Abstract
Recent 16S ribosomal RNA gene (rRNA) molecular profiling of the stomach mucosa revealed a surprising complexity of microbiota. Helicobacter pylori infection and non-steroidal anti-inflammatory drug (NSAID) use are two main contributors to gastritis and peptic ulcer. However, little is known about the association between other members of the stomach microbiota and gastric diseases. In this study, cloning and sequencing of the 16S rRNA was used to profile the stomach microbiota from normal and gastritis patients. One hundred and thirty three phylotypes from eight bacterial phyla were identified. The stomach microbiota was found to be closely adhered to the mucosa. Eleven Streptococcus phylotypes were successfully cultivated from the biopsies. One to two genera represented a majority of clones within any of the identified phyla. We further developed two real-time quantitative PCR assays to quantify the relative abundance of the Firmicutes phylum and the Streptococcus genus. Significantly higher abundance of the Firmicutes phylum and the Streptococcus genus within the Firmicutes phylum was observed in patients with antral gastritis, compared with normal controls. This study suggests that the genus taxon level can largely represent much higher taxa such as the phylum. The clinical relevance and the mechanism underlying the altered microbiota composition in gastritis require further functional studies.
Introduction
Commensal microbiota is an integral part of a human being [1]. The vast majority of microbes inhabit our gastrointestinal tract, with more than 800 species from nine bacterial and one archaeal phyla. This diverse microbiota contributes to gut maturation [2], [3], [4], host nutrition and pathogen resistance [5]. Microbes also directly interact with human host by regulating intestinal epithelial proliferation, fat storage and inflammatory responses [3], [6], [7]. While some microbes can single-handedly cause serious illness, many chronic conditions are probably due to perturbations of the overall microbiota. For example, allergies and asthma are linked to childhood antibiotic use which may alter intestinal microbiota [8]. Other conditions associated with intestinal microbiota include late-onset autism [9], inflammatory bowel disease [10], and cancer [11].
Traditionally, cultivation-based methods are used to obtain microbial isolates for further characterization. Such studies provided the foundation of our understanding of microbiology. However, cultivation is often labor-intensive and can fail for many microbes. Microscopic observation is also used to estimate abundance of microbes, and to a limited extent, assigns microbes to taxa [12]. Recently, 16S ribosomal RNA gene (rRNA) sequence profiles are used to elucidate microbial diversity, often to the phylotype level. Using 16S rRNA sequencing, microbes from mouth [13], [14], esophagus [15], stomach [16], small intestine [17], colon [18], [19] and vagina [20] have been studied. These studies explored microbial diversity within the human body and revealed a vast population of uncultivated and uncharacterized microbes, which had been elusive for cultivation-based methods. Through these high-throughput 16S rRNA sequencing and other metagenomic sequencing efforts, microbiota perturbations were found to be associated with periodontal disease [21] and obesity [22], [23], [24].
In the stomach, gastric acidity kills many ingested microbes. It was generally considered that the stomach is not inhabitable by any microbe until the discovery of Helicobacter pylori and its association with gastritis and peptic ulcer [25]. Other than a few other Helicobacter species [26], [27], [28], it was not expected that the stomach would contain many other live microbes. Reduced acidity due to progressive atrophic gastritis may increase microbial diversity [29]. A study by Monstein et al. using temporal temperature gradient gel electrophoresis (TTGE) and a small-scale 16S rRNA sequencing suggested other microbes such as Enterococcus, Pseudomonas, Streptococcus, Staphylococcus and Stomatococcus were also present in the stomach [30]. A more recent large-scale 16S rRNA sequencing effort identified 128 phylotypes from 8 phyla in 23 North American patients [16]. Interestingly, the presence of H. pylori in the stomach did not affect the overall composition of the microbiota at the phylum level.
In this study, we went further to investigate potential associations between stomach microbiota changes and Non-H. pylori and non-NSAID (NHNN) gastritis. We hypothesized that when H. pylori is not present, other bacterial groups/species may contribute to or be associated with gastritis development. On the microbiota level, we also would like to address a key issue in the field: at what taxon depth(s) does the microbiota appear relatively stable such that perturbations at these levels may be relevant to human health? We used 16S rRNA gene cloning and sequencing to profile the stomach microbiota from normal and NHNN gastritis patients, and taxon-specific real-time quantitative PCR (qPCR) assays to quantify the relative abundance of the Firmicutes phylum and the Streptococcus genus.
Results
Taxon tree analysis
We analyzed both body and antrum biopsies from 5 normal individuals and 5 NHNN antral gastritis individuals (all females, age-matched). All patients were H. pylori negative by both rapid urease test and 16S rRNA sequencing. None of the patients had taken NSAID within 6 months prior to undergoing endoscopy. At least 60 clones from each biopsy (body or antrum, thus at least 120 clones from each individual) were sequenced using broad-range 16S rRNA PCR products. A total of 1223 non-H. pylori microbial sequences were obtained. These microbes belong to 8 phyla (133 phylotypes), of which 5 phyla (Firmicutes, Bacteroidetes, Actinobacteia, Fusobacteria and Proteobacteria) are present in a vast majority (1211 out of 1223, or 99.0%). Nine phylotypes with sequence similarity less than 97% to sequences present in the public databases were identified. Six of these 9 phylotypes were represented by single clones (Supplementary Table S1).
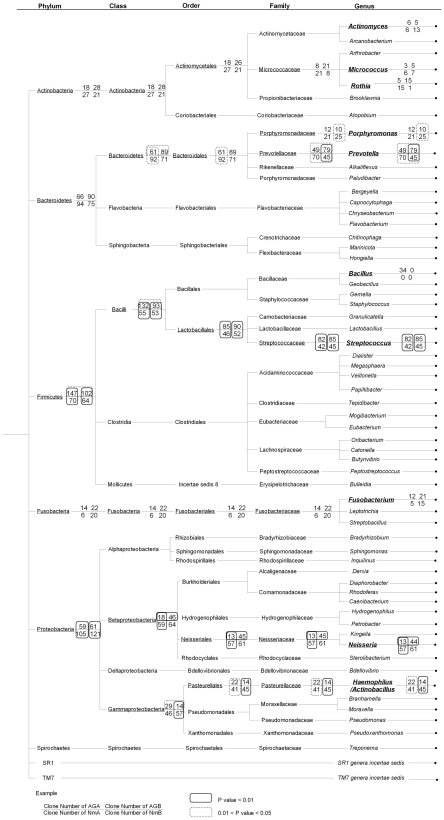
To investigate the overall representation of different taxon levels in the stomach biota, we constructed a taxon tree (Figure 1 and supplementary Figure S1). Interestingly, each phylum was dominated by only one or two lower taxon levels (class, order, family or genus). As a matter of fact, each phylum was dominated by only 1–2 genera. For example, the most abundant phylum Firmicutes was represented by 383 clones, of those 333 clones are from the class Bacilli. Subsequently, 273 clones were from the order Lactobacillales. Two hundred and fifty four clones were from the family Streptococcaceae. And all 254 clones were from the genus Streptococcus. The five most common genera including Streptococcus (254 clones), Prevotella (243), Neisseria (175), Haemophilus (122), Porphyromonas (68), constituted 70.5% of all microbial clones.
Figure 1. The taxon tree for the stomach microbiota.
The tree was created based on the RDPII classifier based on a naive Bayesian rRNA classifier. The clone numbers for the top 5 phyla, top 6 classes, top 6 orders, top 7 families and top 10 genera were shown. Each taxon with at least 10 clones in all four sample groups (AGA, AGB, NmA, NmB) was analyzed by Pearson's chi-square test by comparing the clones numbers between AGA and AGB, NmA and NmB, AGA and NmA, and AGB and NmB. The clone numbers for all phylotypes were shown in Supplementary Figure S1.
Species richness and diversity
When the entire dataset (1223 clones) was used, Good's coverage was 96%, indicating that four additional phylotypes would be expected for every 100 additional clones to be sequenced. This level of coverage indicated that majority of bacterial sequences were present in the sequenced clones. Diversity estimation by EstimateS version 8.0 indicated that about 200 phylotypes may be present in the human stomach biopsy samples (Supplementary Figure S2). We further estimated the species richness in four different biopsy samples (NmA (Normal Antrum), NmB (Normal Body), AGA (Antral Gastritis Antrum), AGB (Antral Gastritis Body); Supplementary Table S2). Species richness was not different between the antral gastritis biopsies and normal biopsies (p>0.1, unpaired t-test).
Bacterial microbiota comparison between two different anatomical locations (antrum and body) in normal patients
In the normal patients, no significant difference was observed between two anatomical locations (antrum and body) for any of the taxon groups, except for the family Prevotellaceae and the genus Prevotella where the p values (Pearson's chi-square test) were between 0.01 to 0.05 (Figure 1).
Firmicutes phylum and Streptococcus genus were enriched in the stomach of antral gastritis patients
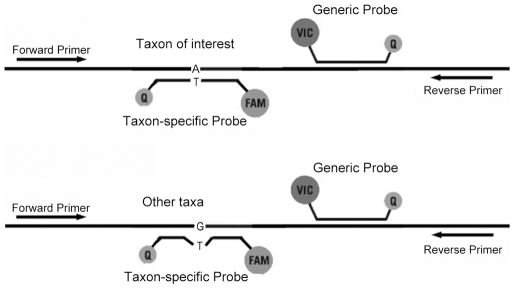
Based on the 1223 16S rRNA sequences, the Firmicutes phylum was the most abundant phylum with 383 clones. The Proteobacteria phylum was a close second with 345 clones. Interestingly, the Firmicutes phylum was more abundant in antral gastritis biopsies than in normal biopsies (41% vs. 22%, Table 1), while the Proteobacteria phylum was more abundant in normal biopsies (37% vs. 20%). Since 16S rRNA sequencing is cost prohibitive for a larger sample size, we developed a taxon-specific real-time quantitative PCR (qPCR) approach to quantify the abundance of Firmicutes and Streptococcus (Figure 2). The taxon-specific qPCR data for Firmicutes were highly correlated with the 16S rRNA sequencing data for the aforementioned 20 biopsy samples (2 biopsies for each of the 5 normal and 5 antral gastritis patients) (Supplementary Figure S3).
Table 1. Clone numbers and percentages for each bacteria phylum in the gastric biopsies from 5 pairs (antrum and body) of normal and 5 pairs of antral gastritis patients.
| Sample | Firmicutes | Proteobacteria | Bacteroidetes | Actinobacteria | Fusobacteria | Other | Total Clone # |
| normal | |||||||
| B07A | 13, 21%* | 10, 16% | 28, 45% | 8, 13% | 2, 3% | 1, 2% | 62 |
| B07B | 9, 15% | 17, 27% | 20, 32% | 15, 24% | 0, 0% | 1, 2% | 62 |
| B14A | 11, 18% | 9, 15% | 29, 48% | 10, 17% | 1, 2% | 0, 0% | 60 |
| B14B | 16, 26% | 15, 24% | 23, 37% | 2, 3% | 6, 10% | 0, 0% | 62 |
| B19A | 12, 19% | 16, 26% | 20, 32% | 9,15% | 1, 2% | 4, 6% | 62 |
| B19B | 14, 23% | 20, 33% | 17, 28% | 3, 5% | 4, 7% | 2, 3% | 60 |
| B33A | 16, 26% | 43, 70% | 1, 2% | 0, 0% | 1,2% | 0, 0% | 61 |
| B33B | 14, 23% | 34, 57% | 4, 7% | 1, 2% | 7, 12% | 0, 0% | 60 |
| B34A | 18, 29% | 27, 44% | 16, 26% | 0, 0% | 1, 2% | 0, 0% | 62 |
| B34B | 11, 18% | 34, 56% | 12, 20% | 0, 0% | 3, 5% | 1, 2% | 61 |
| Average | 22% | 37% | 28% | 8% | 4% | 1% | 100% |
| antral gastritis | |||||||
| B10A | 31, 52% | 6, 10% | 21, 35% | 2, 3% | 0, 0% | 0, 0% | 60 |
| B10B | 33, 54% | 2, 3% | 23, 38% | 2, 3% | 0, 0% | 1, 2% | 61 |
| B16A | 33, 54% | 7, 11% | 7, 11% | 7, 11% | 7, 11% | 0, 0% | 61 |
| B16B | 18, 29% | 8, 13% | 23, 37% | 7, 11% | 5, 8% | 1, 2% | 62 |
| B22A | 16, 26% | 16, 26% | 25, 40% | 0, 0% | 5, 8% | 0, 0% | 62 |
| B22B | 16, 25% | 16, 25% | 23, 37% | 1, 2% | 7, 11% | 0, 0% | 63 |
| B28A | 26, 43% | 17, 28% | 11, 18% | 5, 8% | 2, 3% | 0, 0% | 61 |
| B28B | 15, 25% | 17, 29% | 15, 25% | 9, 15% | 3, 5% | 0, 0% | 59 |
| B35A | 41, 68% | 13, 22% | 2, 3% | 4, 7% | 0, 0% | 0, 0% | 60 |
| B35B | 20, 32% | 18, 29% | 6, 10% | 9, 15% | 7, 11% | 2, 3% | 62 |
| Average | 41% | 20% | 25% | 8% | 6% | 1% | 100% |
Clone number, percentage.
Figure 2. Taxon-specific qPCR for quantifying abundance of a specific taxon within the stomach microbiota.
Two fluorescence probes (FAM and VIC) are located within the same PCR amplicon. The generic probe (VIC) targeting all bacteria sequences was used to quantify the total bacteria quantity. The taxon-specific probe (FAM) targeting to a specific taxon was used to quantify the quantity of the specific taxon. The taxon-specific probe matches perfectly to most species with the specific taxon, but has one or more mismatches to other species outside of the specific taxon. The ddCt value between VIC and FAM was used to quantify the abundance of the specific taxon.
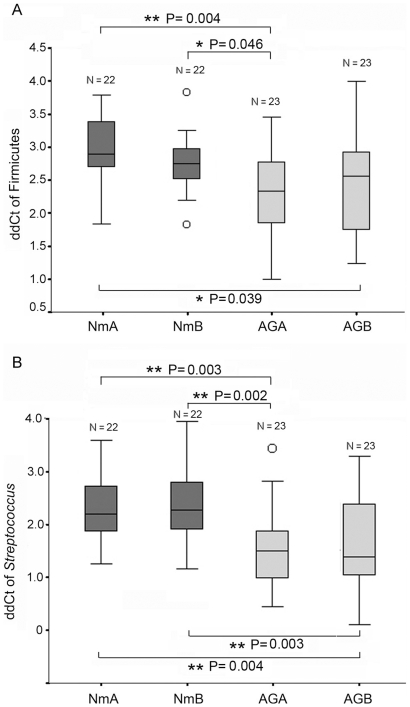
Seventeen additional pairs of antrum and body biopsy samples from normal patients and 18 additional pairs of antrum and body biopsy samples from antral gastritis patients were analyzed by Firmicutes-specific qPCR. Totally, 90 biopsies (46 samples from 23 antral gastritis patients and 44 samples from 22 normal patients) were analyzed (Table 2). The mean age of the antral gastritis patients was 67.6±11.4 (median: 69, range: 46 to 86), while the mean age of the controls was 58.3±14.7 (median: 52, range: 40 to 87). The mean age of the normal group was younger than that of the antral gastritis group. But statistical analysis showed that there was no correlation between age and Firmicutes or Streptococcus abundance (p>0.1) (Supplementary Figure S4). These samples were divided into 4 groups, antral gastritis antrum (AGA), antral gastritis body (AGB), normal antrum (NmA), and normal body (NmB). The abundance of Firmicutes was significantly higher in AGA than in NmA or NmB (One-way ANOVA (Analysis of Variance) test, p = 0.004 and p = 0.046, respectively) and in AGB than in NmA (one way ANOVA, p = 0.039) (Figure 3A). No significant difference was observed between AGA and AGB (one way ANOVA, p = 0.855), or NmA and NmB (p = 0.832).
Table 2. Patient demographics.
| NO. | Sex | Age | RUT | Disease Status | Gastric atrophy |
| P007 | F | 49 | -ve* | NA (endoscopically normal) | No |
| P012 | M | 47 | -ve | NA (endoscopically normal) | No |
| P014 | F | 78 | -ve | NA (endoscopically normal) | No |
| P019 | F | 57 | -ve | NA (endoscopically normal) | No |
| P033 | F | 74 | -ve | NA (endoscopically normal) | No |
| P034 | F | 68 | -ve | NA (endoscopically normal) | No |
| P039 | M | 56 | -ve | NA (endoscopically normal) | No |
| P050 | M | 51 | -ve | NA (endoscopically normal) | No |
| P059 | F | 67 | -ve | NA (endoscopically normal) | No |
| P065 | F | 46 | -ve | NA (endoscopically normal) | No |
| P073 | F | 40 | -ve | NA (endoscopically normal) | No |
| P081 | F | 42 | -ve | NA (endoscopically normal) | No |
| P086 | F | 50 | -ve | NA (endoscopically normal) | No |
| P087 | F | 47 | -ve | NA (endoscopically normal) | No |
| P091 | F | 52 | -ve | NA (endoscopically normal) | No |
| P105 | M | 82 | -ve | NA (endoscopically normal) | No |
| P106 | F | 46 | -ve | NA (endoscopically normal) | No |
| P302 | F | 81 | -ve | NA (endoscopically normal) | No |
| P305 | F | 42 | -ve | NA (endoscopically normal) | No |
| P338 | F | 68 | -ve | NA (endoscopically normal) | No |
| P383 | F | 87 | -ve | NA (endoscopically normal) | No |
| P453 | F | 52 | -ve | NA (endoscopically normal) | No |
| P010 | F | 72 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P016 | F | 86 | -ve | HP Neg mild chronic antral gastritis | No |
| P022 | F | 55 | -ve | endoscopically antral gastritis | No |
| P028 | F | 65 | -ve | HP Neg mild chronic antral gastritis | No |
| P035 | F | 78 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P040 | M | 78 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P045 | M | 75 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | Yes |
| P062 | F | 63 | -ve | HP Neg mild chronic antral gastritis | No |
| P067 | F | 72 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | Yes |
| P074 | F | 68 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P076 | F | 68 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P078 | M | 46 | -ve | endoscopically antral gastritis | No |
| P089 | F | 48 | -ve | HP Neg mild chronic antral gastritis | No |
| P100 | M | 69 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P103 | F | 72 | -ve | endoscopically antral gastritis | No |
| P109 | F | 71 | -ve | HP Neg mild chronic antral gastritis | No |
| P110 | M | 60 | -ve | endoscopically antral gastritis | No |
| P111 | F | 84 | -ve | HP Neg mild gastritis (endoscopically antral gastritis) | No |
| P114 | M | 60 | -ve | endoscopically antral gastritis | No |
| P301 | F | 74 | -ve | HP Neg mild chronic antral gastritis | No |
| P306 | F | 54 | -ve | HP Neg mild chronic antral gastritis | No |
| P451 | F | 52 | -ve | HP Neg mild chronic antral gastritis | No |
| P452 | M | 85 | -ve | HP Neg mild chronic antral gastritis | No |
RUT test negative.
Figure 3. Abundance of the Firmicutes phylum and the Streptoccous genus in different biopsies.
Delta delta Ct (ddCt) values (see text for details) were used to represent the abundance of the two taxa. A higher ddCt value represents a lower abundance of the taxon (abundance = 2−ddCt).
For the same biopsy samples, the genus Streptococcus was also analyzed by Streptococcus-specific qPCR. Streptococcus abundance was 72% and 76% higher in AGA vs. NmA or NmB, respectively, and 66% and 70% higher in AGB vs. NmA or NmB, respectively (Figure 3B). The p values for ANOVA test are shown in Figure 3B. Similar to the Firmicutes assay, no significant difference was observed between AGA and AGB (one way ANOVA, p = 0.999), or NmA and NmB (p = 0.999).
Streptococcus cultivation and biopsy washing
The mere detection of 16S rRNA gene sequences does not imply that live bacteria are present or the bacteria are indeed resident instead of passersby in the stomach. We thus carried out two additional experiments.
Firstly, we attempted bacteria cultivation from the biopsies. A culture condition suitable for Streptococcus was used since they appeared to be over-represented in antral gastritis patients. Sixteen pairs (antrum and body) of biopsies were used for culture on the blood agar plates. Colonies were sequenced for the 16S rRNA gene for identification. Eleven phylotypes of Streptococcus were isolated (Supplementary Table S3). These 11 phylotypes constituted 93.3% (or 237 out of the 254 clones) of all the clones identified in the broad-range 16S rRNA sequencing, indicating that majority of the Streptococcus phylotypes are alive in the gastric biopsies.
Secondly, 14 biopsy samples from both antral gastritis and normal patients were washed in phosphate buffered saline (PBS) with three increasingly harsh conditions. If harsh washing conditions do not remove the bacteria from the biopsy, it is suggestive that these bacteria attach closely to the stomach mucosa. Over 90% of the total bacteria remained attached to the biopsies after three consecutive washings with increasingly harsh conditions (Supplementary Figure S5A). The last washing step was done on high power on a desktop vortex machine. Similarly, majority of the Streptococcus bacteria remained attached to the biopsies after the 3 washing steps (Supplementary Figure S5B).
Discussion
In this study, we have profiled the bacterial microbiota in the paired gastric biopsies (antrum and body) from normal and antral gastritis patients. All patients are H. pylori negative and without NSAID use. Through broad-range 16S rRNA gene sequencing, we identified 1,223 non-H pylori bacteria clones, similar to a previous study (Bik study, 1,056 non-H pylori bacteria clones) [16]. Although the two studies analyzed two geographically (Hong Kong vs. California) and ethnically (Chinese vs. Caucasian, Hispanics and African American) divergent populations, the overall microbiota complexities are surprisingly similar (Table 3). Both studies identified approximately 130 (133 and 127 for this and the Bik study, respectively) phylotypes from seven to eight phyla. Majority of the clones (77.4% of this study and 79.8% of Bik study) were shared. The two most abundant genera (Streptococcus and Prevotella) were also identical. These two genera represented 40.6% and 41.5% of all clones in this study and the Bik study. Both studies indicated that approximately 200 different phylotypes may be present in the stomach mucosa. Such dramatic similarity between the two studies highlights the selective pressure for the microbiota under the harsh stomach environment. Additionally, we found little difference in bacterial microbiota between the two anatomical sites (antrum and body) in normal patients, despite of the clinical relevance for biopsy sampling at different anatomical sites [31].
Table 3. Comparison between this study and the Bik study.
| This study | Bik study | |
| Patients/Samples | 10/20 | 23/23 |
| Clone No. (non H. pylori ) | 1223 | 1056 |
| Phyla | 8 | 7 |
| Total Phylotypes | 133 | 127 |
| New Phylotypes | 9 | 13 |
| Phylotypes in both studies (clone number, percentage) | 59 (946, 77.4%) | 59 (843, 79.8%) |
| Study Specific Phylotypes (clone number, percentage) | 74 (277, 22.6%) | 68 (213, 20.2%) |
| Top 5 genera (clone number) | Streptococcus (254) | Streptococcus (299) |
| Prevotella (243) | Prevotella (139) | |
| Neisseria (175) | Rothia (95) | |
| Haemophilus (122) | Fusobacterium (45) | |
| Porphyromonas (68) | Veillonella (41) |
Given that rigorous washing steps were not able to separate the microbiota from the biopsies, we hypothesize that majority of the identified bacteria are associated tightly with the stomach mucosa. Additionally, we were able to cultivate majority of the Streptococcus phylotypes identified through broad-range 16S rRNA sequencing, suggesting that these bacteria may indeed be true residents in the stomach mucosa.
To further appreciate the overall complexity of stomach microbiota, we constructed a taxon tree based on the identified clones to look into each taxon level including phylum, class, order, family and genus. Interestingly, we found that for each phylum, one or two genera were predominantly present. The five most common genera including Streptococcus (phylum Firmicutes), Prevotella and Porphyromonas (Bacteroidetes), as well as Neisseria and Haemophilus (Proteobacteria), constituted 70.5% of all microbial clones.
Interestingly, the 16S rRNA profiling revealed a significant over-representation of the Firmicutes phylum (primarily due to the over-representation of the Streptococcus genus within the phylum) and an under-representation of the Proteobacteria phylum in the biopsies from antral gastritis patients. We developed a taxon-specific qPCR approach to analyze the abundance of the Firmicutes and streptococcus taxa for 90 biopsies (46 samples from 23 antral gastritis patients and 44 samples from 22 normal patients) and confirmed the over-representation of these two taxa in antral gastritis stomach by 42% and 71%, respectively. Most of the Streptococcus phylotypes identified by sequencing were alpha-hemolytic bacteria that are potential pathogens (e.g. Streptococcus pneumoniae, Streptococcus mitis and Streptococcus salivarius). Certain Streptococcus species are resistant to low pH conditions and may survive in the stomach [32]. Our cultivation data and washing experiment also suggested that these were indeed living, resident biota in the stomach.
Whether the increase in Streptococcus abundance is causative for antral gastritis or a result of local environmental change due to antral gastritis remained to be answered. One potential approach is using germ-free mouse model [33]. Another intriguing question is that whether certain microbiota compositions protect, or alternatively, sensitize the stomach mucosa from invading pathogens such as H. pylori. Lastly, new high throughput sequencing technologies are likely to provide more comprehensive data on microbiota from different anatomical locations along the human digestive tract and at different time points [34].
Materials and Methods
Gastric biopsy samples
This study was approved by the Chinese University of Hong Kong clinical research ethics committee. All patients gave written informed consent for obtaining the study specimens. Two gastric mucosal biopsies (antrum and body of the stomach) were collected from each patient during routine endoscopy at the Prince of Wales Hospital, Hong Kong. To avoid contamination, a new sterilized endoscopy forceps was used when taking a second biopsy from the same patient. The biopsies were snap-frozen on dry ice and stored at −80°C. Patients taking antibiotics or NSAIDs (defined as any use of NSAID for at least one week in the past 3 months prior to endoscopy) or tested positive for H. pylori by rapid urease test (RUT) or histological test were excluded. Patient demography is shown in Table 2.
Construction of 16S rRNA clone libraries and sequencing
Total genomic DNA was isolated from the biopsies by using the DNA mini kit (Qiagen, Valencia, CA, USA) with glass beat beater method as previously described [16]. Two negative controls with only sterile water were also extracted using the same protocol. The extracted DNA concentrations were measured by NanoDrop 1000 Spectrophotometer (Thermo Scientific, Minneapolis, MN, USA). Two universal bacterial 16S rRNA primers, B8F20 [35] (5′-AGAGTTTGATCCTGGCTCAG-3′) and B806R20 [36] (5′- GGACTACCAGGGTATCTAAT-3′) were used to amplify the region corresponding to position 8 to 806 of the Escherichia coli 16S rRNA gene. The 25 µL PCR mixtures included 1× PCR buffer including 1.5 mM MgCl2 (Qiagen), 20 mM tetramethylammonium chloride, 0.1 mM of each dNTP, 0.4 µM of each primer, 1 unit of HotStar Taq DNA polymerase (Qiagen), and 2 µL extracted DNA. A thirty-cycle PCR was performed to amplify the 799 bp fragment. The PCR products were checked by agarose gel electrophoresis. For each product, a single band could be observed under UV light, while no band was seen for the negative controls. The 16S rRNA products were purified with Sephadex G-50 column (Sigma-Aldrich, St. Louis, MO, USA), ligated with T vectors and transformed into E. coli JM109 cells by using the pGEM-T easy vector system (Promega, Madison, WI, USA). We selected 5 patients (10 biopsy samples) with antral gastritis and 5 normal controls (10 biopsy samples) to construct 20 16S rRNA gene libraries. For each gastric biopsy library, at least 60 colonies were selected for sequencing. The PCR products were sequenced by using BigDye terminator v3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA). The sequencing reactions using B8F20 as the sequencing primer were carried out on a ABI 3730xl sequencer (Applied Biosystems).
Phylogenetic analysis and microbial diversity estimation
The chimeric test using the Bellerophon server (http://foo.maths.uq.edu.au/~huber/bellerophon.pl) [37] was used to test potential chimeric sequences. One clone was found to be chimeric and subsequently excluded. Then, the 1223 nonchimeric sequences were analyzed by RDP II (Ribosomal Database Project II) classifier (http://rdp.cme.msu.edu/classifier/classifier.jsp) based on a naive Bayesian rRNA classifier [38]. Basic local alignment search tool (BLAST) provided by Green Genes (http://greengenes.lbl.gov/cgi-bin/nph-blast_interface.cgi) was performed to find the most similar sequences in the database. We used 97% sequence identity as the cutoff for defining phylotypes [39]. Sequences with identity <97% to the existing sequences in the database were considered novel. The taxon tree was constructed by using the classification result of the RPD II classifier. Chao1 estimator of the EstimateS 8 program (http://viceroy.eeb.uconn.edu/estimates) was used to estimate the microbial diversity. Good's method was used to calculate sequencing coverage [40].
Real-time quantitative PCR (qPCR)
Q-PCR primers and probes were designed based on the sequences obtained from the cloned libraries. We first aligned all cloned sequences by ClustalW (http://www.ebi.ac.uk/Tools/clustalw2/index.html) with the default parameters. The qPCR primers were B8F20 and B801R21 (5′- ACCAGGGTATCTAATCCTGTT-3′). The MGB probe sequences are: generic probe (VIC) 5′- CAGCAGCCGCGGTAA-3′, Firmicutes probe (FAM) 5′- AAGATTCCCTACTGCTGCCT-3′ and Streptococcus probe (FAM) 5′- TACACATGGAATTCCAC-3′. To measure the abundance of a specific taxon, two probes (one specific for the taxon of interest and the second generic for all bacteria) were used in the same PCR amplicon. (Figure 2). The 25 µL PCR mixture included 1× Buffer A, 3.5 mM MgCl2, 200 µM dNTP with dUTP instead of dTTP, 400 nM of each primer, 100 nM of each probe, 0.01 U/µL Uracil-N-Glycosylase, and 0.05 U/µL TaqGold (Applied Biosystems). For the Firmicutes-specific assay, the cycling condition was: 1) 50°C for 2 min; 2) 95°C for 10 min; 3) 40 cycles of 95°C for 20 sec, 58°C for 15 sec, 70°C for 80 sec. For the Streptococcus-specific assay, the cycling condition was: 1) 50°C for 2 min; 2) 95°C for 10 min; 3) 40 cycles of 95°C for 20 sec, 57°C for 1 min, 70°C for 1 min. The Streptococcus 16S rRNA fragment (DQ346438) cloned into the pGEM-T easy vector was used as the standard for qPCR (both for the Firmicutes and the Streptococcus assays) in the ABI 7500 real-time PCR system (Applied Biosystems). Due to some slight difference between the generic and taxon-specific probes, delta delta threshold cycle (ddCt) was used to indicate the abundance of the specific taxon in the entire bacteria population.
(CtTSU: Ct of taxon specific probe from unknown samples, CtBUU: Ct of bacterial universal probe from unknown samples, CtTSS: Ct of taxon specific probe from the plasmid standard, CtBSS: Ct of bacterial universal probe from the plasmid standard)
Theoretically, the abundance of a taxon is 2−ddCt.
Streptococcus Cultivation
We obtained 32 additional biopsies from 16 patients for bacterial culture. The biopsies were put in phosphate buffered saline (PBS, pH = 7.2) and cut to smaller pieces by a scalpel. The samples were then spread on blood agar plates (CM331, Oxoid, Basingstoke, UK) with 5% horse blood. The plates were placed in a 5% CO2 incubator at 37°C for 24 hours. The colonies with hemolysis on the blood agar were picked for 16S rRNA sequencing.
Biopsy washing
For biopsy washing test, 14 additional samples from both antral gastritis patients and normal people were collected. Each sample was placed in a 2.0 mL tube and washed 3 times (200 µL PBS for each washing) under increasingly harsh conditions. The first washing was done by gentle hand shaking. The supernatant was transferred out. New PBS was added to the biopsies for further washing. For the second and third washing, the tubes were vortexed by the tube mixer Trio TM-2F (All-lab scientific, AU) at grade 3 and grade 6 power level respectively, roughly corresponding to gentle and vigorous vortexing. Then duplex real-time PCR was performed to test the total bacteria and the Streptococcus quantities in the PBS supernatants from the three washing steps and the washed biopsies.
Statistics analysis
Pearson's chi-square test was used to compare the clone numbers of different taxa between different sample groups (NmA: normal antrum, NmB: normal body, AGA: antral gastritis antrum, AGB: antral gastritis body) from the 16S rRNA sequencing result, when the clone number for each sample group was at least 10. ANOVA test was used to compare the bacterial abundance data from qPCR assays. All analyses were performed using SPSS for windows, version 11.5 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant. For comparing the species richness between normal and antral gastritis patients, the actual phylotype number for each patient was counted first. Unpaired t-test was then used to compare the two patient groups.
Supporting Information
Detailed taxon tree
(2.00 MB TIF)
Species richness estimate
(0.97 MB TIF)
Correlation between qPCR and 16S rRNA cloning and sequencing
(0.98 MB TIF)
Lack of correlation between patient age and Firmicutes or Streptococcus abundance
(2.01 MB TIF)
Harsh washing does not remove the bacteria from the biopsies
(1.90 MB TIF)
Novel phyltoypes
(0.03 MB XLS)
Species richness estimate in different biopsy samples
(0.02 MB XLS)
(0.02 MB XLS)
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work is supported by the Chinese University of Hong Kong. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hooper LV, Gordon JI. Commensal host-bacterial relationships in the gut. Science. 2001;292:1115–1118. doi: 10.1126/science.1058709. [DOI] [PubMed] [Google Scholar]
- 2.Palmer C, Bik EM, Digiulio DB, Relman DA, Brown PO. Development of the Human Infant Intestinal Microbiota. PLoS Biol. 2007;5:e177. doi: 10.1371/journal.pbio.0050177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Backhed F, Ding H, Wang T, Hooper LV, Koh GY, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu J, Gordon JI. Inaugural Article: Honor thy symbionts. Proc Natl Acad Sci U S A. 2003;100:10452–10459. doi: 10.1073/pnas.1734063100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savage DC. Microbial ecology of the gastrointestinal tract. Annu Rev Microbiol. 1977;31:107–133. doi: 10.1146/annurev.mi.31.100177.000543. [DOI] [PubMed] [Google Scholar]
- 6.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Noverr MC, Huffnagle GB. Does the microbiota regulate immune responses outside the gut? Trends Microbiol. 2004;12:562–568. doi: 10.1016/j.tim.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Dethlefsen L, Eckburg PB, Bik EM, Relman DA. Assembly of the human intestinal microbiota. Trends Ecol Evol. 2006;21:517–523. doi: 10.1016/j.tree.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Finegold SM, Molitoris D, Song Y, Liu C, Vaisanen ML, et al. Gastrointestinal microflora studies in late-onset autism. Clin Infect Dis. 2002;35:S6–S16. doi: 10.1086/341914. [DOI] [PubMed] [Google Scholar]
- 10.Hume G, Radford-Smith GL. The pathogenesis of Crohn's disease in the 21st century. Pathology. 2002;34:561–567. [PubMed] [Google Scholar]
- 11.McGarr SE, Ridlon JM, Hylemon PB. Diet, anaerobic bacterial metabolism, and colon cancer: a review of the literature. J Clin Gastroenterol. 2005;39:98–109. [PubMed] [Google Scholar]
- 12.Moore WE, Holdeman LV. Human fecal flora: the normal flora of 20 Japanese-Hawaiians. Appl Microbiol. 1974;27:961–979. doi: 10.1128/am.27.5.961-979.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroes I, Lepp PW, Relman DA. Bacterial diversity within the human subgingival crevice. Proc Natl Acad Sci U S A. 1999;96:14547–14552. doi: 10.1073/pnas.96.25.14547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paster BJ, Boches SK, Galvin JL, Ericson RE, Lau CN, et al. Bacterial diversity in human subgingival plaque. J Bacteriol. 2001;183:3770–3783. doi: 10.1128/JB.183.12.3770-3783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pei Z, Bini EJ, Yang L, Zhou M, Francois F, et al. Bacterial biota in the human distal esophagus. Proc Natl Acad Sci U S A. 2004;101:4250–4255. doi: 10.1073/pnas.0306398101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bik EM, Eckburg PB, Gill SR, Nelson KE, Purdom EA, et al. Molecular analysis of the bacterial microbiota in the human stomach. Proc Natl Acad Sci U S A. 2006;103:732–737. doi: 10.1073/pnas.0506655103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayashi H, Takahashi R, Nishi T, Sakamoto M, Benno Y. Molecular analysis of jejunal, ileal, caecal and recto-sigmoidal human colonic microbiota using 16S rRNA gene libraries and terminal restriction fragment length polymorphism. J Med Microbiol. 2005;54:1093–1101. doi: 10.1099/jmm.0.45935-0. [DOI] [PubMed] [Google Scholar]
- 18.Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–1920. doi: 10.1126/science.1104816. [DOI] [PubMed] [Google Scholar]
- 19.Ley RE, Peterson DA, Gordon JI. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell. 2006;124:837–848. doi: 10.1016/j.cell.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 20.Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med. 2005;353:1899–1911. doi: 10.1056/NEJMoa043802. [DOI] [PubMed] [Google Scholar]
- 21.Lepp PW, Brinig MM, Ouverney CC, Palm K, Armitage GC, et al. Methanogenic Archaea and human periodontal disease. Proc Natl Acad Sci U S A. 2004;101:6176–6181. doi: 10.1073/pnas.0308766101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, et al. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 24.Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444:1022–1023. doi: 10.1038/4441022a. [DOI] [PubMed] [Google Scholar]
- 25.Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311–1315. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 26.Tiveljung A, Borch K, Jonasson J, Mardh S, Petersson F, et al. Identification of Helicobacter in gastric biopsies by PCR based on 16S rDNA sequences: a matter of little significance for the prediction of H. pylori-associated gastritis? J Med Microbiol. 1998;47:695–704. doi: 10.1099/00222615-47-8-695. [DOI] [PubMed] [Google Scholar]
- 27.Eckloff BW, Podzorski RP, Kline BC, Cockerill FR., 3rd A comparison of 16S ribosomal DNA sequences from five isolates of Helicobacter pylori. Int J Syst Bacteriol. 1994;44:320–323. doi: 10.1099/00207713-44-2-320. [DOI] [PubMed] [Google Scholar]
- 28.Andersen LP, Boye K, Blom J, Holck S, Norgaard A, et al. Characterization of a culturable “Gastrospirillum hominis” (Helicobacter heilmannii) strain isolated from human gastric mucosa. J Clin Microbiol. 1999;37:1069–1076. doi: 10.1128/jcm.37.4.1069-1076.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guerre J, Vedel G, Gaudric M, Paul G, Cornuau J. [Bacterial flora in gastric juice taken at endoscopy in 93 normal subjects]. Pathol Biol (Paris) 1986;34:57–60. [PubMed] [Google Scholar]
- 30.Monstein HJ, Tiveljung A, Kraft CH, Borch K, Jonasson J. Profiling of bacterial flora in gastric biopsies from patients with Helicobacter pylori-associated gastritis and histologically normal control individuals by temperature gradient gel electrophoresis and 16S rDNA sequence analysis. J Med Microbiol. 2000;49:817–822. doi: 10.1099/0022-1317-49-9-817. [DOI] [PubMed] [Google Scholar]
- 31.Kimura K. Gastritis and gastric cancer. Asia. Gastroenterol Clin North Am. 2000;29:609–621. doi: 10.1016/s0889-8553(05)70133-3. [DOI] [PubMed] [Google Scholar]
- 32.Quivey RG, Kuhnert WL, Hahn K. Genetics of acid adaptation in oral streptococci. Crit Rev Oral Biol Med. 2001;12:301–314. doi: 10.1177/10454411010120040201. [DOI] [PubMed] [Google Scholar]
- 33.Backhed F, Manchester JK, Semenkovich CF, Gordon JI. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A. 2007;104:979–984. doi: 10.1073/pnas.0605374104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6:e280. doi: 10.1371/journal.pbio.0060280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edwards U, Rogall T, Blocker H, Emde M, Bottger EC. Isolation and direct complete nucleotide determination of entire genes. Characterization of a gene coding for 16S ribosomal RNA. Nucleic Acids Res. 1989;17:7843–7853. doi: 10.1093/nar/17.19.7843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilson KH, Blitchington RB, Greene RC. Amplification of bacterial 16S ribosomal DNA with polymerase chain reaction. J Clin Microbiol. 1990;28:1942–1946. doi: 10.1128/jcm.28.9.1942-1946.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huber T, Faulkner G, Hugenholtz P. Bellerophon: a program to detect chimeric sequences in multiple sequence alignments. Bioinformatics. 2004;20:2317–2319. doi: 10.1093/bioinformatics/bth226. [DOI] [PubMed] [Google Scholar]
- 38.Wang Q, Garrity GM, Tiedje JM, Cole JR. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73:5261–5267. doi: 10.1128/AEM.00062-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stackebrandt E, Goebel BM. A Place for DNA-DNA Reassociation and 16s Ribosomal-Rna Sequence-Analysis in the Present Species Definition in Bacteriology. International Journal of Systematic Bacteriology. 1994;44:846–849. [Google Scholar]
- 40.Good IJ. The population frequencies of species and estimation of population parameters. Biometrika. 1953;40:237–264. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed taxon tree
(2.00 MB TIF)
Species richness estimate
(0.97 MB TIF)
Correlation between qPCR and 16S rRNA cloning and sequencing
(0.98 MB TIF)
Lack of correlation between patient age and Firmicutes or Streptococcus abundance
(2.01 MB TIF)
Harsh washing does not remove the bacteria from the biopsies
(1.90 MB TIF)
Novel phyltoypes
(0.03 MB XLS)
Species richness estimate in different biopsy samples
(0.02 MB XLS)
(0.02 MB XLS)