Abstract
Objective
To compare vaginal repair augmented by mesh with traditional colporrhaphy for the treatment of pelvic organ prolapse.
Design
Prospective randomised controlled trial.
Setting
Tertiary teaching hospital.
Population
One hundred and thirty-nine women with stage ≥2 prolapse according to the pelvic organ prolapse quantification (POP-Q) system requiring both anterior and posterior compartment repair.
Methods
Subjects were randomised to anterior and posterior vaginal repair with mesh augmentation (mesh group, n= 69) or traditional anterior and posterior colporrhaphy (no mesh group, n= 70).
Main outcome measures
The primary outcome was the absence of POP-Q stage ≥2 prolapse at 12 months. Secondary outcomes were symptoms, quality-of-life outcomes and satisfaction with surgery. Complications were also reported.
Results
For subjects attending the 12-month review, success in the mesh group was 81.0% (51 of 63 subjects) compared with 65.6% (40/61) in the no mesh group and was not significantly different (P-value = 0.07). A high level of satisfaction with surgery and improvements in symptoms and quality-of-life data were observed at 12 months compared to baseline in both groups, but there was no significant difference in these outcomes between the two groups. Vaginal mesh exposure occurred in four women in the mesh group (5.6%). De novo dyspareunia was reported by five of 30 (16.7%) sexually active women in the mesh group and five of 33 (15.2%) in the no mesh group at 12 months.
Conclusion
In this study, vaginal surgery augmented by mesh did not result in significantly less recurrent prolapse than traditional colporrhaphy 12 months following surgery.
Keywords: Colporrhaphy, mesh, pelvic organ prolapse, randomised controlled trial
Introduction
In the United States, 200 000 women undergo surgery annually for pelvic organ prolapse.1,2 Combined anterior and posterior colporrhaphy was performed on 35.2% women undergoing prolapse surgery in 2003 and was the most common operation for this condition.2 A lifetime risk of 11.1% for surgery to treat pelvic organ prolapse or urinary incontinence or both was reported by a study from a United States health maintenance organisation.3 Within 4 years of the primary surgical procedure, further surgery for recurrent prolapse and/or incontinence was required in 29.2%.3
Dissatisfaction with traditional colporrhaphy for pelvic organ prolapse has resulted in increased use of mesh to augment vaginal repair procedures to obtain higher success rates. However, the use of mesh during vaginal repair procedures is controversial. Uncontrolled studies have reported significant problems (e.g. dyspareunia and mesh exposure) with the use of mesh during vaginal prolapse surgery.4,5 By contrast, there is wide acceptance of mesh use for prolapse with the abdominal sacral colpopexy procedure.6–8
This study was designed to evaluate whether vaginal surgery with mesh augmentation would reduce the rate of recurrent prolapse at 12 months when compared with traditional colporrhaphy. We also evaluated complications, symptoms, quality-of-life outcomes and patient satisfaction with surgery.
Methods
Women recommended vaginal surgery for anterior and posterior vaginal wall prolapse with stage 2 or more prolapse according to the pelvic-organ-prolapse quantification (POP-Q) system were invited to participate in this study.9 Women requiring only anterior or posterior compartment repair or with prolapse of the vaginal vault or cervix beyond the hymen or, in the opinion of the assessing surgeon, required abdominal prolapse surgery with mesh (e.g. open or laparoscopic sacral colpopexy) were excluded from the study. Women with contraindications for mesh usage, such as prior pelvic radiotherapy, pelvic sepsis, planned future pregnancy or immunocompromised were ineligible for the study. Institutional research and ethics committee approval for this study was obtained. All eligible women who agreed to participate in this study and provided written informed consent were enrolled between February 2003 and August 2005.
A sample size of 128 women (64 in each group) was required to achieve a significance level of 0.05 with a power of 0.8. This was based on the assumptions of 71% cure for traditional colporrhaphy and 93% for vaginal repair with mesh augmentation and a 15% loss to follow-up rate.3,10 Randomisation was computer generated and assignment was revealed prior to surgery. Subjects and surgeons were not blinded to the intervention.
Patients were assessed clinically and the prolapse staged using the POP-Q quantification system. Multichannel urodynamics was performed on subjects with urinary incontinence prior to surgery. All subjects completed validated questionnaires prior to surgery and at 6 and 12 months following surgery. The questionnaires were the Prolapse Symptom Inventory and Quality of Life questionnaire (PSI-QOL), Short-form Urogenital Distress inventory (SUDI), Short-form Incontinence Impact questionnaire (SIIQ) and Cleveland Clinic Continence score (CCCS).11–13 The subjects also completed a visual analogue scale (VAS; 0-100 where 100 represented being completely satisfied and 0 completely dissatisfied) of their satisfaction with surgery at 6 and 12 months following surgery.
The primary outcome was objective success of surgery as defined by the absence of POP-Q stage 2 or more prolapse (i.e. no prolapse at or below a point 1 cm above the hymen at any vaginal site) 12 months following surgery. Secondary outcomes were symptoms, quality-of-life outcomes and patient satisfaction with surgery at 6 and 12 months. Complications of surgery were also reported.
If a tension-free vaginal tape (TVT) or trans-obturator tape was required, this was undertaken at the start of surgery. A vaginal hysterectomy was then performed for women requiring this procedure. The vagina repair procedure was then performed. A perineal repair was performed as required.
Patients randomised to the no mesh group underwent standard anterior and posterior colporrhaphy. Plication of the pre-vesical and pre-rectal tissue with 2/0 polydioxanone sutures was performed. Excess vaginal epithelium was excised as required and closed with a continuous locking suture.
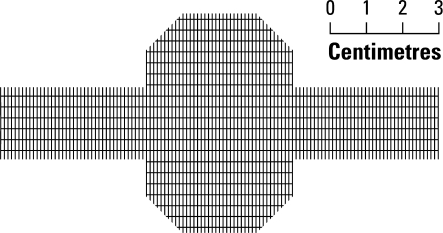
When mesh was used in the anterior vaginal repair, a full thickness midline epithelial incision was made. The vaginal epithelium was mobilised off the underlying pre-vesical tissue. Dissection continued towards each arcus tendineus fascae pelvis (ATFP). The inner aspect of the pubic bone was palpated at the level of the mid-vagina and lateral dissection was then continued through the ATFP with fine scissors using a ‘push-spread’ technique for approximately 3 cm. Only the central area of the pre-vesical fascia was repaired with 2/0 Monocryl (Ethicon, Somerville, NJ, USA). This avoided narrowing the pre-vesical space. The mesh (Gynemesh PS; Ethicon) was soaked in an antibiotic solution prior to placement and liberal wound irrigation with saline was performed during surgery. A cross-shaped piece of mesh was cut and placed over the pre-vesical tissue with the extension arms placed into each paravaginal space (Figure 1). The mesh extension arms abutted the inner aspect of the pubic bone on each side. Excess vaginal epithelium was trimmed as required and closed with a nonlocking continuous everting mattress suture.
Figure 1.
A cross-shaped mesh was used for the anterior vaginal repair. The extension arms were placed into each paravaginal space.
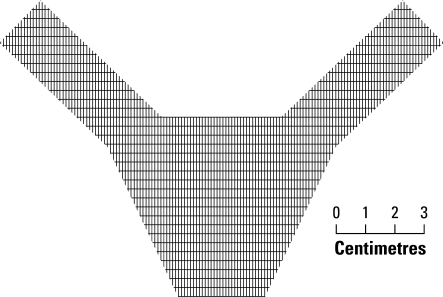
When mesh was used to reinforce the posterior vaginal repair, a full thickness midline epithelial incision was made. The vaginal epithelium was dissected off the underlying pre-rectal tissue. Dissection continued laterally on each side to the levator ani muscles. At the apex, dissection continued through the rectal pillars to each ischial spine and sacrospinous ligament. Only the central area of the pre-vesical fascia was repaired with 2/0 Monocryl. This prevented narrowing the pre-rectal space. A ‘Y’-shaped piece of mesh was cut and placed over the pre-rectal tissue with the extension arms placed in the tunnels created by the dissection onto the sacrospinous ligaments (Figure 2). The mesh extension arms abutted each sacrospinous ligament. Mesh was not placed in the lower third of the posterior vaginal wall. The vaginal epithelium was trimmed as required and closed with a nonlocking continuous everting mattress suture.
Figure 2.
A ‘Y’-shaped mesh was used for the posterior vaginal repair. The extensions arms abutted each sacrospinous ligament.
Sacrospinous ligament fixation of the vaginal vault or uterus as described by Carey and Slack was performed at the discretion of the surgeon.14 For seven subjects, laparoscopic suture sacral hysteropexy was performed as described by Krause et al.15
All patients received intra-operative antibiotics and thromboprophylaxsis. For subjects assigned to the mesh group, perioperative intravenous antibiotics were continued for 48 hours followed by oral antibiotics for a further 5 days.
Follow-up examination was performed at 6 and 12 months. During the examination, the examiner attempted to remain blinded to the surgical intervention received by each subject. Patient satisfaction using a visual analogue score (VAS) and validated symptom and quality-of-life questionnaires (Prolapse Symptom Inventory & QOL [PSI-QOL]) were administered at 6 and 12 months postoperatively.
Fisher’s exact test was used for discrete outcomes. Two-sample t-test was used for parametric continuous data.
Results
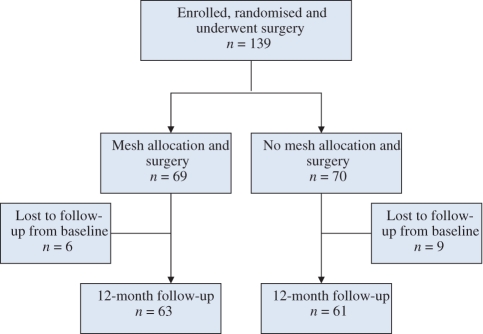
We recruited 139 women into the study (Figure 3). Departure from study protocol occurred in seven women with uterine prolapse who underwent laparoscopic suture sacral hysteropexy (two in the mesh and five in the no mesh group), two women who underwent a single compartment posterior repair (one in the mesh and one in the no mesh group) and one subject treated without mesh with a stage 4 uterine prolapse. In an attempt to replace these subjects, a further 11 women were recruited into the study in addition to the 128 planned recruits. All 139 women remained in the final analysis based on an intention-to-treat analysis. Therefore, for purposes of analysis, there were 69 women in the mesh group and 70 women in the no mesh group. There were no significant differences in demographics between the two groups (Table 1).
Figure 3.
Study flow chart.
Table 1.
Demographics and preoperative details for mesh and no mesh groups
| Variable | Mesh (n= 69) | No mesh (n= 70) | P-value |
|---|---|---|---|
| Age in years, mean (SD) | 59.1 (±11.4) | 57.6(±11.0) | 0.42* |
| Parity, mean (SD) | 3.24 (±1.59) | 3.42 (±1.62) | 0.51* |
| BMI (kg/m2), mean (SD) | 28.89 (±5.56) | 28.66 (±5.04) | 0.81* |
| No. subjects analysed1 | 63 | 61 | |
| Hormone therapy | 18.5% | 15.7% | 0.80** |
| No. subjects analysed1 | 54 | 51 | |
| Prior Prolapse Surgery | 13.6% | 26.2% | 0.08** |
| Prior Hysterectomy | 31.9% | 41.4% | 0.29** |
| No. subjects analysed1 | 22/69 | 29/70 | |
| Dyspareunia5 | 32.4% | 55.6% | 0.06** |
| Proportion1 | 11/35 | 20/34 |
Two sample t-test.
Fisher’s exact test.
Of the 139 women recruited, 108 (58 in the mesh group and 50 in the no mesh group) attended for the 6-month follow up and 124 (63 in the mesh group and 61 in the no mesh group) attended for the 12 month follow up. We chose to report the 12-month results for the primary and secondary outcomes.
A mid-urethral sling for stress incontinence was performed in 49% of the mesh group and 33% of the no mesh group. Twenty-seven percent of women in the mesh group and 28% in the no mesh group had a vaginal hysterectomy. Sacrospinous fixation was performed in 58% of the mesh group and 47% in the no mesh group.
The primary and secondary outcomes at 12 months are detailed in Table 2. For the primary outcome, we examined varying assumptions about data from women lost to follow up. Results are reported just for women returning for follow up (i.e. assuming that data were missing at random); assuming that women lost to follow up were treatment failures; and assuming that women lost to follow up were treatment successes.
Table 2.
Primary and secondary outcomes at 12 months following surgery
| Variable | Mesh (n= 69) | No mesh (n= 70) | P-value |
|---|---|---|---|
| Objective success (POP-Q stage 0 or 1)at 12 months of subjects returning forfollow up | 51/63 (81.0%) | 40/61 (65.6%) | 0.07* |
| Objective success (POP-Q stage 0 or 1)at 12 months assuming subjects lost tofollow up as failures | 51/69 (73.9%) | 40/70 (57.1%) | 0.049* |
| Objective success (POP-Q stage 0 or 1)at 12 months assuming subjects lost tofollow up as successes | 57/69 (82.6%) | 49/70 (70.0%) | 0.11* |
| PSI-QOL, mean change from preoperativeto 12 months score** (SD) | −6.93 (±8.25) | −7.77 (±7.43) | 0.58*** |
| No. subjects analysed | 55 | 53 | |
| SUDI, mean change from preoperativeto 12 months score** (SD) | −20.4 (±29.5) | −17.6 (±30.9) | 0.62*** |
| No. subjects analysed | 59 | 57 | |
| SIIQ, mean change from preoperative to12 months score** (SD) | −17.3 (±30.9) | −15.0 (±33.2) | 0.76*** |
| No. subjects analysed | 35 | 37 | |
| CCCS, mean change from preoperativeto 12 months score** (SD) | −1.00 (±4.20) | −0.75 (±4.30) | 0.78*** |
| No. subjects analysed | 50 | 44 | |
| Subjects reporting a VAS for satisfactionwith surgery of ≥80/100 | 45/59 (91.5%) | 51/63 (81.0%) | 0.12* |
| Awareness of prolapse | 3/61 (4.9%) | 7/62 (11.3%) | 0.32* |
Fisher’s exact test.
A negative change indicates a decrease in score over time and improved symptoms or impaired quality of life.
Two sample t-test for independent means.
Recurrent prolapse occurred most commonly in the anterior compartment. In the mesh group, no recurrence was more than point 0 and in the no mesh group, no recurrence was more than point +1 on POP-Q examination. Of those women with recurrences, one woman has undergone a laparoscopic sacral colpopexy and another has undergone a vaginal repair with mesh. Both subjects were from the no mesh group.
The results of PSI-QOL, SUDI, SIIQ and CCCS questionnaires are detailed in Table 2. For all four questionnaires, higher scores indicate worsening symptoms or impaired quality of life. The changes in scores for each scale from baseline to 12 months following surgery have been reported. Therefore, a positive change indicates an increase in score over time and a negative change indicates a decrease in score over time. For all scales, a negative change in score was observed from baseline to 12 month after surgery indicating improved symptoms or quality of life.
Intra-operative complications included one bladder perforation and one bowel perforation in the no mesh group. Both perforations were noted during the surgery and repaired intra-operatively without postoperative sequeale. One subject in the mesh group experienced significant intra-operative blood loss.
Postoperative complications included four cases (5.6%) of vaginal mesh exposure in the mesh group. Three mesh exposures were anterior and one was both anterior and posterior. Only one patient who developed a mesh exposure had a concomitant vaginal hysterectomy. Three of the mesh exposures presented at the 6-week postoperative review and one presented at 12 months. Three mesh exposures were treated surgically by simple excision of the exposed mesh and one case was managed conservatively. There was one tape exposure from a TVT procedure in the no mesh group.
Women were questioned regarding sexual activity and dyspareunia preoperatively and at 6 and 12 months. Eleven of 34 (32.4%) sexually active women in the mesh group and 20 of 36 (55.6%) in the no mesh group described preoperative dyspareunia. This difference was not significant (P=0.07). At the 6-month review, six of 25 (24.0%) in the mesh group and 11 of 27 (40.7%) in the no mesh group reported dyspareunia (P=0.25). At 12 months, 12 of 30 (40.0%) in the mesh group and 13 of 33 (39.4%) in the no mesh group reported dyspareunia (P=1). De novo dyspareunia was reported by five of 18 (27.8%) sexually active women without preoperative dyspareunia in the mesh group and five of 12 (41.7%) in the no mesh group at 12 months (P=0.46). Dyspareunia following surgery was considered to be because of vaginal stenosis in three women in the mesh group and five women in the no mesh group. Two women underwent vaginoplasty for vaginal stenosis and both were from the no mesh group.
Discussion
Our results failed to demonstrate that vaginal repair surgery augmented by mesh was significantly more successful in terms of reduced recurrent prolapse than traditional colporrhaphy 12 months following surgery. This finding was based on analysis of only those women who returned for the 12-month review. Alternative assumptions about missing data suggested a significantly higher success rate for the primary outcome measure for the mesh group when subjects not returning for review were assumed to be treatment failures.
While designing the study, we chose a relatively homogenous group of women requiring both anterior and posterior vaginal repair surgery with limited apical prolapse. This avoided the need for within group analysis and the problem of how to deal with women developing prolapse in the nonrepaired compartment.16 Departures from the study protocol were included in the final analysis on an intention-to-treat basis. However, the requirement for additional surgery for stress urinary incontinence and vaginal vault prolapse adds heterogeneity to the study population, and this together with protocol departures and missing data, undoubtedly effects the power of our study. Our failure to detect a difference between these procedures does not mean that such a difference could not exist.
Combined anterior and posterior colporrhaphy was chosen as the comparator as this is the most common procedure performed for prolapse in the USA.2 This operation was performed on 35.2% of 199 698 women undergoing prolapse surgery in the USA in 2003 compared to 17.0% of women undergoing anterior and 16.4% undergoing posterior colporrhaphy.2 Four randomised controlled studies have compared traditional colporrhaphy with vaginal repair with synthetic or biological graft augmentation with conflicting results. A recent study demonstrated that anterior colporrhaphy reinforced with mesh significantly reduced recurrent cystocele from 38.5 to 6.7% when compared with traditional anterior colporrhaphy.17 Another study reported that vaginal repair augmented by polyglactin 910 absorbable mesh significantly reduced recurrent cystocele from 43% in the no mesh group to 25% in the mesh group, but there was no difference in the rate of recurrent rectocele between the two groups.18 A further study demonstrated no significant difference in cystocele recurrence rates when three anterior repair techniques were compared, including one group with polyglactin 910 mesh reinforcement.19 Another study reported anterior colporrhaphy augmented by solvent dehydrated fascia lata did not reduce recurrent cystocele compared with traditional colporrhaphy.20 Two further studies have compared abdominal sacral colpopexy with transvaginal sacrospinous colpopexy.8,21 Both studies reported a trend towards the abdominal sacral colpopexy being associated with less recurrent prolapse and dyspareunia than sacrospinous colpopexy. Both studies have been widely interpreted as comparisons between abdominal and vaginal surgery for prolapse. However, in both studies, the subjects were randomised to prolapse surgery with mesh (abdominal sacral colpopexy) and without mesh (sacrospinous colpopexy) with less recurrent prolapse and dyspareunia reported in the mesh group.
The impact of surgery on sexual function is difficult to quantify. On direct questioning, the rates of dyspareunia were high in both groups preoperatively and at 6 and 12 months following surgery. These rates seemed to fluctuate with time. The high prevalence of dyspareunia is consistent with other studies.22,23 There was an improvement in sexual function according to the PSI-QOL questionnaire in both groups following surgery. Interestingly, some women who reported no sexual activity to the medical staff reported sexual dysfunction because of pelvic symptoms in the self-administered PSI-QOL questionnaire. This may reflect a reluctance to discuss these issues with the medical staff. We observed that de novo dyspareunia at 12 months following surgery was higher in the no mesh group compared with the mesh group. This may be explained by the different surgical techniques between traditional colporrhaphy and mesh-augmented repair. With colporrhaphy, the more lateral plication of the pre-vesical and pre-rectal tissues may result in reduced vaginal capacity compared with the mesh repair with plication of only the central pre-vesical and pre-rectal tissues.
The prevalence of vaginal mesh exposure (5.6%) in the mesh group is similar to rates reported for abdominal sacral colpopexy. A comprehensive review of abdominal sacral colpopexy by Nygaard et al. identified a 3.4% prevalence of mesh erosion.6 A more recent study of 313 women treated by abdominal sacral colpopexy reported a mesh erosion rate of 5.4%.24
Conclusion
Our study showed no significant reduction in recurrent prolapse 12 months following anterior and posterior vaginal repair with mesh augmentation compared with standard anterior and posterior colporrhaphy. Given our sample size and the number of patients failing to attend follow up, conclusions regarding the primary outcome were sensitive to assumptions made regarding those lost to follow up. A larger study is required to more conclusively assess the effectiveness and safety of mesh-augmented vaginal repair surgery.
Acknowledgments
This study was supported by a study grant from Ethicon, Somerville, NJ, USA. Data collection, data analysis and the writing up this study of were undertaken independent of Ethicon. The authors wish to thank Professor Ian Gordon for assistance with the statistical analysis.
Disclosure of interest
The first author, Dr Marcus Carey, has a consulting agreement with Ethicon, Somerville, NJ, USA. This consulting agreement involves the evaluation of new products. Included in the new products currently under evaluation is the PROSIMA® (Ethicon) procedure. Dr Carey receives payment for consulting. In the current study, Dr Carey’s competing interest has been managed by the study methodology (i.e. randomisation of subjects; multiple investigators and surgeons; and the intention of the reviewer to remain blinded to the intervention at review).
None of the other authors have competing interests to declare.
Details of ethics approval
Approval to conduct this study was obtained from the Royal Women’s Hospital Research and Ethics Committee on 18th June 2003 (project number: 02/03-The effectiveness of vaginal prolapse surgery employing mesh augmentation). This study was also registered with the Australian New Zealand Clinical Trials Registry (ANZCTR) on 10th October 2005 (ACTR number: ACTRN12605000621617). Website: http://www.anzctr.org.au.
Funding
This study was initiated independent of industry. Ethicon provided a study grant and product (GYNEMESH PS) towards this study. However, data collection, data analysis and writing up of the manuscript were performed independent of Ethicon.
References
- 1.Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol. 2003;188:108–15. doi: 10.1067/mob.2003.101. [DOI] [PubMed] [Google Scholar]
- 2.Shah AD, Kohli N, Rajan SS, Hoyte L. The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J. 2008;19:421–8. doi: 10.1007/s00192-007-0457-y. [DOI] [PubMed] [Google Scholar]
- 3.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 4.Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. BJOG. 2005;112:107–11. doi: 10.1111/j.1471-0528.2004.00332.x. [DOI] [PubMed] [Google Scholar]
- 5.Julian TM. The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol. 1996;186:1472–5. doi: 10.1016/s0002-9378(96)70092-3. [DOI] [PubMed] [Google Scholar]
- 6.Nygaard IE, McCreery R, Brubaker L, Connolly AM, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104:805–23. doi: 10.1097/01.AOG.0000139514.90897.07. [DOI] [PubMed] [Google Scholar]
- 7.Culligan PJ, Murphy M, Blackwell L, Hammons G, Graham C, Heit MH. Long-term success of abdominal sacral colpopexy using synthetic mesh. Am J Obstet Gynecol. 2002;187:1473–82. doi: 10.1067/mob.2002.129160. [DOI] [PubMed] [Google Scholar]
- 8.Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004;190:20–6. doi: 10.1016/j.ajog.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 9.Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 10.Goh JTW, Dwyer PL. Effectiveness and safety of polypropylene mesh in vaginal prolapse surgery. Int Urogynecol J. 2001;12(Suppl 3):S90. [Google Scholar]
- 11.Kobashi KC, Gormley EA, Govier F, Hadley R, Luber K, Nitti V, et al. Development of a validated quality of life instrument for patients with pelvic prolapse. Proceedings of the American Urological Association 95th Annual Meeting. J Urol. 2000;163:76. [Google Scholar]
- 12.Ubersax J, Wyman J, McClish D, Shumaker F, McKlish J, Santl J. Short forms to assess life-quality and symptoms distress for urinary incontinence in women: the Incontinence Impact Questionaire and the Uro-Genital Distress Inventory. Neurourol Urodyn. 1995;14:131–9. doi: 10.1002/nau.1930140206. [DOI] [PubMed] [Google Scholar]
- 13.Agachan F, Pfeifer J, Joo JS, Nogueras JJ, Weiss FG, Wexner SD. Results of perineal procedures for the treatment of rectal prolapse. Am Surg. 1997;63:9–12. [PubMed] [Google Scholar]
- 14.Carey MP, Slack MC. Transvaginal sacrospinous colpopexy for vault and marked uterovaginal prolapse. BJOG. 1994;101:536–40. doi: 10.1111/j.1471-0528.1994.tb13158.x. [DOI] [PubMed] [Google Scholar]
- 15.Krause HG, Goh JT, Sloane K, Higgs P, Carey MP. Laparoscopic sacral suture hysteropexy for uterine prolapse. Int Urogynecol J. 2006;17:378–81. doi: 10.1007/s00192-005-0019-0. [DOI] [PubMed] [Google Scholar]
- 16.Carey M, Slack M, Higgs P, Wynn-Williams M, Cornish A. Vaginal surgery for pelvic organ prolapse using mesh and a vaginal support device. BJOG. 2008;115:391–7. doi: 10.1111/j.1471-0528.2007.01606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hiltunen R, Nieminen K, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Am J Obstet Gynecol. 2007;110(Suppl 2):455–62. doi: 10.1097/01.AOG.0000261899.87638.0a. Part 2. [DOI] [PubMed] [Google Scholar]
- 18.Sand PK, Koduri S, Lobel RW, Winkler HA, Tomezsko J, Culligan PJ, et al. Prospective randomised trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstet Gynecol. 2001;184:1357–64. doi: 10.1067/mob.2001.115118. [DOI] [PubMed] [Google Scholar]
- 19.Weber AM, Walters MD, Piedmonte MR, Ballard LA. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185:1299–306. doi: 10.1067/mob.2001.119081. [DOI] [PubMed] [Google Scholar]
- 20.Gandhi S, Goldberg RP, Kwon C, Koduri S, Beaumont JL, Abramov Y, et al. A prospective randomized trial using solvent dehydrated fascia lata for the prevention of recurrent anterior vaginal wall prolapse. Am J Obstet Gynecol. 2005;192:1649–54. doi: 10.1016/j.ajog.2005.02.061. [DOI] [PubMed] [Google Scholar]
- 21.Benson JT, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomised study with long-term outcome evaluation. Am J Obstet Gynecol. 1996;175:1418–22. doi: 10.1016/s0002-9378(96)70084-4. [DOI] [PubMed] [Google Scholar]
- 22.Oskay UY, Beji NK, Yalcin O. A study of urogenital complaints of postmenopausal women aged 50 and over. Acta Obstet Gynecol Scand. 2005;84:72–8. doi: 10.1111/j.0001-6349.2005.00645.x. [DOI] [PubMed] [Google Scholar]
- 23.Gatt AE, Zinner SH, McCormick WM. The prevalence of dyspareunia. Obstet Gynecol. 1990;75:433–6. [PubMed] [Google Scholar]
- 24.Wu JM, Wells EC, Hundley AF, Connolly A, Williams KS, Visco AG. Mesh erosion in abdominal sacral colpopexy with and without concomitant hysterectomy. Am J Obstet Gynecol. 2006;194:1418–22. doi: 10.1016/j.ajog.2006.01.051. [DOI] [PubMed] [Google Scholar]