Figure 1.
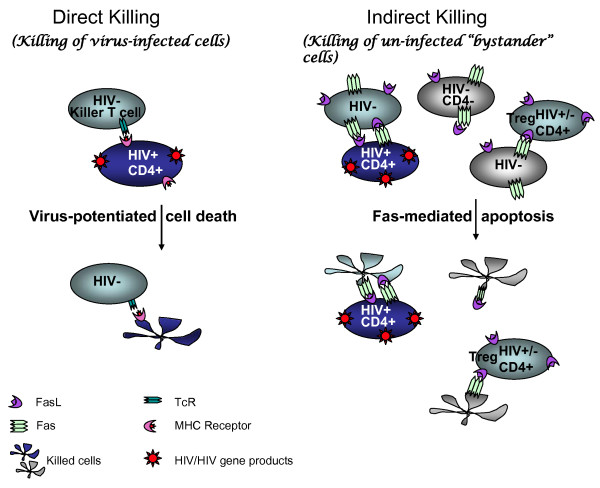
Major mechanisms of leukocyte cell loss in AIDS. Two models for cell death in AIDS are the direct and indirect killing of leukocytes during disease progression. Direct killing, or killing of virus-infected cells, is presumed to be virus-mediated or to occur via immune surveillance of virus-infected cells, most often by killer T cells. The virus-infected cells are predominately memory T cells with the phenotype CD4+CD45RA- or CD4+CD45RA+Fas and are primarily killed by cytotoxic T cells in a Fas-independent manner [52]. Indirect cell death, or killing of uninfected "bystander" cells, has also been documented in vivo. All leukocytes, including uninfected bystander cells, can be activated, with up-regulation of Fas/FasL and other death mediators, after contact with HIV-infected cells or HIV antigens such as soluble tat, gp120, vpr, and nef [20,24,38,39,49]. Thus HIV gene expression contributes to both direct and indirect killing mechanisms. Contact with death ligands like FasL causes apoptosis of activated cells through Fas/FasL signaling. Tregs are major effectors of bystander killing. The finding that HIV+ cells are less susceptible to Fas/FasL killing means that HIV+ cells become enriched when Fas-mediated apoptosis is the major death pathway.
