Abstract
Nutritional and immunological status of patients with obstructive jaundice is usually severely altered, with high mortality rates. The n-3 polyunsaturate fatty acids (PUFA), particularly eicosapentaenoic acid (EPA, 20:5 n-3), posess potent immunomodulatory activities. Thus, our aim was to compare the plasma phospholipid fatty acid (FA) composition of these patients with healthy subjects, as well as before and after 7 days preoperative supplementation with high doses of EPA (0.9 g per day) and docosahexaenoic acid (DHA, 22:6 n-3, 0.6 g per day). We found impaired FA status in obstructive jaundice patients, especially EPA, DHA and PUFA, but significantly increased content of total n-3 FA, 22:5 n-3 FA and particularly EPA, which increased more than 3 fold, after 7 days supplementation. In addition, the n6/n3 ratio significantly decreased from 14.24 to 10.24, demonstrating severely improved plasma phospholipid profile in these patients after the intervention.
Keywords: obstructive jaundice, fatty acid, n-3 fatty acid supplementation, EPA, DHA
Introduction
Nutritional and immunological status of patients with obstructive jaundice is usually severely altered [1]. For selected patients surgery remains the only treatment option with often complicated postoperative course. Major surgery is followed by a period of immunosuppression that increases the risk of morbidity and mortality due to perioperative complications, including bleeding, wound problems, renal and liver malfunction and particularly sepsis [2, 3]. Improving immune function during this period may significantly reduce complications of infection [1]. The potential to modulate the activity of the immune system by interventions with specific nutrients (i.e. immunonutrition), has become associated most closely with attempts to improve the clinical course of critically ill and surgical patients [1]. The immune function could be improved by polyunsaturate fatty acids (PUFA), and among them, an n-3 FA from fish oil-eicosapentaenoic acid (EPA, 20:5 n-3) posesses the most potent immunomodulatory activities [4].
In patients with obstructive hepatitis, malnutrition impairs lipid digestion and uptake, partly due to bacterial degradation of bile salts and ensuing reduced micellular solubilisation. Also, bile production is decreased [5]. Since biliary phosphatidylcholine production seems to be an important source of intestinal essencial fatty acids (EFA) supply, an increased degradation and a reduced bile production could further impair the EFA status [5]. Thus, we proposed that patients with obstructive jaundice have a poor PUFA status, because bile acids contribute to efficient PUFA absorbtion from the gut and because long chain PUFA (LCP) are synthetized from their precursors, mainly in the liver. The dietary PUFA of the n-3 series are very important for maintance of overall health. They are rapidly incorporated into cell membranes and profoundly influence biological responses, from membrane fluidity, cell mobility, the formation of receptors, activation of intracellular signaling pathways directly or through the formation of eicosanoids, to gene expression and cell differentiation [6]. Eicosanoids formed from the n-3 FA are much less potent in causing biological responses, including stimulation of cytokine production and inflammatory reactions, than those formed from the n-6 series [6]. The immune and inflammatory cells contain many transcription factors including NF kappa B (NFκB), which regulates the synthesis of cytokines IL-1, IL-2, IL-6, TNF-α and interferon-β [7]. EPA reduces the production of pro-inflammatory IL-1 and IL-6, as well as TNF-α and -β in response to an inflammatory stimulus [8]. The n-3 PUFA also decrease production of arachidonic acid-derived eicosanoids. Due to a lack of Δ6 desaturase, content of arachidonic acid (AA) in inflammatory cells depends on the uptake of AA synthetized in the liver from plasma [9, 10], i.e. it depends on hepatic desaturases. The mechanism of desaturase activity in obstructive jaundice is unclear, it is not known whether bile salts affect desaturase activity [7]. AA can be converted via an enzymatic process into pro-inflamatory substances, especially prostaglandin E2 (PGE2), which is often increased in chronic inflammatory conditions [10]. Fish oil, rich in EPA and docasahexaenoic acid (DHA), inhibits production of PGE2, as well as lymphocyte proliferation and production of IFN-γ [11].
Regarding the influence of n-3 fatty acids in immunomodulating processes, we tried to improve the FA profile of preoperative patients with obstructive jaundice by seven days preoperative supplementation of high doses n-3 FA. The aim of this pilot study was to evaluate the plasma phospholipid fatty acid composition and possible changes before and after the supplementation.
Patients and Methods
Study design
Thirteen observed patients with obstructive jaundice (10 men, 3 women; mean age, 59 years; range, 54–68 years), who were scheduled for major abdominal surgery, were enrolled in this pilot study. Diagnosis of obstructive jaundice was based on clinical and biochemical data. Before treatment, total bilirubin levels were 319.2 ± 99.1 µmol/l and direct bilirubin 66.6 ± 59.2 µmol/l, AST values 104.3 ± 56.5, ALT values167.4 ± 118.5 and gama GT levels 724.6 ± 485.4 U/l. Patients did not take fish oil supplements or lipid lowering drugs or actively exercised before the study. Fifteen healthy subject, sex and age matched (12 men, 3 women; mean age, 60 years; range, 54–68 years), who have not consumed alcohol, were drawn from medical staff and blood donors as control subjects. They had all biochemical parameters in normal range (total bilirubin 10.8 ± 1.9 µmol/l and direct bilirubin 2.7 ± 1.1 µmol/l, AST 20.0 ± 8.2, ALT 19.2 ± 4.3 and GGT 21.9 ± 4.5 U/l).
Patients undergoing major gastroinestinal surgery, received n-3 soft gelatin capsules with 5 g of fish oil per day, which contained 0.9 g EPA + 0.6 g DHA, in addition to the usual hospital diet, composed mostly of vegetable soups without fats and a lot of water in order to maintain optimal hydratation. A venous blood sample was drawn before and after 7 days of fish oil supplementation. Out of 13 patients, 6 abandoned the supplementation due to an urgent surgery, whereas 7 patients completed the study. All study participants provided written informed consent which was approved by the Ethical Review Boards of the participating institutions in accordance with the principles of the Declaration of Helsinki.
Lipid determination
Serum lipids were extracted by method of Sperry and Brand [12] using chloroform-methanol mixture (2:1 v/v) with 50 mg/100 ml 2,6-di-tert-butyl-4-methylphenol (BHT) added as antioxidant. The phospholipid fraction was isolated by one-dimensional thin-layer chromatography (TLC) in neutral solvent system hexane : diethyl ether : acetic acid (87:12:1, v/v/v) using Silica Gel GF plates (Merck, Darmstadt, Germany).
Fatty acid determination
Methyl esters of phospholipid (PL) fatty acids were prepared by method that have been reported previously [13]. FA methyl esters of isolated plasma phospholipid fractions were separated by gas chromatography using a Varian GC (model 3400) equipped with Rtx 2330 (60 m × 0,53 mm i.d., film thickness 0,2 µm (J and W Scientific Inc Bellefonte, Folsona, CA) fused silica capilary column. The flame ionisation detector was set at 250°C, the injection port at 220°C and the oven temperature programmed from 130°C to 190°C at the heating rate of 3°C/min. The individual fatty acid methyl esters were identified comparing sample peak retention times with authentic standards (Sigma Aldrich Chemie Taufkirchen, Taufkirchen, Germany) and/or the polyunsaturated fatty acids (PUFA)-2 standard mixtures (Sigma Aldrich Chemie Taufkirchen).
Statistical analysis
All results are expressed as means ± SD. Normality was tested using the Kolmogorov-Smirnov test. Since all parameters were normally distributed, the differences between groups were determined by using one way ANOVA followed by Tuckey post-hoc test, accepting an alpha levels of significance p≤0.05.
Results
At the begining of this study, we compared the percentages of FA in plasma phospholipids of patients with obstructive jaundice and in healthy individuals. As we expected, preoperative patients had significantly less proportion of EPA (20:5 n-3), DHA (22:6 n-3) and total n-3, n-6 and PUFA than control subjects (Table 1). The percentages of linoleic (LA, 18:2 n-6) and arachidonic acid (AA, 20:4 n-6) were significantly lower as well. On the other hand, the percentages of short-chain FA, particularly palmitic acid (16:0) and total SFA were higher in patients than in control group. The n6/n3 ratio was also significantly higher in obstructive jaundice patients.
Table 1.
Plasma phospholipid FA profile in healthy subjects and in patients with obstructive jaundice before and after the n-3 FA supplementation.
| Fatty acid | Control group | Patients, baseline | Patients, after supplementation |
|---|---|---|---|
| 16:00 | 23.77 ± 1.13 | 31.6 ± 2.84*** | 32.46 ± 2.40 |
| 16:1 n-7 | 0.24 ± 0.09 | 1.08 ± 0.32*** | 1.23 ± 0.37 |
| 18:00 | 14.88 ± 1.18 | 13.66 ± 2.09 | 13.58 ± 2.74 |
| 18:1 n-9 | 11.85 ± 1.69 | 14.31 ± 2.19** | 14.77 ± 1.14 |
| 18:2 n-6 | 28.39 ± 2.81 | 24.84 ± 3.43* | 22.87 ± 2.03 |
| 20:3 n-6 | 2.71 ± 0.84 | 2.59 ± 1.01 | 2.39 ± 0.65 |
| 20:4 n-6 | 12.41 ± 2.20 | 8.81 ± 1.50*** | 8.75 ± 1.43 |
| 20:5 n-3 | 0.41 ± 0.24 | 0.18 ± 0.07** | 0.55 ± 0.24### |
| 22:4 n-6 | 0.86 ± 0.38 | 0.35 ± 0.13*** | 0.36 ± 0.12 |
| 22:5 n-3 | 0.71 ± 0.16 | 0.35 ± 0.1*** | 0.50 ± 0.16# |
| 22:6 n-3 | 3.84 ± 1.06 | 2.22 ± 0.74*** | 2.53 ± 0.71 |
| SFA | 38.64 ± 2.12 | 45.26 ± 2.73*** | 46.04 ± 2.29 |
| MUFA | 12.09 ± 1.68 | 15.39 ± 2.41*** | 16.0 ± 1.27 |
| PUFA | 49.22 ± 1.92 | 39.34 ± 3.38*** | 37.95 ± 2.65 |
| n-6 | 44.27 ± 1.80 | 36.59 ± 3.24*** | 34.38 ± 2.38 |
| n-3 | 4.96 ± 1.28 | 2.75 ± 0.78*** | 3.58 ± 0.9# |
| n-6/n-3 | 9.47 ± 2.39 | 14.24 ± 3.55** | 10.24 ± 2.78# |
All data are presented as a mean ± SE. Fatty acids concentrations are expressed in % of totally detected FA. SFA-saturated fatty acids. MUFA-monounsaturated fatty acids. PUFA- polyunsaturated fatty acids. **p<0.01, ***p<0.001-between control group and patients before treatment. #p<0.05, ###p<0.001 intergroups compared baseline to after 7 day supplementation.
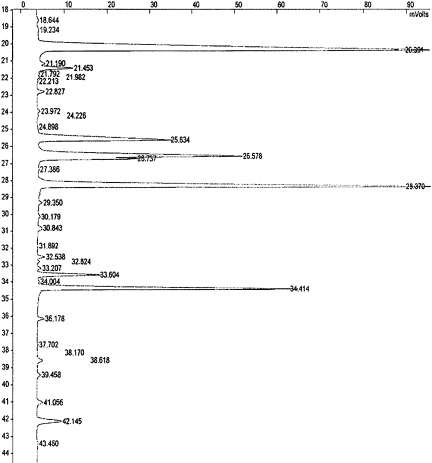
After 7 days supplementation with high doses of EPA (0.9 g per day) and DHA (0.6 g per day), we repeated determination of FA in plasma PL. We found significantly increased content of total n-3 FA and particularly EPA, which increased more than 3 fold (Table 1). The percentage of DHA was also higher, but the increase was not siginificant, while a significant increase in 22:5 n-3 FA was detected as well. In addition, the n6/n3 ratio significantly decreased from 14.24 to 10.24, demonstrating severely improved plasma phospholipid profile in these patients after the intervention. A representative GC chromatogram derived from one patient before the intervention is presented in Fig. 1.
Fig. 1.
A representative example of a GC chromatogram derived from the obstructive jaundice patient before the n-3 PUFA supplementation.
Furthermore, the estimated desaturase acitivies are presented in Table 2. Judging by the 20:4/18:2 ratio as an index of total Δ6 and Δ5 desaturase activities, these enzymes are significantly more active in healthy persons than in obstructive hepatitis patients (p<0.01). On the contrary, the 18:1/18:0 ratio as a measure of action Δ9 desaturase, was significantly higher in the jaundice patients (p<0.05). After the supplementation with n-3 FA, the 22:6/22:5 ratio significantly decreased (p<0.05) in the patients. It could be explained by an increase in DPA after the supplementation with fish oil, rather than by a decrease in Δ4 desaturase activity.
Table 2.
The estimated desaturase activities in control subjects and in patients with obstructive jaundice before and after the n-3 FA supplementation.
| Fatty acids ratio | Control group | Patients, baseline | Patients, after supplementation |
|---|---|---|---|
| 20:4/18:2 | 0.45 ± 0.11 | 0.36 ± 0.07* | 0.38 ± 0.06 |
| 20:4/20:3 | 5.15 ± 2.18 | 3.83 ± 1.16 | 3.95 ± 1.18 |
| 22:6/22:5 | 5.53 ± 1.45 | 6.81 ± 2.96 | 5.21 ± 0.96# |
| 18:1/18:0 | 0.81 ± 0.16 | 1.08 ± 0.27** | 1.13 ± 0.22 |
Discussion
Many abnormalities have been described in obstructive jaundice, but the poor outcome in these patients is still unclear. Immune and reticuloendothelial dysfunction seem to be important in major complications [14]. A number of clinical intervention studies indicate that n-3 PUFA have anti-inflammatory properties and therefore, might be useful in the management of inflammatory and autoimmune diseases [4, 15]. At sufficiently high intakes, long-chain n-3 PUFAs, as found in oily fish and fish oils, decrease the production of inflammatory eicosanoids, cytokines, and reactive oxygen species and the expression of adhesion molecules [16]. As we already mentioned above, the n-3 PUFAs particularly decrease production of arachidonic acid-derived eicosanoids, as well as the production of the classic inflammatory cytokines tumour necrosis factor, IL-1, IL-6 and the expression of adhesion molecules involved in inflammatory interactions between leukocytes and endothelial cells. These latter effects may occur by eicosanoid-independent mechanisms including modulation of the activation of transcription factors involved in inflammatory processes [15, 17]. Long-chain n-3 PUFAs also give rise to a family of anti-inflammatory mediators termed resolvins [17].
Considering all these reasons, in this study we evaluated the FA profile including the n-3 status in plasma phospholipid in patients with obstructive jaundice, who were waiting for surgical intervention. All patients had significantly impaired lipid profile compared with healthy subjects. For instance, we found significantly lower level of two n-6 FA, LA and AA, in jaundice patients. The decreased LA percentage could be explained with absorption disorder in patients with obstructive jaundice [18]. Regarding that AA is synthetised from LA by an action of desaturase and elongase, lower level of AA is probably a consequence of decreased LA pool, as well as inadequate activity of elongase and desaturase system in patients with obstructive jaundice. Contrary to our results, Wardle et al. [14] reported similar percentages of AA in the plasma cholesterol-esters fraction in control subjects and in jaundice patients.
However, our pilot study clearly showed that obstructive jaundice patients after seven days supplementation of n-3 PUFA began the absorption of EPA and DHA and its incorporation into plasma phospholipid composition, that was confirmed by improved plasma PL profile in these patients. The achieved percentages of EPA were even higher than in healthy subjects. The rise in EPA was compensated by a decrease in LA and with slight changes in AA in our study, which is similar to results of Katan et al. [19]. An increased proportion of 22:5 n-3 was also detected, although the patients were not taken this FA as a supplement, but it was obviously synthetised from EPA. After 7 days supplementation of n-3 FA, EPA and DPA (22:5 n-3) significantly increased, while DHA level was almost the same in plasma PL. Despite the relatively short term of supplementation, some authors reported higher proportion of EPA in the cholesterol esters after only 3 days of supplementation in healthy population. In the same study DHA concentration was also increased but in a less degree and more unstable than EPA, within an average of 10.3 days [19]. The weak alteration in DHA could be explained by a longer chain of DHA compared to EPA, or DHA maybe was not incorporated into plasma PL yet, because of too short time for incorporation during supplementation. Supplementation of n-3 FA, however, did not significantly affect the levels of AST, ALT and gama GT, which showed only a slight decrease (data not shown).
The activities of desaturase enzymes were estimated according to the ratios between single FA. We found an increased action of Δ9 desaturase (18:1/18:0 ratio) in patients with obstructive jaundice. The action of Δ9 desaturase is often increased in patients with decreased both n-3 and n-6 PUFA [20]. Regarding significantly lower level of n-3 and n-6 PUFA in plasma of jaundice patients compared to control group, our results are in accordance with previously published [20]. On the contrary, 20:4/18:2 ratio suggesting total Δ6 and Δ5 desaturase activities, was higher in healthy subjects than in our patients. One of the reason could be decreased absorbtion of LA and AA synthesis in obstructive jaundice which led to a lower ratio of 20:4/18:2. In addition, desaturase activity is probably decreased due to the liver disorder, regarding that desaturase and elongase system, as well as PUFA synthesis, are mainly in the liver. Although we did not investigate the aetiology of the FA abnormalities in this study, possibilities include malabsorbtion of essential FA and dysfunction of hepatic FA desaturase enzymes. The direction of observed changes is consistent with the hypothesis that FA abnormalities underlie many of the changes in obstructive jaundice, especially those in immune and reticuloendothelial function. However, the better understanding of the relationship between FA profile improvement and prevention against immune dysfunction requires additional investigations.
Our results indicated the possible need of n-3 PUFA supplementation to a regular hospital diet in patients with obstructive jaundice before surgical treatment. We propose that it may lead at least in part to a better immune response and also in beneficial effect of gastroinestinal surgery. In spite of this conclusion, we have not examined the immunological parameters so far, as well as the fact that the absorption of n-3 PUFA in these patients was happened without participation of bile itself. Our future examinations would address these data.
Acknowledgments
This work was supported by the Project 145071 financed by the Ministry of Science of the Republic of Serbia.
References
- 1.Jiang W.G., Puntis M.C.A. Immune dysfunction in patients with obstructive jaundice, mediators and implications for treatments. H.P.B. Surgery. 1997;10:129–142. doi: 10.1155/1997/49076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunt D.R., Allison M.E.M., Prentice C.R.M., Blumgart L.H. Endotoxaemia, disturbance of coagulation and obstructive jaundice. Am. J. Surg. 1982;144:325–329. doi: 10.1016/0002-9610(82)90011-3. [DOI] [PubMed] [Google Scholar]
- 3.Greig J.D., Krukowski Z.H., Matheson N.A. Surgical morbidity and mortality in one hundred and twenty nine patients with obstructive jaundice. Br. J. Surg. 1988;75:216–219. doi: 10.1002/bjs.1800750309. [DOI] [PubMed] [Google Scholar]
- 4.Simopoulos A.P. Omega3 fatty acids in inflammation and autoimmune diseases. J. Am. Coll. Nutr. 2002;21:495–505. doi: 10.1080/07315724.2002.10719248. [DOI] [PubMed] [Google Scholar]
- 5.Sit E.N., Frits A.J., Muskiet E., Boersma R. The possible role of essential fatty acids in the pathophysiology of malnutrition: a review. Prostaglandins Leukot. Essent. Fatty Acids. 2004;71:241–250. doi: 10.1016/j.plefa.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Alexander J.W. Immunonutrition: the role of omega-3 fatty acids. Nutrition. 1998;14:627–633. doi: 10.1016/s0899-9007(98)00004-5. [DOI] [PubMed] [Google Scholar]
- 7.Miles E.A., Calder P.C. Modulation of immune function by dietary fatty acids. Proc. Nutr. Soc. 1998;57:277–292. doi: 10.1079/pns19980042. [DOI] [PubMed] [Google Scholar]
- 8.Caughey G.E., Gibson R.A., James M.J. The effect on human tumor necrosis factor α and interleukin 1β production of diets enriched in n-3 fatty acid from vegetable oil or fish oil. Am. J. Clin. Nutr. 1996;63:116–122. doi: 10.1093/ajcn/63.1.116. [DOI] [PubMed] [Google Scholar]
- 9.Crocker I., Lawson N., Fletcher J. Effect of pregnancy and obstructive jaundice on inflammatory diseases: the work of P S Hench revisited. Ann. Rheum. Dis. 2002;61:307–310. doi: 10.1136/ard.61.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chilton L., Surette M.E., Swan D.D., Fonteh A.N., Johnson M.M., Chilton F.H. Metabolism of gammalinolenic acid in human neutrophils. J. Immunol. 1996;156:2941–2947. [PubMed] [Google Scholar]
- 11.Trebble T.M., Wootton S.A., Miles E.A., Mullee M., Arden N.K., Ballinger A.B., Stroud M.A., Burdge G.C., Calder P.C. Prostaglandin E2 production and T cell function after fish-oil supplementation: response to antioxidant cosupplementation. Am. J. Clin. Nutr. 2003;78:376–382. doi: 10.1093/ajcn/78.3.376. [DOI] [PubMed] [Google Scholar]
- 12.Sperry M.W., Brand F.C. The determination of total lipides in blood serum. J. Biol. Chem. 1954;3:69–76. [PubMed] [Google Scholar]
- 13.Ristic M.D., Ristic V., Tepsic V., Ranic M., Ristic G., Vrbaski S., Estelacki I. Effect of soybean leci-vita product on serum lipids and fatty acids composition in patients with elevated serum cholesterol and triglyceride levels. Nutr. Res. 2003;23:465–477. [Google Scholar]
- 14.Wardle E.N., Wright N.A. Endotoxin and acute renal failure associated with obstructive jaundice. Br. Med. J. 1970;4:472–474. doi: 10.1136/bmj.4.5733.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawayami Y., Murakami Y., Kawakami T., Muroyama N., Takiue T., Moritani Y., Okita M. Abnormal fatty acid profile of blood cell phospholipids and dietary fatty acid intake in patients with ulcerative colitis. J. Clin. Biochem. Nutr. 2005;37:95–102. [Google Scholar]
- 16.Hirai K., Kozuki M., Miyanaga K., Miyagawa F., Takezoe R., Hasegawa M., Mori M. Lower levels of eicosapentaenoic acid and the ratio of docosahexanoic acid to arachidonic acid in sera of patients with milti-infarct dementia. J. Clin. Biochem. Nutr. 2005;36:83–89. [Google Scholar]
- 17.Calder P.C. n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am. J. Clin. Nutr. 2006;83:1505S–1519S. doi: 10.1093/ajcn/83.6.1505S. [DOI] [PubMed] [Google Scholar]
- 18.Crocker I.P., Lawson N., Baker P.N., Fletcher J. The anti-inflammatory effects of circulating fatty acids in obstructive jaundice: similarities with pregnancy-induced immunosuppression. Q. J. Med. 2001;94:475–484. doi: 10.1093/qjmed/94.9.475. [DOI] [PubMed] [Google Scholar]
- 19.Katan M.B., Deslypere J.P., Van Birgelen A.P., Penders M., Zegwaard M. Kinetics of the incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue: an 18-month controlled study. J. Lipid Res. 1997;38:2012–2022. [PubMed] [Google Scholar]
- 20.William H.S., James P., Scott S., Jones P. Comparation of the effects of fish and fish-oil capsules on the n-3 fatty acid content of blood cells and plasma phospholipids. Am. J. Clin. Nutr. 2007;86:1621–1625. doi: 10.1093/ajcn/86.5.1621. [DOI] [PubMed] [Google Scholar]