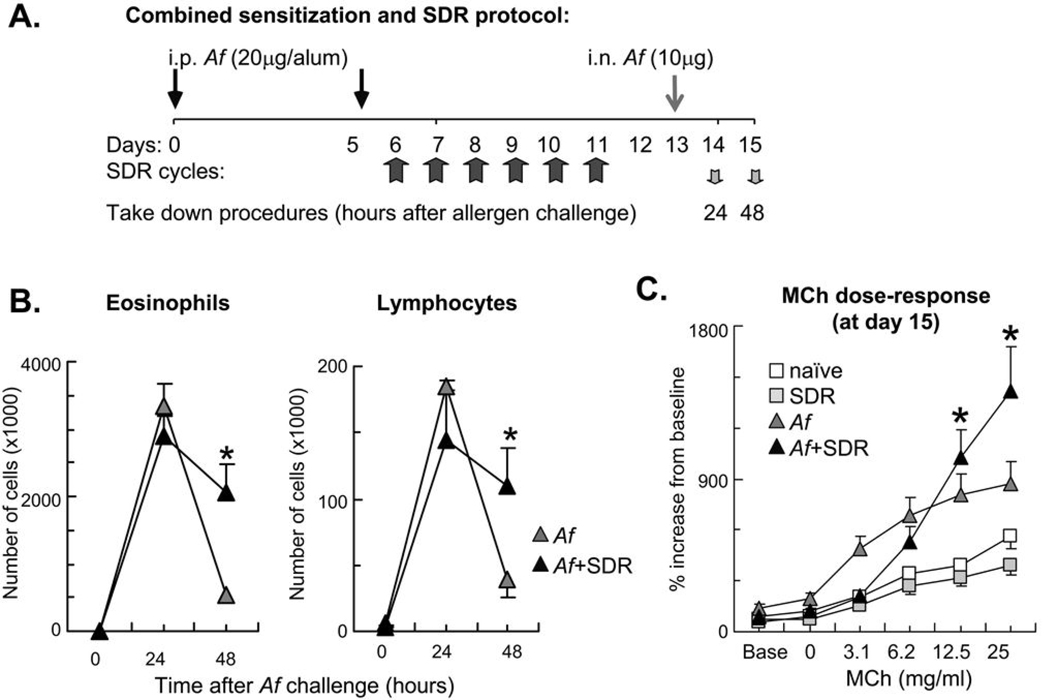
Figure 1.
Combination of allergic airway sensitization and SDR caused delayed resolution of the inflammatory airway response and enhancement of allergic airway hyperresponsiveness at high methacholine concentrations. (A): In a combined protocol for allergic sensitization and SDR, mice received intraperitoneal (i.p.) Af in alum on days 0 and 5 followed by repeated SDR for 2 hours on days 6 through 11. Mice received intranasal (i.n.) allergen challenge on day 13 and were sacrificed either 24 or 48 hours later. Control naïve and SDR mice were sacrificed on day 15. (B): Combination of allergic airway sensitization and SDR increased number of airway eosinophils and lymphocytes 48h after Af challenge. BAL differential cell count was evaluated in Giemsa preparations. Naïve and SDR mice did not receive allergen challenge. There was no difference between naïve and SDR mice. (C): Exposure to allergen and stress enhanced airway hyperresponsiveness at high methacholine concentrations. Mice were studied 48 h after a single Af challenge. Mice received increasing doses of inhaled methacholine (MCh). Lung function was assessed using non-invasive plethysmography and the enhanced pause (Penh). There was no difference between naïve and SDR mice. Data are expressed as % changes from baseline. Baseline Penh measurements were as follows: naïve: 0.385±0.050; SDR:0.471±0.028; Af:0.924±0.367; Af+SDR:0.614±0.082 (B–C): Mean±SEM of n=5–8 each; *p<0.05 (Af vs. Af+SDR).