Abstract
Background
Paraneoplastic neurological disorders associated with anti-Ri-antibodies, which are typically present with opsoclonus-myoclonus-ataxia. Most cases with anti-Ri-antibodyassociated paraneoplastic syndrome due to breast cancer occur in women - its occurrence in men is extremely rare.
Case Report
We present herein the case of a male patient with breast cancer who had atypical anti-Ri-antibody-associated paraneoplastic syndrome presenting as complete horizontal ophthalmoplegia, left trigeminal sensory symptoms, and truncal ataxia. Following the diagnosis of paraneoplastic syndrome, chemotherapy and immunomodulating treatment including intravenous immunoglobulin and oral prednisolone were administered. Although the patient was negative for serum anti-Ri-antibodies 14 weeks later, his symptoms persisted.
Conclusions
To our knowledge, this is the first case report of ophthalmoplegia without opsoclonus-myoclonus in a male anti-Ri-antibody-positive patient with breast cancer.
Keywords: breast cancer, anti-Ri-antibody, paraneoplastic syndrome
Introduction
Paraneoplastic neurological disorders associated with anti-Ri-antibodies (also known as anti-neuronal nuclear antibodies type II) mainly present with opsoclonus-myoclonus-ataxia.1 Ophthalmoplegia without opsoclonus is very rare.2,3 Although anti-Ri-antibodies have been reported in patients with gynecological tumors and small-cell lung cancer,1,4 they are mostly identified in patients with breast cancer. Most cases due to breast cancer occur in women. Its occurrence in men is extremely rare; there is thus far only one reported case, in which paraneoplastic opsoclonus-myoclonus was found in a man with breast cancer and anti-Ri-antibodies.5 We present herein the case of a male patient with breast cancer who had atypical anti-Ri-antibody paraneoplastic syndrome presenting as complete horizontal ophthalmoplegia, left trigeminal sensory symptoms, and truncal ataxia.
Case Report
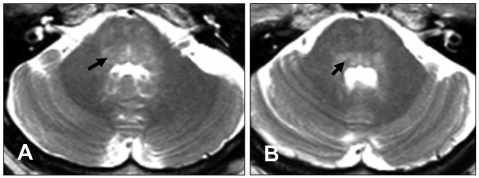
A 52-year-old man was referred to a hospital with subacute onset of binocular diplopia, left facial numbness, and gait disturbance. He was diagnosed with breast cancer 1 month after the onset of symptoms and then underwent a right modified radical mastectomy to remove an invasive ductal carcinoma. Neurologic examination revealed left trigeminal hypesthesia and complete horizontal gaze palsy without opsoclonus- myoclonus. His motor strength and deep tendon reflexes were normal. Sensation was intact to all modalities. The patient exhibited a wide-based gait and could not perform tandem gait. His cerebrospinal fluid showed normal cell counts and protein values, and negative cytology and viral markers. Immunofluorescence analysis revealed that the patient's serum contained anti-Ri-antibodies (serial dilutions revealed a specific antibody titer of 1 : 60), and was negative for anti-Hu, anti-Yo, and neuromyelitis optica antibodies. A brain magnetic resonance imaging (MRI) scan revealed a high-signal-intensity lesion in the pontine tegmentum that was not enhanced with gadolinium (Fig. 1). A brain magnetic resonance angiogram showed no significant steno-occlusive lesion. Initial infusion of intravenous immunoglobulins (400 mg/kg/day for 3 days) was administered 4 months after symptom onset, followed by a maintenance dose (400 mg/ kg/day) every 2 months for 1 year. Concurrent chemotherapy of doxorubicin, cyclophosphamide, and dexamethasone was administered. After four cycles of chemotherapy, the patient's serum tested negative for anti-Ri-antibodies, and a follow-up brain MRI showed neither abnormal signal change nor atrophy in the brainstem. Further extensive searching, including whole-body positron-emission tomography, produced no evidence of tumor recurrence. However, this patient's neurological deficit has persisted during the subsequent 3-year follow-up, in spite of intensive chemotherapy and immunomodulating treatment.
Fig. 1.
T2-weighted magnetic resonance images showing bilateral symmetric hyperintense lesions in the pontine tegmentum. A: Parapontine reticular formation (arrow) in the lower pons. B: Medial longitudinal fasciculus (arrow) in the mid pons.
Discussion
Whilst opsoclonus-myoclonus ataxia syndrome is often used to describe anti-Ri-antibody-associated paraneoplastic disorder, it has a wide spectrum of neurological manifestations.6,7 The present case emphasizes the clinical heterogeneity of this disorder. However, even in the absence of opsoclonus, oculomotor dysfunction is usually prominent,8,9 and the brainstem is a major site of autoimmunity. The main clinical features in our patient were brainstem syndrome involving the structures of the dorsal pons: the parapontine reticular formation, abducens nucleus, medial longitudinal fasciculus, and trigeminal nucleus of the spinal tract.
In anti-Ri-antibody-positive patients, brain MRI findings are usually normal, with only a few exceptions. There are reports of an abnormal signal in the dorsal midbrain,10 and atrophy of the cerebellar vermis1 on brain MRI, associated with anti-Ri-antibodies. In our patient, MRI disclosed symmetric hyperintense lesions in the dorsal pons that were reversible with treatment. However, his symptoms persisted even after the lesion had disappeared. Tumor removal and chemotherapy did not improve the paraneoplastic abnormalities and the effect of immunoglobulin was also disappointing. Thus, it appears that irreversible, rather than functional damage to the neurons causes the symptoms of anti-Ri-antibody-associated paraneoplastic syndrome.
The underlying tumor in our case was an invasive ductal cell carcinoma of the breast. The incidence of breast caner in man is low in the literature, representing approximately 1% of all breast cancer diagnoses.11 To our knowledge, this is the first case report of ophthalmoplegia without opsoclonus-myoclonus in a male, anti-Ri-antibody-positive patient with breast cancer. The findings of this case support the differentiation of anti-Ri-antibody-associated paraneoplastic syndrome even in the absence of opsoclonus, and that it can also occur in male patients with breast cancer.
References
- 1.Luque FA, Furneaux HM, Ferziger R, Rosenblum MK, Wray SH, Schold SC, Jr, et al. Anti-Ri: an antibody associated with paraneoplastic opsoclonus and breast cancer. Ann Neurol. 1991;29:241–251. doi: 10.1002/ana.410290303. [DOI] [PubMed] [Google Scholar]
- 2.Escudero D, Barnadas A, Codina M, Fueyo J, Graus F. Anti-Ri-associated paraneoplastic neurologic disorder without opsoclonus in a patient with breast cancer. Neurology. 1993;43:1605–1606. doi: 10.1212/wnl.43.8.1605. [DOI] [PubMed] [Google Scholar]
- 3.Ohmer R, Golnik KC, Richards AI, Kosmorsky GS. Ophthalmoplegia associated with the anti-Ri antibody. J Neuroophthalmol. 1999;19:246–248. [PubMed] [Google Scholar]
- 4.Voltz R. Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis, and therapy. Lancet Neurol. 2002;1:294–305. doi: 10.1016/s1474-4422(02)00135-7. [DOI] [PubMed] [Google Scholar]
- 5.Wirtz PW, Sillevis Smitt PA, Hoff JI, de Leeuw B, Lammers GJ, van Duinen SG, et al. Anti-Ri antibody positive opsoclonus-myoclonus in a male patient with breast carcinoma. J Neurol. 2002;249:1710–1712. doi: 10.1007/s00415-002-0913-z. [DOI] [PubMed] [Google Scholar]
- 6.Pittock SJ, Lucchinetti CF, Lennon VA. Anti-neuronal nuclear autoantibody type 2: paraneoplastic accompaniments. Ann Neurol. 2003;53:580–587. doi: 10.1002/ana.10518. [DOI] [PubMed] [Google Scholar]
- 7.Kastrup O, Meyring S, Diener HC. Atypical paraneoplastic brainstem encephalitis associated with anti-ri-antibodies due to thymic carcinoma with possible clinical response to immunoglobulins. Eur Neurol. 2001;45:285–287. doi: 10.1159/000052145. [DOI] [PubMed] [Google Scholar]
- 8.Sutton IJ, Barnett MH, Watson JD, Ell JJ, Dalmau J. Paraneoplastic brainstem encephalitis and anti-Ri antibodies. J Neurol. 2002;249:1597–1598. doi: 10.1007/s00415-002-0863-5. [DOI] [PubMed] [Google Scholar]
- 9.Ko MW, Dalmau J, Galetta SL. Neuro-ophthalmologic manifestations of paraneoplastic syndromes. J Neuroophthalmol. 2008;28:58–68. doi: 10.1097/WNO.0b013e3181677fcc. [DOI] [PubMed] [Google Scholar]
- 10.Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 9-1988. A 57-year-old woman with worsening opsoclonus. N Engl J Med. 1988;318:563–570. doi: 10.1056/NEJM198803033180907. [DOI] [PubMed] [Google Scholar]
- 11.Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men: a population-based study. Cancer. 2004;101:51–57. doi: 10.1002/cncr.20312. [DOI] [PubMed] [Google Scholar]