Abstract
Purpose
Geographic variation in risk factors may underlie geographic disparities in coronary heart disease (CHD) and stroke mortality.
Methods
Framingham CHD Risk Score (FCRS) and Stroke Risk Score (FSRS) were calculated for 25,770 stroke-free and 22,247 CHD-free participants from the REasons for Geographic And Racial Differences in Stroke cohort. Vital statistics provided age-adjusted CHD and stroke mortality rates. In an ecologic analysis, the age-adjusted, race-sex weighted, average state-level risk factor levels were compared to state-level mortality rates.
Results
There was no relationship between CHD and stroke mortality rates (r = 0.04; p = 0.78), but there was between CHD and stroke risk scores at the individual (r = 0.68; p < 0.0001) and state (r = 0.64, p < 0.0001) level. There was a stronger (p < 0.0001) association between state-level FCRS and state-level CHD mortality (r = 0.28, p = 0.18), than between FSRS and stroke mortality (r = 0.12, p = 0.56).
Conclusions
Weak associations between CHD and stroke mortality and strong associations between CHD and stroke risk scores suggest geographic variation in risk factors may not underlie geographic variations in stroke and CHD mortality. The relationship between risk factor scores and mortality was stronger for CHD than stroke.
Keywords: Stroke, Coronary Heart Disease, Geography, Risk Factors, Mortality
Introduction
There is substantial geographic variation in heart disease and stroke mortality, with higher stroke mortality in the Southeastern US (the “Stroke Belt”) [Lanska 1993; Howard 1995] and higher coronary heart disease (CHD) mortality along the Ohio-Mississippi River Basin (the “Coronary Valley”). [Pickle 1999] Of the numerous hypothesized reasons for these geographic variations in stroke and CHD mortality, [Howard 1999, Perry 1998], the most obvious are geographic variations in the contributing risk factors. While some have accepted this “risk factor hypothesis” as the cause for the geographic disparities in mortality, there are scant data examining this association.
Several publications have addressed the “risk factor hypothesis” of the geographic variation in stroke mortality using data from the National Health and Nutrition Examination Surveys (NHANES). NHANES was primarily designed to provide national estimates, but can also provide important information describing differences between regions. [Centers for Disease Control 2004] Some reports suggest that there may be a higher prevalence of hypertension, the most potent stroke risk factor, in the southeastern US for some race-sex strata [Obisean 2000; Hall 1997; Jones 1997], supporting the hypothesis that geographic variation in hypertension may contribute to the geographic variation in stroke mortality.
Under the “risk factor hypothesis,” states with a higher average cardiovascular risk factor profile should have a have higher cardiovascular disease mortality. Heart disease and stroke are diseases that share most, but not all, risk factors. Therefore, a significant correlation should exist between the average CHD and stroke risk factor burden across states, that should in turn should underlie a high correlation between CHD and stroke mortality.
In this paper we assess the “risk factor hypothesis” by: 1) describing the agreement between heart disease and stroke mortality at the state level, 2) examining the agreement between heart disease and stroke risk factor scores at the state level using data from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study, and 3) assessing the association of the geographic variation in state-level average risk factor scores and the geographic variation in state-level heart disease and stroke mortality rates.
Methods
State-level stroke (ICD-10 codes I60-I69) and ischemic heart disease (ICD codes I20-I25) age-adjusted (2000 US standard population) mortality rates for the population over age 45 for years 2003-2005 (inclusive) were calculated using the vital statistics assessed through the CDC Wonder System. [CDC 2007]
Risk factor data were from the REGARDS study, a national community-based longitudinal cohort study of 30,228 black and white individuals over age 45 years, recruited between January 2003 and October 2007. Twenty percent of the sample was selected from the “buckle” of the Stroke Belt (coastal plain region of NC, SC and GA), 30% from the Stroke Belt states (remainder of NC, SC, and GA, plus AL, MS, TN, AR, and LA), and the remaining 50% from the other 40 contiguous states. Participants were recruited using a combination of mail and telephone contact, and medical and risk factor history obtained by computer-assisted telephone interview. Physical measures were subsequently collected at an in-home examination including blood pressure, blood and urine samples, and electrocardiogram. Although not employed in the current report, participants were followed by telephone at six-month intervals for surveillance of incident stroke and coronary heart disease. Study methods were reviewed and approved by the Institutional Review Boards at the collaborating institutions. Additional methodological details are provided elsewhere. [Howard 2005]
As of March 2008, data were available on 30,198 study participants. The Framingham Stroke Risk Score (FSRS) [Wolf 1991; D’Agostino 1994] and the Framingham Coronary Heart Disease Risk Score (FCRS) [D’Agostino 2001; Wilson 1998] were calculated as summary indices of the risk factor profile for stroke and CHD respectively. The FSRS estimates the probability of stroke during the next 10-year period and is defined only for stroke-free individuals (not calculated for 1,920 participants self-reported stroke, and 101 participants who unsure of previous stroke). Of the remaining 27,982 participants, 2,212 (7.9%) were excluded as they had missing data on one or more of the factors included in the FSRS (see Table 1), providing FSRS scores for 25,770 participants. The FCRS, which estimates the 10-year risk of incident CHD, is defined only for CHD-free individuals (not calculated for 6,714 participants who have a history of CHD defined as self-reported myocardial infarction, or MI by ECG, or a previous coronary artery by-pass, or a previous coronary angioplasty or stent). Of the remaining 23,289 participants, an additional 1,042 (4.5%) were excluded as they had missing data on one or more of the FCRS components (see Table 1), providing FCRS scores for 22,247 participants. The relationship between the FCRS and the FSRS was calculated among 20,254 individuals for whom both scores could be calculated.
Table 1.
Components risk factors included in the calculation of the Framingham Risk Scores for stroke and coronary heart disease
| Risk factor | FSRSa | FCRSb |
|---|---|---|
| Age | X | X |
| Sex | X | X |
| Hx of heart disease | X | |
| Systolic blood pressure | X | X |
| Diastolic blood pressure | X | |
|
Use of anti-hypertensive medications |
X | |
| Diabetes | X | X |
| Current cigarette smoking | X | X |
| Atrial fibrillation | X | |
| Left ventricular hypertrophy | X | |
| Total cholesterol | X | |
| HDL cholesterol | X |
Framingham Stroke Risk Score - excludes individuals with history of stroke
Framingham Coronary Heart Disease Score - excludes individuals with history of CHD
The state-level stroke and CHD mortality rates are age adjusted, but reflect the distribution of race and sex represented in each state. Therefore, we calculated the average FSRS and FCRS adjusting for age and weighting the race-sex strata to achieve proportionate representation by race and sex for comparison to published mortality rates. Twenty-five states with at least 15 REGARDS participants in each race-sex group (black females - BF, black males -BM, white females - WF, and white males - WM) were included in the analysis. These select states had a total of at least 172 total REGARDS participants (see Table 2), a sample size that provides an estimated standard error of mean Framingham scores of 0.76. Linear regression was used to produce an age-adjusted average risk factor score for each race-sex stratum for each state (i.e., least squares means). Then the average FSRS and FCRS were calculated for each state as a weighted average of the four age-adjusted means for each race-sex stratum, where weights were proportional to the state population in each of the four race-sex strata.
Table 2.
REGARDS sample size for 25 states with at least 15 participants in each race-sex group, with a total sample size of 28,534 (includes both those with stroke and CHD, who were subsequently deleted in the calculations of the FCRS and FSRS)
| All | Black Females |
Black Males |
White Females |
White males |
|
|---|---|---|---|---|---|
| Alabama | 1639 | 505 | 287 | 463 | 384 |
| Arkansas | 794 | 158 | 89 | 261 | 286 |
| California | 2337 | 733 | 376 | 642 | 586 |
| Florida | 1060 | 225 | 181 | 305 | 349 |
| Georgia | 3038 | 838 | 498 | 931 | 771 |
| Illinois | 854 | 332 | 224 | 128 | 170 |
| Indiana | 325 | 80 | 62 | 91 | 92 |
| Kentucky | 229 | 44 | 31 | 72 | 82 |
| Louisiana | 2143 | 618 | 367 | 573 | 585 |
| Maryland | 619 | 183 | 167 | 98 | 171 |
| Massachusetts | 219 | 29 | 19 | 75 | 96 |
| Michigan | 1063 | 392 | 272 | 187 | 212 |
| Mississippi | 1216 | 319 | 190 | 341 | 366 |
| Missouri | 449 | 123 | 86 | 98 | 142 |
| New Jersey | 232 | 67 | 46 | 57 | 62 |
| New York | 891 | 312 | 197 | 181 | 201 |
| North Carolina | 3437 | 730 | 382 | 1250 | 1075 |
| Ohio | 1106 | 335 | 245 | 244 | 282 |
| Oklahoma | 172 | 40 | 24 | 47 | 61 |
| Pennsylvania | 624 | 179 | 108 | 150 | 187 |
| South Carolina | 3186 | 665 | 324 | 1217 | 980 |
| Tennessee | 1289 | 277 | 157 | 443 | 412 |
| Texas | 847 | 257 | 178 | 172 | 240 |
| Virginia | 430 | 95 | 84 | 105 | 146 |
| Wisconsin | 335 | 54 | 44 | 113 | 124 |
The result of these calculations were four measures, state-level measures of mortality for both CHD and stroke, and state-level, age adjusted, race-sex weighted measures of risk factor levels as assessed by the FSRS and FCRS. It is reasonable to assess the relationships between these four measures since, both for both mortality and average risk factor levels, the relative ranking of the states is remarkably stable over time. For example, despite changes from ICD-9 to ICD-10 coding, the Spearman correlation of state stroke mortality rates in 2003-2005 (used in this report) with rates a decade earlier (1993-1995) is 0.84 (p < 0.0001), and the correlation with rates two decades earlier (1983-1985) is 0.85 (0 < 0.0001). Likewise, the Spearman correlation of ischemic heart disease mortality rates in 2003-2005 (used in this report) with rates a decade earlier was 0.76 (p < 0.0001), and with rates two decades earlier was 0.49 (p = 0.0003). Hence, despite changes in ICD coding that could have a larger impact on heart disease rates than stroke, those states that with high rates in the current report have been consistent over time. Because risk factor prevalence is a product of life-time habits and exposures, the relative ranking for state-level risk factor profiles are unlikely to substantially change over time periods of moderate length (i.e., decades). For example, data from the Behavioral Risk Factor Surveillance System (BRFSS) suggests the correlation between states for the obesity in 1995 with obesity in 2007 is 0.77 (p < 0.0001). [CDC BRFSS Prevalence and Trends Data, 2009] Likewise, the correlation of between states in the proportion of smokers in 1995 compared to 2007 is 0.73 (p < 0.0001), and the proportion of self-reported diabetes is 0.47 (p = 0.0006). Another example of the substantial geographic stability of the risk factors is the persistence of the higher rates of hypertension in the southeastern stroke belt observed in NHANES between 1988 and 1991 [Hall 1997, Jones 1999], which was recently confirmed between 2003 to 2007 in the REGARDS population [Cushman 2008]. As the relationships between the states for both mortality and risk factors span decades, the overlap of the measures used in this paper are appropriate.
Results
There was little evidence of an association between the 2003-2005 mortality rates for CHD and stroke (r = 0.04, p = 0.78) for the 50 states (Figure 1a). Geographically close states tended to cluster with regard to CHD and stroke mortality. For example, New York ranked 1st for CHD mortality and 50th for stroke mortality, but also other Northeastern states had high CHD and low stroke mortality including Rhode Island, New Jersey, Delaware, New Hampshire, Pennsylvania, and Vermont. Many of the “stroke belt” states were high for both stroke mortality and CHD mortality including Tennessee, Mississippi, Arkansas, North Carolina, Kentucky, Missouri, Louisiana, South Carolina, Georgia, Alabama, and Virginia. Many of the Great Plain and Mountain states had moderate stroke mortality and low CHD mortality rate including Utah, Minnesota, Montana, Colorado, Nebraska, Wyoming, Idaho, Kansas, Wisconsin, Nevada, and North and South Dakota.
Figure 1.
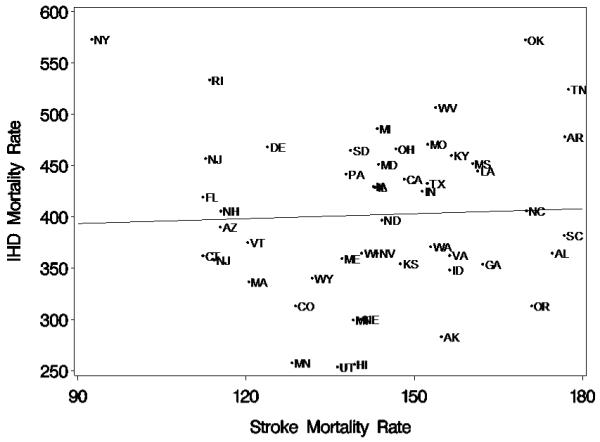
a: Relationship of age adjusted 2003-2005 stroke mortality rate and CHD mortality rate for ages 45+ for all 50 states (r = 0.04, p = 0.78)
There were 25 states with at least 15 REGARDS participants in each race-sex group (Table 2). These 25 states included 28,534 of the 30,193 (95%) REGARDS participants recruited at the time of this analysis. As shown in Figure 1b, there was also little evidence of an association of CHD and stroke mortality in these 25 states (r = -0.11; p = 0.61).
Figure 1.
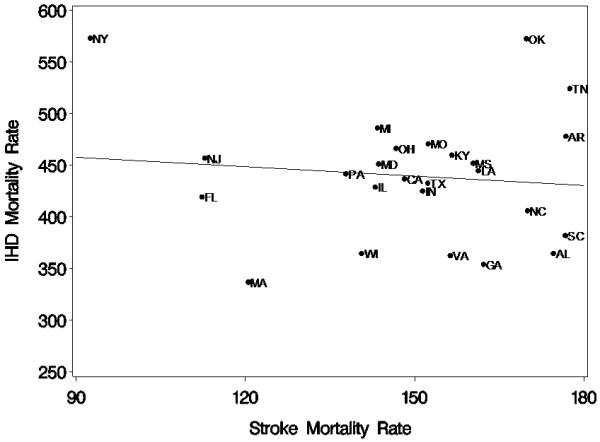
b: Relationship of age adjusted 2003-2005 stroke mortality rate and CHD mortality rate for ages 45+ for the 25 states included in the analysis (r = -0.11, p = 0.61).
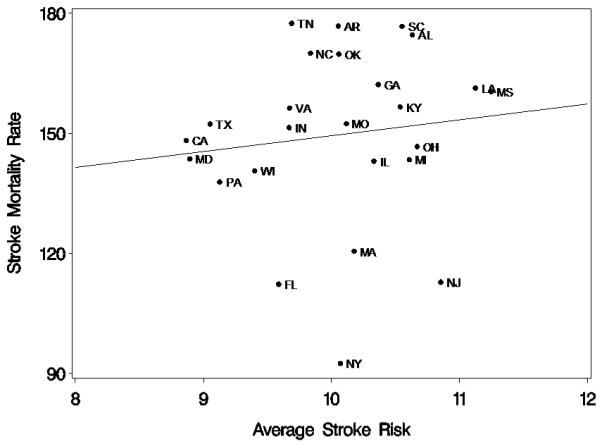
There was a substantial correlation of FCRS and the FSRS among REGARDS participants, where after normalization of distributions by taking the log of each score, the correlation of the two scores was 0.68 (p < 0.0001); hence, in general individuals at high risk for stroke were also at high risk of CHD. After age adjustment and race-sex weighting, the correlation between state-level average FCRS and FSRS was substantial (Figure 2; r = 0.64; p < 0.0001).
Figure 2.
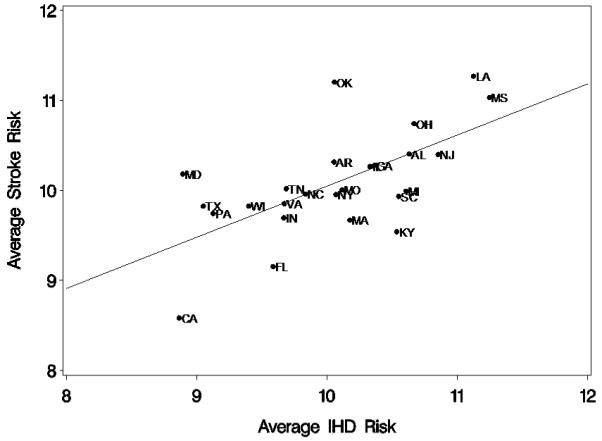
Relationship between average CHD and average stroke risk (r = 0.64, p < 0.0001)
The association between state-level age adjusted and race-sex weighted average risk scores and the state-level mortality rate for the 25 included states are shown for CHD in Figure 3a and for stroke in Figure 3b. For CHD, the correlation between state-level average FCRS and state-level mortality was moderate, but not statistically significant (r = 0.28; p = 0.18), while the association between the state-level average FSRS and the state-level stroke mortality was somewhat less (r = 0.12; p = 0.56). The difference between the correlation between CHD risk and mortality as compared to stroke risk and mortality was estimated by bootstrap methods (1000 replications) to be 0.142 ± 0.007, with 73% of replications having a larger correlation for CHD than for stroke, indicating the correlation between risk and mortality rates was significantly (p < 0.0001) larger for CHD than for stroke.
Figure 3.
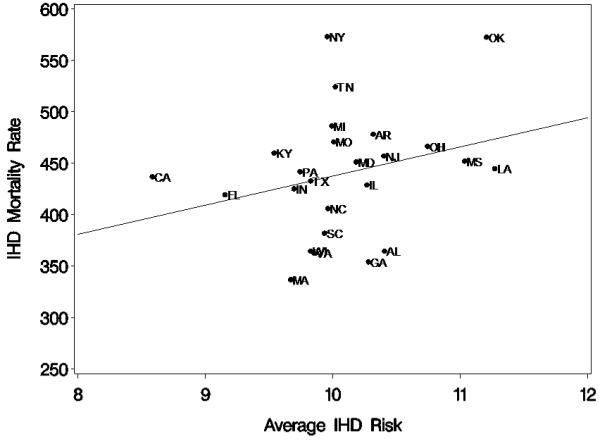
a: Relationship of average Framingham CHD Score and CHD mortality rate at the state level (r = 0.28; p = 0.18)
Figure 3.
b: Relationship of average Framingham Stroke Score and stroke mortality rate at the state level (r = 0.12, p = 0.56)
Discussion
These data suggest that it is likely that the “risk factor hypothesis” explains only a modest amount of the geographic variation in heart disease mortality, and a smaller portion of the geographic variation for stroke mortality. It is surprising that there was no association between the state-level CHD and stroke mortality rates, especially given the strong association between individual and state-level CHD and stroke risk factor levels. These findings suggest that it is unlikely that geographic variations in average level of risk factors are the primary contributor to geographic variation in both heart disease and stroke mortality.
We observed a moderate association between the state-level variation in CHD risk score and CHD mortality, but a weaker association between stroke risk score and stroke mortality. Hence, it seems more likely that geographic variation in traditional CHD risk factors underlie geographic variation in CHD mortality, and that geographic variation in traditional stroke risk factors play a smaller role in the geographic variation in stroke mortality.
There could be many alternative explanations for the lack of association between state-level stroke risk factor levels and stroke mortality; however, while a wealth of alternative hypotheses have been proposed (including differences in gene frequencies, novel risk factors, infection rates, socioeconomic status, lifestyle choices such as diet or exercise, case fatality rates, differential cause of mortality following an initial stroke or CHD event), [Howard 1999; Perry 1998] there is a dearth of data to assess these hypotheses. REGARDS is among the currently funded studies working to provide these data, and further insights are forthcoming.
There are several strengths and weaknesses of these analyses. REGARDS offers a large sample of community-dwelling residents over age 45, an age that places them at risk for stroke and heart disease. REGARDS has a sample size approximately three times larger than NHANES III for this age range. However, unlike NHANES, REGARDS includes only African American and white participants, so cannot assess questions for other race-ethnic strata. In addition, the Framingham Risk Scores (both CHD and stroke) were developed in largely white populations in the Northeast, and our analyses are based on the assumption that these risk functions are appropriate in African Americans and residents of other regions. As proposed by the Framingham study, the FSRS is calculated only for those individuals who are stroke free, while the FCRS is calculated only for those individuals who are free of CHD. It is possible that the stroke or CHD risk function with these individuals included could show a stronger relationship with mortality. Importantly, we are correlating the risk score data with the state-level mortality rates, and we cannot be sure that those individuals at high risk for CHD and stroke are the same individuals who die of CHD and stroke; that is, assuming causation in this ecologic analysis is problematic. NHANES also has clear advantages over REGARDS in the establishment of sample weights that allow more precise and unbiased estimates of the prevalence of risk factors at the national level. Finally, it is possible that the stronger relationship between CHD risk and mortality (as compared to the association between stroke risk and mortality) could be because of a potential higher predictive performance in the CHD risk assessment. We are unaware of any analyses that assess the relative predictive performance of these two indices.
Our current data suggest that differences in established risk factors are more likely to underlie the geographic variations in CHD mortality than stroke mortality. Lack of association between stroke and CHD mortality at the state level is surprising, particularly given the substantial observed association of stroke and CHD risk scores both in individuals and at the state level. This pattern supports the conclusion that it is unlikely that differences in risk factors underlie both the geographic variations in CHD and stroke mortality. There is a continuing need to assess alternative causes for geographic variation in stroke mortality.
Acknowledgments
The research reported in this article was supported by cooperative agreement NS 041588 from the National Institute of Neurological Disorders and Stroke
List of Abbreviations
- AL
Alabama
- AR
Arkansas
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
Coronary heart disease
- ECG
Electrocardiogram
- FCRS
Framingham coronary heart disease risk score
- FSRS
Framingham stroke risk score
- GA
Georgia
- LA
Louisiana
- MI
Myocardial Infarction
- MS
Mississippi
- NC
North Carolina
- NHANES
National Health and Nutrition Examination Surveys
- REGARDS
REasons for Geographic And Racial Differences in Stroke
- SC
South Carolina
- TIA
Transient ischemic attack
- TN
Tennessee
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Centers for Disease Control National Health and Nutrition Examination Survey (NHANES) 1999-2002. 2004 http://www.cdc.gov/nchs/nhanes.htm.
- Centers for Disease Control CDC BRFSS Prevalance and Trends Data. Source: http://apps.nccd.cdc.gov/BRFSS/index.asp. Retrieved February 2009.
- CDC Wonder System http://wonder.cdc.gov/mortSQL.html. Retrieved June 2008.
- Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, Temple EM, Howard VJ. Estimated 10-year stroke risk by region and race in the United States. Ann Neurol. 2008;64:507–513. doi: 10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25(1):40–43. doi: 10.1161/01.str.25.1.40. [DOI] [PubMed] [Google Scholar]
- D’Agostino S, Grundy S, Sullivan LM, Wilson P, for the CHD Risk Prediction Group Validation of the Framingham Coronary Heart Disease Prediction Scores: Results of a Multiple Ethnic Groups Investigation. JAMA. 2001;286(2):180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- Hall WD, Ferraro CM, Moore MA, Hall JE, Flack JM, Cooper W, Simmons JD, Egan BM, Lackland DT, Perry M, Jr., Roccella EJ. Hypertension-related morbidity and mortality in the Southeastern United States. Am J Med Sci. 1997;313:195–209. doi: 10.1097/00000441-199704000-00002. [DOI] [PubMed] [Google Scholar]
- Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, Burke GL. Is the stroke belt disappearing: an analysis of racial, temporal and age effects. Stroke. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- Howard G. Why do we Have a Stroke Belt in the Southeastern United States? A Review of Unlikely and Uninvestigated Potential Causes. Am J Med Sci. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- Howard VJ, Cushman M, Pulley LV, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic and Racial Differences in Stroke (REGARDS) Study: Objectives and Design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- Jones D, Basile J, Cushman W, Egan B, Ferrario C, Hill M, Lackland D, Mensah G, Moore M, Ofili E, Roccella EJ, Smith R, Taylor H. Managing hypertension in the Southeastern United States: Applying the guidelines from the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC VI) Am J Med Sci. 1999;318:357–364. [PubMed] [Google Scholar]
- Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939-1941 to 1979 to 1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- Obisesan TO, Vargas CM, Gillum RF. Region, urbanization, and hypertension in the Third National Health and Nutrition Examination Survey. Stroke. 2000;31:19–25. doi: 10.1161/01.str.31.1.19. Geographic variation in stroke risk in the United States. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health Community Initiatives to Eliminate Stroke Program, FY 2004-2007. http://www.omhrc.gov/templates/content.aspx?ID=3342, retrieved April 27, 2006.
- Perry HM, Roccella EJ. Conference report on stroke mortality in the Southeastern United States. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- Pickle LW, Gillum RF. Geographic variation in cardiovascular disease mortality in US blacks and whites. J Nat Med Ass. 1999;91:545–56. [PMC free article] [PubMed] [Google Scholar]
- Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22(3):312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]


