panksepp J, Miller A. Handbook of Emotion, Adult Development and Aging. New York: Academic Press; 1996. Emotions and the aging brain: Regrets and remedies; pp. 3–26. [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-regulation processes and health: The importance of optimism and goal adjustment. Journal of Personality. 2006;74(6):1721–1747. doi: 10.1111/j.1467-6494.2006.00426.x. [DOI] [PubMed] [Google Scholar]
- Rothbaum R, Weisz JR, Snyder SS. Changing the world and changing the self: A two-process model of perceived control. Journal of Personality and Social Psychology. 1982;42(1):5–37. [Google Scholar]
- Ryff CD, Dienberg Love G, Urry HL, Muller D, Rosenkranz MA, Friedman EM, et al. Psychological well-being and ill-being: Do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics. 2006;75(2):85–95. doi: 10.1159/000090892. [DOI] [PubMed] [Google Scholar]
- Schimmack U, Oishi S. The influence of chronically and temporarily accessible information on life satisfaction judgments. Journal of Personality & Social Psychology. 2005;89(3):395–406. doi: 10.1037/0022-3514.89.3.395. [DOI] [PubMed] [Google Scholar]
- Schulz R, Bookwala J, Knapp JE, Scheier M, Williamson GM. Pessimism, age, and cancer mortality. Psychology & Aging. 1996;11(2):304–309. doi: 10.1037//0882-7974.11.2.304. [DOI] [PubMed] [Google Scholar]
- Schulz R, Drayer RA, Rollman B. Depression as a risk factor for non-suicide mortality in the elderly. Biological Psychiatry. 2002;52(3):205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 10. College Station, TX: 2007. [Google Scholar]
- Stock WA, Okun MA, Benin M. Structure of subjective well-being among the elderly. Psychology & Aging. 1986;1(2):91–102. doi: 10.1037//0882-7974.1.2.91. [DOI] [PubMed] [Google Scholar]
- Wechsler D. WAIS-R manual: Wechsler adult intelligence scale-revised. Cleveland, OH: Psychological Corporation/Harcourt Brace Jovanovich; 1981. [Google Scholar]
- Zimmer Z, Martin LG, Hui-Sheng L. Determinants of old-age mortality in Taiwan. Social Science & Medicine. 2005;60(3):457–470. doi: 10.1016/j.socscimed.2004.06.006. [DOI] [PubMed] [Google Scholar]


