Abstract
Bone mineral density (BMD) is the best established marker for bone health. Over the last years a large number of studies have pointed to the variability in many target genes and their relation with bone mass and with other determinants of fracture risk such as ultrasound bone properties, skeletal geometry and bone turnover markers. The importance of genetic factors in the bone quality is substantial, but no consensus exists yet on the genes that are involved. Furthermore, there are many differences of clinical outcomes during bone-active treatments in the population-based studies. Heterogeneity in drug response may reflect varying responsiveness to boneactive treatments due to allele variation in the polymorphic target genes. In this regard, polymorphisms of vitamin D receptor and estrogen receptor loci appear genetic determinants of their corresponding hormonal treatment response such as vitamin D and estrogens. The present review focuses on the genetic determinants involved in the clinical response to bisphosphonate treatments for bone disorders. Knowledge of the molecular and functional consequences of the target genes is crucial to fully appreciate their significance and understand their potential clinical implications.
Keywords: bisphosphonate, collagen type 1, genetics, interleukine 1, polymorphism, vitamin D receptor.
Introduction
While medicinal use has been relatively recent, bisphosphonates (BPs) were first synthesized over a century ago by Von Baeyer & Hoffmann (1). However, commercial application for these compounds did not take place until 1960 when Blazer & Worms (2) reported their use for dental detergent solutions as complexing agents for calcium and magnesium. Then, cyclical etidronate (ETN) was one of the first bisphosphonates to be used for osteoporosis treatment (3) and clinical experience has shown it to be a safe and effective drug for the prevention and treatment of vertebral osteoporosis (4, 5). Today, BPs are a widely utilized class of compounds for the prevention and treatment of a variety of bone diseases (6-10).
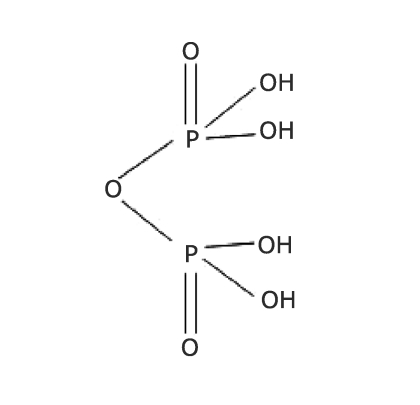
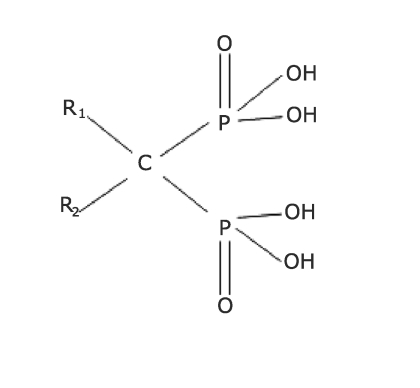
BPs are compounds with a molecular structure analogous to inorganic pyrophosphate (Fig. 1), the simplest of polyphosphates, which is able to inhibit the aggregation and the dissolution of calcium phosphate crystals in vitro. In vivo, pyrophosphate physiologically prevents the calcification of soft tissues (11) and could play a role in the processes of bone mineralisation. By substituting an oxygen atom (P–O–P) with a carbon atom (P–C–P) in the pyrophosphate molecule (Fig. 2), it is possible to obtain a class of compounds which are resistant to pyrophosphatase while maintaining the chemical-physical properties of pyrophosphate. These compounds can be considered stable analogues of pyrophosphate, resistant to hydrolysis. Due to the presence of a double link with phosphate by a single carbon atom these molecules are called “bisphosphonates”. Like pyrophosphate, BPs inhibit the formation, aggregation and dissolution of calcium phosphate crystals. Furthermore, they have a high affinity for bone mineralised matrix and are able to inhibit bone resorption processes increasing bone mineral density (BMD), their most important biological effect. It is generally accepted that BPs inhibit bone resorption by preventing osteoclast formation, restraining the bone-resorbing activity of osteoclasts and acting indirectly on stromal and hemopoietic cells (12). The BPs are classified according to the molecular mechanism of action. Non-nitrogen-containing BPs are metabolized by osteoclast to cytotoxic ATP analogues that are accumulated within the cell, whereas nitrogen-containing bisphosphonates inhibit the farnesyl-diphosphonate synthase, an enzyme in the mevalonate pathway (13). In spite of these different mechanisms, both classes of BPs ultimately lead to apoptosis by activation of caspases (14). This explains why these compounds are used, besides in osteoporosis, in all the pathological conditions characterised by increased bone resorption, such as Paget disease, malignant hypocalcaemia during myeloma, osteolytic bone metastasis and fibrous dysplasia of bone.
Figure 1.
- Chemical structure of pyrophosphate.
Figure 2.
- Chemical structure of bisphosphonates.
To date, interest of most scientists and clinicians working in genetics, is to recognize the markers useful in the diagnosis and in the patient management. In this view, genetics not only offer possibility to precociously recognize patients at risk to develop bone disorders, but also to foresee the individual response to drugs. Pharmacogenetics has the potential to allow early specific
and efficacious treatments, with consequent better chances for the patient health and reduced economic loss for the patient and the society.
The present review focuses on the available molecular data of BP treatments regarding predictor markers for their clinical drug response. Many clinical clues suggest human genetic backgrounds play major role determining treatment effectiveness. Clinical response to BP treatments seems to be affected by specific genotypes of target genes such as vitamin D receptor (VDR), collagen type 1 (COLIA1) and interleukin-1β (IL1B). In our opinion, this review could offer argument of pharmacological data reanalysis and/or new future health strategies.
Vitamin D receptor gene
That the gene encoding for VDR is the major genetic locus of bone mass has been well established since 1990s (15). The VDR gene is located on the long arm of chromosome 12 (12q12-14) and is composed by 10 exons, the first of which is not transcribed, and 8 introns (16). The 9 coding exons are transcribed into the VDR messenger RNA (mRNA), which in turn is translated into the functional VDR protein.
Nearly 300 polymorphisms of the human VDR gene have been reported (17), and especially in the regulatory region (18), leading to a precise haplotype map of the VDR gene. Several restriction fragment length polymorphisms (RFLPs) in the human VDR locus have been used in population-based studies (19). The respective restriction endonuclease sites have been conventionally indicated with lowercase letter (t, a, b or f, respectively for TaqI, ApaI, BsmI and FokI restriction endonucleases), while uppercase letter (T, A, B or F) indicates the absence of the restriction site. The BsmI and ApaI polymorphisms lie in a VDR untranslated region (intron 8) and probably do not confer any functional diversity per se (19). Similarly, the silent nucleotide substitution in exon 9 that creates the TaqI polymorphism does not affect the amino acid composition of VDR protein (15). Because of their next sites, these VDR 3’end polymorphisms (i.e. BsmI, TaqI and ApaI RFLPs) are in linkage disequilibrium such that A and B alleles are strongly associated with t allele, while a and b alleles with the absence of TaqI restriction site (T allele) (19).
The VDR BsmI genotype has been reported to be involved in the individual response to antiosteoporotic BP drugs, such as ETN (20) and alendronate (ALN) (21, 22). In 1999, Marc et
al. (20) studied 24 late postmenopausal women with osteoporosis during ETN treatment. In their limited series, the lumbar spine BMD increased significantly faster in the BB and Bb groups (7.3% and 7.0%, respectively) compared with the bb group (2.5%) during 1 year of 400 mg/day ETN therapy and 1000 mg/day calcium supplementation (20). The biochemical marker of bone resorption (urinary hydroxyproline excretion) as well as the bone formation marker (serum levels of osteocalcin) decreased during ETN treatment (20).
With respect to VDR genotype, a significantly higher decrease in osteocalcin level was observed in bb as compared with BB subjects (20).
In the Palomba et al. (21) study, the influence on BMD gain due to the VDR BsmI genotype during various antiresorptive treatments was evaluated in 1,100 postmenopausal Caucasian women. In line with two previous uncontrolled prospective studies (22, 23), the effect of 10 mg/day ALN and 60 mg/day raloxifene (RLX) varied according to VDR BsmI genotype (21). The 1-yr administration of ALN and RLX treatments induced a significantly greater improvement in BMD and bone turnover
markers in VDR bb and in VDR BB genotypes, respectively (21). Moreover, VDR Bb heterozygotes had an intermediate percentage change in lumbar BMD, serum osteocalcin and urinary deoxypyridinoline levels, which was not significantly different from that seen in BB and bb homozygotes (21). Furthermore, in VDR bb homozygotes and in Bb heterozygotes, ALN plus hormonal replacement therapy (HRT) (0.625 mg/day conjugated equine estrogens plus 2.5 mg/day medroxyprogesterone acetate) and ALN plus RLX associations induced a greater influence on BMD compared with HRT alone or RLX alone, respectively, but were not more effective than 1-yr ALN alone (21). Finally, in VDR BB homozygotes, ALN plus RLX induced a greater BMD gain than ALN plus HRT or ALN alone or RLX alone (21). From these results, it is conceivable that ALN and HRT, administrated alone or together, have a weak influence in women with the VDR BB genotype (or the linked TT genotype) (22, 24). However, these findings did not support the remarkable BMD response to ALN plus HRT reported in other Caucasian studies (25, 26), being the VDR BB genotype most frequent in Caucasians (27). On the contrary, RLX segregated with a considerable bone gain in the VDR bb genotype while no VDR genotype effect is detected after ALN plus RLX withdrawal (21).
In conclusion, at the moment, there are scarce clinical and experimental data on molecular mechanism by which VDR genotypes may influence the bone gain during BP-based treatments.
Collagen type 1 gene
The collagen type 1 is an important component of bone matrix and previous work has identified a G-T substitution affecting a Sp1 binding site in the transcriptional control region of the COLIA1 gene. Alleles in which a G-base is present at the Sp1 binding are designed S, whereas alleles in which a Tbase is present at this site are designed as the s allelic variant. Clinical studies have shown that T containing s allele is associated with reduced BMD and osteoporotic fracture in several populations (28-32).
The first intron of the COLIA1 gene has been shown to be of importance in the regulation of collagen transcription (33-35) and there is good evidence to suggest that COLIA1 Sp1 alleles
influence gene regulation. A previous study (32) has shown that the S allele has increased binding affinity for the Sp1 protein in gel shift assays as compared with the S allele.
Studies of allele-specific transcription showed an increased abundance of primary RNA transcripts derived from the s allele compared with the S allele in bone samples from Ss heterozygotes. Cultured osteoblasts from Ss heterozygotes also produced increased amounts of collagen α1(1) chain, relative to the α2(1) chain. Finally, the yield strength of bone samples derived from Ss heterozygotes was found to be significantly reduced independently from differences in bone density when compared with bone from SS individuals (32, 33). This findings emphasize the importance of COLIA1 Sp1 alleles as determinant of bone mass and of bone quality.
Though femoral neck BMD has also been found to increase in patients who have been ETN-treated, the response at this sitenis less marked than at the spine (36). The poor response of femoral BMD to ETN has generally been attributed to the lower rate of bone turnover in cortical bone which predominates in the femoral neck (37). Qureshi et al. (38) reported that there is also a significant heterogeneity in response of femoral BMD to ETN (400 mg daily for 14 days), which is related to COLIA1 Sp1 genotype in 52 early postmenopausal women. Though individual with SS genotype (n = 32) responded reasonably well to ETN therapy with a 2.36% increase in femoral BMD after 2 years, those with the osteoporosis-associated Ss or ss (n = 19) genotypes responded poorly, such that BMD fell by–0.62% (38). This difference in response in BMD was observed throughout the treatment period and also during a treatment-free follow-up period of 1 year (38). The genotyperelated differences in response of BMD could not be attributed to confounding factors such as anthropomorphic criteria or baseline BMD since COLIA1 genotype was an independent predictor of femoral BMD response in a multiple regression analysis.
The mechanism by which the COLIA1 Sp1 polymorphism predicts the response of femoral neck BMD, but not spine BMD to etidronate (38) remains unclear and will require further investigation. There is some evidence to suggest that the unfavorable s allele may act as a marker for increased age-related bone loss (31, 39, 40), although this has not been observed in all studies (41). Similarly, the s allele has been associated in some studies with reduced collagen production, as reflected by serum collagen propeptide levels (28) and with increased bone resorption, as reflected by urinary pyridinoline cross link excretion (30), although this has not been observed in other studies (42). In this regard, deoxypyridinoline values were significantly higher at baseline in the SS
genotype compared with the Ss+ss group (38). Values of deoxypyridinoline/ creatinine ratio and of pyridinoline/creatinine ratio fell to a similar extent in both genotypes in response to ETN, so differences in inhibition of bone resorption are unlikely to have been responsible for the differing response between genotypes at the hip (38).
Finally, it is possible that the poor response of femoral BMD in the Ss+ss genotype group may be a reflection of an impaired osteoblastic response or abnormalities in collagen synthesis. In keeping with this hypothesis, recent work has been shown that osteoblasts cultured from patients who carry the s allele produce an abnormally increased ratio of the collagen type 1 α1 chain, relative to the collagen type 1 α2 chain (32).
Whatever the underlying mechanism, the data by Qureshi et al. (38) have potential clinical implications in identifying a subgroup of patients whose femoral BMD response poorly to ETN
therapy. While the results of their study must be treated with caution in view of the limited sample size (n = 52), the consistency of the response during ETN treatment and in the followup phase suggests that the genotype-specific differences in response to femoral BMD is a real phenomenon. If their data can be confirmed by other studies, COLIA1 genotyping may be of clinical value in targeting BP therapy to those most likely to respond, with potential advantages in term of cost and clinical outcome.
Interleukin-1β gene
It is well known that cytokines are involved in the regulation of bone remodeling (43) and are also associated with several bone diseases (44). In particular, interleukin-1β (IL-1β) is a potent osteoclast-activating factor that promotes bone resorption both in vitro and in vivo (45, 46) and is antagonized by IL-1 receptor antagonist (IL-1Ra) (47). Well-estrablished evidence indicates
that osteoclasts are the direct target cells of IL-1 which prolongs the viability of purified osteoclasts (48). In situ hybridization experiments revealed mRNA expression of IL-1 type 1 (IL-1R1) and type 2 receptors (IL-1R2) in murine and rat osteoclasts in normal bone and in inflammatory bone tissues (49). IL-1 increases mature osteoclast survival by inducing the activation of nuclear factor κB (NFκB) (50) and the expression of the receptor activator of NFκB ligand (RANKL) in osteoblasts (51). These results suggest that the direct effect of IL- 1 on osteoclasts is an important mechanism by which IL-1 mediates physiological and pathological bone resorption.
The IL1 gene family is located on chromosome 2q (52) and encodes nine proteins, including IL-1α, IL-1β, IL-1Ra and IL-1R1 which are coded by IL1A, IL1B, IL1RN and IL1R1 gene respectively
(53). IL-1Ra competes with IL-1β for the IL-1R1 receptor, and it is a potent inhibitor of IL-1 activity (54, 55).
Cytokine expression levels are partially associated with genetic polymorphisms located mainly in the promoter and coding sequences of the genes that encode for these proteins. The IL1B gene has at least two biallelic polymorphisms, at positions –511 in the promoter region (56) and +3953 within exon 5 (57) both of which are related to changes in the production of the cytokine (58, 59). Five alleles have been described, corresponding to 2 to 6 copies of the repetitive sequence which forms part of the variable number of tandem repeats (VNTR) located within intron 2 of the IL1RN gene, but only the 4-repeat (IL1RN*1) and the 2-repeat (IL1RN*2) alleles are commonly found. In vitro studies have shown that the IL1RN*2 allele is associated with higher IL1RN production (60, 61), and healthy carriers of the IL1RN*2 allele have significantly higher plasma levels of IL1RN than non-carriers (62). A polymorphism (G to A) in position –1622 in the promoter region of the IL1R1 gene has been described. Individuals that carry the wild-type genotype have higher IL-1R1 plasma levels than those with the mutant genotype (63).
Due to the fact that interleukins are involved in bone remodeling, displays over-expression in osteoclasts and is increased after BP treatment, Corral-Gudino et al. (64) hypothesized that variations in genes of the IL-1 family could be associated with clinical outcome of Paget disease to BP treatments. Interestingly, they found that the –511C/T polymorphism of the IL1B gene is associated with resistance to BP treatments (e.g. ETN, clodronate, tiludronate and risedronate-based) (64). It has been reported that the C/T polymorphism at position –511 in the human IL1B gene is associated with variations in IL-1‚ plasma levels. The allele T has been related to increased serum levels of IL-1β (58, 59). Bearing in mind the pro-resorptive effects of IL-1β, one would expect more severe presentation of Paget disease and poorer response to treatment with higher
levels of IL-1α. Nevertheless, carriers of allele T (n = 96) show a better response to treatment with BPs when compared with homozygous carriers of allele C (n = 69) (64).
The mechanisms underlying resistance to BP-based treatments are poorly understood (65). It is known that resistance to one BP may be followed by response to another BP drug (66, 67). Since IL-1β prolongs the life span of osteoclasts (68), it seems unlikely that the poorer response to BPs observed in homozygous carriers of allele C, that relates to lower levels of IL-1β, could be attributed to a mechanism related to osteoclast apoptosis (69). It is well documented that both BP classes induce macrophage apoptosis and decrease the production of IL-1β (70-72). Thus, we could expect a higher promotion of osteoclast differentiation in carriers of the T allele because of higher levels of IL-1β. In this situation, more osteoclasts are susceptible to BPs, whereas macrophage induced osteoclastogenesis slows down. Therefore, the osteoclast precursor pool would be more efficiently depleted in carriers of the T allele than in carriers of the C allele. However, this hypothesis needs to be confirmed in an appropriate experimental model.
On the other hand, It might be possible that the reported data by (64) were the consequence of linkage disequilibrium between the IL1B locus and another potential locus encoding for a protein involved in BP metabolism. However, polymorphisms in exon 5 of the IL1B gene, intron 2 of the IL1RN gene and promoter region of IL1R1 gene, all located close to IL1B locus, are not associated with response to BP treatment in 165 patients (64), suggesting a direct relationship between IL1B gene polymorphism and response to BP treatment at least in patients with Paget disease.
Although the study limits mainly regarding the small sample size series (64), –511 C/T IL1B polymorphism is proposed as response marker to BP treatment. Thus, –511C/T IL1B polymorphism could be used to select the more convenient BP compound prescribing the more active drug for homozygous carriers of allele C. The above data prompt future pharmacogenetic studies with BPs not only in Paget disease but in other metabolic bone diseases such as osteoporosis.
Conclusions
The potential implication of pharmacogenomics in clinical research and clinical medicine is that disease could be treated according to genetic and specific individual markers, selecting medications and dosages that are optimized for individual patients (“the right drug into the right patient”) (19). The possibility of defining patient populations genetically may improve outcomes by predicting individual responses to drugs, and could improve therapy safety and efficacy. This personalizing of medicines has been the holy grail of pharmacogenomics since sequencing the human genome was conceptualized (73).
The available data suggest that none of the allelic variations in the proposed target genes could completely value the pharmacogenetics of the antiosteoporotic BP drugs. One limitation is represented by the ethnic-dependent allelic distribution of gene loci. Therefore, population analyses should encompass large homogeneous ethnic cohorts. A second level of complexity is represented by the need to analyze simultaneously all the functional gene variants within a individual background. In this regard, the application of genomic technologies such as gene sequencing, statistical genetics and gene expression analysis to drug development, holds great promise for the future of medicine.
Future studies and preventive strategies to management bone disorders need to take in account individual genetic backgrounds.
References
- 1.Von Baeyer H, Hoffmann KS. Acetodiphosphoriga sauer. Ber. 1897;30:1973. [Google Scholar]
- 2.Blaser B, Worms KH. Application of organic acylation products of phosphorus or their derivatives as complexing agents for metal ions. Henkel & Cie G.m.b.H., Germany 1,082,235. 1960 May 25; [Google Scholar]
- 3.Francis MD, Valent DJ. Historical perspectives on the clinical development of bisphosphonates in the treatment of bone diseases. J Musculoskelet Neuronal Interact. 2007;7:2–8. [PubMed] [Google Scholar]
- 4.Storm T, Thamsborg G, Steiniche T, et al. Effect of intermittent cyclical etidronate therapy on bone mass and fracture rate in women with postmenopausal osteoporosis. N Engl J Med. 1990;322:1265–71. doi: 10.1056/NEJM199005033221803. [DOI] [PubMed] [Google Scholar]
- 5.Watts NB, Harris ST, Genant HK, et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med. 1990;323:73–9. doi: 10.1056/NEJM199007123230201. [DOI] [PubMed] [Google Scholar]
- 6.DiMeglio LA. Bisphosphonate therapy for fibrous dysplasia. Pediatr Endocrinol Rev. 2007;4:S440–5. [PubMed] [Google Scholar]
- 7.Major P. Optimal management of metastatic bone disease. Eur J Oncol Nurs. 2007;11:S32–7. doi: 10.1016/j.ejon.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Weisinger JR, Carlini RG, Rojas E, et al. Bone disease after renal transplantation. Clin J Am Soc Nephrol. 2006;1:1300–13. doi: 10.2215/CJN.01510506. [DOI] [PubMed] [Google Scholar]
- 9.Maricic M. New and emerging treatments for osteoporosis. Curr Opin Rheumatol. 2007;19:364–9. doi: 10.1097/BOR.0b013e328172dc1a. [DOI] [PubMed] [Google Scholar]
- 10.Schibler D, Russell RG, Fleisch H. Inhibition by pyrophosphate and polyphosphate of aortic calcification induced by vitamin D3 in rats. Clin Sci. 1968;35:363–72. [PubMed] [Google Scholar]
- 11.Devogelaer JP. reatment of bone diseases with bisphosphonates, excluding osteoporosis. Curr Opin Rheumatol. 2000;12:331–5. doi: 10.1097/00002281-200007000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Das H, Wang L, Kamath A, et al. Vgamma2Vdelta2 T-cell receptor-mediated recognition of aminobisphosphonates. Blood. 2001;98:1616–8. doi: 10.1182/blood.v98.5.1616. [DOI] [PubMed] [Google Scholar]
- 13.Rogers MJ. From molds and macrophages to mevalonate: a decade of progress in understanding the molecular mode of action of bisphosphonates. Calcif Tissue Int. 2004;75:451–61. doi: 10.1007/s00223-004-0024-1. [DOI] [PubMed] [Google Scholar]
- 14.Benford HL, McGowan NW, Helfrich MH, et al. Visualization of bisphosphonate-induced caspase-3 activity in apoptotic osteoclasts in vitro. Bone. 2001;28:465–73. doi: 10.1016/s8756-3282(01)00412-4. [DOI] [PubMed] [Google Scholar]
- 15.Morrison NA, Qi JC, Tokita A, et al. Prediction of bone density from vitamin D receptor alleles. Nature. 1994;367:284–7. doi: 10.1038/367284a0. [DOI] [PubMed] [Google Scholar]
- 16.Haussler MR, Whitfield GK, Haussler CA, et al. The nuclear vitamin D receptor: biological and molecular regulatory properties revealed. J Bone Miner Res. 1998;13:325–49. doi: 10.1359/jbmr.1998.13.3.325. [DOI] [PubMed] [Google Scholar]
- 17.Nejentsev S, Godfrey L, Snook H, et al. Comparative high-resolution analysis of linkage disequilibrium and tag single nucleotide polymorphisms between populations in the vitamin D receptor gene. Hum Mol Genet. 2004;13:1633–9. doi: 10.1093/hmg/ddh169. [DOI] [PubMed] [Google Scholar]
- 18.Fang Y, van Meurs JB, d’Alesio A, et al. Promoter and 3'-untranslated-region haplotypes in the vitamin d receptor gene predispose to osteoporotic fracture: the rotterdam study. Am J Hum Genet. 2005;77:807–23. doi: 10.1086/497438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Massart F, Brandi ML. Bone mass pharmacogenetics and ethnic health implications. Clin Cases Miner Bone Metab. 2007;4:131–138. [PMC free article] [PubMed] [Google Scholar]
- 20.Marc J, Prezelj J, Komel R, et al. VDR genotype and response to etidronate therapy in late postmenopausal women. Osteoporos Int. 1999;10:303–6. doi: 10.1007/s001980050231. [DOI] [PubMed] [Google Scholar]
- 21.Palomba S, Orio F Jr, Russo T, et al. BsmI vitamin D receptor genotypes influence the efficacy of antiresorptive treatments in postmenopausal osteoporotic women. A 1-year multicenter, randomized and controlled trial. Osteoporos Int. 2005;16:943–952. doi: 10.1007/s00198-004-1800-5. [DOI] [PubMed] [Google Scholar]
- 22.Palomba S, Numis FG, Mossetti G, et al. Effectiveness of alendronate treatment in postmenopausal women with osteoporosis: relationship with BsmI vitamin D receptor genotypes. Clin Endocrinol. 2003;58:365–71. doi: 10.1046/j.1365-2265.2003.01724.x. [DOI] [PubMed] [Google Scholar]
- 23.Palomba S, Numis FG, Mossetti G, et al. Raloxifene administration in post-menopausal women with osteoporosis: effect of different BsmI vitamin D receptor genotypes. Hum Reprod. 2003;18:192–8. doi: 10.1093/humrep/deg031. [DOI] [PubMed] [Google Scholar]
- 24.Kurabayashi T, Tomita M, Matsushita H, et al. Association of vitamin D and estrogen receptor gene polymorphism with the effect of hormone replacement therapy on bone mineral density in Japanese women. Am J Obstet Gynecol. 1999;180:1115–20. doi: 10.1016/s0002-9378(99)70603-4. [DOI] [PubMed] [Google Scholar]
- 25.Bone HG, Greenspan SL, McKeever C, et al. Alendronate and estrogen effects in postmenopausal women with low bone mineral density. Alendronate/Estrogen Study Group. J Clin Endocrinol Metab. 2000;85:720–6. doi: 10.1210/jcem.85.2.6393. [DOI] [PubMed] [Google Scholar]
- 26.Johnell O, Scheele WH, Lu Y, et al. Additive effects of raloxifene and alendronate on bone density and biochemical markers of bone remodeling in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2002;87:985–92. doi: 10.1210/jcem.87.3.8325. [DOI] [PubMed] [Google Scholar]
- 27.Massart F. Human races and pharmacogenomics of effective bone treatments. Gynecol Endocr. 2005;20:36–44. doi: 10.1080/09513590400019437. [DOI] [PubMed] [Google Scholar]
- 28.Garnero P, Borel O, Grant SF, et al. Collagen Ialpha1 Sp1 polymorphism, bone mass, and bone turnover in healthy French premenopausal women: the OFELY study. J Bone Miner Res. 1998;13:813–7. doi: 10.1359/jbmr.1998.13.5.813. [DOI] [PubMed] [Google Scholar]
- 29.Grant SF, Reid DM, Blake G, et al. Reduced bone density and osteoporosis associated with a polymorphic Sp1 binding site in the collagen type I alpha 1 gene. Nat Genet. 1996;14:203–5. doi: 10.1038/ng1096-203. [DOI] [PubMed] [Google Scholar]
- 30.Keen RW, Woodford-Richens KL, Grant SF, et al. Association of polymorphism at the type I collagen (COL1A1) locus with reduced bone mineral density, increased fracture risk, and increased collagen turnover. Arthritis Rheum. 1999;42:285–90. doi: 10.1002/1529-0131(199902)42:2<285::AID-ANR10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 31.Uitterlinden AG, Burger H, Huang Q, et al. Relation of alleles of the collagen type Ialpha1 gene to bone density and the risk of osteoporotic fractures in postmenopausal women. N. Engl J Med. 1998;338:1016–21. doi: 10.1056/NEJM199804093381502. [DOI] [PubMed] [Google Scholar]
- 32.Mann V, Hobson EE, Li B, et al. A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by affecting bone density and quality. J Clin Invest. 2001;107:899–907. doi: 10.1172/JCI10347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bornstein P, McKay J, Morishima JK, et al. Regulatory elements in the first intron contribute to transcriptional control of the human alpha 1(I) collagen gene. Proc Natl Acad Sci U S A. 1987;84:8869–73. doi: 10.1073/pnas.84.24.8869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bornstein P, McKay J. The first intron of the alpha 1(I) collagen gene contains several transcriptional regulatory elements. J Biol Chem. 1988;263:1603–6. [PubMed] [Google Scholar]
- 35.Rossouw CM, Vergeer WP, du Plooy SJ, et al. DNA sequences in the first intron of the human pro-alpha 1(I) collagen gene enhance transcription. J Biol Chem. 1987;262:15151–7. [PubMed] [Google Scholar]
- 36.Wimalawansa SJ. Combined therapy with estrogen and etidronate has an additive effect on bone mineral density in the hip and vertebrae: four-year randomized study. Am J Med. 1995;99:36–42. doi: 10.1016/s0002-9343(99)80102-8. [DOI] [PubMed] [Google Scholar]
- 37.Eastell R. Treatment of postmenopausal osteoporosis. N Engl J Med. 1998;338:736–46. doi: 10.1056/NEJM199803123381107. [DOI] [PubMed] [Google Scholar]
- 38.Qureshi AM, Herd RJ, Blake GM, et al. COLIA1 Sp1 polymorphism predicts response of femoral neck bone density to cyclical etidronate therapy. Calcif Tissue Int. 2002;70:158–63. doi: 10.1007/s00223-001-1035-9. [DOI] [PubMed] [Google Scholar]
- 39.Harris SS, Patel MS, Cole DE, et al. Associations of the collagen type Ialpha1 Sp1 polymorphism with five-year rates of bone loss in older adults. Calcif Tissue Int. 2000;66:268–71. doi: 10.1007/pl00005842. [DOI] [PubMed] [Google Scholar]
- 40.MacDonald HM, McGuigan FA, New SA, et al. COL1A1 Sp1 polymorphism predicts perimenopausal and early postmenopausal spinal bone loss. J Bone Miner Res. 2001;16:1634–41. doi: 10.1359/jbmr.2001.16.9.1634. [DOI] [PubMed] [Google Scholar]
- 41.Heegaard A, Jorgensen HL, Vestergaard AW, et al. Lack of influence of collagen type Ialpha1 Sp1 binding site polymorphism on the rate of bone loss in a cohort of postmenopausal danish women followed for 18 years. Calcif Tissue Int. 2000;66:409–13. doi: 10.1007/s002230010083. [DOI] [PubMed] [Google Scholar]
- 42.Langdahl BL, Ralston SH, Grant SF, et al. An Sp1 binding site polymorphism in the COLIA1 gene predicts osteoporotic fractures in both men and women. J Bone Miner Res. 1998;13:1384–9. doi: 10.1359/jbmr.1998.13.9.1384. [DOI] [PubMed] [Google Scholar]
- 43.Rifas L. Bone and cytokines: beyond IL-1, IL-6 and TNF-alpha. Calcif Tissue Int. 1999;64:1–7. doi: 10.1007/s002239900570. [DOI] [PubMed] [Google Scholar]
- 44.Kwan Tat S, Padrines M, Theoleyre S, et al. IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 2004;15:49–60. doi: 10.1016/j.cytogfr.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Gowen M, Wood DD, Ihrie EJ, et al. Aninterleukin 1 like factor stimulates bone resorption in vitro. Nature. 1983;306:378–80. doi: 10.1038/306378a0. [DOI] [PubMed] [Google Scholar]
- 46.Sabatini M, Boyce B, Aufdemorte T, et al. Infusions of recombinant human interleukins 1 and 1 cause hypercalcemia in normal mice. Proc Natl Acad Sci U S A. 1988;85:5235–9. doi: 10.1073/pnas.85.14.5235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guise TA, Garrett IR, Bonewald LF, et al. Interleukin-1 receptor antagonist inhibits the hypercalcemia mediated by interleukin-1. J Bone Miner Res. 1993;8:583–7. doi: 10.1002/jbmr.5650080509. [DOI] [PubMed] [Google Scholar]
- 48.Jimi E, Shuto T, Koga T. Macrophage colony-stimulating factor and interleukin 1 maintain the survival of osteoclast-like cells. Endocrinology. 1995;136:808–11. doi: 10.1210/endo.136.2.7835314. [DOI] [PubMed] [Google Scholar]
- 49.Xu L, Kukita T, Nakano Y, et al. Osteoclasts in normal and adjuvant arthritis bone tissues express the mRNA for both type I and II interleukin-1 receptors. Lab Invest. 1996;75:677–87. [PubMed] [Google Scholar]
- 50.Lacey DL, Tan HL, Lu J, et al. Osteoprotegerin ligand modulates murine osteoclast survival in vitro and in vivo. Am J Pathol. 2000;157:435–8. doi: 10.1016/S0002-9440(10)64556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zaidi M, Blair HC, Moonga BS, et al. Osteoclastogenesis, bone resorption and osteoclast-based therapeutics. J Bone Miner Res. 2003;18:599–609. doi: 10.1359/jbmr.2003.18.4.599. [DOI] [PubMed] [Google Scholar]
- 52.Steinkasserer A, Spurr NK, Cox S, et al. The human IL-1 receptor antagonist gene (IL1RN) maps to chromosome 2q14-q21, in the region of the IL-1-alpha and IL-1-beta loci. Genomics. 1992;13:654–7. doi: 10.1016/0888-7543(92)90137-h. [DOI] [PubMed] [Google Scholar]
- 53.Nicklin MJH, Barton JL, Nguyen M, et al. Sequence-based map of the nine genes of the human interleukin-1 cluster. Genomics. 2002;79:718–25. doi: 10.1006/geno.2002.6751. [DOI] [PubMed] [Google Scholar]
- 54.Dinarello CA. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–147. [PubMed] [Google Scholar]
- 55.Dinarello CA. The role of the interleukin-1-receptor antagonist in blocking inflammation mediated by interleukin-1. N Engl J Med. 2000;343:732–4. doi: 10.1056/NEJM200009073431011. [DOI] [PubMed] [Google Scholar]
- 56.di Giovine FS, Takhsh E, Blakemore AI, et al. Single base polymorphism at –511 in the human interleukin-1β gene (IL1β) Hum Mol Genet. 1992:1–450. doi: 10.1093/hmg/1.6.450. [DOI] [PubMed] [Google Scholar]
- 57.Pociot F, Molvig J, Wogensen L, et al. A Taq I polymorphism in the human interleukin-1β (IL-1β) gene correlates with IL-1β secretion in vitro. Eur J Clin Invest. 1992;22:396–402. doi: 10.1111/j.1365-2362.1992.tb01480.x. [DOI] [PubMed] [Google Scholar]
- 58.Hall SK, Perregaux DG, Gabel CA, et al. Breedveld, Seymour AB Correlation of polymorphic variation in the promoter region of the Interleukin 1β gene with secretion of interleukin 1 proteinβ. Arthritis Rheum. 2004;50:1976–83. doi: 10.1002/art.20310. [DOI] [PubMed] [Google Scholar]
- 59.El-Omar EM, Carrington M, Chow WH, et al. Interleukin 1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402. doi: 10.1038/35006081. [DOI] [PubMed] [Google Scholar]
- 60.Tarlow JL, Blakemore AI, Lennard A, et al. Polymorphism in human IL-1 receptor antagonist gene intron 2 is caused by variable numbers of an 86 bp tandem repeat. Hum Genet. 1993;91:403–4. doi: 10.1007/BF00217368. [DOI] [PubMed] [Google Scholar]
- 61.Danis VA, Millington M, Hyland VJ, et al. Cytokine production by normal human monocytes: inter-subject variation and relationship to an IL-1 receptor antagonist (IL-1Ra) gene polymorphisms. Clin Exp Immunol. 1995;99:303–10. doi: 10.1111/j.1365-2249.1995.tb05549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hurme M, Santtila S. IL-1 receptor antagonist (IL-1Ra) plasma levels are co-ordinately regulated by both IL-1Ra and IL-1beta genes. Eur J Immunol. 1998;28:2598–602. doi: 10.1002/(SICI)1521-4141(199808)28:08<2598::AID-IMMU2598>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 63.Bergholdt R, Larsen ZM, Andersen NA, et al. Characterization of new polymorphisms in the 5’UTR of the human interleukin-1 receptor type 1 (IL1R1) gene: linkage to type 1 diabetes and correlation to IL-1RI plasma level. Genes Immun. 2000;1:495–500. doi: 10.1038/sj.gene.6363719. [DOI] [PubMed] [Google Scholar]
- 64.Corral-Gudino L, del Pino-Montes J, García-Aparicio J, et al. –511 C/T IL1B gene polymorphism is associated to resistance to bisphosphonates treatment in Paget disease of bone. Bone. 2006;38:589–94. doi: 10.1016/j.bone.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 65.Lyles KW. What is “resistance” in Paget’s disease of bone? Arthritis Rheum. 2003;48:2097–9. doi: 10.1002/art.11135. [DOI] [PubMed] [Google Scholar]
- 66.Rendina D, Mossetti G, Viceconti R, et al. Risedronate and pamidronate treatment in the clinical management of patients with severe Paget’s disease of bone and acquired resistance to bisphosphonates. Calcif Tissue Int. 2004;75:189–96. doi: 10.1007/s00223-004-0103-3. [DOI] [PubMed] [Google Scholar]
- 67.Joshua F, Epstein M, Major G. Bisphosphonate resistance in Paget’s disease of bone. Arthritis Rheum. 2003;48:2321–3. doi: 10.1002/art.11136. [DOI] [PubMed] [Google Scholar]
- 68.Lacey DL, Tan HL, Lu J, et al. Osteoprotegerin ligand modulates murine osteoclast survival in vitro and in vivo. Am J Pathol. 2000;157:435–8. doi: 10.1016/S0002-9440(10)64556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wei S, Kitaura H, Zhou P, et al. IL-1 mediates TNFinduce osteoclastogenesis. J Clin Invest. 2005;115:282–90. doi: 10.1172/JCI23394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rogers MJ, Chilton KM, Coxon FP, et al. Bisphosphonates induce apoptosis in mouse macrophage-like cells in vitro by a nitric oxide-independent mechanism. J Bone Miner Res. 1996;11:1482–91. doi: 10.1002/jbmr.5650111015. [DOI] [PubMed] [Google Scholar]
- 71.Matsuda T, Matsui K, Shimakoshi Y, et al. 1-Hydroxyethylidene-1,1-bisphosphonate decreases the postovariectomy enhanced interleukin 1 secretion from peritoneal macrophages in adult rats. Calcif Tissue Int. 1991;49:403–6. doi: 10.1007/BF02555851. [DOI] [PubMed] [Google Scholar]
- 72.Van Beek ER, Lowik CW, Papapoulos SE. Bisphosphonates sup press bone resorption by a direct effect on early osteoclast precursors without affecting the osteoclastogenic capacity of osteogenic cells: the role of protein geranylgeranylation in the action of nitrogen-containing bisphosphonates on osteoclast precursors. Bone. 2002;30:64–70. doi: 10.1016/s8756-3282(01)00655-x. [DOI] [PubMed] [Google Scholar]
- 73.Massart F, Reginster JY, Brandi ML. Genetics of menopause-associated diseases. Maturitas. 2001;40:103–116. doi: 10.1016/s0378-5122(01)00283-3. [DOI] [PubMed] [Google Scholar]