Summary
Before the era of highly active antiretroviral therapy, more than 40% of human immunodeficiency virus (HIV)-infected children experienced renal complications. In sub-Saharan Africa, approximately 2.1 million children are infected with HIV-1. In the absence of antiretroviral therapy, young African children frequently died of AIDS-related complications before renal diseases could be manifested or diagnosed. As antiretroviral therapy has become more available, and their survival has increased, our experience in treating kidney disease in HIV-infected children has improved. This article discusses relevant clinical and pathologic findings related to kidney disease in HIV-infected children.
Keywords: HIV-infected children, pediatric AIDS, childhood HIV-associated nephropathy, immune complex renal diseases, HIV-HUS, South Africa
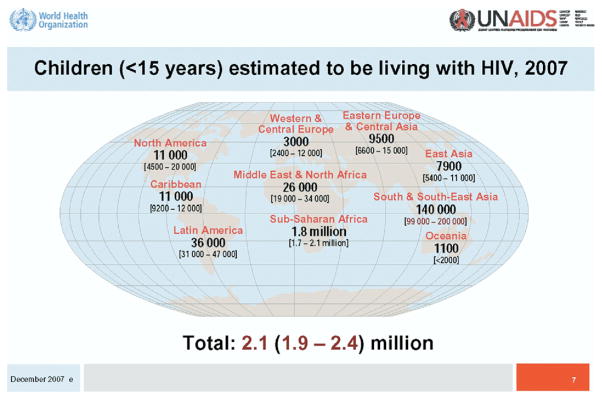
At the end of 2007 there were 33.2 million individuals infected with human immunodeficiency virus (HIV)-1, of whom approximately 2.1 million were children younger than 15 years of age.1 More than 85% of all HIV-infected children live in sub-Saharan Africa (Fig. 1). Considering new infections, unreported cases, and the increased survival of children receiving appropriate antiretroviral therapy (ART), this number probably will increase. In the absence of ART, approximately 40% of all HIV-infected children living in the United States experienced renal complications leading to poor growth, accelerated progression of acquired immune deficiency syndrome (AIDS), and/or premature death.2 In contrast, the presence of renal disease in HIV-infected African children not treated with ART is overshadowed by the high prevalence of diarrheal and respiratory diseases, including Pneumocystis jiroveci (previously known as Pneumocystis carinii) pneumonia.3–5 Without access to standard therapy, African children younger than 2 years of age frequently died from diarrhea-induced dehydration or respiratory infections, even before renal diseases could be manifested or diagnosed.4,5 As ART and other supportive treatments have become more available, the survival of African children has increased, and our knowledge and experience in treating childhood HIV-associated renal diseases has improved. This article discusses relevant clinical and pathologic renal findings in HIV-infected children, and compares the experience in children from South Africa and the United States.
Figure 1.
World Health Organization assessment of the number of children infected with HIV-1. Figure reprinted with permission from UNAIDS.1
HIV-INFECTED CHILDREN IN SOUTH AFRICA AND THE UNITED STATES
In mid-2006 there were approximately 300,000 children in South Africa with HIV infection, and more than 21,000 were receiving ART.1,4,5 The provision of ART for children varies throughout South Africa. Coverage of children in urgent need of therapy is highest in the Northern and Western Cape, approaching 60%. The Western Cape has an estimated 11,000 children; however, at the end of April 2008 there were only 3,898 children receiving ART.4,5 Currently 40% to 60% of all pediatric admissions to hospitals in South Africa may be HIV-related.4,5 The epidemiology and pathogenesis of HIV-associated renal diseases is not yet well documented among African children, but with the growing availability of ART, this information has become more important for appropriate management.
In contrast to African countries, the United States has a small percentage of the world’s children living with HIV/AIDS. At the end of the year 2005, the World Health Organization estimated that approximately 9,000 children younger than 15 years of age were living with HIV/AIDS in North America (Fig. 1). However, it should be acknowledged that for each pediatric AIDS case reported, there might be as many as 3 unreported cases.1,6 African American children represent approximately 65% of all HIV-infected children living with HIV/AIDS in the United States.6,7
HISTORY OF HIV-ASSOCIATED PEDIATRIC RENAL DISEASES IN THE UNITED STATES
The first cases describing an HIV-associated nephropathy (HIVAN) in African American children were reported by Strauss et al8,9 from Miami, and confirmed almost simultaneously in children from New York.10 These pediatric studies were published approximately 3 years after HIVAN was described in adult patients from New York and Miami.11,12 It should be noted, however, that the focal segmental glomerulosclerosis (FSGS) lesions described in the first adult cases of HIVAN were considered similar to the glomerular lesions seen in the setting of heroin use.11,12 What were considered unique features of HIVAN were the rapid progression of the disease and the combination of FSGS with tubular microcystic changes.11,12 The diagnosis of FSGS in young children with HIV infection provided key evidence to support the notion that HIV-1 was capable of inducing renal disease independent of drug use.8–10
During the early years of the AIDS epidemic, American children frequently died of nonrenal AIDS-related complications.2,7–10 Autopsy reports frequently described and attributed renal tubular-interstitial lesions to acute tubular necrosis. Subsequently, with the recognition of the renal histology of HIVAN, this renal disease was identified in perinatally infected children at 2 to 3 years of age.2,7–10 Although the presence of renal disease contributed to poor quality of life and premature death, these children usually died before they developed end-stage renal disease (ESRD).2,7–10,13 Since the widespread establishment of ART in 1996, the clinical outcome of HIV-infected children in the United States has improved dramatically.7–10,14 HIVAN is diagnosed at an older age, and the pool of HIV-infected children surviving and requiring dialysis or transplantation has increased considerably.7,14,15 It is anticipated that as ART becomes available to more children in resource-limited settings, a similar epidemiologic and clinical pattern will be seen in Africa.
CLINICAL FEATURES OF HIV-ASSOCIATED PEDIATRIC RENAL DISEASES
Children with HIV disease may present with renal manifestations, which can be exacerbations of common renal conditions or may be specific to HIV-1 viral activity in the kidney.
Urinary Tract Infections
Urinary tract infections may be diagnosed with increased frequency in children with HIV, but this often reflects difficulties in collecting a representative urine sample that is not contaminated in the face of diarrheal disease (the most common presentation of HIV infection in many infants) or severe napkin dermatitis. Severe urinary tract infections and pyelonephritis were seen in 23% of a group of 60 children with HIV and renal involvement studied in Johannesburg, South Africa.4
Acute Renal Failure and HIV-Associated Hemolytic Uremic Syndrome
Acute renal failure caused by dehydration remains a problem, especially in infants, requiring rehydration by oral, nasogastric, or intravenous routes. Intravenous fluids may not be easily available in some resource-poor areas.
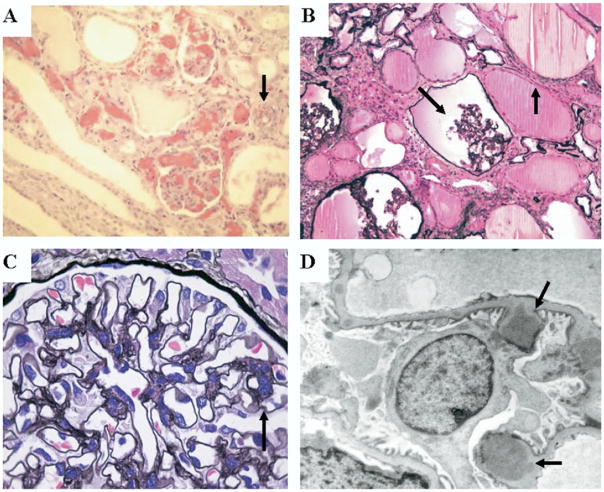
HIV-infected children also can develop an atypical, fatal form of hemolytic uremic syndrome (HUS) defined by the presence of microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure.2,13 Unlike the classic form of Shiga-toxin–induced HUS, HIV-HUS is characterized by an insidious clinical onset, preserved urine output, and the absence of preceding diarrhea. Rapid progression to ESRD or death from infectious or bleeding complications is common.2,13 The presence of thrombotic microangiopathic (TMA) glomerular lesions is characterized by the accumulation of fibrin and often is associated with microcystic tubular changes (Fig. 2A). The pathogenesis of childhood HIV-HUS is not clearly understood. It appears that HIV-HUS is triggered by infectious agents that induce endothelial injury leading to the development of renal TMA lesions.2,13 The presence of proteinuria and high viral load in HIV-infected children are risk factors for the development of HIV-HUS.2,13 Alternatively, some HIV-infected children may develop renal TMA lesions without clinical symptoms of HUS,2,8 but the prevalence of asymptomatic TMA lesions in HIV-infected children is unknown. In South Africa, HIV-HUS typically is seen in children younger than 2 years of age, who usually present in critical condition, often too sick to undergo renal biopsy, but with the classic clinical symptoms of HUS. These children are treated with supportive therapy and peritoneal dialysis, but often die from overwhelming sepsis without the growth of any specific organism. Because of the high mortality rates associated with HIV-HUS, it is necessary to be aware of this syndrome, and to make an early diagnosis to prevent its fatal complications.2,13
Figure 2.
Representative photomicrographs of renal sections from children with HIV-HUS, HIVAN, and HIVICK. (A) Light microscopy renal section from a child with HIV-HUS showing collapsed glomerular capillary loops with red blood cell fragments and tubular microcysts. The black arrow shows an arteriole with luminal narrowing owing to red cell fragments and intramural thrombosis (hematoxylin-eosin stain, 200×). (B) Light microscopy renal section from a child with HIVAN. The black arrows show a shrunken glomerulus and microcystic tubular dilatation (Jones methenamine silver stain, 200×). Figure 2B courtesy of Dr. William Bates and Dr. Peter Nourse. (C) Light microscopy renal section from a child with HIVICK showing mesangial prominence. The glomerular tuft is lobulated with double contours of the glomerular basement membrane (black arrow) (Jones methenamine silver stain, 700×). (D) Transmission electron microscopy from a glomerular capillary in a child with HIVICK. The black arrows show subepithelial deposits (4.000×). Figure 2C and D courtesy of Drs. Stewart Goetch and Professor Udai Kala.
Nephropathy
HIV-infected children can present with the classic clinical features of the nephrotic syndrome, including heavy proteinuria, edema, and hypoalbuminemia. Alternatively, the renal disease may be manifested clinically by persistent and isolated proteinuria. Thus, some programs are attempting to screen for proteinuria in children known to have HIV disease. There is a wide spectrum of renal diseases that occur in the setting of HIV infection. Although a clinical diagnosis can be made in some cases, renal biopsy studies show varying frequencies of histologic patterns.16–18 Biopsy diagnosis can reveal the typical histologic features of minimal change nephrotic syndrome, mesangioproliferative glomerular lesions, and “lupus-like” renal lesions.2,8–16 Other patients show renal changes consistent with the diagnosis of HIVAN or HIV-immune complex disease (HIVICK) (Fig. 2B–D).17,18 Thus, performing a renal biopsy is the only way to establish a definitive diagnosis.
HIVAN is the most widely recognized cause of heavy proteinuria in HIV-infected African American children,2,8–10 and black race is an established risk factor for the development of HIVAN.7–12 In adults, HIVAN usually presents with the classic histologic findings of collapsing FSGS and tubular microcystic changes.17,18 In contrast, HIV-infected children more frequently show mesangial hyperplasia and/or classic FSGS in combination with the microcystic tubular lesions.2,8–10 Children with mesangial hyperplasia show a slower rate of progression of their renal disease when compared with children with classic or collapsing FSGS.2,9 Although unproven, it has been argued that mesangial hypercellularity may be an early sign of FSGS.9
Studies from the United States have shown that HIVAN is a common cause of chronic kidney disease in HIV-infected adults.18–20 Early studies in children and adults suggested that HIVAN usually develops during the late stages of HIV disease, in association with a high viral load and a low CD4+ cell count.2,8–10,19,20 A recent study has found that reduction of the HIV viral load by ART may prevent progression of proteinuria and improve the clinical outcome of HIV-infected children.14
Studies in HIV-infected patients from Africa have found a variety of renal diseases.5,20–22 One study from South Africa examined 99 adult biopsy specimens and showed the presence of classic HIVAN and HIVICK in approximately 27% and 21%, respectively.21 These renal diseases play an important role in the development of chronic kidney disease. Renal biopsy specimens with HIVICK may show subepithelial immune deposits inducing a “ball-in-cup” glomerular basement membrane reaction.21 The renal histologic lesions found in 2 pediatric renal biopsy studies from South Africa are shown in Table 1.
Table 1.
Renal Histologic Findings in Two Studies From HIV-Infected Children With Renal Disease Living in South Africa
| Number of Pediatric Patients | Johannesburg5: 52 of 60 Underwent a Biopsy (86%) | Cape Town22: 14 of 14 Underwent a Biopsy (100%) |
|---|---|---|
| HIVICK | 50.8% | 7% |
| FSGS/HIVAN | 11.5% | 36% |
| Mesangioproliferative glomerulonephritis | 2.2% | 28.5% |
| Minimal change disease | 2.2% | |
| Severe interstitial nephritis | 11.5% | 7% |
| Infectious changes (including TB) | 1.5% | 21.5% |
| Acute tubular necrosis | 5.9% | |
| Kaposi’s sarcoma | 2.2% | |
| Bladder stones | 2.2% |
Tubulopathy
The presence of renal tubular disorders in HIV-infected African American children was recognized during the early years of the HIV epidemic.2,9 A more recent study from Venezuela found that renal tubular disorders also are common in HIV-infected Hispanic children.23 Hypercalciuria was seen most frequently, with a potential for nephrocalcinosis, but crystalluria, hyperchloremia, and metabolic acidosis also are seen. These metabolic complications may be in part responsible for the growth impairment frequently seen in HIV-infected children.2,9 Tubular disorders may induce sodium, potassium, and phosphate wasting states, which also mistakenly could be attributed to gastrointestinal diseases. Renal tubular disorders often are identified when electrolyte abnormalities do not improve after diarrhea or other gastrointestinal complications have resolved. Treatment can be clinically difficult because a large oral intake of supplements is required. This therapy can have side effects such as diarrhea, in the case of phosphate, which could perpetuate an ongoing cycle of electrolyte losses. In addition, the renal concentration ability of HIV-infected children might be impaired, and the infusion of intravenous hypotonic or isotonic solutions must be monitored closely to prevent the development of acute dysnatremic disorders causing severe neurologic complications or death.2,24 Finally, tubular disorders also could be related to nephrotoxic effects of medications, such as antibiotics or the antiretroviral agent tenofovir.25
Chronic Kidney Disease
Insidious onset of renal failure is usually the norm if HIV-infected children are not screened for the presence of renal diseases. Early onset proteinuria is a useful clinical clue indicating the presence of renal disease. Symptoms such as polyuria, polydipsia, fatigue, headache, seizures, and hypertension together with unexplained severe acidosis can be suggestive of chronic kidney disease. However, many patients in resource-limited areas may present only with marked proteinuria, or even with oliguria and ESRD.
DIAGNOSIS OF HIV-ASSOCIATED RENAL DISEASE IN CHILDREN
Clinical features of HIV infection such oral candidiasis, failure to thrive, and lymphadenopathy may be observed on physical examination before the diagnosis of HIV infection is established. The interpretation of blood tests confirming HIV infection is age-dependent, especially in young children, and should be discussed with an infectious disease expert.
The initial renal evaluation should include blood urea nitrogen, serum creatinine and electrolytes, and urine electrolytes to evaluate for tubulopathies. The urinary sediment can provide important clues such as the presence of clusters of renal epithelial cells forming cyst-like structures, which are seen in children with HIVAN and HIV-HUS.2,26 All HIV-infected children should be screened for proteinuria at least once a year. Proteinuria is not always detected in diluted urine samples during the early stages of HIVAN or in the presence of tubular disorders.2 Although hypertension is not a typical finding in the early stages of HIVAN, the blood pressure should be monitored regularly. The presence of (1) hypertension, (2) macroscopic hematuria, (3) microscopic hematuria without proteinuria, (4) increased blood urea nitrogen or serum creatinine values without significant proteinuria, and (5) persistent proteinuria in white children, are all clinical features not typical of HIVAN, and should be a clear indication to search for an alternative etiology of the renal disease.2 Ultrasound examination should be performed to assess renal size and echogenicity and exclude obstruction or anatomic pathology, with renal biopsy to follow if indicated owing to the presence of proteinuria. If clinically indicated, infections such as tuberculosis (TB) should be excluded. Further investigations may be limited according to resource availability in some settings.
TREATMENT OF HIV-ASSOCIATED RENAL DISEASE IN CHILDREN
Before the introduction of ART, treatment consisted only of supportive symptomatic therapy. In one study, children with HIV-related kidney disease who were on corticosteroids for treatment of lymphocytic interstitial pneumonitis showed a variable response of the renal disease to corticosteroids.2 The short-term effects of corticosteroids may be well tolerated,2,9,27,28 but their long-term risks in HIV-infected children are unknown, especially in countries with a high prevalence of TB. Moreover, in the absence of appropriate ART, corticosteroids have been unable to prevent the progression of HIV-associated childhood renal diseases.2,9,10
Diuretics, angiotensin-converting enzyme inhibitors, and angiotensin-receptor blockers are other forms of supportive therapy available for HIV-related kidney disease in children.2,9,27–29 These agents should be used with caution in HIV-infected children with nephrotic syndrome, severe hypoalbuminemia, tubular disorders causing salt wasting, and diarrhea or other gastrointestinal problems.2,9 These clinical situations induce extracellular volume contraction and activate the renin-angiotensin system. Blocking the renin-angiotensin system under clinical conditions in which the renal perfusion pressure is dependent on high levels of angiotensin II will decrease the glomerular filtration rate, and can induce acute renal failure if these changes are not recognized in a timely manner.
The introduction of ART has revolutionized the clinical management of HIV-associated renal disease.14,27–30 The use of ART is associated with a marked improvement of HIVAN, resulting in slower progression to ESRD,28,29 or even in recovery from dialysis-dependent renal failure30 provided the kidney damage is not too severe.
In resource-limited countries with a high prevalence of HIV infection, chronic renal failure often presents late in the course of the illness. Onset of this condition often is undetected because renal disease screening, such as urine testing and blood pressure monitoring, is not performed routinely. These children may present with nonspecific signs such as anemia, failure to thrive, poor appetite, and lack of energy. ESRD with fluid overload and hypertension are often the presenting signs. Renal ultrasound may show large kidneys consistent with HIVAN, or in the case of long-standing kidney disease, already may show signs of fibrosis with small kidneys.
Dialysis
In the early days of managing HIV-related renal disease, dialysis was thought to be contraindicated because of poor survival and concern about the infection rate on dialysis. With time, renal replacement therapy was shown to be possible, especially in pediatric patients in whom dialysis therapies have offered improved survival.7,9,14,31 A debate still remains as to which modality, peritoneal or hemodialysis, is the most appropriate for children. Peritoneal dialysis may be associated with increased infections, but is more readily available than hemodialysis in resource-poor countries, and may present less risk for health care professionals. Nevertheless, the peritoneal fluid contains HIV-infected mononuclear cells and should be handled with all the necessary precautions to prevent the transmission of HIV-1 to health care workers.2 In the United States, hemodialysis is the preferred modality in perinatally infected children because of the availability of resources and expertise for this treatment, as well as the added burden of peritoneal dialysis for the family members who are often managing their own HIV disease as well as that of the child.7,14,31 It is important to reduce the HIV viral load of children undergoing dialysis as much a possible, to improve their quality and length of life, and to make them eligible candidates for kidney transplant.
Transplantation
In the early years of the AIDS epidemic, HIV infection was considered an absolute contraindication to kidney transplantation because the combination of transplantation plus immunosuppression appeared to shorten the AIDS-free time in HIV-infected patients, compared with hemophiliac control groups.32 Subsequently, improvements in HIV-related morbidity and mortality with ART have prompted a re-evaluation of renal transplantation in this population.33 For example, studies in adherent adults have suggested that adult patients with HIV infection do better after transplantation than on dialysis. The immunosuppressant drugs used are similar to those used in non-HIV transplants. Renal transplantation in adults can be successful, provided there is stable maintenance of ART, the HIV viral load is undetectable for at least 6 months, and the CD4 cell count is greater than 200 cells/mm3.
In a group of HIV-positive patients receiving solid-organ transplants in the 1980s, who were infected either preoperatively or postoperatively, the best survival results (70%) were in fact shown in the pediatric group.33 The selection of children for transplantation, and the assessment of their immune status, should take into consideration the age and weight of the child, as well as different parameters for CD4 counts33,34: (1) younger than 1 year of age: aim to get to 1 year or 10 kg on dialysis, (2) 1 to 6 years of age: CD4% greater than 25%, taking into account the absolute CD4 count, and (3) older than 6 years of age: CD4 count greater than 200 cells/μL.
To date, very few pediatric nephrology units worldwide have transplanted a significant number of HIV-infected children, but this clinical experience is expected to increase as more HIV-infected children undergo this procedure. In addition to the challenges faced by adult transplant recipients, additional problems specific to pediatric patients include the need for cooperative providers and families to supervise the double-compliance required for both ART and immunosuppressive regimens. This is particularly concerning in adolescents, both in terms of risk-taking behavior and poor compliance associated with this age.31 Poor compliance with ART can lead to increased HIV resistance patterns and complicate management. Overall, renal transplantation in adults, and seemingly in children, can be successful in HIV-positive patients provided the HIV disease is under control.
In children who are immunosuppressed both by HIV as well as the use of immunosuppressant medications, there remains concern that overwhelming infections will occur, including typical nosocomial bacteria, viruses such as cytomegalovirus and Epstein-Barr virus, and atypical organisms. Tuberculosis remains a significant problem in many parts of Africa, and the prevalence has escalated with the HIV epidemic. TB was an important cause of pediatric systemic illness in 2 South African studies. Thirty-three percent of pediatric renal patients in a Johannesburg study had or were currently being treated for pulmonary TB,5 and renal TB was observed in 2 of 14 (14%) pediatric patients in a Cape Town study.22 In a separate review from Cape Town, among 150 HIV-negative pediatric renal transplants, the incidence of TB acquired posttransplantation was 9.8%. This was compared with 9.7% of liver transplant patients in the same center, illustrating the high prevalence of TB in this community.35 Multidrug-resistant TB and extensively drug-resistant TB have become a major concern. In addition, anti-TB medications can induce liver enzymes that affect the metabolism and serum levels of some immunosuppressant agents and other drugs, complicating the clinical management of transplant recipients.36
In addition to the potential for infectious complications, the transplantation of HIV-infected children also raises ethical concerns. The scarcity of organs for transplantation may force organs to be allocated to the best-possible-outcome recipient without concomitant risk factors. In Africa, HIV infection itself has resulted in a reduction in the number of suitable donors, with resultant lower organ availability and increased waiting times. Ideas have circulated about using HIV-positive donors for HIV-positive recipients, but significant controversy has arisen around this topic. In particular, there is concern about different HIV viral strains and associated drug resistance.
Ethical aspects of living donor transplantation are also important, especially in children, in whom pre-emptive transplantation may avoid the physical and psychologic stress of dialysis and improve retarded growth. Judgment then also arises between the values of life in children versus adults. In these circumstances, commercialism may be considered and should be prevented according to the Ethical Council of the Transplantation Society for both ethical and medical reasons. The risk is very high, not only for donors but for transplant recipients as well, because there may be poor screening not only for HIV-1 but also for other infectious agents.37
SCREENING FOR RENAL DISEASE IN HIV-INFECTED CHILDREN
Many HIV-associated renal diseases are asymptomatic during their early stages, thus recommendations have been made that all individuals be assessed for the presence of kidney disease at the time of HIV diagnosis.29,38 This screening is even more important in children, who may have a longer life expectancy if treated appropriately. Screening should include urinalysis and serum creatinine levels to estimate renal function.38,39
A South African study screened 615 HIV-infected adults who were not receiving ART for proteinuria, in an attempt to make an early diagnosis of HIVAN.39 Renal biopsy was performed in 30 patients with proteinuria or microalbuminuria, and 25 of 30 (83%) of these renal biopsies revealed histologic features consistent with HIVAN. Microalbuminuria was found to be an early manifestation of HIVAN. These findings suggest that screening HIV-infected patients for microalbuminuria might facilitate the early diagnosis of HIVAN.39,40 Given the large number of HIV-infected people in Africa, the early detection and treatment of HIVAN should become a major priority.
CONCLUSIONS
In children, initiation of ART with reduction of viral load and restitution of the immune system currently provides the most promising treatment to prevent the progression of childhood HIVAN to ESRD.7,14 Hopefully in the near future, better education, prevention, and treatment programs will lead to the eradication of this fatal childhood disease. However, at present, HIV disease, including renal disease, remains a major problem in sub-Saharan Africa, where other health priorities may prevail,35 resources are lacking, and, most importantly, there is lack of ART availability.
Acknowledgments
Supported by National Institutes of Health grants R0-1 DK-49419, R0-1 HL55605, and R21 NICAN-AT-002278 (P.E.R.).
The authors thank Professor Brian Eley, Head of Paediatric Infectious Disease and HIV Service, Red Cross Children’s Hospital, Cape Town, for assistance with up to date HIV population statistics locally in pediatric patients; Dr. William Bates, Division of Anatomical Pathology, Department of Pathology, National Health Laboratory Service (NHLS) and Faculty of Health Sciences, University of Stellenbosch, and Dr. Peter Nourse, Department of Pediatric Nephrology, Tygerberg Hospital and University of Stellenbosch (Cape Town) for providing a light microscopy picture from a child with HIVAN (Fig. 2B); and Drs. Stewart Goetch (Department of Histopathology) and Professor Udai Kala, Head of Pediatric Nephrology, from Baragwanath Hospital, University of Witwatersrand (Johannesburg), for providing the light and electron microscopy pictures from children with HIVICK (Fig. 2C and D). Finally, the authors would like to thank Dr. Christina Wyatt from Mount Sinai School of Medicine, New York, for reading the manuscript and providing very helpful suggestions.
References
- 1.UNAIDS. AIDS epidemic update. 2007 Available from: www.unaids.org/en/KnowledgeCentre/HIVData/EpiUpdate/EpiUpdArchive/2007/
- 2.Ray PE, Rakusan TM, Loechelt BJ, Selby DM, Liu X-H, Chandra RS. Human immunodeficiency virus (HIV)-associated nephropathy in the children from the Washington D.C. area; 12 Years’ experience. Semin Nephrol. 1998;18:396–05. [PubMed] [Google Scholar]
- 3.Benson C, Kaplan J, Masur H. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. Clin Infect Dis. 2005;40 (Suppl 1):S1–84. doi: 10.1086/427295. [DOI] [PubMed] [Google Scholar]
- 4.McCulloch MI. Introduction to pediatric HIV disease [abstract] Pediatr Nephrol. 2007;22:1438, 298. [Google Scholar]
- 5.Kala U, Petersen K, Faller G, Goetsch S. Spectrum of severe renal disease in children with HIV/Aids at Chris Hani Baragwanath Hospital, Johannesburg [abstract] Pediatr Nephrol. 2007;22:1439, 301. [Google Scholar]
- 6.Fauci SA. HIV-1 and AIDS. 20 years of science. Nat Med. 2003;9:839–43. doi: 10.1038/nm0703-839. [DOI] [PubMed] [Google Scholar]
- 7.Ray PE, Xu L, Rakusan T, Liu XH. A 20 year history of childhood HIV-associated nephropathy. Pediatr Nephrol. 2004;19:1075–92. doi: 10.1007/s00467-004-1558-1. [DOI] [PubMed] [Google Scholar]
- 8.Pardo VL, Meneses R, Ossa L, Jaffe DJ, Strauss J, Roth D, et al. AIDS-related glomerulopathy: occurrence in specific risk groups. Kidney Int. 1987;31:1167–73. doi: 10.1038/ki.1987.124. [DOI] [PubMed] [Google Scholar]
- 9.Strauss J, Abitbol CL, Zilleruelo G, Scott G, Paredes A, Malaga S, et al. Renal disease in children with the acquired immunodeficiency syndrome. N Engl J Med. 1989;321:625–30. doi: 10.1056/NEJM198909073211001. [DOI] [PubMed] [Google Scholar]
- 10.Connor E, Gupta S, Joshi V, DiCarlo F, Offenberger J, Minnefor A, et al. Acquired immunodeficiency syndrome associated renal disease in children. J Pediatr. 1988;113:39–44. doi: 10.1016/s0022-3476(88)80525-0. [DOI] [PubMed] [Google Scholar]
- 11.Rao TK, Filippone EJ, Nicastri AD, Landesman SH, Frank S, Chen CK, et al. Associated focal and segmental glomerulosclerosis in the acquired immunodeficiency syndrome. N Engl J Med. 1984;310:669–73. doi: 10.1056/NEJM198403153101101. [DOI] [PubMed] [Google Scholar]
- 12.Pardo V, Aldana M, Colton RM, Fischl MA, Jaffe D, Moskowitz L, et al. Glomerular lesions in the acquired immunodeficiency syndrome. Ann Intern Med. 1984;101:429–34. doi: 10.7326/0003-4819-101-4-429. [DOI] [PubMed] [Google Scholar]
- 13.Ray PE, Liu XH, Xu L, Rakusan T. Basic fibroblast growth factor in HIV-associated hemolytic uremic syndrome. Pediatr Nephrol. 1999;13:586–93. doi: 10.1007/s004670050749. [DOI] [PubMed] [Google Scholar]
- 14.Chaparro AI, Mitchell CD, Abitbol CL, Wilkinson JD, Baldarragi G, Lopez E, et al. Proteinuria in children infected with the human immunodeficiency virus. J Pediatr. 2008;152:844–9. doi: 10.1016/j.jpeds.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 15.El Syegh S, Keller MJ, Huprikar S, Murphy B. Solid organ transplantation in HIV-infected recipients. Pediatr Transplant. 2004;8:214–21. doi: 10.1111/j.1399-3046.2004.00190.x. [DOI] [PubMed] [Google Scholar]
- 16.Haas M, Kaul S, Eustace JA. HIV-associated immune complex glomerulonephritis with “lupus-like” features: a clinicopathologic study of 14 cases. Kidney Int. 2005;67:1381–90. doi: 10.1111/j.1523-1755.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 17.Fabian J, Katz I, Gerntholtz T, Goetsch S, Naicker S. Chronic kidney disease in human immunodeficiency virus infection. Panminerva. 2007;49:51–66. [PubMed] [Google Scholar]
- 18.Wyatt CM, Klotman PE. HIV-1 and HIV-associated nephropathy 25 years later. Clin J Am Soc Nephrol. 2007;2 (Suppl):S20–4. doi: 10.2215/CJN.03561006. [DOI] [PubMed] [Google Scholar]
- 19.Winston JA, Klotman ME, Klotman PE. HIV-associated nephropathy is a late, not early, manifestation of HIV-1 infection. Kidney Int. 1999;55:1036–40. doi: 10.1046/j.1523-1755.1999.0550031036.x. [DOI] [PubMed] [Google Scholar]
- 20.Emen CP, Arogundade F, Sanusi A, Adelusola K, Wokoma F, Akinsola A. Renal disease in HIV-seropositive patients in Nigeria: an assessment of prevalence, clinical features and risk factors. Nephrol Dial Transplant. 2008;23:741–6. doi: 10.1093/ndt/gfm836. [DOI] [PubMed] [Google Scholar]
- 21.Gerntholtz TE, Goetsch SJ, Katz I. HIV-related nephropathy: a South African perspective. Kidney Int. 2006;69:1885–91. doi: 10.1038/sj.ki.5000351. [DOI] [PubMed] [Google Scholar]
- 22.Nourse P, Bates W, Gajjar P, Sinclair P, Sinclair-Smith, McCulloch M. Paediatric HIV renal disease in Cape Town, South Africa [abstract] Pediatr Nephrol. 2007;22:1597, 750. [Google Scholar]
- 23.Gonzalez C, Arietta G, Langmann CB, Zibaoui P, Escalona L, Dominguez LF, et al. Hypercalciuria is the main renal abnormality finding in human immunodeficiency virus-infected children in Venezuela. Eur J Pediatr. 2008;16:509–15. doi: 10.1007/s00431-007-0538-4. [DOI] [PubMed] [Google Scholar]
- 24.Friedman AL, Ray PE. Maintenance fluid therapy: what it is and what it is not. Pediatr Nephrol. 2008;23:677–80. doi: 10.1007/s00467-007-0610-3. [DOI] [PubMed] [Google Scholar]
- 25.Hussain S, Khayat A, Tolaymat A, Rathmore MH. Nephrotoxicity in a child with perinatal HIV on tenofovir, didanosine and lopinavir/ritonavir. Pediatr Nephrol. 2006;21:1034–6. doi: 10.1007/s00467-006-0109-3. [DOI] [PubMed] [Google Scholar]
- 26.Ray PE, Liu XH, Henry D, Dye L, Xu L, Orestein JM, et al. Infection of human primary renal epithelia cells with HIV-1 from children with HIV-associated nephropathy. Kidney Int. 1998;53:1217–29. doi: 10.1046/j.1523-1755.1998.00900.x. [DOI] [PubMed] [Google Scholar]
- 27.Wyatt CM, Klotman PE. HIV-associated nephropathy in the era of antiretroviral therapy. Am J Med. 2007;120:488–92. doi: 10.1016/j.amjmed.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 28.Kimmel PL, Barisoni L, Kopp JB. Pathogenesis and treatment of HIV-associated renal diseases: lessons from clinical and animal studies, molecular pathologic correlations, and genetic investigations. Ann Intern Med. 2003;139:214–26. [PubMed] [Google Scholar]
- 29.Gupta SK, Eustace JA, Winston JA, Boydstun II, Ahuja TS, Rodriguez RA, et al. Guidelines for the management of chronic kidney disease in HIV-infected patients: recommendations of the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2005;40:1559–85. doi: 10.1086/430257. [DOI] [PubMed] [Google Scholar]
- 30.Szczech LA, Gupta SK, Habash R, Guasch A, Kalayjian R, Appel R, et al. The clinical epidemiology and course of the spectrum of renal diseases associated with HIV infection. Kidney Int. 2004;66:1145–52. doi: 10.1111/j.1523-1755.2004.00865.x. [DOI] [PubMed] [Google Scholar]
- 31.Abitbol CL, Friedman LB, Zilleruelo G. Renal manifestations of sexually transmitted diseases and the kidney. Adolesc Med Clin. 2005;16:45–65. doi: 10.1016/j.admecli.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Tzakis AG, Cooper MH, Dummer JS, Ragni M, Ward JW, Starzl TE. Transplantation in HIV+ patients. Transplantation. 1990;49:354–8. doi: 10.1097/00007890-199002000-00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stock PG, Roland ME, Carlson L, Freise CE, Roberts JP, Hirose R, et al. Kidney and liver transplantation in human immunodeficiency virus-infected patients: a pilot safety and efficacy study. Transplantation. 2003;76:370–5. doi: 10.1097/01.TP.0000075973.73064.A6. [DOI] [PubMed] [Google Scholar]
- 34.South African Renal Society. Draft guidelines for management of solid organ transplantation in HIV infected patients— kidney transplantation. 2008 In press. [Google Scholar]
- 35.McCulloch MI. Infections in paediatric transplantation in developing countries. Paper presented at: 4th Congress of the International Pediatric Transplant Association (IPTA) on Pediatric Transplantation; 2007 March 20; Cancun, Mexico. [Google Scholar]
- 36.McCulloch MI. Resource allocation and outcome of dialysis and transplantation in a developing country [abstract]. Pediatr Nephrol; Paper presented at: 14th Congress of the International Paediatric Nephrology Association; 2007. p. 1432.p. 254. [Google Scholar]
- 37.Bruzzone P, Berloco PB. Ethical aspects of renal transplantation from living donors. Transplant Proc. 2007;39:1785–6. doi: 10.1016/j.transproceed.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 38.Fine DM, Atta MG. Kidney disease in the HIV-infected patient. AIDS Patient Care STDS. 2007;21:813–24. doi: 10.1089/apc.2006.0210. [DOI] [PubMed] [Google Scholar]
- 39.Han TM, Naicker S, Ramdial PK, Assounga AG. A cross-sectional study of HIV-seropositive patients with varying degrees of proteinuria in South Africa. Kidney Int. 2006;69:2243–50. doi: 10.1038/sj.ki.5000339. [DOI] [PubMed] [Google Scholar]
- 40.Naicker S, Han TM, Fabian J. HIV/AIDS—dominant player in chronic kidney disease. Ethn Dis. 2006;16 (Suppl 2):S56–60. [PubMed] [Google Scholar]