Abstract
Objective
We introduced a new information technology-based diabetes management system, called the Internet-based glucose monitoring system (IBGMS), and demonstrated its short-term and long-term favorable effects. However, there has been no report on clinical effects of such a new diabetes management system on the development of diabetic complications so far. This study was used to simulate the complication reducing effect of the IBGMS, given in addition to existing treatments in patients with type 2 diabetes.
Research Design and Methods
The CORE Diabetes Model, a peer-reviewed, published, validated computer simulation model, was used to project long-term clinical outcomes in type 2 diabetes patients receiving the IBGMS in addition to their existing treatment. The model combined standard Markov submodels to simulate the incidence and progression of diabetes-related complications.
Results
The addition of IBGMS was associated with improvements in reducing diabetic complications, mainly microangiopathic complications, including diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and diabetic foot ulcer. The IBGMS also delayed the development of all diabetic complications for more than 1 year.
Conclusions
This study demonstrated that the simulated IBGMS, compared to existing treatment, was associated with a reduction of diabetic complications. As a result, it provides valuable evidence for practical application to the public in the world.
Keywords: diabetic complications, health economics, Internet, simulation
Introduction
Diabetes remains one of the most serious challenges facing modern medicine and places a huge clinical and financial burden on health care services. Between 2000 and 2030, the worldwide prevalence of diabetes is projected to rise from 171 to 366 million, with over 90% of these cases being type 2 diabetes.1 Type 2 diabetes has become a major health concern in all of Asia, as well as in Korea, over the last decade2 as lifestyles become increasingly westernized and industrialization continues its rapid growth, representing a substantial health and economic burden to a country's health care system, both now and in the future.3 Furthermore, people in Asia tend to develop diabetes with a lesser degree of obesity at younger ages, suffer longer with complications of diabetes, and die sooner than people in other regions.2
Controlled clinical trials have shown that prolonged maintenance of the appropriate hemoglobin A1c (HbA1c) level reduces the risk of developing diabetes complications in individuals with type 1 and type 2 diabetes.5–7 Despite attempts to achieve improved diabetes management and despite the availability of multiple therapeutic options, average glycemic control in patients with diabetes has not improved in the United States and Europe since the early 1980s, especially not in type 2 diabetes.8–11 The percentage of United Kingdom patients achieving targets of HbA1c ≤7.0% was only 14.4% in 1998.12 In addition, data from the National Health and Nutrition Examination Surveys in the United States showed that overall glycemic control did not improve between the assessment periods of 1988–1994 and 1999–2000.13,14 Similar findings have been reported in other countries.10,11 Clearly, an improved approach and better implementation are required to improve glycemic control in patients with diabetes and to limit the development of diabetes-related complications.
In 2004, we introduced a new information technology-based glucose control system, called the Internet-based glucose monitoring system (IBGMS), and demonstrated its short-term effect.15 The IBGMS, which is characterized by a bidirectional system through which both the patient and the physician can communicate interactively by close monitoring and by a data-based management system that includes charts of IBGMS, can provide seasonal advice and feedback, continuous motivation for glucose control, frequent encouragement, problem assessment, and individualized education about diet and exercise, as well as drug modification. We also reported on its long-term effect on HbA1c reduction and glucose stability,16 which was a prospective, randomized controlled trial involving 80 patients with type 2 diabetes over 30 months duration. Findings showed that the mean HbA1c and HbA1c fluctuation index were significantly lower in the intervention than in the control, indicating that the addition of the IBGMS has the potential to provide superior long-term control of blood glucose and achieving glucose stability compared to usual care. In addition, other similar systems for diabetes management using the Internet or telecommunication were introduced and their efficacy was demonstrated in the United States and the United Kingdom.17,18 Further information is needed, however, concerning the complication reduction rate of such a system before its application could be considered in the general population. In this study, we simulated the prevalence of diabetic complications over a 35-year period and compared the results of the use of IBGMS with those of a usual care, conventional outpatient management system.
Research Design and Methods
Model Description and Assumptions
The structure, data inputs, and validation of the CORE Diabetes Model have been published previously in detail.5,13,19,20 The model is based on a series of submodels that simulate the micro- and macrovascular and acute metabolic complications of diabetes and one that simulates nonspecific mortality. Each submodel has a Markov-based structure using probabilities derived from published sources. HbA1c-dependent adjustments for the risks of developing complications in type 2 diabetes were derived from about 130 other landmark studies. The CORE Diabetes Model has been validated previously against 66 published analyses, including external (third order) validation of simulations of type 2 diabetes.13,19,20
Time Horizon
The simulation was run over a 35-year period to capture the development of all relevant complications in patient lifetimes.
Simulations
Second-order Monte Carlo simulation was utilized in all simulations to account for both patient-level uncertainty and uncertainty at the parameter level. This was done by running 1000 samples, each of 1000 patients, through the model.
Results
Cohort Characteristics
For base case analysis, a theoretical cohort was defined with similar baseline demographics, risk factors, and preexisting complications to the population described by Cho and colleagues16 (mean age 53 years, duration of diabetes 6.8 years, body mass index 23.3 kg/m2, baseline HbA1c 7.6%), as outlined in Table 1. Ethnicity in the model was set to 100% Asian. In subgroup analyses, the cohort characteristics at baseline were slightly different in terms of demographics and risk factors, although baseline cardiovascular complications were assumed to be the same as in the base case. Cohort characteristics for the IBGMS versus usual care subgroup analysis are presented in Table 1.
Table 1.
Summary of Baseline Demographics and Patient Characteristics for Base Case Analysis
| Characteristica | Value |
|---|---|
| Patient demographics | |
| Age at baseline | 61 years |
| Duration of diabetes | 7 years |
| Proportion male | 58.0% |
| Baseline risk factors | |
| Mean HbA1c | 8.50% |
| Mean SBP | 138 mm Hg |
| Mean total cholesterol | 226.5 mg/dl |
| Mean HDL | 43.7 mg/dl |
| Mean LDL | 147.76 mg/dl |
| Mean triglycerides | 213.3 mg/dl |
| Mean BMI | 28.64 kg/m2 |
| Baseline cardiovascular disease complications | |
| Proportion with previous myocardial infarction | 6.65% |
| Proportion with previous angina | 6.20% |
| Proportion with previous peripheral vascular disease | 5.46% |
| Proportion with previous congestive heart failure | 4.86% |
SBP, systolic blood pressure; HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol; BMI, body mass index; all values derived from the MERIA meta-analysis.11
Intervention Effects
For base case analysis, the effects of the IBGMS were based on data reported in the Cho et al.16 analysis. In the simulation, treatment effects were implemented by applying the increases or reductions shown in Table 2 to the baseline values for each parameter. For example, with HbA1c in the IBGMS treatment, a reduction of 1.02% points was applied to the baseline mean of 7.50%. Long-term changes in HbA1c were thereafter assumed to follow the pattern seen in United Kingdom Prospective Diabetes Study patients, with an annual reincrease (following the initial treatment arm-dependent decrease from baseline seen in the first year) of HbA1c of approximately 0.15% points/year, independent of type of treatment.21
Table 2.
Summary of the IBGMS versus Usual Care Effects from the Cho et al.16 Analysis Used in the Model (Base Case)
| Effecta | IBGMS | Usual care |
|---|---|---|
| Change from baseline in HbA1c (% points) | −1.02 | −0.05 |
| Change from baseline in total cholesterol (mg/dl) | −5.5 | −12.4 |
| Change from baseline in LDL (mg/dl) | −4.8 | −5.3 |
| Change from baseline in HDL (mg/dl) | 3.1 | 0.6 |
| Change from baseline in triglycerides (mg/dl) | −7.3 | −35.7 |
| Change from baseline in BMI (kg/m2) | 0.3 | 0.1 |
HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol; BMI, body mass index.
Cumulative Incidence of Diabetic Complications
The predicted cumulative incidence of diabetic complications in subjects with type 2 diabetes is shown in Figure 1: cumulative incidence of eye complications (A), diabetic nephropathy (B), foot ulcer and neuropathy (C), and macrovascular complications (D). Microvascular complications of retinopathy and nephropathy were reduced in the intervention group. The prevalence of foot ulcer and neuropathy was also decreased with intervention. Of macrovascular complications, the prevalence of myocardial infarction and peripheral vascular disease was decreased with intervention; however, that of stroke and congestive heart failure was not decreased.
Figure 1.
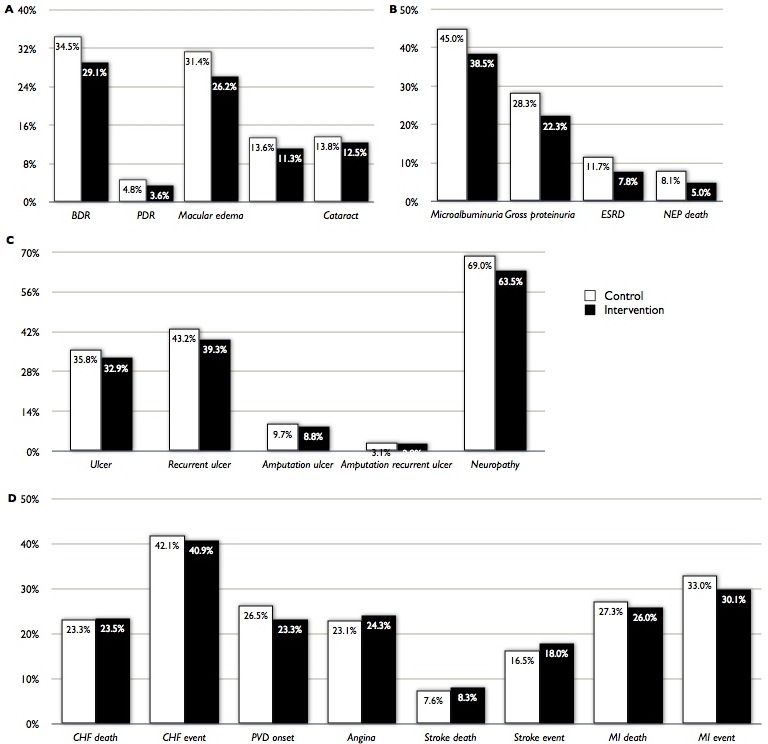
Predicted cumulative incidence of diabetic complications in subjects with type 2 diabetes. A shows the cumulative incidence of eye complications, B, diabetic nephropathy, C, ulcer and neuropathy and D, macrovascular complications. White bar indicates control group and black bar intervention group. BDR, background diabetic retinopathy; PDR, proliferative diabetic retinopathy; ESRD, End stage renal disease; CHF, congestive heart failure; PVD, peripheral vascular disease; MI, myocardial infarction)
Figure 2 shows the time alive, free of complications. Development of most of the complications was delayed by more than 1 year with intervention. In the intervention group, neuropathy developed 2 years after the control group.
Figure 2.
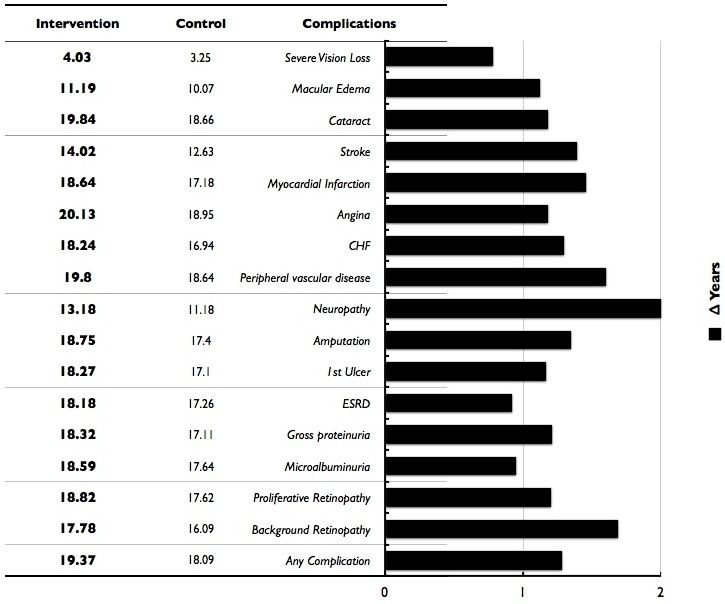
Time alive and free of complications in control and intervention groups. Bar represents the time difference between intervention and control group. CHF, congestive heart failure; ESRD, end stage renal failure; CVD, cardiovascular disease
Discussion
We report on the first study to evaluate the long-term simulation results of the complication reducing rate of the information technology-based intensive diabetes management system in patients with type 2 diabetes. This simulation study demonstrated that, over patient lifetimes, the addition of IBGMS to existing treatment was associated with a reduction in diabetic complications in patients with type 2 diabetes. IBGMS therefore appeared superior to usual care in reducing diabetic complications. Microangiopathies, including diabetic retinopathy, diabetic nephropathy, and neuropathy, were all reduced in the intervention group compared to conventional usual care. The intervention system was also expected to reduce the incidence of diabetic foot ulcer.
However, in comparison of macroangiopathies, such as congestive heart failure, angina, and stroke, there was little difference between the two groups, although the incidence of myocardial infarction and mortality as a consequence of myocardial infarction was lower in the intervention group.
We attribute the result to the fact that many other factors in addition to glucose control, such as blood pressure, lipid level, and smoking, can also aggravate macrovascular complications. Therefore, to reduce the incidence of macrovascular complications, patients should try to keep blood pressure and lipid levels within target ranges and to stop smoking, as well as controlling blood glucose.
The Internet-based glucose monitoring system was expected to delay the development of all diabetic complications, diabetic retinopathy, diabetic neuropathy, diabetic foot ulcer, diabetic neuropathy, myocardial infarction, congestive heart failure, peripheral vascular disease, and stroke for at least more than 1 year in the 35-year simulation test. This means that diabetic patients can live for more than 1 year without any complications by the intervention system. As a result, with the system, the quality of life can be improved much more.
However, it should be noted that this simulation was based on data from subjects being managed in a well-established diabetes center where blood pressure and serum lipids were relatively well controlled. As most diabetic patients, however, are not treated in such a well-established center, it is conceivable that the use of IBGMS might be associated with even greater benefits when applied to the general population. Furthermore, IBGMS could improve clinical practice in primary care settings by the clinical decision supporting system, which will be developed by practical recommendations. Another important barrier for the implementation of IBGMS is the burden of the health providers for operating the IBGMS. For minimizing this, we will be able to develop and merge an automatic patient monitoring software into the IBGMS. In this simulation test, we demonstrated the beneficial effect of the Internet-based glucose monitoring system on reducing diabetic complications. This system is expected to be a new additional tool for more effective glucose control, and its impact will be enormous when it is applied to the general population. For that purpose, we should show data for the economic impact of the system. We have to calculate not only the cost-saving effect resulting from the reduction of complications, but also the labor cost for maintaining the system for a long-term period. With results of the economic impact of the system, we will be able to try to apply the system to general populations all over the world.
Acknowledgements
We thank Sung-Hee Cho, product manager of Novo Nordisk Pharma Korea, for her sincere assistance and the company Novo Nordisk Pharma. We also thank William Jeffcoate for comments and critical reading of the manuscript.
Abbreviations
- HbA1c
hemoglobin A1c
- IBGMS
Internet-based glucose monitoring system
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 3.Chou P, Li CL, Tsai ST. Epidemiology of type 2 diabetes in Taiwan. Diabetes Res Clin Pract. 2001;54:S29–35. doi: 10.1016/s0168-8227(01)00306-0. [DOI] [PubMed] [Google Scholar]
- 4.Caro JJ, Ward AJ, O'Brien J. Lifetime costs of complications resulting from type 2 diabetes in the U.S. Diabetes Care. 2002;25:476–481. doi: 10.2337/diacare.25.3.476. [DOI] [PubMed] [Google Scholar]
- 5.Writing Team for the Diabetes Control Complications Trial/Epidemiology of Diabetes Interventions Complications Research Group. Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA. 2002;287:2563–2569. doi: 10.1001/jama.287.19.2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–713. [PMC free article] [PubMed] [Google Scholar]
- 7.Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with noninsulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995;28:103–117. doi: 10.1016/0168-8227(95)01064-k. [DOI] [PubMed] [Google Scholar]
- 8.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 9.Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27:17–20. doi: 10.2337/diacare.27.1.17. [DOI] [PubMed] [Google Scholar]
- 10.Ubink-Veltmaat LJ, Bilo HJ, Groenier KH, Houweling ST, Rischen RO, Meyboom-de Jong B. Prevalence, incidence and mortality of type 2 diabetes mellitus revisited: a prospective population-based study in The Netherlands (ZODIAC-1) Eur J Epidemiol. 2003;18:793–800. doi: 10.1023/a:1025369623365. [DOI] [PubMed] [Google Scholar]
- 11.Berger B, Stenstrom G, Sundkvist G. Incidence, prevalence, and mortality of diabetes in a large population. A report from the Skaraborg Diabetes Registry. Diabetes Care. 1999;22:773–778. doi: 10.2337/diacare.22.5.773. [DOI] [PubMed] [Google Scholar]
- 12.New JP, Hollis S, Campbell F, McDowell D, Burns E, Dornan TL, Young RJ. Measuring clinical performance and outcomes from diabetes information systems: an observational study. Diabetologia. 2000;43:836–843. doi: 10.1007/s001250051458. [DOI] [PubMed] [Google Scholar]
- 13.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 14.Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27:17–20. doi: 10.2337/diacare.27.1.17. [DOI] [PubMed] [Google Scholar]
- 15.Kwon HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM, Kim SR, Chang SA, Kim HS, Cha BY, Lee KW, Son HY, Lee JH, Lee WC, Yoon KH. Establishment of blood glucose monitoring system using the internet. Diabetes Care. 2004;27:478–483. doi: 10.2337/diacare.27.2.478. [DOI] [PubMed] [Google Scholar]
- 16.Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, Yoo SJ, Song KH, Son HS, Kim HS, Lee WC, Cha BY, Son HY, Yoon KH. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with an ubiquitous medical care system. Diabetes Care. 2006;29:2625–2631. doi: 10.2337/dc05-2371. [DOI] [PubMed] [Google Scholar]
- 17.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28:1624–1629. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farmer AJ, Gibson OJ, Dudley C, Bryden K, Hayton PM, Tarassenko L, Neil A. A randomized controlled trial of the effect of real-time telemedicine support on glycemic control in young adults with type 1 diabetes. Diabetes Care. 2005;28:2697–2702. doi: 10.2337/diacare.28.11.2697. [DOI] [PubMed] [Google Scholar]
- 19.Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM, Lammert M, Spinas GA. The CORE Diabetes Model: Projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5–26. doi: 10.1185/030079904X1980. [DOI] [PubMed] [Google Scholar]
- 20.Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM, Lammert M, Spinas GA. Validation of the CORE Diabetes Model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(Suppl 1):S27–40. doi: 10.1185/030079904X2006. [DOI] [PubMed] [Google Scholar]
- 21.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]


