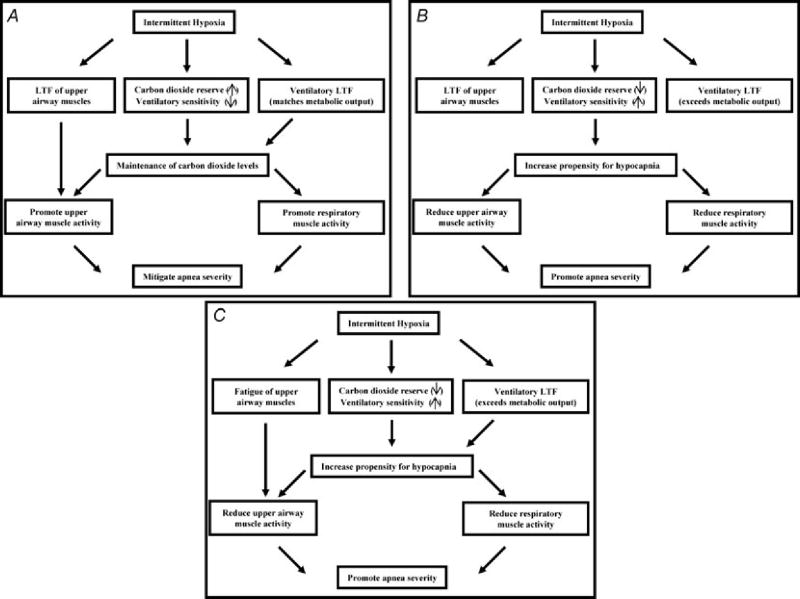
Figure 3. Three scenarios that address the potential influence of intermittent hypoxia on apnea severity.
A, the ideal scenario is presented in which exposure to intermittent hypoxia promotes breathing stability. In this scenario, exposure to intermittent hypoxia leads to long-term facilitation of upper airway muscle activity, promoting the maintenance of upper airway patency. Likewise, carbon dioxide reserve is unaltered or increased while ventilatory sensitivity is unaltered or reduced. These chemoreflex characteristics promote the maintenance of carbon dioxide levels, ensuring that hypocapnia does not develop, which could restrain the manifestation of LTF of upper airway muscle activity. Ultimately, this integrated response promotes breathing and potentially mitigates the severity of apnoea. B, a scenario in which long-term facilitation is induced in upper airway muscles following exposure to intermittent hypoxia but ultimately is ineffective in mitigating apnoea because decreases in carbon dioxide reserve and increases in chemoreflex sensitivity increase the propensity for developing hypocapnia. The induced hypocapnia restrains LTF of upper airway muscle activity and respiratory muscle activity, ultimately resulting in the promotion of apnoea. C, a scenario in which exposure to intermittent hypoxia leads to fatigue of the upper airway muscles and results in a decrease in the carbon dioxide reserve and increase in chemoreflex sensitivity, ultimately resulting in a worse case scenario that results in the promotion of apnoea.