Abstract
The secreted metastasis-inducing protein, human anterior gradient 2 (AGR2), has been independently reported to be associated with either a reduced or an increased survival of different groups of patients with breast cancer. We now aim to analyze the expression of AGR2 in a third completely independent group of patients using a specific AGR2 monoclonal antibody (mAb). Primary tumors from a group of 315 patients suffering from operable (stage I and II) breast cancer with 20-years follow-up were immunocytochemically stained with a specific mAb to AGR2 and associations with prognostic factors and patient survival were analyzed. The mAb specifically recognized AGR2 in Western blots, and positive staining for AGR2 was significantly associated with involved lymph nodes and staining for estrogen receptor α, progesterone receptor, and the metastasis-inducing proteins osteopontin, S100P, and S100A4. After 20 years of follow-up, only 26% of patients with AGR2-positive carcinomas survived compared with 96% of those with AGR2 negative carcinomas, with the highly significant difference in median survival times of 68 and >216 months, respectively (P < 0.0001). Cox’s multivariate regression analysis showed that staining for AGR2 was one of the most significant independent prognostic indicators, with a corrected relative risk of 9.4. The presence of AGR2 in the primary tumor is therefore a possible prognostic indicator of poor patient outcome in breast cancer.
Anterior gradient 2 (AGR2) protein is a secreted protein first described in Xenopus laevis embryos, where it induces the formation of the forebrain and the mucus-secreting cement gland.1 Human AGR2 is also found co-expressed with estrogen receptor α (ERα) in breast cancer cell lines2 and its presence significantly correlates with ERα in breast carcinoma specimens.3 Subsequent studies have found elevated expression of AGR2 in adenocarcinomas of the esophagus, pancreas, prostate, and non-small cell lung cancer, showing that it is a widely overexpressed protein in human carcinomas.4,5,6,7,8,9,10 We have shown that human AGR2 is expressed at higher levels in malignant, rather than in benign breast tumors,11 and that, when introduced in an expression vector into the benign, nonmetastatic rat mammary cell line, Rama 37,12 it causes metastasis in syngeneic rats.11 These results suggest that AGR2’s metastasis-inducing properties may contribute toward the malignant progression of some breast cancers. Certain molecules shown to induce metastasis in experimental breast cancer in rodents, for example, S100A4, S100P, and osteopontin (OPN),13,14,15,16 provide a potential source for markers that may be useful as prognostic factors in predicting patient outcome in human breast cancer.
Using a polyclonal antibody (PAb) to AGR2, a strong positive association was shown between AGR2 and ERα and between AGR2 and low histological grade in a retrospective cohort of 351 breast cancer patients treated by adjuvant hormonal therapy.17 In these patients, levels of AGR2 were also associated with a relatively poor outcome in patients with ERα-positive breast cancers after treatment with antiestrogen therapy.17 In contrast to these results, it has been reported that in another panel of 155 breast carcinoma patients treated with various adjuvant therapies, immunocytochemically detected AGR2 in the cancer cells was associated with significantly longer patient survival times, although there was still a significant correlation with the presence of ERα and lower tumor grade.18 To resolve these apparent conflicting associations of AGR2 protein with patient survival, the expression of immunocytochemically detectable AGR2 protein has now been determined in the primary tumors of an independent group of 315 patients suffering from operable breast cancer and treated by surgery alone with no accompanying adjuvant therapy. A new specific monoclonal antibody (mAb) to AGR2, which does not cross-react with the closely-related AGR3 protein,3 has been used to improve the accuracy of detection of AGR2. The results show that, in this large group of breast cancer patients, the presence of immunocytochemically detectable AGR2 protein in the primary tumor is strongly associated with a reduced survival of the corresponding patients.
Materials and Methods
Patients and Specimens
Archival paraffin-embedded specimens were obtained from the primary tumors of 315 unselected patients suffering from operable (stage I and stage II) breast cancer and treated by simple mastectomy with sampling of axillary lymph nodes (17%) or modified radical mastectomy (83%), no adjuvant therapy including hormonal therapy was given.13,14,16,19,20 The archival blocks were stored at room temperature in a modern centrally controlled air-conditioned histology laboratory. All sections were freshly cut and immunocytochemical staining was checked periodically with no loss of antigenicity observed. The patients presented to general surgery clinics in the Merseyside region between 1976 and 1982 and had ages ranging from 29 to 92 years, mean 57 years, and 98.5% had invasive carcinoma of no special type. Patients were followed up for 14 to 20 years, mean 16 years. The distribution of menopausal status, treatment, tumor type, tumor size, histological grade, and lymph node status was as described previously13,14,15 (Table 1). Summary of overall patient survival and for the significant pathological prognostic variables over 20 years is shown in Table 2. Local Ethics Committee Approval was obtained and the patient data were anonymized.
Table 1.
Clinical, Pathological, and Molecular Characteristics of the Patient Cohorts
| Tumor variable | Positive tumors (%) | Negative tumors (%) | Missing samples |
|---|---|---|---|
| Menopausal status | |||
| Premenopausal | 70 (23.7%) | ||
| Postmenopausal | 218 (73.9%) | ||
| Oophrectomy | 7 (2.4%) | ||
| Missing | 20 | ||
| Treatment | |||
| Simple mastectomy | 53 (16.8%) | ||
| Modified radical mastectomy | 262 (83.2%) | ||
| Missing | 0 | ||
| Tumor type | |||
| Invasive ductal carcinoma | 291 (92.4%) | ||
| Invasive lobular carcinoma | 19 (6.1%) | ||
| Special type colloid and medullary carcinoma | 5 (1.5%) | ||
| Missing | 0 | ||
| Tumor size | |||
| T1 <2 cm in diameter | 32 (10.5%) | ||
| T2 ∼2–5 cm in diameter | 201 (66.1%) | ||
| T3 >5 cm in diameter | 53 (17.4%) | ||
| T4 fixed to chest wall | 18 (5.9%) | ||
| Missing | 11 | ||
| Histological grade | |||
| I | 73 (25.8%) | ||
| II | 138 (48.8%) | ||
| III | 72 (25.4%) | ||
| Missing | 32 | ||
| Involved lymph nodes | 108 (46.8%) | 123 (53.2%) | 84 |
| ERα staining | 166 (39.3%) | 142 (60.7%) | 7 |
| PgR staining | 115 (38.3%) | 185 (61.7%) | 15 |
| AGR2 staining | 208 (66%) | 107 (34%) | 0 |
| C-erbB-2 staining | 71 (23%) | 238 (77%) | 6 |
| C-erbB-3 staining | 180 (59.2%) | 124 (40.8%) | 11 |
| S100A4 staining | 126 (40.3%) | 187 (59.7%) | 2 |
| S100P staining | 147 (53.3%) | 129 (46.7%) | 39 |
| p53 staining | 124 (39.6%) | 189 (60.4%) | 2 |
| Cathepsin D staining | 201 (82.4%) | 43 (17.6%) | 71 |
| pS2 staining | 129 (41.6%) | 181 (58.4%) | 5 |
| Osteopontin staining | 202 (67.1%) | 99 (32.9%) | 14 |
Tumor variables and cutoffs used in immunocytochemical staining to separate the two categorical groups are described in Materials and Methods.
Table 2.
Summary of Overall Patient Survival and for the Significant Pathological Prognostic Variables
| Follow-up | Proportion of surviving patients ± 95% CI* (Probability, P value†)
|
|||||
|---|---|---|---|---|---|---|
| 5 years | P value | 10 years | P value | 20 years | P value | |
| All patients | 0.67 ± 0.03 | 0.56 ± 0.03 | 0.50 ± 0.03 | |||
| Tumor variables | ||||||
| Tumor size‡ | ||||||
| <5 cm | 0.71 ± 0.03 | 0.018 | 0.60 ± 0.03 | 0.026 | 0.55 ± 0.04 | 0.024 |
| >5 cm | 0.57 ± 0.06 | 0.46 ± 0.06 | 0.39 ± 0.06 | |||
| Histological grade‡ | ||||||
| I, II | 0.71 ± 0.03 | 0.002 | 0.60 ± 0.03 | 0.001 | 0.53 ± 0.04 | 0.003 |
| III | 0.49 ± 0.06 | 0.38 ± 0.06 | 0.38 ± 0.06 | |||
| Lymph nodes‡ | ||||||
| − | 0.76 ± 0.04 | 0.001 | 0.65 ± 0.04 | <0.0001 | 0.57 ± 0.05 | <0.0001 |
| + | 0.56 ± 0.05 | 0.44 ± 0.05 | 0.40 ± 0.05 | |||
Cumulative proportions surviving ±1.96 SD to give ±95% CI.
Significance of difference between subgroups calculated using Wilcoxon Gehan statistics 1 degree of freedom (1 d.f.).
Subgroups: tumor size T1, T2 <5 cm versus T3, T4 >5 cm in diameter; histological grade I, II, versus III; and lymph nodes without (−, negative) vs with (+, positive) involved tumors.
Immunocytochemical Staining
Histological sections were cut at 4 μm on 3-aminopropyltriethoxysilane-coated slides.21 To enhance the immunocytochemical staining, antigen retrieval was undertaken in 10 mmol/L citrate buffer at pH 6.0 in a microwave oven for 15 minutes at 850 W.22 Endogenous peroxidase activity was blocked with 0.05% (v/v) H2O2 in methanol.23 Mouse mAb to human AGR2 was affinity-purified from the patented hybridoma clone 7A10 (PCT/GB2007/003235), produced against a peptide (Eurogentec, Seraing, Belgium), unique to human AGR2 and not present in human AGR3. mAb was diluted 1/100 in 0.5% (w/v) bovine serum albumin in PBS and applied to the slides for 16 hours at room temperature. Indirect immunocytochemical staining was performed according to the manufacturer’s instructions with the DAKO EnVision+ System kit (DakoCytomation, Glostrup, Denmark). Nuclei were counterstained blue in Mayers’ hemalum. Blocked mAb was prepared by mixing with 700 μg/ml purified human recombinant AGR2 (rAGR2) or rAGR3 protein.11,17 Affinity-purified rabbit PAb to AGR211 was used at 1/400 and visualized with 1/200 diluted biotinylated donkey anti-rabbit Ig (Amersham Biosciences, Amersham, UK) in an AB Complex (Amersham Biosciences)24 to confirm the results. Photographs were recorded on a Reichert Polyvar microscope fitted with a Wratten 44 blue-green filter on Ilford Pan F plus, black-and-white film. Stained sections were scored using light microscopy by two independent observers according to the percentage of carcinoma cells positive for AGR2, from two sections of each specimen, 10 fields per section at ×200 magnification. Scores were divided into five classes: negative (−), <1%; borderline (±), 1 to 5%; intermediate (+), 5 to 25%; moderate (++), 25 to 50%; and strong (+++), 50 to 100% of carcinoma cells stained.13 The use of the percentage of stained cells gave more reliable and accurate results than using intensity alone or in combination, which tended to inflate the scores.
Immunocytochemical staining data on the same set of patients had been obtained previously for S100A4,13 OPN,14 c-erbB-2, c-erbB-3, ERα, progesterone receptor (PgR), pS2, p5325 and S100P16 using a 5% cut-off and for cathepsin D20 using a 1% cut-off to differentiate between the negatively and positively staining carcinomas (Table 1). These cut-offs yielded the highest risk factors between the two groups in this particular set of patients.
Western Blotting
Approximately 10 μg of protein extract from tumor specimens14 and from the cultured normal (Huma 7), benign (Huma 123 and Huma 109), and malignant (T47D, ZR-75, MCF-7, MDA-MB-231) human breast cell lines11 was subjected to SDS-PAGE on 12.5% (w/v) polyacrylamide gels. The resolved proteins were electro blotted onto polyvinylidine difluoride membranes as previously described 11 but using the primary mAb to AGR2 without or with 1 mg/ml human rAGR2 protein and a secondary anti-mouse HRP-conjugated IgG diluted 1/1000. Bound antibody was detected by the SuperSignal West Pico Chemiluminescent Substrate (Pierce Biotechnology Inc., Northumberland, UK). Chemiluminescent signals were collected using a ChemiDoc XRS system and analyzed using Quantity One software (Bio-Rad, Hercules, CA). Membranes were reprobed with a rabbit PAb to β-actin (New England BioLabs UK, Hitchin, UK) and the level of AGR2 was normalized to that of β-actin.11
Statistical Analyses
Statistical analysis of Western blot and immunocytochemical staining was performed by least-squares regression using StatsDirect software version 2.6.2 (StatsDirect, Cheshire, UK). Cross tabulation was used to compare groups in negative and positive categories for two tumor variables. Any significant association of mAb staining for AGR2 with pathological and molecular variables was tested using a two-tailed Fisher’s Exact test. Tumor variables used were tumor size, histological grade, nodal status, staining for S100P, OPN, ERα, c-erbB-2, c-erbB-3, S100A4, PgR, p53, pS2, cathepsin D and AGR2 stained by the PAb. The cut-off value between those groups of patients designated negatively or positively stained for AGR2 and for the other proteins was set at 1 or 5% as specified above.
Analysis of patient survival was performed over a follow-up period of 240 months, those who died of causes other than cancer were eliminated. The association of staining for AGR2 in primary breast cancers with patient survival was calculated from life tables constructed from survival data using Kaplan-Meier plots, and analyzed using generalized Wilcoxon (Gehan) statistics.26 Unadjusted relative risk (RR) for survival and 95% confidence intervals (95% CI) for each staining class was calculated using Cox’s univariate analysis.13 Classes were then divided into the two categorical groups with the greatest difference in survival (negative <1% and positive >1%) for subsequent survival analyses for staining for AGR2. To determine the relative contribution to patient survival, a multivariate analysis was performed using the Cox’s proportional hazards model on 166 patients with full data sets.27 Data processing and analyzing was performed using Excel 2007 (Microsoft, Redmond, WA), and all statistical calculations were performed using SPSS version 16.0 (SPSS, Chicago, IL).
Results
Immunocytochemical Staining of Human Breast Carcinomas for AGR2
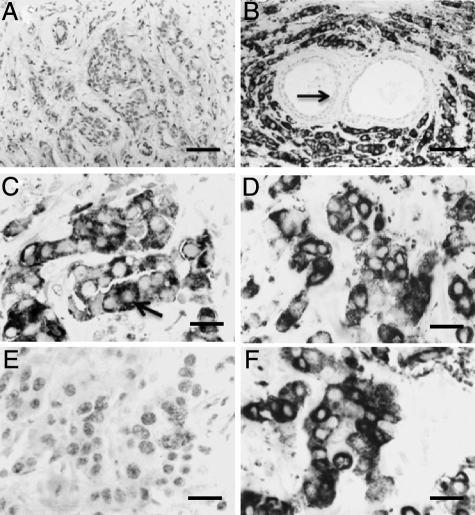
Histological sections of primary tumors from different invasive carcinomas showed a heterogenous staining pattern when incubated with mAb to AGR2, ranging from no staining (Figure 1A), to strongly positive staining for AGR2 (Figure 1B). Normal glandular tissue was usually unstained, and there was no staining of host stromal cells (Figure 1B). Immunocytochemical staining for AGR2 was located primarily in secretory granules in the cytoplasm and on the surface of carcinoma cells (Figure 1C). When serial sections of the same positively staining carcinoma (Figure 1D) were incubated with mAb to AGR2 plus 700 μg/ml human rAGR2, staining was abolished entirely but not with rAGR3 (Figure 1, E and F). When 315 breast carcinomas were examined, 107 (34%) were classified as not staining (−; <1% carcinoma cells stained), 93 (30%) showed borderline staining (±; 1 to 5% carcinoma cells stained), 61 (19%) were intermediately stained (+; 5 to 25% carcinoma cells stained), 26 (8%) were moderately stained (++; 25 to 50% carcinoma cells stained), and 28 (9%) were strongly stained (+++; >50% carcinoma cells stained) for AGR2 (Materials and Methods). For patient survival analyses, the moderate (++) and strongly (+++) staining groups were combined into one single group of 54 (17%) carcinomas due to the small number of patients in these groups. For generation of two categorical immunocytochemical staining groups, the borderline staining carcinomas (±) were combined with the positive staining carcinomas (+, ++, +++) into one group of positively stained carcinomas, leaving the clearly negatively stained carcinomas (−) as the other categorical group. There was a high level of consistency in scoring for the mAb to AGR2 between the two observers with agreement in 91.2% of cases, corresponding to a kappa score of 0.82. Intratumor heterogeneity was 5.0% for two well separated sections of the same carcinoma. The level of agreement with the PAb was not quite so high between observers at 87.4% (κ = 0.73) or between widely separated sections at 11.0%.
Figure 1.
Immunocytochemical staining of primary carcinomas by AGR2 mAb. A: Section of an invasive carcinoma showing no immunocytochemical staining for AGR2. B: Section of an invasive carcinoma showing strong positive staining for AGR2 (+++). The normal glandular tissue is unstained (arrow). C: Section of an invasive carcinoma at higher magnification showing positive staining for AGR2 (+++) in secretory granules (arrow). D–F: Serial sections of the same carcinoma incubated with D, mAb to AGR2 showing positive cytoplasmic staining (+++); E, mAb to AGR2 plus 700 μg/ml recombinant AGR2 showing no staining; or F, mAb to AGR2 plus 700 μg/ml recombinant AGR3 showing no diminution of positive staining (+++) over that in D. Magnification, A and B, ×220; C, ×685; D–F, ×545. Bars, A and B, 50 μm; C, 15 μm; D–F, 20 μm.
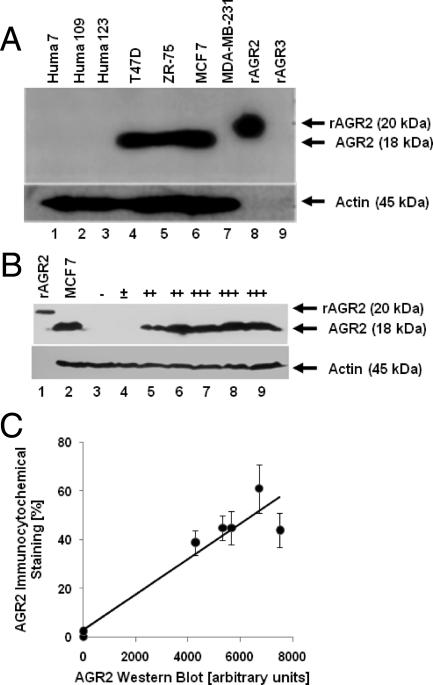
Western Blots for AGR2
A single positive immunoreactive band was observed on Western blots with mAb to AGR2 in cell extracts from ERα-positive human breast carcinoma cell lines, T47D, ZR-75, and MCF-7; but was not detectable in ERα-negative normal Huma 7, benign Huma 109, and Huma 123 or malignant MDA-MB-231 breast epithelial cell lines (Figure 2A). The size of the mAb immunoreactive band is consistent with the expected size of native AGR2.11 mAb to human AGR2 reacted with human rAGR2 protein, but not with human rAGR3 protein (Figure 2A). The same sized mAb immunoreactive band for AGR2 was detected in extracts from five of the seven human breast carcinomas tested (Figure 2B). The proportions of immunoreactive AGR2, determined by scanning densitometry of Western blots, showed a good correlation with the percentage of immunocytochemically stained carcinoma cells from histological sections of the same carcinomas (correlation coefficient, r2 = 0.92, P < 0.0001) (Figure 2C). Hence, the percentage of stained carcinoma cells was a reasonable estimate of the level of immunoreactive AGR2 in the specimen.
Figure 2.
Western blots of AGR2 protein in human mammary cell lines and clinical tumor specimens using mAb. A: Protein samples (10 μg) from human mammary cell lines were: Huma 7 (lane 1), Huma 109 (lane 2), Huma 123 (lane 3), T47D (lane 4), ZR-75 (lane 5), MCF-7 (lane 6), and MDA-MB-231 (lane 7). Controls of 0.5 μg of purified recombinant protein AGR2 (rAGR2) (lane 8) and rAGR3 (lane 9) were also included. B: Protein samples from purified recombinant rAGR2 (0.5 μg) (lane 1), from human breast cancer cell line, MCF7 (10 μg) (lane 2), and from invasive carcinomas (10 μg) of the following classes of immunocytochemical staining for AGR2: unstained negative (−; lane 3), borderline (±; lane 4), moderate (++; lanes 5 and 6) and strong (+++; lanes 7 to 9) were analyzed. Samples were subjected to SDS-PAGE using 12.5% (w/v) polyacrylamide gels and transferred to polyvinylidene difluoride membranes (Materials and Methods). The membranes were incubated with mAb to AGR2 (A and B, top), reprobed with anti-β-actin (A and B, bottom), and visualized by chemiluminescence. The position of recombinant rAGR2, natural AGR2 and actin are shown on the right (Materials and Methods). C. Relationship between Western blotting and immunocytochemical staining of primary carcinomas for AGR2. The mean (n = 3)of scanning densitometry of the 18-kDa band in representative Western blots shown in B normalized for variations in β-actin levels were plotted against the mean ± SD of the percentage of positively stained carcinoma cells. Least squares regression analysis produced a straight line y = 0.0072x + 3.3781 with an r2 value of 0.92, and P < 0.0001, where r2 = 1 is a perfect fit.
Association of AGR2 with Other Tumor Variables
Immunocytochemical staining of AGR2 was compared with other tumor variables reported to be predictive of patient outcome; these included tumor size, histological grade, nodal status, and the presence of immunoreactive ERα, PgR, OPN, S100P, S100A4, c-erbB-2, c-erbB-3, pS2, p53, and cathepsin D and assessed using Fisher’s Exact test. For this purpose, the borderline staining group of carcinomas for AGR2 (±) was combined with the stained carcinomas (+, ++, +++) into one group of positive staining carcinomas (±, +, ++, +++), leaving the clearly negative carcinomas (−) as the other group, ie, using 1% cut-off. The cut-off level used for the other tumor variables was the one that achieved the most significant difference in patient outcome in this group of patients (Materials and Methods). All tumor variables, except histological grade, tumor size, c-erbB-2, p53 and cathepsin D, showed a significant association with positive staining for AGR2 (P < 0.05), the most significant were staining for PgR, OPN, S100P, and S100A4 (P < 0.0001) (Table 3). The same group of carcinomas immunocytochemically stained by PAb to AGR2 yielded similar associations, the most significant being staining for ERα, OPN, S100P, and S100A4 (P < 0.0001) (data not shown). As expected, staining with mAb to AGR2 and with PAb to AGR2 were highly significantly associated (P < 0.0001) (Table 3). When the association of staining by mAb to AGR2 with the other tumor variables was investigated using the 5% cut-off level, the variables found to have a significant association were: involved lymph nodes (P = 0.05) and staining for ERα (P = 0.01), PgR (P = 0.05), pS2 (P < 0.0001), c-erbB-3 (P = 0.001), OPN (P < 0.0001), S100P (P < 0.0001), S100A4 (P < 0.0001), and PAb staining for AGR2 (P < 0.0001).
Table 3.
Association of Staining by mAb to AGR2 with Other Tumor Variables
| Tumor variable* | AGR2-negative† no. (%) | AGR2-positive† no. (%) | Statistical significance‡ |
|---|---|---|---|
| Node negative | 48 (63.2) | 75 (48.4) | 0.036§ |
| Node positive | 28 (36.8) | 80 (51.6) | |
| Grade I, II | 67 (75.3) | 146 (74.5) | 1 |
| Grade III | 22 (24.7) | 50 (25.5) | |
| Tumor <5 cm | 83 (80.6) | 150 (74.6) | 0.26 |
| Tumor >5 cm | 20 (19.4) | 51 (25.4) | |
| ERα negative | 64 (58.7) | 81 (39.7) | 0.002§ |
| ERα positive | 45 (41.3) | 123 (60.3) | |
| PgR negative | 79 (75.2) | 109 (54.5) | <0.0001§ |
| PgR positive | 26 (24.8) | 91 (45.5) | |
| OPN negative | 74 (68.5) | 29 (14.6) | <0.0001§ |
| OPN positive | 34 (31.5) | 169 (85.4) | |
| S100P negative | 82 (82) | 51 (28.3) | <0.0001§ |
| S100P positive | 18 (18) | 129 (71.7) | |
| S100A4 negative | 96 (87.3) | 96 (46.2) | <0.0001§ |
| S100A4 positive | 14 (12.7) | 112 (53.8) | |
| C-erbB-2 negative | 87 (80.6) | 155 (75.2) | 0.324 |
| C-erbB-2 positive | 21 (19.4) | 51 (24.8) | |
| C-erbB-3 negative | 58 (53.7) | 67 (33.3) | 0.001§ |
| C-erbB-3 positive | 50 (46.3) | 134 (66.7) | |
| pS2 negative | 76 (69.7) | 108 (52.4) | 0.004§ |
| pS2 positive | 33 (30.3) | 98 (47.6) | |
| p53 negative | 71 (65.1) | 122 (58.4) | 0.277 |
| p53 positive | 38 (34.9) | 87 (41.6) | |
| Cathepsin D negative | 18 (22.5) | 29 (17.2) | 0.386 |
| Cathepsin D positive | 62 (77.5) | 140 (82.8) | |
| pAGR2 negative | 74 (69.2) | 23 (11.3) | <0.0001§ |
| pAGR2 positive | 33 (30.8) | 180 (88.7) |
Lymph nodes with (positive) or without tumor deposits (negative); grade, histological grade III versus histological grades I and II; tumor size >5 cm versus <5 cm in diameter; immunocytochemical staining for molecular variables using 5% cut-off for positive versus negative staining class for OPN, ERα, PgR, S100P, S100A4, c-erbB-3, p53 and pS2, and using 1% cut-off for positive versus negative staining class for pAGR2 (using polyclonal antibody to AGR2), and for cathepsin D.
Number of patients with carcinomas either classified as staining (positive) or not staining (negative) for AGR2 using a mAb with a cut-off of 1% between positive and negative staining groups. Parentheses indicate the percentage of patients.
Probability between paired samples from Fisher’s Exact test, two sided.
Significant differences, P < 0.05.
Association between Staining for AGR2 and Patient Survival
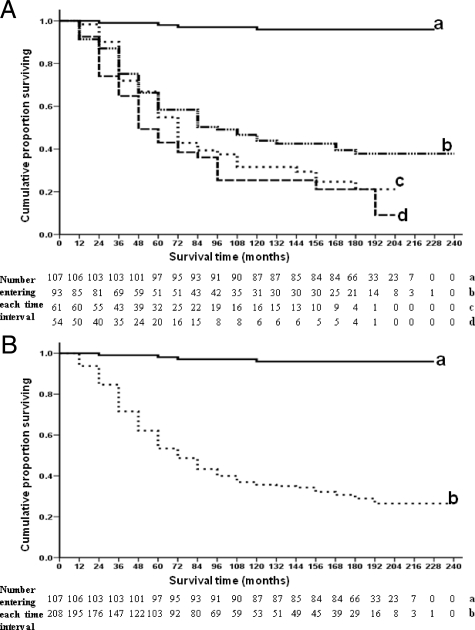
When the cumulative proportion of patients surviving at 12 monthly intervals after time of presentation were plotted for patients with primary tumors in each staining class for mAb to AGR2 (Figure 3A), the four curves showed a progressive decrease in survival and were highly significantly different overall (Wilcoxon test, P < 0.0001). Thus, there were 96, 38, 21, and 9% survivors with median survival times of >216, 87, 65, and 47 months for the AGR2 negative (−), borderline (±), intermediate (+), and moderate/strong (++/+++) staining classes, respectively. The difference between the negative (−) and borderline (±) class was highly significant (P < 0.0001), while that between the borderline (±) and intermediate (+) (P = 0.09) and between the intermediate (+) and moderate/strong staining classes (++/+++) (P = 0.25) were not significant (Figure 3A). Similarly using Cox’s univariate analysis, the relative risk (RR) between the negative (−) and the borderline (±) classes was much higher at 24 (95% CI, 9 to 66) than between the borderline (±) and intermediate (+) classes at 1.4 (95% CI, 0.9 to 2.1) and the intermediate (+) and moderate/strong (++/+++) classes at 1.3 (95% CI, 0.8 to 2.0). Thus the patients were separated into two distinct categorical groups, those with <1% staining and those with >1% carcinoma cells staining for AGR2 (ie, 1% cut-off). Of the 107 patients who were identified as being AGR2-negative, 96% were alive after 20 years compared with 26% of the 208 patients classified as AGR2 positive. The median survival time of patients classified as AGR2-negative was >216 months in comparison with 68 months for those classified as AGR2-positive. The data showed that over a period of 20 years, patients who possessed AGR2-positive carcinomas had a highly significantly poorer survival rate than those who had AGR2-negative carcinomas (Wilcoxon test, χ2 = 97.4, 1 d.f., P < 0.0001); significant differences were achieved after only 12 months of follow-up (χ2 = 6.88, 1 d.f., P = 0.009). Patients with AGR2-positive tumors had a RR of 30.5 (95% CI, 11.25–82.6) of dying. If the patients were separated into two groups using a 5% cut-off level, the difference in survival between the two groups was also significantly different (χ2 = 48.9, 1 d.f., P < 0.0001), but the RR was less at 3.95 (95% CI, 2.80–5.56). Similar significant differences (χ2 = 51.9, 1 d.f., P < 0.0001) were obtained if the same specimens were stained immunocytochemically with PAb to AGR2 using a 1% cut-off level between patients with positive and negative staining primary tumors, but the RR was smaller at 7.4 (95% CI, 4.1 to 13.5) (Table 4).
Figure 3.
Association of immunocytochemical staining by monoclonal antibody to AGR2 with overall survival of patients for different classes of immunocytochemical staining (A) and for using a cut-off of 1% between the two staining classes (B). A: The cumulative proportion of surviving patients as a fraction of the total for each year after presentation of patients with carcinoma cells classified as: a, −, completely negative staining (unbroken line; 100% = 107 patients); b, ±, borderline staining (broken line–dash dot dot dot dash; 100% = 93 patients); c, +, intermediate staining (dotted line; 100% = 61 patients); and d, ++/+++ moderate/strong staining (dashed line; 100% = 54 patients) for AGR2 is shown. There were 103 censored observations in a (19 dead of other causes); 39 in b (16 dead of other causes); 17 in c (10 dead of other causes); and 14 in d (13 dead of other causes). The cumulative proportions surviving ±1.96 SD to give ±95% CIs were (a) 0.97 ± 0.02, (b) 0.58 ± 0.05, (c) 0.43 ± 0.06, and (d) 0.39 ± 0.07 at 5 years; (a) 0.96 ± 0.02, (b) 0.42 ± 0.05, (c) 0.32 ± 0.06, and (d) 0.25 ± 0.07 at 10 years; (a) 0.96 ± 0.02, (b) 0.38 ± 0.05, (c) 0.21 ± 0.06, and (d) 0.09 ± 0.06 at 15 years; and (a) 0.96 ± 0.02, (b) 0.38 ± 0.05, (c) 0.21 ± 0.06, and (d) 0.0 ± 0.0 at 20 years. Overall, the four curves are highly significantly different (Wilcoxon statistic χ2 = 102.5, 3 d.f., P < 0.0001), and significantly different in the pairwise combination (a) with (b) (χ2 = 68.19, 1 d.f., P < 0.0001); but not (b) with (c) (χ2 = 1.081, 1 d.f., P = 0.094); or (c) with (d) (χ2 = 2.089, 1 d.f., P = 0.246). B: The cumulative proportion of surviving patients as a fraction of the total for each year after presentation for either a, patients with carcinomas classified as negatively staining (unbroken line) or b, positively staining (dotted line) for AGR2 is shown. For AGR2-negative carcinomas, 100% corresponds to 107 patients, and 100% for AGR2-positive carcinomas corresponds to 208 patients. There were 103 censored observations in a (19 dead of other causes) and 70 in b (39 dead of other causes). The cumulative proportions surviving ±1.96 SD to give ±95% CIs were (a) 0.97 ± 0.02 and (b) 0.49 ± 0.04 at 5 years; (a) 0.96 ± 0.02 and (b) 0.35 ± 0.03 at 10 years; (a) 0.96 ± 0.02 and (b) 0.26 ± 0.04 at 15 years; and (a) 0.96 ± 0.02 and (b) 0.26 ± 0.04 at 20 years. The two curves are highly significantly different (Wilcoxon statistic χ2 = 97.4, 1 d.f., P < 0001). In Cox’s univariate analysis RR = 30.5; 95% CI = 11.3 to 82.6.
Table 4.
Association of Tumor Variables with Patient Survival Times
| Tumor variable | Patient no.* | χ2† | P† | RR‡ | 95% CI‡ |
|---|---|---|---|---|---|
| Tumor size§ | 339 | 13.624 | 0.003 | 1.50 | 1.06–2.13 |
| Histological grade¶ | 311 | 12.85 | 0.002 | 1.59 | 1.12–2.26 |
| Nodal status∥ | 257 | 18.01 | <0.0001 | 2.00 | 1.39–2.88 |
| S100P** | 303 | 73.31 | <0.0001 | 7.34 | 4.69–11.51 |
| OPN** | 333 | 95.35 | <0.0001 | 21.5 | 9.49–48.9 |
| ERα** | 340 | 4.84 | 0.028 | 0.74 | 0.54–1.02 |
| C-erbB-2** | 344 | 10.03 | 0.002 | 1.69 | 1.19–2.40 |
| C-erbB-3** | 335 | 0.37 | 0.545 | 1.23 | 0.88–1.73 |
| S100A4** | 349 | 131.50 | <0.0001 | 8.75 | 6.01–12.7 |
| PgR** | 330 | 3.598 | 0.058 | 0.78 | 0.56–1.10 |
| p53** | 348 | 4.61 | 0.032 | 1.31 | 0.96–1.80 |
| pS2** | 344 | 0.955 | 0.329 | 1.25 | 0.91–1.72 |
| mAGR2†† | 315 | 97.40 | <0.0001 | 30.5 | 11.25–82.6 |
| pAGR2†† | 327 | 51.94 | <0.0001 | 7.43 | 4.11–13.5 |
| Cathepsin D†† | 270 | 2.818 | 0.093 | 1.39 | 0.84–2.29 |
Total number of patients in group, abbreviations: OPN, osteopontin; ERα, estrogen receptor α; PgR, progesterone receptor; m, monoclonal antibody; p, polyclonal antibody.
χ2 and probability (P) determined by generalised Wilcoxon Gehan statistics.
RR and 95% CI were determined using a Cox univariate analysis with 1 d.f. (Materials and Methods).
Tumor size T1 versus T2 versus T3 versus T4, P for 3 d.f. RR and 95% CI for tumor size <5 cm (T1, T2) versus tumor size >5 cm/attached to chest wall (T3, T4); RR for 1 step: T1 versus T2 = 1.45 (95% CI, 0.78–2.71), T1 versus T3 = 1.70 (95% CI, 0.85–3.39), T1 versus T4 = 3.91 (95% CI, 1.79–8.52), all 1 d.f.
Histological grade I versus II versus III, χ2 and P for 2 d.f. RR and 95% CI for grade I, II versus III; RR for 1 step: I versus II = 1.68 (95% CI, 1.08–2.61); I versus III = 2.26 (95% CI, 1.40–3.64), all for 1 d.f.
Nodal status: no nodes versus 1 or more nodes with tumor, χ2 and P for 1 d.f.
Negative versus positive staining using a 5% cut-off between the two groups; χ2 and P for 1 d.f.
Negative versus positive staining, using a 1% cut-off between the two groups; χ2 and P for 1 d.f.
Association of AGR2 and Other Tumor Variables with Patient Survival
In addition to that of AGR2, the association of patient survival times with the other tumor variables using generalized Wilcoxon Gehan statistics and Cox’s univariate analysis had been determined previously for the same group of patients (Table 4). Significant associations were seen between survival time of the patients, and the following tumor variables: tumor size (P = 0.003; RR = 1.50), histological grade (P = 0.002; RR = 1.59), nodal status (P < 0.0001; RR = 2.00), staining for OPN (P < 0.0001; RR = 21.5), S100A4 (P < 0.0001; RR = 8.75), S100P (P < 0.0001; RR = 7.34), c-erbB-2 (P = 0.002; RR = 1.69), ERα (P = 0.028; RR = 0.74), and p53 (P = 0.032; RR = 1.31). Staining for c-erbB-3, PgR, pS2 and cathepsin D did not show a significant association with patient survival time in this group of patients (Table 4). All tumor variables except staining for S100A4 had smaller values of the Wilcoxon statistic χ2 and hence higher P values than staining for AGR2. Most of the tumor variables have RR >1, but ERα and PgR had RR <1 (Table 4). To determine whether the significance of the relationship between mAb staining for AGR2 and patient survival time is independent of other tumor variables, Cox’s Multiple Regression analysis was performed using only those variables that showed a significant difference in univariate analysis alone. Of these tumor variables, staining for AGR2, S100P, c-erbB-2, S100A4, OPN, and p53 were all found to be significantly independently associated, with staining for AGR2 being the tumor variable to emerge with the highest RR of 9.46 (95% CI, 2.8 to 31.6) in terms of patient survival (Table 5). The pathological tumor variables tumor size (P = 0.058), histological grade (P = 0.16) and lymph node status (P = 0.10) were not significantly independently associated with patient survival, since they were eliminated from the final equation in the stepwise analysis (Supplemental Tables S1 to S6, see http://ajp.amjpathol.org).
Table 5.
Summary of Results for Cox’s Proportional Hazards Model for Cancer-Related Deaths
| Tumor variable* | β† | SE‡ | χ2§ | df¶ | P∥ | RR** | 95% CI** |
|---|---|---|---|---|---|---|---|
| AGR2 | 2.247 | 0.616 | 13.317 | 1 | 0.0001 | 9.463 | (2.83–31.639) |
| S100P | 1.070 | 0.324 | 10.887 | 1 | 0.001 | 2.916 | (1.544–5.507) |
| C-erbB-2 | 0.893 | 0.272 | 10.740 | 1 | 0.001 | 2.442 | (1.432–4.165) |
| S100A4 | 0.809 | 0.268 | 9.124 | 1 | 0.003 | 2.247 | (1.329–3.799) |
| OPN | 1.520 | 0.534 | 8.098 | 1 | 0.004 | 4.573 | (1.605–13.028) |
| p53 | 0.640 | 0.254 | 6.342 | 1 | 0.012 | 1.896 | (1.152–3.119) |
Tumor variable that showed a statistically significant association with patient survival times in the univariate analysis for 166 patient cases available with full data sets. Only comparison between patients with involved lymph nodes, all tumor sizes (T1–T4), all histological grades (I–III), staining for AGR2 (using AGR2 mAb), S100P, OPN, S100A4, ERα, c-erbB-2 and p53 were made. Analysis is shown in full in Supplemental Data (Supplemental Tables S1 to S6, see http://ajp.amjpathol.org).
Value of β parameter (=loge RR) in the Cox’s multiple regression analysis (Materials and Methods).
SE of β.
Cox’s statistic χ2.
Degree of freedom.
Probability from Cox’s statistic, χ2, 1 d.f. in each case. Overall, χ2 = 111.21, 6 d.f., P < 0.0001; residual χ2 = 14.29, 4 d.f., P = 0.006.
RR for survival and 95% CI from multivariate analysis.
Discussion
There have been two previous reports concerning the relationship of the immunocytochemical expression of AGR2 in primary breast cancer and patient outcome, one showing an association with longer18 and one with shorter17 survival times. The former patients received a mixture of adjuvant therapies including no therapy,18 whereas the latter ER-positive group received only adjuvant endocrine therapy.17 The purpose of the present study, therefore, has been to establish the level of specific expression of AGR2 in the primary carcinomas of 315 breast cancer patients who have undergone only surgical resection with no adjuvant therapy and to relate its expression to prognostic indicators and patient survival. The proportion of 66% of the primary tumors stained by the mAb to AGR2 using a 1% boundary of stained carcinoma cells to separate the positive from the negative staining carcinomas compares favorably with that of 68% found in this group of patients and with that of 65% found in an entirely independent group of adjuvant endocrine-treated patients17 using the PAb to AGR2. These proportions are smaller than the 87% reported by Fritzsche et al,18 using a PAb to an AGR2 peptide in a group of 155 breast cancer patients. Their assessment, however, is based on multiplication of the percentage of tumor cells staining by their intensity and therefore effectively counting any result above 0 as positive. Our reduced level of immunocytochemical staining is not an artifact of tissue preservation due to lack of accessibility of the antigen for the antibody or its specificity in immunocytochemistry or Western blots (Results). Moreover the observed interobserver and intratumor variability in immunocytochemical staining of the breast carcinomas with mAb to AGR2 is sufficiently small (8.8 and 5.0%, respectively) not to affect the reported results.
When the patients are grouped into four classes according to the percentage of cellular staining produced by mAb to AGR2, the class proportion of stained carcinoma cells is highly correlated with the time of death of the patients using either Wilcoxon statistics (Wilcoxon test χ2 = 102.5, 3 d.f., P < 0.0001) (Figure 3A) or log-rank sums (Mantel Cox χ2 = 119.9, 3 d.f., P < 0.0001). The graded response in patient death may suggest that the change in AGR2 is associated with its cause. Since the most significant difference occurs between the negative (−) and borderline (±) staining classes of tumors (Figure 3A), patients have been subsequently divided into two categorical staining groups at this boundary (Figure 3B). In this report, we show that the overall survival of patients with primary tumors expressing immunocytochemically detectable levels of AGR2 is highly significantly worse than for those patients with tumors classified as negative for AGR2 (Figure 3B). The degree of association using the Wilcoxon statistic (χ2 = 97.4, 1 d.f.) is more significant than almost all other tumor variables tested in this group of patients, except staining for S100A4 (χ2 = 131.5, 1 d.f.) (Table 4). When analyzed using log-rank sums, a similar high level of significant difference is obtained (Mantel Cox χ2 = 106.6, 1 d.f., P < 0.0001) and the median survival time of the positive group of 65 (95% CI, 48.8) months (data not shown) compares favorably with that of 68 months obtained using Wilcoxon statistics (Figure 3B). The significance of this association holds if the cut-off used to separate the positive and negative staining groups is set at 5% rather than 1% for the mAb and at 1% (Results) or 5% (χ2 = 46.5, 1 d.f., P < 0.0001) (data not shown) for the PAb to AGR2, thus demonstrating that this relationship is not dependent on the level of cut-off or type of antibody used. The fact that Fritzsche et al18 find positive PAb staining for AGR2 to be significantly associated with longer overall survival times (log-rank test, P = 0.035) may reflect the difference in the method of scoring, as outlined earlier and/or in patient treatment/follow-up times (median times, 75 versus 188 months). In the latter case, the fact that predominantly adjuvant-treated patients with AGR2-positive tumors started to show consistently shorter relapse times after the median time of follow-up of 75 months18 may suggest that, if followed up for longer periods of time, the survival curves may also crossover. The RR of death of patients with AGR2 mAb-positive tumors of 30.5 is the highest of all of the tumor variables measured and compares favorably with those of 21.5, 8.7, and 7.3 for the other metastasis-inducing proteins16,28,29 OPN, S100A4, and S100P, respectively. This RR is much greater than for conventional pathological tumor variables of tumor size, histological grade and lymph node status with RRs of 1.5 to 2.0, all of which are significant on their own (P ≤ 0.003) (Table 4). The analysis of histotype as a prognostic factor cannot be conducted with confidence because of the small percentage of tumors that are not invasive ductal carcinomas in this patient group (invasive lobular 6.1%, special type 1.5%).
When those tumor variables that have shown a significant correlation with time of survival in this group of breast cancer patients (Table 4)13,14,16,25 are tested for association with mAb staining for AGR2 in the primary carcinomas, staining for the hormone-related products ERα, PgR, and pS2 (Fisher’s Exact test, P ≤ 0.004) and involved lymph nodes (P = 0.04) are significantly correlated at both the 1 and 5% (data not shown) cut-off levels, in agreement with a previous report using a PAb to AGR2 peptides.18 However the most strongly correlated are staining for the metastasis-inducing proteins OPN,28 S100A4,29 and S100P.16 These strong correlations are maintained for cut-off levels of 1 or 5% using either the mAb or PAb (data not shown) to AGR2 (all P < 0.0001), demonstrating that they are not dependent on cut-off levels or source of antibody to AGR2. These results may suggest that the underlying change responsible for the overexpression of these four metastasis-inducing proteins is the same or similar. However, although the induction of the four metastasis-inducing proteins culminates in an apparently coordinated manner in the primary carcinomas, they all appear as significant independent prognostic indicators when assessed in Cox’s proportional hazards model in this group of patients. Staining for AGR2 is the most significantly associated with the highest RR of 9.5, followed by the other three metastasis-inducing proteins, then c-erbB-2 and p53 (Table 5). The standard pathological variables are confounded by combinations of more powerful independent molecular variables (Supplemental Tables S1 to S6, see http://ajp.amjpathol.org).
AGR2 is known to be a secreted adhesive protein.1,7,11 It is induced by estrogen in ERα expressing breast cancer cell lines,2,11 like OPN,30 consistent with its coordinated appearance with ERα, PgR, and pS2 in the human breast cancer specimens reported here, and its suppression in primary breast carcinomas after treatment of the corresponding patients with aromatase inhibitors.31 It can also be induced independently, in concert with OPN, by physiological stress, including oxygen deprivation.32 In cultured cells it can induce cell migration, anchorage independent growth and increase tumorigenicity in nude mice,33 and increase cell attachment and induce metastasis in syngenic rats11 without increasing rates of cell proliferation,11,33 in line with the other three metastasis-inducing proteins.29,28,16 The relatively coordinated overproduction of four proteins that can induce metastasis in a rat mammary model has now identified a new subgroup of breast cancer patients with a poor outcome. Since AGR2 is also secreted,11,33 and it can inhibit the p53 dependent response to DNA damage4 and its mRNA is found in circulating tumor cells,6 it is a good candidate for use as a prognostic test34 for likely patient outcome in breast and potentially other adenocarcinomas.4,5,8 Moreover, since the mAb used for staining for AGR2 has a higher discriminatory ability between those patients who survive and those who will die from metastatic disease, it may be more appropriate for this purpose than the PAb already published.17,18
Supplementary Material
Acknowledgments
We thank Christopher Holcombe and the Breast Unit, Royal Liverpool University Hospital for clinical assistance; Dr. Evelyn Williams and the staff of the NorthWest Intelligence Service (Liverpool Office) for providing patient outcome data; Joseph Carroll for excellent technical assistance; and Elizabeth Edgar, Lau Ngai Ka, and Grace Marsden for help in data collection.
Footnotes
Address reprint requests to Dong Liu Barraclough at the current address: Unit of Clinical Chemistry, School of Clinical Sciences, 4th Floor Duncan Building, Daulby Street, Liverpool, L69 3GA, UK., Phone: 44-151-7064258; Fax: 44-151-7065813; or Philip S. Rudland, School of Biological Sciences, Biosciences Building, University of Liverpool, Liverpool, L69 7ZB, UK. E-mail: dongliu@liverpool.ac.uk. and dell@liverpool.ac.uk.
Supported by Cancer and Polio Research Fund, North West Cancer Research Fund (grant CR758), Cancer Tissue Bank Research Centre, Genetic Innovation Network Development Award (grant GIN039), and North West Regional Development Agency through a National Biomanufacturing Centre (NBC) Access Fund grant (NBCAF002).
The monoclonal antibody to human AGR2 was affinity-purified from the patented hybridoma clone 7A10 (patent application number PCT/GB2007/003235) by three authors (R.B., D.L.B., and P.S.R.).
Supplemental material for this article can be found on http://ajp.amjpathol.org.
References
- Aberger F, Weidinger G, Grunz H, Richter K. Anterior specification of embryonic ectoderm: the role of the Xenopus cement gland-specific gene XAG-2. Mech Dev. 1998;72:115–130. doi: 10.1016/s0925-4773(98)00021-5. [DOI] [PubMed] [Google Scholar]
- Thompson DA, Weigel RJ. hAG-2, the human homologue of the Xenopus laevis cement gland gene XAG-2, is coexpressed with estrogen receptor in breast cancer cell lines. Biochem Biophys Res Commun. 1998;251:111–116. doi: 10.1006/bbrc.1998.9440. [DOI] [PubMed] [Google Scholar]
- Fletcher GC, Patel S, Tyson K, Adam PJ, Schenker M, Loader JA, Daviet L, Legrain P, Parekh R, Harris AL, Terrett JA. hAG-2 and hAG-3, human homologues of genes involved in differentiation, are associated with oestrogen receptor-positive breast tumours and interact with metastasis gene C4.4a and dystroglycan. Br J Cancer. 2003;88:579–585. doi: 10.1038/sj.bjc.6600740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohler E, Craig AL, Cotton J, Lawrie L, Dillon JF, Ross P, Kernohan N, Hupp TR. The Barrett’s antigen anterior gradient-2 silences the p53 transcriptional response to DNA damage. Mol Cell Proteomics. 2004;3:534–547. doi: 10.1074/mcp.M300089-MCP200. [DOI] [PubMed] [Google Scholar]
- Iacobuzio-Donahue CA, Maitra A, Olsen M, Lowe AW, van Heek NT, Rosty C, Walter K, Sato N, Parker A, Ashfaq R, Jaffee E, Ryu B, Jones J, Eshleman JR, Yeo CJ, Cameron JL, Kern SE, Hruban RH, Brown PO, Goggins M. Exploration of global gene expression patterns in pancreatic adenocarcinoma using cDNA microarrays. Am J Pathol. 2003;162:1151–1162. doi: 10.1016/S0002-9440(10)63911-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smirnov DA, Zweitzig DR, Foulk BW, Miller MC, Doyle GV, Pienta KJ, Meropol NJ, Weiner LM, Cohen SJ, Moreno JG, Connelly MC, Terstappen LW, O'Hara SM. Global gene expression profiling of circulating tumor cells. Cancer Res. 2005;65:4993–4997. doi: 10.1158/0008-5472.CAN-04-4330. [DOI] [PubMed] [Google Scholar]
- Zhang JS, Gong A, Cheville JC, Smith DI, Young CY. AGR2, an androgen-inducible secretory protein overexpressed in prostate cancer. Genes Chromosomes Cancer. 2005;43:249–259. doi: 10.1002/gcc.20188. [DOI] [PubMed] [Google Scholar]
- Kristiansen G, Pilarsky C, Wissmann C, Kaiser S, Bruemmendorf T, Roepcke S, Dahl E, Hinzmann B, Specht T, Pervan J, Stephan C, Loening S, Dietel M, Rosenthal A. Expression profiling of microdissected matched prostate cancer samples reveals CD166/MEMD and CD24 as new prognostic markers for patient survival. J Pathol. 2005;205:359–376. doi: 10.1002/path.1676. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Forootan SS, Liu D, Barraclough R, Foster CS, Rudland PS, Ke Y. Increased expression of anterior gradient-2 is significantly associated with poor survival of prostate cancer patients. Prostate Cancer Prostatic Diseases. 2007;10:293–300. doi: 10.1038/sj.pcan.4500960. [DOI] [PubMed] [Google Scholar]
- Fritzsche FR, Dahl E, Dankof A, Burkhardt M, Pahl S, Petersen I, Dietel M, Kristiansen G. Expression of AGR2 in non-small cell lung cancer. Histol Histopathol. 2007;22:703–708. doi: 10.14670/HH-22.703. [DOI] [PubMed] [Google Scholar]
- Liu D, Rudland PS, Sibson DR, Platt-Higgins A, Barraclough R. Human homologue of cement gland protein, a novel metastasis inducer associated with breast carcinomas. Cancer Res. 2005;65:3796–3805. doi: 10.1158/0008-5472.CAN-04-3823. [DOI] [PubMed] [Google Scholar]
- Dunnington DJ, Hughes CM, Monaghan P, Rudland PS. Phenotypic instability of rat mammary tumor epithelial cells. J Natl Cancer Inst. 1983;71:1227–1240. [PubMed] [Google Scholar]
- Rudland PS, Platt-Higgins A, Renshaw C, West CR, Winstanley JH, Robertson L, Barraclough R. Prognostic significance of the metastasis-inducing protein S100A4 (p9Ka) in human breast cancer. Cancer Res. 2000;60:1595–1603. [PubMed] [Google Scholar]
- Rudland PS, Platt-Higgins A, El-Tanani M, de Silva Rudland S, Barraclough R, Winstanley JH, Howitt R, West CR. Prognostic significance of the metastasis-associated protein osteopontin in human breast cancer. Cancer Res. 2002;62:3417–3427. [PubMed] [Google Scholar]
- de Silva Rudland S, Martin L, Roshanlall C, Winstanley J, Leinster S, Platt-Higgins A, Carroll J, West C, Barraclough R, Rudland P. Association of S100A4 and osteopontin with specific prognostic factors and survival of patients with minimally invasive breast cancer. Clin Cancer Res. 2006;12:1192–1200. doi: 10.1158/1078-0432.CCR-05-1580. [DOI] [PubMed] [Google Scholar]
- Wang G, Platt-Higgins A, Carroll J, de Silva Rudland S, Winstanley J, Barraclough R, Rudland PS. Induction of metastasis by S100P in a rat mammary model and its association with poor survival of breast cancer patients. Cancer Res. 2006;66:1199–1207. doi: 10.1158/0008-5472.CAN-05-2605. [DOI] [PubMed] [Google Scholar]
- Innes HE, Liu D, Barraclough R, Davies MP, O'Neill PA, Platt-Higgins A, de Silva Rudland S, Sibson DR, Rudland PS. Significance of the metastasis-inducing protein AGR2 for outcome in hormonally treated breast cancer patients. Br J Cancer. 2006;94:1057–1065. doi: 10.1038/sj.bjc.6603065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritzsche FR, Dahl E, Pahl S, Burkhardt M, Luo J, Mayordomo E, Gansukh T, Dankof A, Knuechel R, Denkert C, Winzer KJ, Dietel M, Kristiansen G. Prognostic relevance of AGR2 expression in breast cancer. Clin Cancer Res. 2006;12:1728–1734. doi: 10.1158/1078-0432.CCR-05-2057. [DOI] [PubMed] [Google Scholar]
- Winstanley J, Cooke T, Murray GD, Platt-Higgins A, George WD, Holt S, Myskov M, Spedding A, Barraclough BR, Rudland PS. The long-term prognostic significance of c-erbB-2 in primary breast cancer. Br J Cancer. 1991;63:447–450. doi: 10.1038/bjc.1991.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley JH, Leinster SJ, Cooke TG, Westley BR, Platt-Higgins AM, Rudland PS. Prognostic significance of cathepsin-D in patients with breast cancer. Br J Cancer. 1993;67:767–772. doi: 10.1038/bjc.1993.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warburton MJ, Mitchell D, Ormerod EJ, Rudland P. Distribution of myoepithelial cells and basement membrane proteins in the resting, pregnant, lactating, and involuting rat mammary gland. J Histochem Cytochem. 1982;30:667–676. doi: 10.1177/30.7.6179984. [DOI] [PubMed] [Google Scholar]
- Cuevas EC, Bateman AC, Wilkins BS, Johnson PA, Williams JH, Lee AH, Jones DB, Wright DH. Microwave antigen retrieval in immunocytochemistry: a study of 80 antibodies. J Clin Pathol. 1994;47:448–452. doi: 10.1136/jcp.47.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streefkerk J. Inhibition of erythrocyte pseudoperoxidase activity by treatment with hydrogen peroxide following methanol. J Histochem Cytochem. 1972;20:829. doi: 10.1177/20.10.829. [DOI] [PubMed] [Google Scholar]
- Hsu S, Raine L, Fanger H. Use of avidin-biotin-peroxidase complex (ABC) in immunoperoxidase techniques. J Histochem Cytochem. 1981;29:577. doi: 10.1177/29.4.6166661. [DOI] [PubMed] [Google Scholar]
- Platt-Higgins AM, Renshaw CA, West CR, Winstanley JH, de Silva Rudland S, Barraclough R, Rudland PS. Comparison of the metastasis-inducing protein S100A4 (p9ka) with other prognostic markers in human breast cancer. Int J Cancer. 2000;89:198–208. [PubMed] [Google Scholar]
- Altman DG. Practical statistics for medical research. Chapman & Hall,; 1991:pp. 403–405. Edited by London. [Google Scholar]
- Cox DR. Regression Models and Life-Tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- Oates AJ, Barraclough R, Rudland PS. The identification of osteopontin as a metastasis-related gene product in a rodent mammary tumour model. Oncogene. 1996;13:97–104. [PubMed] [Google Scholar]
- Davies BR, Davies MP, Gibbs FE, Barraclough R, Rudland PS. Induction of the metastatic phenotype by transfection of a benign rat mammary epithelial cell line with the gene for p9Ka, a rat calcium-binding protein, but not with the oncogene EJ-ras-1. Oncogene. 1993;8:999–1008. [PubMed] [Google Scholar]
- El-Tanani M, Barraclough R, Wilkinson MC, Rudland PS. Metastasis-inducing DNA regulates the expression of the osteopontin gene by binding the transcription factor Tcf-4. Cancer Res. 2001;61:5619–5629. doi: 10.1100/tsw.2002.238. [DOI] [PubMed] [Google Scholar]
- Mackay A, Urruticoechea A, Dixon JM, Dexter T, Fenwick K, Ashworth A, Drury S, Larionov A, Young O, White S, Miller WR, Evans DB, Dowsett M. Molecular response to aromatase inhibitor treatment in primary breast cancer. Breast Cancer Res. 2007;9:R37. doi: 10.1186/bcr1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweitzig DR, Smirnov DA, Connelly MC, Terstappen LW, O'Hara SM, Moran E. Physiological stress induces the metastasis marker AGR2 in breast cancer cells. Mol Cell Biochem. 2007;306:255–260. doi: 10.1007/s11010-007-9562-y. [DOI] [PubMed] [Google Scholar]
- Wang Z, Hao Y, Lowe AW. The adenocarcinoma-associated antigen. AGR2, promotes tumor growth, cell migration, and cellular transformation. Cancer Res. 2008;68:492–497. doi: 10.1158/0008-5472.CAN-07-2930. [DOI] [PubMed] [Google Scholar]
- Murray E, McKenna EO, Burch LR, Dillon J, Langridge-Smith P, Kolch W, Pitt A, Hupp TR. Microarray-formatted clinical biomarker assay development using peptide aptamers to anterior gradient-2. Biochemistry. 2007;46:13742–13751. doi: 10.1021/bi7008739. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.