Abstract
OBJECTIVE
In patients with long-standing type 1 diabetes, we investigated whether improved β-cell function can be achieved by combining intensive insulin therapy with agents that may 1) promote β-cell growth and/or limit β-cell apoptosis and 2) weaken the anti–β-cell autoimmunity.
RESEARCH DESIGN AND METHODS
For this study, 20 individuals (mean age 39.5 ± 11.1 years) with long-standing type 1 diabetes (21.3 ± 10.7 years) were enrolled in this prospective open-label crossover trial. After achieving optimal blood glucose control, 16 subjects were randomized to exenatide with or without daclizumab. Endogenous insulin production was determined by repeatedly measuring serum C-peptide.
RESULTS
In 85% of individuals with long-standing type 1 diabetes who were screened for participation in this trial, C-peptide levels ≥0.05 ng/ml (0.02 nmol/l) were found. Residual β-cells responded to physiological (mixed-meal) and pharmacological (arginine) stimuli. During exenatide treatment, patients lost 4.1 ± 2.9 kg body wt and insulin requirements declined significantly (total daily dose on exenatide 0.48 ± 0.11 vs. 0.55 ± 0.13 units · kg−1 · day−1 without exenatide; P = 0.0062). No signs of further activation of the underlying autoimmune disease were observed. Exenatide delayed gastric emptying, suppressed endogenous incretin levels, but did not increase C-peptide secretion.
CONCLUSIONS
In long-standing type 1 diabetes, which remains an active autoimmune disease even decades after its onset, surviving β-cells secrete insulin in a physiologically regulated manner. However, the combination of intensified insulin therapy, exenatide, and daclizumab did not induce improved function of these remaining β-cells.
In the past 2 decades, several lines of research dominated the field of type 1 diabetes: trials to alter the immunological response against β-cells and attempts to develop and replace β-cells. The latter, represented by islet transplantation in the clinical arena, has led to the realization that lasting insulin independence could not be achieved (1), but progress was made by gaining insight into β-cell development (2–4) and immunomodulation. Experimental therapies such as administration of the monoclonal antibody anti-CD3 and the β-cell antigen GAD65 slowed β-cell destruction when administered soon after disease onset (5,6). Currently, however, no therapy is available that results in a complete halt or reversal of β-cell failure.
We initiated this trial in patients with well-controlled long-standing type 1 diabetes who had evidence of endogenous insulin production documented by measurable C-peptide concentrations ≥0.3 ng/ml (0.1 nmol/l). The study participants received exenatide, a glucagon-like peptide (GLP)-1 agonist, to stimulate β-cell recovery and possibly regeneration (7,8); 50% of patients also received daclizumab to diminish the underlying autoimmunity and to curb a potential autoimmune reactivation. β-Cell function was repeatedly assessed by measuring basal and stimulated C-peptide concentrations (9). We speculated that the difference between greater β-cell mass and improved function could be determined by observing the duration of any treatment effect; i.e., if the intervention resulted in increased β-cell mass, improved pancreatic insulin production would be expected to persist beyond the exenatide treatment. Daclizumab was chosen as a mild immunosuppressive agent because of its safety profile and its demonstrated efficacy in other T-cell–mediated autoimmune conditions such as uveitis and multiple sclerosis (10,11).
RESEARCH DESIGN AND METHODS
Individuals with type 1 diabetes who contacted the National Institutes of Health (NIH) recruitment office were asked to complete a questionnaire. At the NIH clinical center, 47 patients were selected for testing and 20 were enrolled (Table 1; Fig. 1). Inclusion criteria were 1) age 18–60 years, 2) C-peptide ≥0.3 ng/ml (0.1 nmol/l) at baseline or after arginine stimulation, 3) positive antibodies (GAD65, ICA-512) and/or a typical history of type 1 diabetes, 4) duration of disease ≥5 years, and 5) BMI 20–30 kg/m2. Exclusion criteria were gastroparesis, diabetic nephropathy, insulin requirement ≥0.8 units · kg−1 · day−1, and hypoglycemia unawareness. To determine reference values, we performed mixed-meal testing in three healthy individuals (all female, mean age 33.3 ± 11.1 years, BMI 21.7 ± 1.8 kg/m2). This study (NCT00064714) was approved by the institutional review board of the National Institute of Diabetes and Digestive and Kidney Diseases. All patients provided written informed consent.
Table 1.
Clinical and immunological characteristics of the 20 enrolled patients at screening
| No. | Sex | BMI (kg/m2) | Duration of disease (years) | A1C (%) | Basal (stim) C-peptide (ng/ml) | Antibodies |
HLA haplotypes |
T-cell reactivity |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICA512 | GAD65 | DRB1 | DQB1 | Toronto (no. of + antigens) | Seattle (no. of + sections) | ||||||
| 1 | F | 24.3 | 10.2 | 7.6 | 0.70 (1.00) | neg | pos | 0301, 1601 | 0201, 0502 | 4 | 0 |
| 2 | F | 27.1 | 22.0 | 6.2 | 0.75 (0.80) | pos | pos | 0404, 0404 * | 0302, 0302 * | 9 | NR |
| 3 | F | 21.0 | 6.3 | 8.4 | 0.75 (1.00) | pos | pos | 0301, 0401 | 0201, 0302 | 9 | 18 |
| 4 | M | 29.1 | 21.0 | 8.0 | 0.93 (1.10) | neg | pos | 0301, 0401 | 0201, 0302 | 4 | NR |
| 5 | F | 30.9 | 16.8 | 6.5 | 0.57 (0.80) | pos | neg | 0401, 0402 | 0302, 0302* | 5 | 12 |
| 6 | M | 23.8 | 38.4 | 7.1 | 0.20 (0.50) | neg | neg | 0301, 0405 | 0201, 0302 | 0 | NR |
| 7 | F | 21.7 | 22.5 | 7.4 | 0.39 (0.60) | neg | neg | 0301, 0301 * | 0201, 0201 * | 3 | 5 |
| 8 | M | 22.6 | 25.6 | 7.5 | 0.58 (0.89) | neg | neg | 0405, 0405* | 0302, 0302* | 10 | 4 |
| 9 | F | 31.2 | 16.8 | 7.1 | 0.44 (0.62) | neg | pos | 0301, 0405 | 0201, 0302 | 10 | 5 |
| 10 | M | 24.7 | 5.9 | 5.9 | 0.63 (0.94) | neg | pos | 0102, 1501 | 0501, 0602 | 6 | NR |
| 11 | M | 24.6 | 24.0 | 7.9 | 0.15 (0.62) | neg | neg | 0404, 1104 | 0302, 0301 | 12 | 9 |
| 12 | M | 29.8 | 36.1 | 5.6 | 0.22 (0.36) | neg | pos | 0301 † , 0401 | 0201, 0302 | 10 | NR |
| 13 | M | 27.1 | 37.1 | 7.0 | 0.76 (1.10) | neg | pos | 0301 † , 0301 † | 0201, 0201 | 11 | 0 |
| 14 | F | 30.0 | 4.1 | 7.0 | 0.60 (0.91) | pos | pos | 0401, 1302 | 0301, 0604 | 11 | NR |
| 15 | M | 27.4 | 12.4 | 6.8 | 1.20 (1.80) | neg | pos | 0301, 1601 | 0201, 0502 | 1 | 14 |
| 16 | F | 27.5 | 30.4 | 8.9 | 0.27 (0.42) | neg | pos | 0401, 0701 | 0202, 0302 | 9 | 0 |
| 17 | F | 20.1 | 33.4 | 8.1 | 0.54 (0.68) | neg | pos | 0301, 0401 | 0201, 0302 | NR | NR |
| 18 | M | 26.1 | 29.8 | 10.2 | 0.62 (0.72) | neg | neg | 0301, 1501 | 0201, 0602 | NR | NR |
| 19 | F | 27.9 | 11.7 | 5.7 | 0.36 (0.56) | pos | pos | 0408, 1104 | 0304, 0603 | NR | NR |
| 20 | F | 22.0 | 21.4 | 6.8 | 0.48 (0.68) | pos | pos | 0101, 0401 | 0302, 0501 | NR | NR |
| 9M/11F | 25.9 ± 3.4 | 21.3 ± 10.7 | 7.3 ± 1.1 | 0.57 (0.81) | 6 of 20 | 14 of 20 | See legend | See legend | 14 of 16 | 7 of 10 | |
Patients 1–16 were randomized to one of four study arms and patients 1–14 completed the trial. Of the patients, 16 of 20 had high-susceptibility HLA haplotypes; 1 had a mixed and 1 a protective haplotype (indicated in bold print).
*Homozygosity is highly likely but could only be proven by family studies, which were not available;
†HLA type could not be differentiated with certainty (0301 vs. 0328); underlined numbers indicate that the haplotype belongs to one of five most susceptible subtypes (25). neg, negative; NR, no results available; pos, positive.
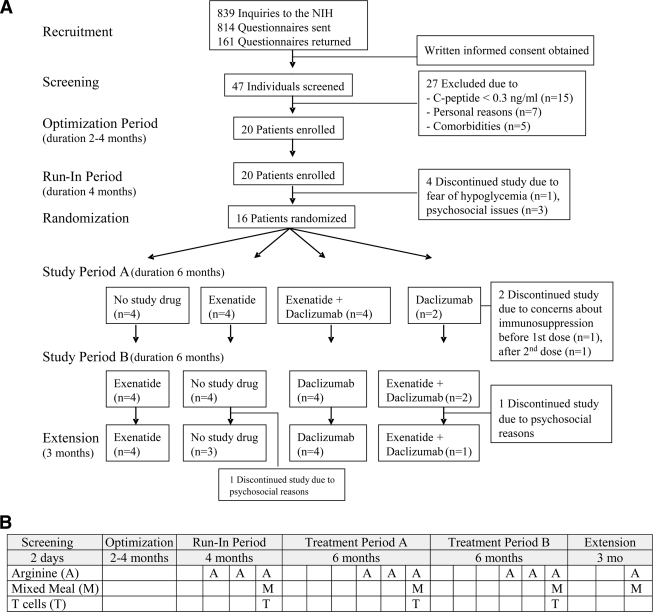
Figure 1.
Study design (A) and timeline for testing procedures (B): 20 patients entered the optimization period, 16 were randomized, and 14 completed the entire trial. B: A, arginine stimulation test; M, mixed-meal test; T, T-cell proliferation test.
Study design
The study followed a prospective randomized open-label crossover design (Fig. 1). It consisted of an optimization period of 2–4 months during which the NIH study team improved the patients' glucose control. Patients then entered the run-in period, a 4-month period during which no major changes in diabetes management were made. At screening and during the run-in period, patients underwent a total of four arginine stimulation tests and two mixed-meal tests to determine baseline C-peptide secretion (Fig. 1B). Thereafter, subjects were randomized to one of four treatment arms (insulin only, insulin plus exenatide, insulin plus exenatide plus daclizumab, or insulin plus daclizumab). After 6 months (period A), patients treated with exenatide discontinued its administration, whereas patients not previously treated with exenatide initiated it. The treatment assignment regarding daclizumab remained unchanged during this second 6-month interval (period B). In both periods A and B, three arginine stimulation tests and one mixed-meal test were performed. Finally, enrollees entered a 3-month extension period, in which they continued the assigned treatment of period B. Special attention was paid to prevent or treat vitamin D deficiency, hyperlipidemia, and hypertension.
Exenatide (Byetta; Amylin, San Diego, CA) was administered subcutaneously via a noncommercial pen that allowed dose adjustments in 2.5-μg increments. Dose and frequency were gradually increased from 2.5 μg twice daily to 10 μg four times daily. At the onset of exenatide therapy, insulin bolus doses were reduced by 50%, whereas basal insulin (for insulin pump users) and long-acting insulin doses (for multiple–daily injection users) remained unchanged. Insulin bolus doses were gradually titrated upward according to blood glucose values. Daclizumab (Zenapax; Roche, Nutley, NJ) was infused intravenously at 2 mg/kg over 30 min once monthly.
Arginine and mixed-meal tests were performed after an overnight fast. With pretest blood glucose levels of ∼150 mg/dl (8.3 nmol/l), two intravenous lines were placed. Baseline blood samples were obtained at −10 and 0 min before intravenous infusion of 5 g arginine (10% solution). Samples were collected from the contralateral cephalic vein at 2, 3, 4, 5, 7, 9, and 10 min and immediately placed on ice until centrifuged at 2,000 rpm for 10 min at 4°C. Samples were then aliquoted and frozen at −20°C.
Mixed-meal tests were performed 30 min after the arginine stimulation tests. Patients assigned to exenatide received medication 15 min prior to testing. Blood samples were obtained at −10, 0, 15, 30, 45, 60, 90, 120, 150, 180, and 240 min. At time point 0 min, patients consumed Boost High Protein (7 ml/kg body wt, maximally 400 ml) in ≤10 min. Blood samples were processed and stored as described above.
Assays
C-peptide was determined with a solid-phase, two-site immunochemiluminescent assay (Esoterix, lower limit of detection 0.05 ng/ml [0.02 nmol/l]). Cross-reactivity with insulin was <0.01% at 100 and 200 μU/ml human insulin. The glucose oxidase method was used for serum glucose measurements. A1C was determined by high-performance liquid chromatography (normal 4.8–6.4%). Glucagon was measured using a double-antibody radioimmunoassay (Esoterix, lower limit of detection 10 pg/ml). Acetaminophen was determined by a particle-enhanced turbidimetric inhibition immunoassay with the analytical range 10–300 μg/ml (lowest detectable dose 2.5 μg/ml). Total GLP-1 was measured with a radioimmunoassay (Millipore, lower limit of detection 3.0 pmol/l).
T-cell assays were performed at three time points (Fig. 1B) in two different laboratories (M. Dosch, Toronto, Canada; and B. Brooks-Worrell and J. Palmer, Seattle, WA) (12). At both sites, T-cell proliferation in response to diabetes-related antigens was determined by direct 3H-thymidine incorporation. Samples were labeled as positive for autoimmunity if the T-cells proliferated to ≥3 (Toronto) or ≥4 (Seattle) of the test antigens compared with responses against unspecific control antigens. The Toronto laboratory used a panel of 12 predefined diabetes-related peptide or protein antigens and included exogenous interleukin-2 in the assay medium. The Seattle laboratory used mixtures of antigen eluted from gel-fractionated human islet cell proteins with 18 size fractions separated by SDS polyacrylamide gel. HLA haplotypes were determined using sequence-specific primers at the Department of Transfusion Medicine at the NIH Clinical Center.
Statistical analyses
Sample size calculations were based on data from 1) NIH patients having undergone islet transplantation with no C-peptide before transplantation but measurable C-peptide after transplantation and 2) data on the variability of individual patient values in periods similar to the run-in period of this study. Sample size estimates were designed to detect a 50% increase of C-peptide levels on exenatide treatment, resulting in a sample size estimate of 12 patients.
Primary outcome measures were based on basal (−10 and 0 min) and stimulated (single highest value during test procedure) C-peptide levels. These were measured monthly before and during arginine stimulation during the last 3 months of each treatment period (Fig. 1B). C-peptide values were averaged across these three time points. Because 50% of patients also received daclizumab, two-way analyses of variance (ANOVAs) were run to assess daclizumab treatment and its possible interaction with exenatide: daclizumab usage was a second factor and the period-sequence by daclizumab interaction term was included. Because the P values for the interaction term were highly nonsignificant (basal P = 0.74; stimulated P = 0.81), as were the P values for the overall effect of daclizumab (basal P = 0.87; stimulated P = 0.84), the daclizumab and no-daclizumab groups were combined in the main analyses of exenatide. To eliminate confounding due to a possible period effect (e.g., due to prolonged intensive insulin treatment), the test based on the two-sample t approach was used (13). Two-sided P values ≤0.05 were considered significant and results were presented as means ± SD if not indicated otherwise.
RESULTS
Patient characteristics are shown in Table 1. The 9 male and 11 female Caucasian patients (mean age 39.5 ± 11.1 years) had type 1 diabetes duration of 21.3 ± 10.7 years. At screening, A1C was 7.3 ± 1.1% (range 5.6–10.2%). Patients used multiple daily injections (MDI, n = 7) or continuous subcutaneous insulin infusions (insulin pump, n = 13). Four patients were antibody negative but had a typical history of type 1 diabetes with childhood onset and/or positive family history and high-risk HLA haplotypes (Table 1). Only patients 10 and 18 had mixed or entirely protective HLA haplotypes, which may explain their presentation at an older age.
C-peptide secretion
Of 47 subjects who underwent detailed screening procedures, 40 completed both arginine stimulation and mixed-meal tests: 55% had measurable C-peptide in both tests, 12.5% only after arginine stimulation, and 17.5% only in the mixed-meal test. Thus, 85% had detectable C-peptide ≥0.05 ng/ml (0.02 nmol/l) in two common stimulation tests.
Once intensified glucose management began (but before introduction of exenatide and daclizumab), 4 patients (patients 17–20) discontinued their participation due to fear of hypoglycemia or psychosocial problems. In the remaining 14 patients, A1C decreased from 7.2 ± 0.9% at screening to 6.5 ± 0.7% at the end of the run-in period (P = 0.0003). The pharmacological (arginine) and physiological (mixed-meal) stimulation of C-peptide was reduced by intensified insulin treatment (Fig. 2A) during the run-in period. All patients secreted less C-peptide compared to their screening results (P < 0.0001 for basal and stimulated C-peptide), and 11 patients (69%) had no detectable C-peptide in their first arginine stimulation test in this study period.
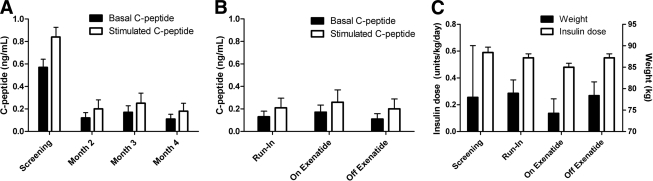
Figure 2.
Results of C-peptide responses to arginine stimulation (A and B) and changes of insulin doses and weight according to treatment assignment (C). C-peptide results are shown at screening (basal versus stimulated C-peptide, P < 0.0001) and during run-in period (tests were conducted in months 2, 3, and 4 of run-in period [basal versus stimulated C-peptide, P = 0.0078]) (A) after 6 months of exenatide therapy versus not having received exenatide (irrespective of assignment to daclizumab) (B) with reference to mean results of run-in period. Data are means ± SEM. To convert C-peptide from conventional (ng/ml) to Si units (nmol/l), multiply by factor 0.333.
C-peptide secretion was insignificantly higher during exenatide treatment, and the addition of daclizumab did not change this outcome (Fig. 2B). Mean basal C-peptide levels were 0.029 ng/ml (0.01 nmol/l) higher on exenatide versus off exenatide (95% CI −0.058 to 0.115 ng/ml, P = 0.48), and stimulated C-peptide levels were 0.024 ng/ml (0.008 nmol/l) higher on exenatide (95% CI −0.090 to 0.138 ng/ml, P = 0.66). Further, there was no difference when analyzing C-peptide secretion depending on the study period when exenatide was administered. These results remained unchanged when taking into account data from the 3-month extension period.
Weight loss, insulin doses, and glucose control
All but one patient (patient 13) lost weight during the 6-month period on exenatide (74.2 ± 12.6 vs. 78.4 ± 12.1 kg on vs. off exenatide, respectively; P = 0.0003). The observed weight loss ranged between 1.1 and 8.8 kg (mean 4.1 ± 2.9 kg). The magnitude of weight loss did not correlate with the frequency of reported nausea. Exenatide was well tolerated, and patients simply described diminished appetite. Glucose control did not change as reflected by similar A1C values (6.51 ± 0.56 vs. 6.64 ± 0.64% on vs. off exenatide, respectively; P = 0.39), but insulin requirements were reduced (total daily dose 0.48 ± 0.11 vs. 0.55 ± 0.13 units · kg−1 · day−1 on vs. off exenatide, respectively; P = 0.0062). This reduction was caused by 30% lower preprandial insulin doses (short-acting insulin doses 0.18 ± 0.05 vs. 0.25 ± 0.09 units · kg−1 · day−1 on vs. off exenatide, respectively; P = 0.0056). Irrespective of exenatide treatment, episodes of hypoglycemia (defined as glucose values <55 mg/dl [3.0 nmol/l]) were rare (1.21 ± 1.72 vs. 0.93 ± 1.21 episodes per week on vs. off exenatide, respectively; P = 0.45).
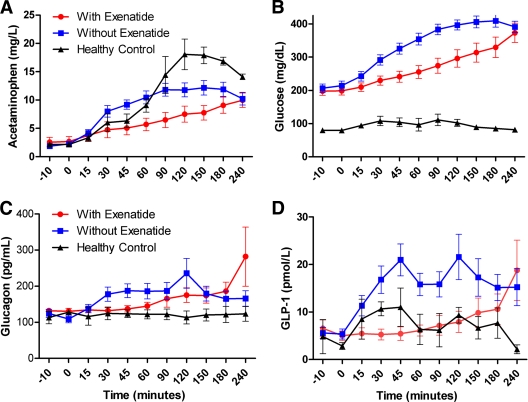
Gastric emptying, glucagon, and GLP-1
Exenatide delayed gastric emptying as determined by acetaminophen absorption (Fig. 3A). Glucose absorption was similarly delayed (Fig. 3B). Fasting glucagon levels remained unchanged whether patients received exenatide or not and were indistinguishable from those of normal control subjects. In contrast to results from patients with type 2 diabetes, meal-stimulated glucagon levels were not suppressed by exenatide, with neither area under the curve nor peak levels being different according to treatment status. In contrast, exenatide suppressed endogenous GLP-1 levels (Fig. 3D).
Figure 3.
Results of mixed-meal testing, conducted according to study timeline (Fig. 1B). Exenatide administered before a mixed meal delayed gastric emptying (A; P = 0.041) and glucose absorption (B; P = 0.052), did not change glucagon levels (C; P = 0.414), and suppressed GLP-1 (D; P = 0.024). P values reflect differences of areas under the curve comparing patients' results on and off exenatide; data are means ± SEM. To convert glucose from conventional (mg/dl) to Si units (nmol/l), multiply by factor 0.0555.
T-cell reactivity
The Toronto laboratory returned complete results for all 44 samples shipped to the laboratory, whereas the Seattle laboratory returned complete results for 28 of 44 samples due to problems with sample viability or high or low background proliferation (Table 1). All subjects tested positive for diabetes-related T-cell autoreactivity in one or both of the assays used at one or more time points. Using the Toronto assay, 13 of 16 subjects were consistently positive, whereas only 1 subject was consistently negative, and that subject tested positive by the Seattle assay. The Seattle assay was more variable, but the majority (16 of 28) of tests was concordant with the Toronto result.
CONCLUSIONS
This clinical trial was based on the observation that some endogenous insulin secretion may persist in long-standing type 1 diabetes (14) and on the assumption that such function might recover (15). Our data and results from other investigators support the notion that residual β-cells either avoid autoimmune-mediated cell death and/or that new β-cells are generated throughout life (16). We were able to document that the surviving β-cells not only contribute a minimal amount of insulin but respond to various stimuli with prompt insulin release.
Several studies suggest that β-cell survival is mostly limited by the ever-vigilant autoimmunity (17). Our results confirmed diabetes-associated T-cell reactivity in almost all subjects even after up to 3 decades of disease duration. Few studies of T-cell autoimmunity have been performed in long-standing diabetes, and in particular there are no blinded controlled studies distinguishing people with diabetes from control subjects. It has been shown that pancreatic-draining lymph nodes harbor many insulin-reactive T-cells in subjects with long-standing type 1 diabetes compared with healthy control subjects (18). Because the T-cell assays in our study were performed at the end of the run-in period, the excellent glucose control may have induced β-cell quiescence, protecting β-cells from immune killing and thereby promoting autoreactive T-cells to traffic out of the pancreatic-draining lymph nodes and into the bloodstream.
Although our present results do not support the original hypothesis that near-normal glycemia, in combination with exenatide and daclizumab, can induce clinically relevant β-cell recovery, it cannot be ruled out that other interventions might. Indeed, plausible explanations exist for our negative findings, including minimal residual β-cell mass associated with advanced patient age and prolonged duration of disease as well as insufficient immunosuppression (19,20). Another factor might have been excellent glucose control because animal studies suggest hyperglycemia may be necessary to promote β-cell proliferation (21). Furthermore, recent studies have questioned exenatide's ability to promote β-cell proliferation (22,23). Although our results are based on data from 14 patients taking exenatide for 6–9 months, it is important to note that this crossover study has the equivalent power to a parallel group study with ≥56 patients (28 patients in each group, intervention and control). Thus, the sample size is small but comparable to other relevant studies in the field. Furthermore, looking at only the possible positive effect of exenatide, our data allow us to claim at a 97.5% level of confidence that the treatment caused ≤0.115 ng/ml improvement in basal C-peptide secretion, which we did not regard as clinically relevant.
At the same time, important knowledge about the natural history of β-cell function was gained. We found that the majority of patients with long-standing type 1 diabetes had surviving β-cells, which promptly responded to standard physiologic and pharmacologic stimuli. Furthermore, exogenous insulin diminished both basal and stimulated C-peptide. This finding highlights the importance of standardizing pretest conditions such as ambient blood glucose and exogenous insulin dosing when evaluating β-cell function.
Of special clinical interest is the exenatide-induced weight loss and reduction in insulin requirements without increased frequency of hypoglycemia. Exenatide suppressed GLP-1 levels and delayed gastric emptying associated with slower glucose absorption. In contrast to the expected suppression of inappropriately elevated glucagon levels (24), we did not see reduced hyperglucagonemia with exenatide. We speculate that this is due to the long-standing abnormal intra-islet cross talk between α- and β-cells.
In conclusion, residual β-cells may play an important role as a potential source of new β-cells in future trials, especially in younger patients and at an earlier stage of the disease. More combination therapies that include immunomodulators with agents that improve β-cell function and growth are needed to expand residual β-cell mass to a degree that individuals with type 1 diabetes may eventually become insulin independent.
Acknowledgments
This research was supported primarily by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the Clinical Center/National Institutes of Health.
A Cooperative Research and Development Agreement was established between NIDDK and Amylin Pharmaceuticals, which provided funding for a research nurse, T-cell assays, and hormone assays performed by Esoterix. No other potential conflicts of interest relevant to this article were reported.
We thank Rebecca J. Brown for her help with manuscript preparation; Patricia Swanson and Terri Wakefield for protocol management; Janet Lee, Pam Costner, and Pamela Brooks for patient care and sample processing; and, most importantly, our patients.
Footnotes
Clinical trial reg. no. NCT00064714, www.clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Hirshberg B, Rother KI, Digon BJ, 3rd, Lee J, Gaglia JL, Hines K, Read EJ, Chang R, Wood BJ, Harlan DM: Benefits and risks of solitary islet transplantation for type 1 diabetes using steroid-sparing immunosuppression: the National Institutes of Health experience. Diabetes Care 2003; 26: 3288– 3295 [DOI] [PubMed] [Google Scholar]
- 2. Dor Y, Brown J, Martinez OI, Melton DA: Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 2004; 429: 41– 46 [DOI] [PubMed] [Google Scholar]
- 3. Teta M, Rankin MM, Long SY, Stein GM, Kushner JA: Growth and regeneration of adult beta cells does not involve specialized progenitors. Dev Cell 2007; 12: 817– 826 [DOI] [PubMed] [Google Scholar]
- 4. Zhou Q, Brown J, Kanarek A, Rajagopal J, Melton DA: In vivo reprogramming of adult pancreatic exocrine cells to beta-cells. Nature 2008; 455: 627– 632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Herold KC, Gitelman SE, Masharani U, Hagopian W, Bisikirska B, Donaldson D, Rother K, Diamond B, Harlan DM, Bluestone JA: A single course of anti-CD3 monoclonal antibody hOKT3γ1(Ala-Ala) results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of type 1 diabetes. Diabetes 2005; 54: 1763– 1769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ludvigsson J, Faresjö M, Hjorth M, Axelsson S, Chéramy M, Pihl M, Vaarala O, Forsander G, Ivarsson S, Johansson C, Lindh A, Nilsson NO, Aman J, Ortqvist E, Zerhouni P, Casas R: GAD treatment and insulin secretion in recent-onset type 1 diabetes. N Engl J Med 2008; 359: 1909– 1920 [DOI] [PubMed] [Google Scholar]
- 7. Xu G, Stoffers DA, Habener JF, Bonner-Weir S: Exendin-4 stimulates both β-cell replication and neogenesis, resulting in increased β-cell mass and improved glucose tolerance in diabetic rats. Diabetes 1999; 48: 2270– 2276 [DOI] [PubMed] [Google Scholar]
- 8. Xue S, Wasserfall CH, Parker M, Brusko TM, McGrail S, McGrail K, Moore M, Campbell-Thompson M, Schatz DA, Atkinson MA, Haller MJ: Exendin-4 therapy in NOD mice with new-onset diabetes increases regulatory T cell frequency. Ann N Y Acad Sci 2008; 1150: 152– 156 [DOI] [PubMed] [Google Scholar]
- 9. Dy EC, Harlan DM, Rother KI: Assessment of islet function following islet and pancreas transplantation. Curr Diab Rep 2006; 6: 316– 322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nussenblatt RB, Peterson JS, Foster CS, Rao NA, See RF, Letko E, Buggage RR: Initial evaluation of subcutaneous daclizumab treatments for noninfectious uveitis: a multicenter noncomparative interventional case series. Ophthalmology 2005; 112: 764– 770 [DOI] [PubMed] [Google Scholar]
- 11. Bielekova B, Richert N, Howard T, Blevins G, Markovic-Plese S, McCartin J, Frank JA, Würfel J, Ohayon J, Waldmann TA, McFarland HF, Martin R: Humanized anti-CD25 (daclizumab) inhibits disease activity in multiple sclerosis patients failing to respond to interferon beta. Proc Natl Acad Sci U S A 2004; 101: 8705– 8708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seyfert-Margolis V, Gisler TD, Asare AL, Wang RS, Dosch HM, Brooks-Worrell B, Eisenbarth GS, Palmer JP, Greenbaum CJ, Gitelman SE, Nepom GT, Bluestone JA, Herold KC: Analysis of T-cell assays to measure autoimmune responses in subjects with type 1 diabetes: results of a blinded controlled study. Diabetes 2006; 55: 2588– 2594 [DOI] [PubMed] [Google Scholar]
- 13. Senn S: Cross-over trials in Statistics in Medicine: the first '25′ years. Stat Med 2006; 25: 3430– 3442 [DOI] [PubMed] [Google Scholar]
- 14. Liu EH, Digon BJ, 3rd, Hirshberg B, Chang R, Wood BJ, Neeman Z, Kam A, Wesley RA, Polly SM, Hofmann RM, Rother KI, Harlan DM: Pancreatic beta cell function persists in many patients with chronic type 1 diabetes, but is not dramatically improved by prolonged immunosuppression and euglycaemia from a beta cell allograft. Diabetologia 2009; 52: 1369– 1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kuroda A, Yamasaki Y, Imagawa A: Beta-cell regeneration in a patient with type 1 diabetes mellitus who was receiving immunosuppressive therapy. Ann Intern Med 2003; 139: W81. [DOI] [PubMed] [Google Scholar]
- 16. Meier JJ, Bhushan A, Butler AE, Rizza RA, Butler PC: Sustained beta cell apoptosis in patients with long-standing type 1 diabetes: indirect evidence for islet regeneration? Diabetologia 2005; 48: 2221– 2228 [DOI] [PubMed] [Google Scholar]
- 17. Sutherland DE, Sibley R, Xu XZ, Michael A, Srikanta AM, Taub F, Najarian J, Goetz FC: Twin-to-twin pancreas transplantation: reversal and reenactment of the pathogenesis of type I diabetes. Trans Assoc Am Physicians 1984; 97: 80– 87 [PubMed] [Google Scholar]
- 18. Kent SC, Chen Y, Bregoli L, Clemmings SM, Kenyon NS, Ricordi C, Hering BJ, Hafler DA: Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature 2005; 435: 224– 228 [DOI] [PubMed] [Google Scholar]
- 19. Meier JJ, Butler AE, Saisho Y, Monchamp T, Galasso R, Bhushan A, Rizza RA, Butler PC: β-Cell replication is the primary mechanism subserving the postnatal expansion of β-cell mass in humans. Diabetes 2008; 57: 1584– 1594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. von Herrath M, Sanda S, Herold K: Type 1 diabetes as a relapsing-remitting disease? Nat Rev Immunol 2007; 7: 988– 994 [DOI] [PubMed] [Google Scholar]
- 21. Alonso LC, Yokoe T, Zhang P, Scott DK, Kim SK, O'Donnell CP, Garcia-Ocaña A: Glucose infusion in mice: a new model to induce β-cell replication. Diabetes 2007; 56: 1792– 1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crutchlow MF, Yu M, Bae YS, Deng S, Stoffers DA: Exendin-4 does not promote Beta-cell proliferation or survival during the early post-islet transplant period in mice. Transplant Proc 2008; 40: 1650– 1657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sherry NA, Chen W, Kushner JA, Glandt M, Tang Q, Tsai S, Santamaria P, Bluestone JA, Brillantes AM, Herold KC: Exendin-4 improves reversal of diabetes in NOD mice treated with anti-CD3 monoclonal antibody by enhancing recovery of beta-cells. Endocrinology 2007; 148: 5136– 5144 [DOI] [PubMed] [Google Scholar]
- 24. Dupré J, Behme MT, McDonald TJ: Exendin-4 normalized postcibal glycemic excursions in type 1 diabetes. J Clin Endocrinol Metab 2004; 89: 3469– 3473 [DOI] [PubMed] [Google Scholar]
- 25. Erlich H, Valdes AM, Noble J, Carlson JA, Varney M, Concannon P, Mychaleckyj JC, Todd JA, Bonella P, Fear AL, Lavant E, Louey A, Moonsamy P. Type 1 Diabetes Genetics Consortium. HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: analysis of the type 1 diabetes genetics consortium families. Diabetes 2008; 57: 1084– 1092 [DOI] [PMC free article] [PubMed] [Google Scholar]