Abstract
Anterior cruciate ligament surgery and rehabilitation have changed drastically during the past 30 years. The patellar tendon autograft fixed with buttons provides tight bone-to-bone placement of the graft and quick bony healing, which allows accelerated rehabilitation to obtain full range of motion and strength. Although surgical stability is easily reproducible, long-term patient satisfaction is difficult to guarantee. Full knee range of motion should be compared to that of the contralateral normal knee, including full hyperextension. We followed the progress of all patients to gauge the utility of our rehabilitation program. In order of importance, the lack of normal knee range of motion (within 2° extension and 5° of flexion compared with that of the normal knee), partial or total medial meniscectomy, partial or total lateral meniscectomy, and articular cartilage damage were related to lower subjective scores. Rehabilitation after ACL reconstruction must first strive to achieve full symmetrical knee range of motion before aggressive strengthening can begin. Our current perioperative rehabilitation starts at the time of injury and preoperatively includes aggressive swelling reduction, hyperextension exercises, gait training, and mental preparation. Goals after surgery are to control swelling while regaining full knee range of motion. After quadriceps strengthening goals are reached, patients can shift to sport-specific exercises. When using a graft from the contralateral knee, the conflicting goals of strengthening the donor site and achieving full knee range of motion are divided between the knees. Thus, normal range of motion and strength can be achieved more easily and more quickly than when using an ipsilateral graft. Regardless of the graft source, a systematic rehabilitation program that emphasizes the return to symmetrical knee motion, including hyperextension, is necessary to achieve the optimum result.
Introduction
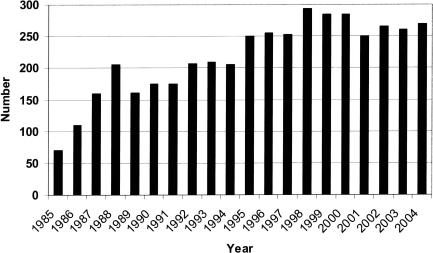
Since 1982, when the senior author dedicated his practice to anterior cruciate ligament (ACL) reconstruction, he has performed more than 5000 of the procedures. Although successful results after ACL reconstruction are not universally predictable, the surgical process has become easily reproducible as a standard methodology has evolved.1 Now performing about 225 ACL reconstructions per year (Fig. 1), the senior author continues to use a medial mini-arthrotomy for excellent exposure to the joint and optimal tunnel and graft placement. Based on the positive results of ACL revision surgery that utilized a contralateral patellar tendon graft source, we have used a patellar graft from the contralateral knee for primary ACL reconstruction surgeries since 1994.2–4 Button fixation is used to prevent overtensioning; it allows tight bone fit in the tunnels and rapid bone-to-bone healing. The consistent results have led to a postoperative expectation for the return of stability, strength, and the ability to return to sports in most patients.3,5
Fig. 1.
The senior author now performs about 250 anterior cruciate ligament (ACL) reconstructions per year. The only other surgeries performed are knee arthroscopies and patellar realignments (about 300 per year)
Despite anticipation of positive surgical results based on current technical methodology, even well-performed ACL surgery can result in a poor outcome if rehabilitation is not conducted appropriately.6–8 Since 1982, we have cautiously and gradually implemented evolutionary changes in our rehabilitation program based on continual postoperative follow-up of previous patients.1,9 In the field of orthopedics, where communication between a knee surgeon and physical therapist is essential, we have unified the two equally important halves of the recovery process. Our present philosophy integrates preoperative and postoperative rehabilitation into a streamlined “cascade of events” that stresses regaining total knee symmetry through a series of identifiable goals and associated exercises.
What is symmetry?
People have symmetrical knees that are unique to the individual. Patients who have a problem with one of their knees usually stop using it normally with basic everyday activities such as walking, squatting, ascending and descending stairs. Eventually the problem manifests as loss of knee motion and strength. Many physicians tell patients who complain of knee problems to work on strengthening the knee to regain functionality, but lack of motion is the underlying problem that causes the loss of strength. To achieve full, symmetrical motion, the first thing to work on is any range of motion (ROM) deficit. Our objective test results show the importance of obtaining full symmetrical ROM after ACL reconstruction. When evaluating full ROM, an important consideration is that 99% of women and 95% of men exhibit some degree of hyperextension in their knees with averages of 5° and 6°, respectively.10 Even the loss of 3°–5° of extension compared with the opposite knee can result in lower postoperative subjective scores. Thus, the definition of full ROM must depend on symmetry between the knees rather than the conventional practice of gauging knee motion against a fixed standard.
Historical results
The theories regarding acute ACL reconstruction have changed dramatically since the senior author began practicing. Conventional ACL reconstruction studies, focusing on surgical technique and instrumentation, fixation, graft tension, meniscus repair, and the articular, cartilage repair method, have been associated with complications related to inadequate understanding of knee function. These programs have relied on protection of the reconstructed ligament by limiting knee extension, weight-bearing, and the return to activities after surgery to achieve stability. Although stability could be achieved, it was generally at the expense of postoperative complications.1
Anterior cruciate ligament injury, its treatment, and its rehabilitation continue to be an area of interest to both clinicians and researchers. Surgical procedures have been refined, and rehabilitation programs are constantly being evaluated and updated to minimize morbidity and allow the safest, most predictable return to activity. The most applicable factors found by the senior author in shaping his current rehabilitation program included the following: (1) Patient noncompliance and observing its effect on the outcomes were essential parts of the rehabilitation program evolution. (2) Immediate surgery following acute ACL tears is undesirable for a variety of reasons. (3) The contralateral patellar tendon is an excellent graft source based on the ease of rehabilitation associated with its use in ACL revision results. (4) Regaining full ROM equal to the contralateral knee is the most important factor for ensuring the best long-term successful surgery result.
In one of our long term studies, many patients admitted to being noncompliant.9 Surprisingly, those patients achieved faster return of strength and a quicker return to activities with no graft failure. Assessing motion was the basis for our early rehabilitation program; and, as noncompliant patients demonstrated good motion without swelling or pain faster than our compliant patients, we soon began to realize that conventional rehabilitation programs may have been more restrictive than necessary. Owing to those unexpected results, we decided to shift the focus of our rehabilitation program to include patient goals of: (1) obtaining full ROM preoperatively; (2) staying down postoperatively with the reconstructed knee above the heart; (3) using a Cryo/Cuff cold/compression device (Cryo/Cuff; Aircast, Summit, NJ, USA) before and after surgery; (4) fully extending the knee on the day of surgery and maintaining full extension for the remainder of the postoperative period; (5) bending the knee past 90° on the day of surgery. Based on patient noncompliance, we also deemphasized that the use of crutches, splints, and braces and reduced our overall time projection for return to full activity. These evolutionary changes became the basis of our current rehabilitation model, a progressive scheme that allows patients to advance as they achieve quantifiable goals.
Many of the problems and complications found with ACL reconstructions stemmed from the belief that immediate surgery was needed following acute knee injuries. Despite its common practice, arthrofibrosis is more likely to result from an acutely repaired ACL. A previous study by Shelbourne and Dersam1 showed that stability results following surgery are similar in acute and chronic cases, but acute surgery was associated with a much higher incidence of postoperative motion deficits.6,7,11 Although it first appeared that the time from injury was important, we soon determined that it was the condition of the knee that was crucial for surgical timing. Rather than a definitive time window between injury and surgery, a patient must achieve a series of goals that has become the basis of our current rehabilitation program.
A secondary benefit of avoiding immediate reconstruction is improved psychological readiness in the patient. ACL surgery requires vigorous and extensive rehabilitation efforts from patients. Thus, for optimal recovery from surgery, there must not only be expert medical care but also patient commitment.12 By encouraging active participation on the part of the patient and encouraging the establishment of a meaningful relationship with a physical therapist during the preoperative period, patients fare better with postoperative rehabilitation. By delaying surgery, patients have time for the mental preparation associated with the surgery and can begin to understand what is involved with the surgery itself and their responsibilities with rehabilitation. They are able to address the periods of depression, denial, and anger that have been shown to occur before final acceptance of an injury.12 Thus, the patient should arrive in the operating room ready to go with an attitude of looking forward to the reconstructive procedure and with an understanding of the postoperative rehabilitation.
Currently, the autogenous bone-patellar tendon- bone graft is our graft of choice for ACL reconstruction. Typically, the graft has been obtained from the ipsilateral knee. A study of revision ACL reconstruction details an alternative procedure to take the graft from the contralateral, noninvolved knee, allowing two rehabilitation programs to take place. The contralateral graft site has shown significant benefits by dividing the rehabilitation goals for the ACL knee and the graft knee, allowing a more efficient process.13,14 By dividing the work between the two knees, the patient is kept busy with easily gauged progress, knowing that he or she is taking an active role in the recovery process. Although we have embraced the benefits of a contralateral patellar tendon graft, the prescribed perioperative rehabilitation scheme is applicable to various graft sources with an underlying ultimate goal to ensure restoration of full ROM and strength and a faster return to full capability in sports without compromising stability.
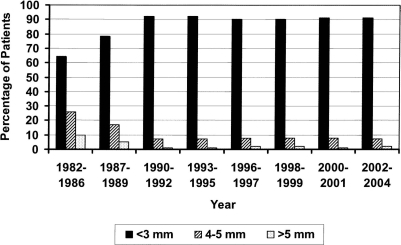
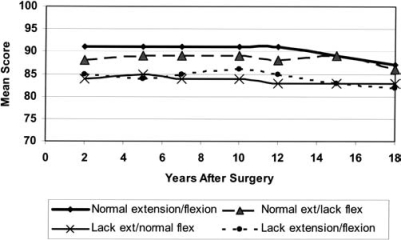
Our results at 10–20 years after surgery show that full knee ROM equal to that of the opposite normal knee is the definitive factor of long-term patient satisfaction. Many surgeons believe that early postoperative limitations in knee motion, strengthening, and functional activities are necessary because of the weakness of the ACL graft and the fixation to the graft. Our surgical results consistently display stability while simultaneously allowing full ROM during the early postoperative period (Fig. 2).9 Patients who maintained full ROM postoperatively fared significantly better in both subjective and objective research tests. Optimal results occurred for patients with two fully symmetrical knees according to International Knee Documentation Committee (IKDC) standards (Table 1). In order of importance, the lack of normal knee range of motion (within 2° of extension and 5° of flexion compared with that of the normal knee), partial or total medial meniscectomy, partial or total lateral meniscectomy, and articular cartilage damage are related to lower subjective scores (Fig. 3). Patients with deficient extension and flexion reported the worst subjective scores. Thus, obtaining full motion before surgery, especially hyperextension, has become a key variable that we use to determine surgical timing, and it is the primary goal of early postoperative rehabilitation.
Fig. 2.
Objective stability has been consistently obtained. Values shown are the manual maximum differences between knees as measured with the KT-1000 arthrometer
Table 1.
International Knee Documentation Committee criteria for the evaluation of range of motion in the reconstructed knee compared with that of the opposite knee
| IKDC rating | Extension | Flexion |
|---|---|---|
| Normal | ≤2° | ≤5° |
| Near normal | 3°–5° | 6°–15° |
| Abnormal | 6°–10° | 16°–25° |
| Severely abnormal | >10° | >25° |
IKDC, International Knee Documentation Committee
Fig. 3.
Subjective results of the 10- to 20-year study show the importance of obtaining full, symmetrical range of motion. The best long-term subjective scores were seen for patients who had normal knee extension
Because the key factor in ACL reconstruction success is full ROM, we have adopted the practice of taking the graft from the opposite knee, so the conflicting goals of strengthening the donor site and achieving full knee ROM are divided between the knees. The primary benefit of using a patellar tendon graft over a hamstring graft or allograft is its predictable stability. Because everyone undergoing ACL surgery would like to have the best postoperative results, with data showing that stability can be achieved in almost all correctly performed surgeries the patellar tendon provides an optimal graft site. We also examined variables other than stability that facilitated or prevented good results (ROM, strength, and patient confidence in the reconstructed knee). Autogenous hamstring grafts can provide reliable stability results but inhibit the regeneration of hamstring function, a particularly detrimental side effect for the young athlete. Our biggest challenge in advocating the patellar tendon graft became maintaining the high success rate of stability while also achieving the goals of full ROM, strength, and confidence. Our successful results are due to the combination of the contralateral patellar graft and our unique perioperative rehabilitation program.
Perioperative rehabilitation program
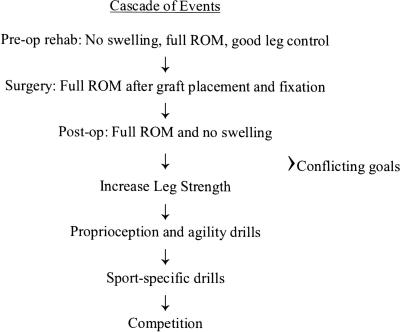
The principal result of the integration of our research has led to the emergence of our unique perioperative rehabilitation protocol (Fig. 4), which has been used in our office for more than 15 years. With the knowledge that full ROM is essential, not only for athletes to function at a high level but for less active patients to be able to perform comfortably everyday activities such as squatting, kneeling, and ascending and descending stairs, we designed our perioperative rehabilitation program with the principal goal of achieving postoperative symmetry of the two knees. The program starts at the time of injury and preoperatively includes aggressive swelling reduction, hyperextension exercises, gait training, and mental preparation. Goals after surgery are to control swelling while regaining full knee ROM. After quadriceps strengthening goals are reached, patients can shift to sport-specific exercises.
Fig. 4.
Cascade of events outlines a systematic rehabilitation program that emphasizes the return to symmetrical knee motion that includes hyperextension. ROM, range of motion
Regardless of the graft source fixation, preoperative and postoperative rehabilitation, and surgical timing, the ultimate goal of all patients is to achieve knee symmetry like they had preoperatively. So long as the surgical procedure does not preclude the reclamation of full ROM, the rehabilitation program should be appropriately designed to facilitate this goal. We have designed the following program as the best way for patients to achieve their goals working with our physical therapy staff.
Preoperative rehabilitation
It is essential that rehabilitation of an ACL injury begin immediately after the initial office evaluation. Prior to any operative intervention, patients are referred to our physical therapist for preoperative evaluation and readiness. Details of the patient’s present athletic activities and any future aspirations are important when planning postoperative rehabilitation. Physical therapists follow patients closely and communicate with the surgeon regarding the patient’s mental and physical preparation for surgery, as the success of reconstruction depends on both factors.3,12
Patients who desire ACL reconstruction are counseled about preoperative rehabilitation and their active role in the process. Before surgery is considered, patients are expected to meet a series of conditions, including completely normal ROM equal to that of the opposite knee, reduced knee effusion, normal gait, and good leg control. To achieve those ends, a series of exercises is utilized along with a Cryo/Cuff to reduce swelling. The exercises include towel stretches (Fig. 5), heel props exercises, standing extension habit, wall slide and heel slide exercises, and gait training. We perform preoperative testing so we can have objective measures for closely monitoring postoperative progress. Preoperative KT-1000 arthrometer measurements document knee laxity, and isokinetic testing objectively measures quadriceps muscle strength. Obtaining full ROM before surgery reduces the likelihood of motion problems postoperatively, so surgery is not performed until a patient has full extension equal to that of the noninvolved knee and is able to sit on his or her heels (Fig. 6). Other benefits of preoperative rehabilitation include familiarizing the patient with the same exercises he or she will be performing postoperatively and establishing a meaningful relationship between physical therapist and patient.
Fig. 5.
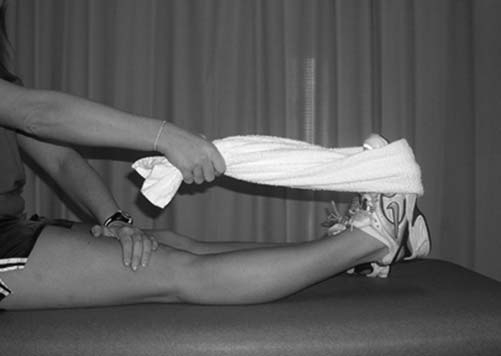
Towel stretch for knee extension. The towel is used to lift the heel of the affected lower extremity to end-range hyperextension by pulling the end of the towel upward toward the shoulder
Fig. 6.

Achieving full symmetrical flexion means the patient should be able to kneel and sit back on heels comfortably
Immediate postoperative rehabilitation
Postoperative rehabilitation begins in the operating room after graft placement to ensure full ROM and to prevent overtension. An antiembolism stocking is placed on the ACL-reconstructed leg along with a Cryo/Cuff (Fig. 7). The ACL-reconstructed knee is then placed in a continuous passive movement (CPM) machine to elevate the lower leg above the heart, as the key to early wound healing is eliminating knee effusion and hemarthrosis.1 The CPM machine is utilized for slow, assisted flexion to 125°. Heel slide exercises are performed with a yardstick positioned next to the leg with the zero end lined up with the end of the heel. The patient flexes the knee with the help of a towel looped under the thigh, and terminal flexion is held for 1min. The number of centimeters the heel has traveled is recorded by referencing the yardstick. The initial flexion should fall approximately in the range of 110°–120°, and the patient should use the yardstick method to gauge progress during the subsequent days. Hyperextension exercises include heel prop and towel stretch exercises. Heel prop exercises involve propping the heel on a rolled towel and then placing a 2.5-pound weight just distal to the incision for a 10-min period. Following heel raises, a patient performs three to five knee “thunks,” in which he or she flexes the knee to a height of several inches and then relaxes it, allowing it to fall into hyperextension. To complete the extension exercises, five to ten towel stretches are performed in combination with active heel raises to demonstrate quadriceps control. The patient stays in the hospital overnight to allow patient and family education about the goals that should be achieved during the first week at home. He is released the next day so long as he can demonstrate full extension, at least 110° of flexion, and is able to lift the ACL-reconstructed leg independently with quadriceps muscle contraction.
Fig. 7.

Cryo/Cuff provides both compression and cold therapy to reduce swelling. This modality used in combination with elevation in the continuous passive motion machine can effectively reduce any intraarticular effusion or hemarthrosis
Continuing postoperative rehabilitation
Once at home, patients are instructed to minimize swelling by limiting out-of-bed activities for the first 5 days after surgery and using the Cryo/Cuff and CPM at all times when not performing exercises. The previously mentioned exercise sets are all performed six times per day, with measurements recorded in a home exercise log. Patients receive a phone call from the physical therapist daily so they can ask any questions they have about their rehabilitation. Throughout the first phase of rehabilitation, knee extension is emphasized more than flexion. If extension becomes an issue, the Elite Seat, a portable, reclining extension device controlled by a hand lever, can be utilized (Fig. 8). The first postoperative visit is conducted about 1 week after surgery. At that time, progress is assessed; and if satisfactory goals have been achieved, the patient progresses to the next phase of rehabilitation. Aggressive strengthening exercises are introduced once the patient achieves full knee flexion. Regeneration of the graft site is achieved by high repetitions of step-up exercises on a step box. When full terminal extension and knee flexion are present, strengthening with the use of a stair machine and leg press exercises is initiated. For the first 4 weeks, the tendon is induced to regrow and hypertrophy. For the subsequent 4 weeks, the tendon is made stronger; after this point, specific functional exercises are conducted. Early return to sports-specific drills such as shooting baskets and kicking a ball can be started. Prior to increasing activity level, patients should have full hyperextension and be able to sit on their heels comfortably. When the return of strength is 70% of the preoperative normal leg value, functional progression of sports agility can be initiated. If swelling occurs in the ACL-reconstructed knee or the ROM decreases at any time, activity should be curtailed until full motion has been reestablished. The full range of expected goals and corresponding exercises from time of surgery until 8 weeks postoperatively are detailed in Table 2. At this point, the patient has ideally progressed to sport-specific drills and is making the jump from part-time to full-time competition.1,9
Fig. 8.
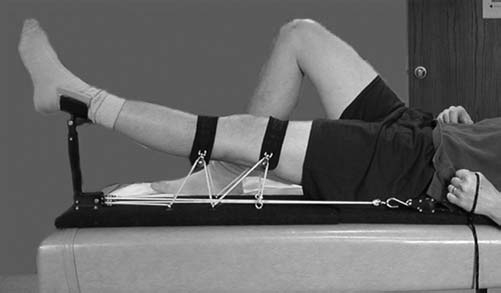
The Elite Seat device allows the patient to recline completely, which relaxes the hamstrings. The patient uses a pulley control to increase the mechanical force for knee extension
Table 2.
Perioperative rehabilitation phases
| Phase | Goals | Specific exercises |
|---|---|---|
| Preoperative | Attaining normal physiology and motion | Heel props, towel stretches, prone hangs; gait and stance training; heel slides, flexion hangs, wall slides |
| Immediately postoperative phase: through first week | Full extension, 115° of flexion; limited effusion; unassisted leg lifts and ambulation with normal gait | CPM flexion, heel slides, straight leg raises, heel props, towel cold/compression device continually |
| Intermediate phase: weeks 2–4 | Full extension, 120° of flexion, limitedeffusion; unassisted leg lifts and ambulation with normal gait | Heel props, towel stretches, Elite Seat, correct stance and walking, heel slides, wall slides, flexion hangs; step box — low level; cold/compression device |
| Advanced strengthening phase | Full motion and symmetrical strength in both knees | Progressing from above to step box at higher level, leg press, straight-line running; StairMaster, elliptical trainer, progression to sports specific exercise; cold/compression as needed; knee motion monitored daily: adjust strengthening and activities to ensure full motion is maintained |
| Return to competition | Symmetrical; normal knees; full competition | Sports-specific exercise, functional progression, return to competition |
CPM, continuous passive movement
Postoperative studies
Following surgery, patients participate in subjective and objective postoperative evaluations in which patients are sent modified Noyes and IKDC subjective questionnaires on a yearly basis. They are also asked to return for objective evaluation 1, 2, 5, 10, 15 and 20 years after surgery.
Comment
There is controversy over what features make a knee normal. Most physicians agree that a normal knee is stable, has good strength, and allows normal gait and functional activities. We suggest that the concept of symmetry between legs should define what is normal for a knee; hence, a normal knee is equal in motion, swelling, strength, and function to that of its contralateral counterpart. We base “normal” following ACL injury on the characteristics of the contralateral knee and then restore the ACL-reconstructed knee to that same level of motion, swelling, strength, and function.
Another controversy concerns the description of normal knee motion. Whereas some authors describe normal range of motion as 0°–135°, our studies show that most individuals have some degree of hyperextension.10 When dealing with young athletes, the goal of ACL reconstruction should not be to simply restore stability to the knee but to do so without causing iatrogenic problems such as permanent loss of motion, strength, or function. No other complication has as much potential to create a poor outcome as lack of normal knee motion — hence its emphasis in our rehabilitation protocol.4,6,7 Considering the young average age of our patients (22 years) and their preference to return to active life styles without being restricted by their knees, we have found that our perioperative rehabilitation protocol ensures the best results.9,12
The perioperative rehabilitation program outlined above is a proven method that has evolved from continual research since 1982. All of the changes in our rehabilitation program have been made in an effort to decrease the complications associated with ACL reconstruction; however, as a secondary benefit we have observed that patients are able to return to sports earlier than with conventional rehabilitation. Rehabilitation after ACL reconstruction must first strive to achieve full symmetrical knee ROM before aggressive strengthening can begin. When using a graft from the contralateral knee, the conflicting goals of strengthening the donor site and achieving full knee ROM are divided between the knees, expediting the return of full motion and strength. Regardless of the graft source, a systematic rehabilitation program that emphasizes the return to symmetrical knee motion that includes hyperextension is necessary to achieve the optimum result. We strive for all patients to maintain the highest standards for both knees, as the patient’s highest function will be at the level of the worst knee.
References
- 1.Shelbourne KD, Dersam MD. The evolution of rehabilitation for anterior cruciate ligament reconstruction. In: Williams RJ, Johnson DP, editors. Controversies in orthopaedic surgery: sports injuries to the knee. Oxford: Oxford University Press; 2003. pp. 135–50. [Google Scholar]
- 2.Shelbourne KD, O’Shea JJ. Revision anterior cruciate ligament reconstruction using the contralateral bone-patellar tendon-bone graft. Instr Course Lect. 2002;51:343–6. [PubMed] [Google Scholar]
- 3.Shelbourne KD, Thomas JA. Contralateral patellar tendon and the Shelbourne experience. Part 1. Revision anterior cruciate ligament reconstruction and rehabilitation. Sports Med Arthrosc Rev. 2005;13:25–31. doi: 10.1097/01.jsa.0000147194.03137.4e. [DOI] [Google Scholar]
- 4.Shelbourne KD, Thomas JA. Contralateral patellar tendon and the Shelbourne experience. Part 2. Results of revision anterior cruciate ligament reconstruction and rehabilitation. Sports Med Arthrosc Rev. 2005;13:69–72. doi: 10.1097/01.jsa.0000147183.24447.b6. [DOI] [Google Scholar]
- 5.Rubinstein RA, Jr, Shelbourne KD, Van Meter CD, McCarroll JC, Rettig AC. Isolated autogenous bone-patellar tendon-bone graft site morbidity. Am J Sports Med. 1994;22:324–7. doi: 10.1177/036354659402200305. [DOI] [PubMed] [Google Scholar]
- 6.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction: the effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–6. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 7.Mohtadi NG, Webster-Bogaert S, Fowler PJ. Limitation of motion following anterior cruciate ligament reconstruction: a case-control study. Am J Sports Med. 1991;19:620–5. doi: 10.1177/036354659101900612. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DL, Fu FH. Anterior cruciate ligament reconstruction: why do failures occur? Instr Course Lect. 1995;44:391–406. [PubMed] [Google Scholar]
- 9.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five to fifteen year evaluations. Am J Sports Med. 2000;28:446–52. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 10.De Carlo MS, Sell KE. Normative data for range of motion and single-leg hop in high school athletes. J Sport Rehab. 1997;6:246–55. [Google Scholar]
- 11.Shelbourne KD, Johnson BC. Effects of patellar tendon width and preoperative quadriceps strength on strength return after anterior cruciate ligament reconstruction with ipsilateral bone-patellar tendon-bone autograft. Am J Sports Med. 2004;32:1474–8. doi: 10.1177/0363546503262171. [DOI] [PubMed] [Google Scholar]
- 12.Udry E, Shelbourne KD, Gray T. Psychological readiness for anterior cruciate ligament surgery: describing and comparing the adolescent and adult experiences. J Athl Train. 2003;38:167–71. [PMC free article] [PubMed] [Google Scholar]
- 13.Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med. 2000;28:651–8. doi: 10.1177/03635465000280050501. [DOI] [PubMed] [Google Scholar]
- 14.De Carlo M, Shelbourne KD, Oneacre K. Rehabilitation program for both knees when the contralateral autogenous patellar tendon graft is used for primary anterior cruciate ligament reconstruction: a case study. J Orthop Sports Phys Ther. 1999;29:144–59. doi: 10.2519/jospt.1999.29.3.144. [DOI] [PubMed] [Google Scholar]