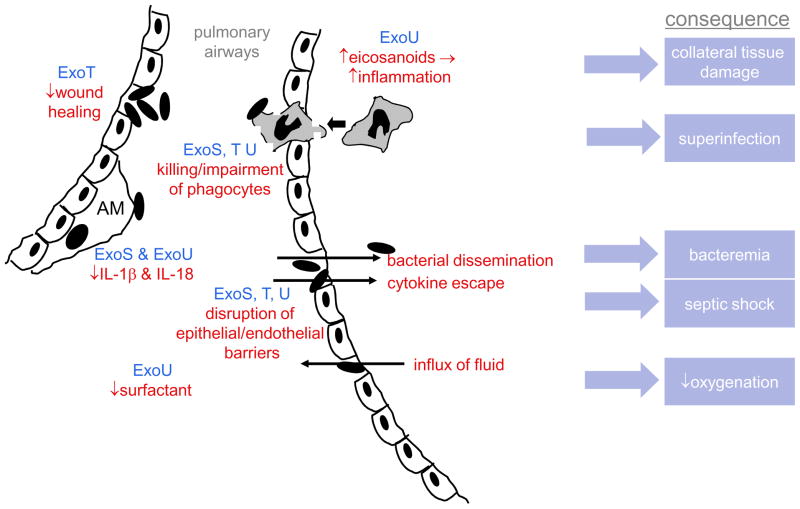
Figure 4. Role of type III effector proteins in the pathogenesis of acute pneumonia.
In early infection, P. aeruginosa exploits breaches in the epithelial mucosa, which is facilitated by ExoT-mediated inhibition of wound healing. ExoU and ExoS block IL-1β and IL-18 production by alveolar macrophages, blunting or biasing the early inflammatory response. When subsequent development of an inflammatory response does occur, it is excessively amplified by ExoU-induced eicosanoid release and causes collateral damage to host tissues. However the recruited phagocytes are unable to eradicate P. aeruginosa because they are killed or impaired by ExoS, ExoT, and ExoU; the resulting paucity of functional phagocytes makes the lungs prone to superinfection by other bacteria. ExoS, ExoT, and ExoU also disrupt epithelial/endothelial barriers, allowing bacteria and proinflammatory cytokines to escape to the bloodstream, leading to bacteremia and septic shock, respectively. These same breaches allow protein-rich fluid to flow into the air spaces of the lung, which together with ExoU-mediated decreases in pulmonary surfactant, causes decreased lung compliance and oxygenation. AM=alveolar macrophage