Abstract
Objective
Psychological factors may be important determinants of adherence to antihypertensive medication, since they have been repeatedly found to be associated with an increased risk of hypertension, coronary heart disease and health-damaging behaviours. We examined the importance of several psychological attributes (sense of coherence, optimism, pessimism, hostility, anxiety) with regard to antihypertensive medication adherence assessed by pharmacy refill records.
Methods
A total of 1,021 hypertensive participants, aged 26–63 years, who were employees of 8 towns and 12 hospitals in Finland were included in the analyses.
Results
We found 60% of patients to be totally adherent, 36% partially adherent and 4% totally non-adherent. Multinomial regression analyses revealed high sense of coherence to be associated with lower odds of being totally non-adherent versus being totally adherent (OR = 0.55; 95% 0.31–0.96). This association was independent of factors that influenced adherence to antihypertensive medication, such as sociodemographic characteristics, health-related behaviours, self-reported medical history of doctor-diagnosed co-morbidity, and anteriority of hypertension status. The association was not specific to certain types of antihypertensive drugs.
Conclusions
High sense of coherence may influence antihypertensive medication-adherence behaviour. Aspects characterising this psychological attribute, such as knowledge (comprehensibility), capacity (manageability), and motivation (meaningfulness) may be important determinants of adherence behaviour for asymptomatic illnesses, such as hypertension, in which patients often do not feel or perceive the immediate consequences of skipping medication doses.
Keywords: Adult, Antihypertensive Agents, therapeutic use, Comorbidity, Female, Finland, Humans, Hypertension, drug therapy, psychology, Male, Middle Aged, Odds Ratio, Patient Compliance, psychology, statistics & numerical data, Prospective Studies, Regression Analysis, Treatment Refusal, psychology, statistics & numerical data
Keywords: hypertension, medication adherence, pharmacy refill records, psychological factors
INTRODUCTION
Hypertension is a major risk factor for cardiovascular morbidity and mortality worldwide 1. Despite the availability of effective drugs in high-resource health systems, the adherence to antihypertensive medications remains far from optimal. The World Health Organisation (WHO) estimated the adherence to pharmacotherapy for hypertension to be between 50–70% and identified poor adherence as the main cause of failure to control hypertension 2. According to the WHO definition, adherence is “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes -- corresponds with agreed recommendations from a health care provider”3, 4. Many factors may contribute to adherence and these can be divided into patient-related factors, regimen-related factors, and factors related to the health care provider. 4–7
Among patient factors, psychological factors may be important determinants of adherence to antihypertensive medication, since they have been found repeatedly to be associated with an increased risk of hypertension, 8–10 coronary heart disease and health-related behaviours 11. As adherence describes the extent to which a patient’s behaviour corresponds with medical recommendations, it would be of great public health importance to elucidate the influence of psychological attributes in the dynamics of adherence to antihypertensive medication.
Widely studied psychological factors related to antihypertensive medication adherence include negative emotions (depression) 7, 12, 13 and cognitive variables such as knowledge, attitudes and beliefs towards antihypertensive medication. 12, 14 Little research has been done on the contribution of other potentially important psychological factors known to influence behaviours, such as sense of coherence, optimism, pessimism, hostility and anxiety.15 The aim of the present study is to examine the importance of these psychological attributes with regard to antihypertensive medication adherence assessed by pharmacy refill records among Finnish public sector employees.
METHODS
Study population
The data were from the on-going prospective cohort study of Finnish Public Sector employees, focusing on local government employees of 10 towns and employees in six hospital districts that provide municipal services and public specialized health care in Finland 16, 17. The first questionnaire survey was conducted in 1997–1998 and included measurement of psychological attributes for a sub-cohort comprising the total personnel of 8 towns and 12 hospitals. Of the 16,948 respondents (response rate 70%), 1,021 were hypertensive based on the records from national health registers. They formed the analytical sample for the present study. The ethics committee of the Finnish Institute of Occupational Health approved the study.
Measures
Psychological attributes
Sense of coherence (SOC) was measured using the 13-item short form of Antonovsky’s 18 original 29-item Orientation to Life Questionnaire (OLQ). This version covered all three aspects of SOC, that are meaningfulness, comprehensibility, and manageability (Cronbach α = 0.85). The respondents were asked to check their level of agreement with each of the items on a seven-point semantic differential scale with two anchoring phrases (e.g., 1=never happened, 7=always happened). Examples of the items are as follows: “Most of the things you do in the future will probably be completely fascinating” (an item assessing meaningfulness); “Do you have the feeling that you are in an unfamiliar situation and don’t know what to do?” (comprehensibility); and “How often do you have the feeling that you’re not sure you can keep things under control” (manageability).
Dispositional optimism and pessimism were assessed using a structured survey tool, the revised Life Orientation Test (LOT-R). 19 This measure includes six statements, of which three are worded positively for optimism (Cronbach’s α = 0.65) (e.g., “In uncertain times, I usually expect the best”), and three are worded negatively to indicate pessimism (Cronbach’s α = 0.74) (e.g., “If something can go wrong for me, it will”). The respondents were asked to indicate how well the statements described them in general, as expressed on a scale ranging from 1 (not at all) to 4 (very much so), a slight modification of the standard 5-point response format. A high score referred to high optimism and high pessimism.
Hostility was measured using the Finnish Twin Study Scale of Hostility (Cronbach’s α = 0.68). 20 The items consists of self-ratings of anger responses (do not get angry easily, get angry easily), irritability (get irritated easily, do not get irritated easily), and argumentativeness (seldom get into arguments, prone to get into arguments easily), reflecting the affective and behavioural components of hostility in particular. Responses to the items were on a 7-point Likert-style scale.
Anxiety was measured using six items from the Anxiety-Trait Scale (items 1, 6, 10, 13, 16, and 19). 21 This scale asks respondents to indicate how well statements (eg, “I feel calm” and “I feel upset”) describe them in general, expressed on a scale ranging from 1 (not at all) to 4 (very much so) (Cronbach α = 0.85).
Hostility and anxiety were assessed from the entire study sample but measures of other psychological attributes were available only for the employees in the service of the 8 towns.
Hypertension
Personal identification numbers, a unique number containing birth date and code for sex assigned to all citizens in Finland, were used to link the study participants to their medication records in the National Drug Reimbursement Register and Drug Prescription Register kept by the Social Insurance Institution of Finland. We identified hypertensive participants in need of continuous antihypertensive medication from the Drug Reimbursement Register. It contains information on persons entitled to special reimbursement for antihypertensive medication and the date when special reimbursement was granted. In Finland, the national sickness insurance scheme covers all permanent residents of the country and provides at present basic reimbursement of 42% for all filled prescriptions and special reimbursement of 72% or 100% for many chronic and severe diseases. To the 72% category belong several major diseases, such as hypertension, asthma and coronary heart disease. Patients who apply for special reimbursement must attach a detailed medical certificate prepared by the treating physician, who also provides data to confirm the diagnosis of chronic hypertension. This is further checked by a physician at the Social Insurance Institution who reviews each case history. The diagnostic criteria of qualification for special reimbursement are stricter than the current care guidelines for hypertension: a documentation of repeated blood pressure measurements ≥200 systolic or ≥105 diastolic, or lower figures ≥95 diastolic with signs of complications or cardiovascular co-morbidities, a strong family history for ischemic heart disease, or below 50 years of age in men and below 40 years in women are required. Moreover, in hypertensive patients without signs of complications the entitlement for hypertension may be granted only after six months of continuous and effective pharmacotherapy following a 6-month transition period with lifestyle counselling and monitoring.
The survey was restricted to respondents who were entitled to such a ‘special’ reimbursement during the whole survey year.
Adherence to antihypertensive treatment
Since 1994, all prescriptions reimbursed by the sickness insurance scheme have been included in the Drug Prescription Register of the Social Insurance Institution. This register was searched for drugs coded as C02 (antihypertensives), C03 (diuretics), C07 (beta blocking agents), C08 (calcium channel blockers) or C09 (agents acting on the renin-angiotensin system) as per the WHO Anatomical Therapeutic Chemical Classification with the corresponding Defined Daily Doses (DDDs) (WHO Collaborating Centre for Drug Statistics Methodology, 2004). The Social Insurance Institution obtains these data from all pharmacies in Finland as part of the national drug reimbursement scheme. 22 These records cover the entire study population but exclude hospitalised patients. In this study, adherence was measured by the days covered by filled prescriptions of antihypertensive medication. The rates of filled prescriptions are considered as accurate measures of medical adherence in a closed pharmacy system, such as in Finland, especially when the refills are measured at several points of time. 7 In Finland, all prescriptions are written by a physician and each prescription can cover 100 DDDs or for a maximum use of three months.
Based on defined daily doses, we calculated for each participant the number of days supply of prescribed antihypertensive drugs filled during the survey year (1997–1998). The medication data were obtained for 1,021 participants. A validated method was used to assess exposure to antihypertensive drugs. 23 This consists of using pharmacy records to calculate a proxy duration for the dispensed antihypertensives with an exposure time-window. 23 We combined consecutive and overlapping periods of antihypertensive medication to form periods of treatment and used a maximum of 50-day time-window between refills when combining them into one period of treatment allowing for identification of participants who were recommended only half the DDD.
Then we categorized participants into three groups: total non-adherence (0 day), partial adherence (1 to 364 days), and total adherence (365 days). This classification was preferred due to the distribution of the annual length of the antihypertensive treatment (figure 1).
Figure 1.
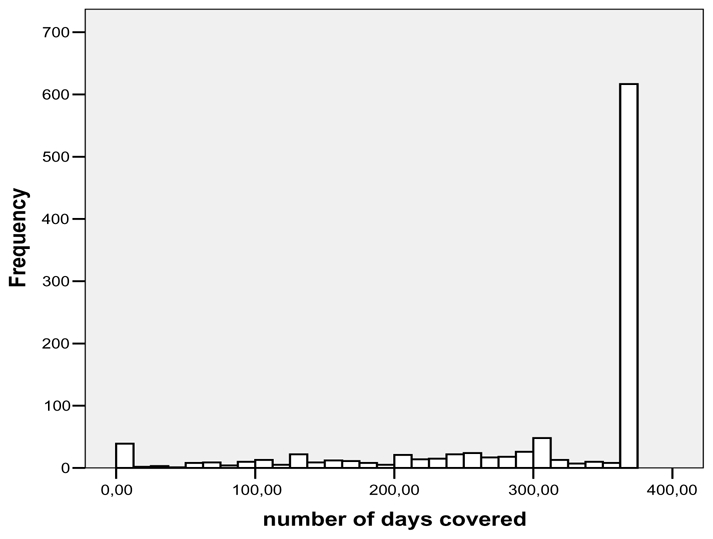
Distribution of the number of treatment days covered with the purchased antihypertensive drugs during the survey year (1997-
Covariates
Covariates used in the present sample were assessed by using survey responses and data from employer’s registers related to the survey year.
Sociodemographic characteristics included gender, age and socioeconomic position (3 categories: upper non-manual workers, lower non-manual workers, and manual workers), marital status (married/cohabitating or other).
Psychological distress was assessed using the 12-item version of the General Health Questionnaire (GHQ-12) (Cronbach α = 0.89), which produces results comparable to the longer versions of the GHQ 24. Individuals scoring ≥4 were identified as those with psychological distress.
Health-related behaviours were assessed by using standard questionnaire measurements on smoking status (current smoker/not) and the habitual frequency and amount of beer, wine, and spirits intake. Responses to the alcohol questions were transformed into grams of alcohol consumed per week. A three-category variable was created to represent heavy drinkers (average weekly consumption ≥210 g of absolute alcohol), light drinkers (average weekly consumption <210 g of absolute alcohol) 25 and non-drinkers (0g). Physical activity was measured by the metabolic equivalent task index 26 and was expressed as the sum score of metabolic equivalent task-hours per day (MET-h\d) and was dichotomised (<2 MET- h/d or >2 MET- h/d. Self-reported weight and height were used to measure body mass index (kg/m2)
Physical and mental morbidity were measured using a self-administered checklist of common chronic conditions and diseases (i.e., rhinopharyngitis, asthma, chronic bronchitis, osteoarthritis, rheumatoid arthritis, fibromyalgia, depression, angina or myocardial infarction, stroke or Transient Ischemic Attack (TIA), sciatica, ulcer, migraine and diabetes) 27. For each disease, the respondent was asked to indicate whether a physician had diagnosed him or her as having the disease.
Statistical analysis
Differences in hypertension status as a function of sample characteristics were assessed using a chi-square test. The relationships between participant’s characteristics and adherence to antihypertensive medication were modelled using multinomial logistic regression. We examined the relationships between psychological attributes and adherence to antihypertensive medications by using multivariate multinomial logistic regression. In model 1, the relationship between each psychological attribute and adherence was adjusted for age and sex. In model 2, significant associations in model 1 were additionally adjusted for smoking and BMI. These were then additionally adjusted for self-reported medical diagnostic of physical co-morbidity (model 3), and for time lag between the hypertension diagnostic and psychological attributes assessment (model 4). Only covariates that were associated with adherence to antihypertensive medication with a p value <0.10 in the bivariate analysis were considered in further multivariate regressions. Model 4 was also used to further examine the association between significant psychological attributes and adherence separately for each type of antihypertensive drug. As some participants were prescribed more than one class of antihypertensive drugs, we additionally adjusted these analyses for the use of other antihypertensive drugs.
RESULTS
Characteristics of the participants are shown in table 1. Among the 1021 hypertensive participants 616 (60%) were totally adherent, 367 (36%) partially adherent and 38 (4%) totally non-adherent (figure 1). The mean annual DDD of antihypertensives was 459.1 corresponding to a mean of 1.25 (SD 0.85) DDDs per day during the survey year.
Table 1.
Sample characteristics (total n =1,021)
| Variables | Hypertension N (%) | p value or for trend | |
|---|---|---|---|
| Sex | Male | 212(36.2) | 0.046 |
| Female | 809 (31.9) | ||
| Age in years | ≤ 40 | 139(17.6) | <0.001 |
| 40–55 | 631(35.4) | ||
| > 55 | 251(45.6) | ||
| Marital status | Married/cohabitating | 798(33.3) | 0.127 |
| Other | 207(30.2) | ||
| Occupational status | Upper non-manual | 222(34.1) | 0.670 |
| Lower non-manual | 515(30.9) | ||
| Manual | 267(35.0) | ||
| Smoking status | No | 873(34.2) | <0.001 |
| Current smoker | 132(25.7) | ||
| Alcohol consumption | Non-drinkers | 160(34.4) | 0.872 |
| Light-drinkers | 764(32.0) | ||
| Heavy-drinkers | 90(36.7) | ||
| BMI | ≤ 19.9 | 17(18.3) | <0.001 |
| 20–24.9 | 277(23.9) | ||
| 25–29.9 | 423(35.6) | ||
| ≥ 30 | 267(45.0) | ||
| Physical activity>2 MET/day | Yes | 284(35.9) | 0.025 |
| No | 723(31.6) | ||
| Psychological distress | No | 740(32.6) | 0.934 |
| Yes | 276(32.7) | ||
| Depression | No | 830(32.0) | 0.241 |
| Yes | 130(35.0) | ||
| Rhinopharyngite | No | 706(35.8) | <0.001 |
| Yes | 272(20.6) | ||
| Asthma | No | 882(36.8) | <0.001 |
| Yes | 81(13.6) | ||
| Chronic bronchitis | No | 825(33.3) | 0.006 |
| Yes | 133(27.0) | ||
| Myocardial infarction | No | 891(31.7) | 0.009 |
| Yes | 68(41.5) | ||
| Stroke | No | 908(32.6) | 0.001 |
| Yes | 44(47.3) | ||
| Osteoarthritis | No | 723(32.3) | 0.024 |
| Yes | 242(35.9) | ||
| Rheumatoid arthritis | No | 926(33.3) | <0.001 |
| Yes | 20(11.8) | ||
| Fibromyalgia | No | 923(32.6) | 0.116 |
| Yes | 28(25.5) | ||
| Prolapsed intervertebral disc | No | 696(32.5) | 0.143 |
| Yes | 261(34.3) | ||
| Ulcer | No | 870(32.) | 0.321 |
| Yes | 83(35.2) | ||
| Migraine | No | 683(31.9) | 0.742 |
| Yes | 288(33.8) | ||
| Diabetes | No | 869(32.0) | 0.742 |
| Yes | 79(33.1) | ||
The associations between covariates and adherence to antihypertensive medications are shown in Table 2. Table 3 presents the association between psychological attributes and adherence to antihypertensive medication. In model 1, when each psychological attribute was simply adjusted for age and sex, sense of coherence (OR = 0.62; 95% CI 0.36 to 1.05) was the only psychological attribute to be associated with lower odds of being totally non-adherent versus being totally adherent. This association persisted (OR = 0.55; 95% 0.31 to 0.96) after serial adjustments for smoking and BMI, self-reported medical diagnosis of physical co-morbidity, and for time lag between the hypertension diagnostic and psychological profiles assessment (models 2 to 4).
Table 2.
Associations between characteristics of hypertensive participants (n=1,021) and adherence
| Odds Ratio (95% CI) |
|||
|---|---|---|---|
| Variables | N | Partial adherence vs. total adherence | Total non adherence vs. total adherence |
| Sex | |||
| Male | 212 | 0.80 (0.58–1.12) | 2.14 (1.08–4.25)† |
| Age in years | |||
| ≤ 40 | 139 | 1.46 (0.95–2.25)* | 2.19 (0.87–5.50)* |
| 40–55 | 631 | 0.92 (0.68–1.25) | 0.69 (0.31–1.52) |
| > 55 | 251 | 1 | 1 |
| Married | |||
| No | 207 | 0.89 (0.64–1.23) | 1.15 (0.53–2.50) |
| Occupational status | |||
| Manual | 222 | 1.05 (0.72–1.52) | 0.67 (0.22–2.05) |
| Lower non-manual | 515 | 0.98 (0.72–1.34) | 1.39 (0.63–3.06) |
| Upper non-manual | 267 | 1 | 1 |
| Smoking status | |||
| Non-smoker | 873 | 1.47 (0.98–2.19)* | 1.99 (0.60–6.61) |
| Alcohol consumption | |||
| Non-drinkers | 160 | 1.15 (0.64–2.05) | 0.57 (0.14–2.38) |
| Light-drinkers | 764 | 1.73 (1.05–2.83)† | 1.06 (0.36–3.10) |
| Heavy-drinkers | 90 | 1 | 1 |
| BMI | |||
| ≤ 19.9 | 17 | 1.84 (0.62–5.47) | 13.95 (2.82–68.87)‡ |
| 20–24.9 | 277 | 1.68 (1.17–2.41)‡ | 3.33 (1.18–9.47)† |
| 25–29.9 | 424 | 1.65 (1.18–2.29)‡ | 2.29 (0.82–6.41) |
| ≥ 30 | 267 | 1 | 1 |
| Physical activity >2 MET/day | |||
| No | 284 | 0.92 (0.69–1.23) | 0.55 (0.24–1.27) |
| Psychological distress | |||
| No | 740 | 0.90 (0.68–1.20) | 1.31 (0.59–2.93) |
| Depression | |||
| No | 830 | 0.92 (0.62–1.35) | 0.78 (0.31–1.92) |
| Rhinopharyngite | |||
| No | 706 | 1.06 (0.79–1.42) | 1.07 (0.50–2.25) |
| Asthma | |||
| No | 882 | 0.72 (0.45–1.15) | 0.91 (0.27–3.09) |
| Bronchitis | |||
| No | 825 | 1.24 (0.83–1.83) | 1.12 (0.42–2.94) |
| Myocardial infarction | |||
| No | 891 | 1.25 (0.74–2.12) | 3.05 (0.41–22.77) |
| Stroke | |||
| No | 908 | 0.95 (0.51–1.77) | - |
| Osteoarthritis | |||
| No | 723 | 0.87 (0.64–1.17) | 5.77 (1.37–24.33)† |
| Rheumatism | |||
| No | 926 | 1.20 (0.45–3.22) | 0.34 (0.08–1.75) |
| Fibromyalgia | |||
| No | 923 | 1.21 (0.54–2.73) | 1.17 (0.15–9.04) |
| Prolapsed intervertebral disc | |||
| No | 693 | 0.99 (0.74–1.34) | 1.98 (0.81–4.82) |
| Ulcer | |||
| No | 870 | 0.84 (0.52–1.34) | 0.73 (0.25–2.14) |
| Migraine | |||
| No | 683 | 0.89 (0.67–1.19) | 2.13 (0.88–5.22)* |
| Diabetes | |||
| No | 869 | 1.95 (1.14–3.33)‡ | 1.99 (0.47–8.51) |
| Hypertension anteriority (years) | |||
| 0–2 | 311 | 2.08 (1.41–3.09)† | 0.10 (0.02–0.45)‡ |
| 2–5 | 222 | 1.43 (0.93–2.20)* | 0.51 (0.21–1.23) |
| 5–10 | 292 | 1.42 (0.95–2.14)* | 0.63 (0.29–1.37) |
| >10 | 196 | 1 | 1 |
p<0.10;
p<0.05;
p<0.01;
P<0.001
Table 3.
Associations between psychological attributes and adherence (n = 518 – 1015)
| Odds Ratio (95% CI) |
|||
|---|---|---|---|
| Psychological attributes | N | Partial adherence vs. total adherence | Total non adherence vs. total adherence |
| Model 1 | |||
| Sense of coherence | 550 | 1.01 (0.81–1.25) | 0.62 (0.36–1.05)* |
| Pessimism | 543 | 1.09 (0.81–1.47) | 1.06 (0.51–2.02) |
| Optimism | 549 | 0.88 (0.66–1.19) | 0.79 (0.38–1.65) |
| Hostility | 1015 | 1.07 (0.96–1.19) | 0.97 (0.74–1.27) |
| Anxiety | 1000 | 1.19 (0.94–1.51) | 0.99 (0.54–1.81) |
| Model 2 | 535 | ||
| Sense of coherence | 0.98 (0.79–1.23) | 0.58 (0.33–1.00)† | |
| Model 3 | 518 | ||
| Sense of coherence | 0.97 (0.77–1.22) | 0.54 (0.31–0.95)† | |
| Model 4 | 518 | ||
| Sense of coherence | 0.97 (0.77–1.23) | 0.55 (0.31–0.96)† | |
p<0.10,
p≤0.05
Model 1: OR per 1unit increase in standardised psychological attribute score adjusted for age and sex
Model 2: model 1 adjusted for smoking, BMI.
Model 3: model 2 adjusted for self-reported medical diagnostic of physical co-morbidity (Osteoarthritis, Migraine, and Diabetes)
Model 4: model 3 adjusted for the time lag between the hypertension diagnostic and psychological attributes assessment
Table 4 presents the fully adjusted model for the association between sense of coherence and adherence by antihypertensive drug class. Similar pattern of associations showing sense of coherence to be associated with lower odds of being totally non-adherent versus being totally adherent were observed for all antihypertensive drugs classes, except for diuretics. However, 95% confidence intervals were wide for all these associations.
Table 4.
Associations between sense of coherence and adherence by antihypertensive drug classes (n=518)
| Odds Ratio (OR, 95% CI) |
||
|---|---|---|
| Outcome | Partial adherence vs. total adherence (reference) | Total non adherence vs. total adherence (reference) |
| Psychological attribute | ||
| Antihypertensives (C02)§ (n** = 6/518) | ||
| Sense of coherence | 0.50 (0.06–4.24) | 0.51 (0.09–2.99) |
| Diuretics (C03)‡ (n = 124/518) | ||
| Sense of coherence | 1.04 (0.66–1.65) | 1.20 (0.82–1.76) |
| Beta blocking agents (C07)‡ (n =252/518) | ||
| Sense of coherence | 1.04 (0.75–1.45) | 0.83 (0.61–1.13) |
| Calcium channel blockers (C08)‡ (n =134/518) | ||
| Sense of coherence | 0.65 (0.45–1.00)† | 0.72 (0.51–1.01)* |
| Agents acting on the renin-angiotensin system (C09)‡ (n = 269/518) | ||
| Sense of coherence | 1.06 (0.78–1.44) | 0.89 (0.66–1.19) |
p<0.10,
p≤0.05
OR per 1unit increase in standardised psychological attribute score adjusted for age, sex (only few participants had pharmacy refill records for this class of drug)
OR per 1unit increase in standardised psychological attribute score adjusted for age, sex, smoking, BMI, self-reported medical diagnostic of physical co-morbidity (Osteoarthritis, Migraine, and Diabetes), time lag between the hypertension diagnostic and psychological attributes assessment and other classes of antihypertensive drugs when one was considered.
Number of participants with pharmacy refill records for specific antihypertensive drug class. Some participants were prescribed more than one class of antihypertensive drugs
DISCUSSION
We examined the independent associations between several psychological attributes and adherence to antihypertensive medication assessed by pharmacy refill records among hypertensive Finnish public sector employees. We found that only about 60% of the patients were totally adherent. High sense of coherence was associated with lower risk of being totally non-adherent. This association was found to be independent of factors that influenced adherence to antihypertensive medication, such as sociodemographic characteristics, health-related behaviours, self-reported medical history of doctor-diagnosed co-morbidity, and anteriority of hypertension status. We found no strong evidence to suggest that this association would be specific to certain types of antihypertensive drug, but the estimation was imprecise due to small numbers.
To our knowledge, this is the first study to depict quantitatively the relationship between several psychological attributes and adherence to antihypertensive medication. We found only one study to have examined previously the association between hostility and antihypertensive medication adherence 15. Results from this multi-centre randomized double-blind study revealed that hypertensive men with high hostility scores were likely to report that they had trouble remembering to take their antihypertensive medications on a daily basis when compared to those with low hostility scores. However, the study assessed adherence by self-reports and hence could not eliminate the possibility that self-reports may be influenced by factors such as social desirability and introduce common method bias as personality was also determined based on self-reports in that study 28.
A strength of the present study is the assessment of adherence using pharmacy refill records of antihypertensive medication rather than self-reported data. It is of great importance to specify whether patients actually filled their prescriptions, as the first step in adherence to a medication is to actually get that medication. 29 Second, we were able to control for a wide range of potential confounders that have been often found to be related to hypertension control 5, including co-morbidity and anteriority of the hypertension status.
The association of SOC with lower non-adherence to antihypertensive medication is consistent with studies that have examined the influence of SOC on medication adherence for other pathologies. For example, a study 30 conducted among 65 participants with type 1 or type 2 diabetes found that SOC was related to better adherence which mediated the effect of SOC on glycemic control. Another study31 conducted among 99 patients undergoing antiretroviral therapy from an outpatient clinic found lower SOC to be related to more missed doses. Medication adherence is an important self-management activity and our results suggest that SOC might reflect a psychological factor underpinning adherence behaviour.
SOC was defined by Antonovsky18 as representing the salutogenic resources available to individuals. These resources, when strong, lead individuals to believe that what happens in life is predictable, and understandable (comprehensibility); that resources are available to help overcome difficulties as they arise (manageability); and that the demands created by exposure to difficulties are seen as challenges and are worthy of engagement (meaningfulness). Hence, persons with high SOC might perceive demands imposed by their hypertensive status as challenges, worthy of engagement, rather than as threats or stressors, and this might facilitate good adaptation to the disease and its treatment. SOC could be associated with better adherence because it may be a protective factor against demoralisation and may alleviate the development of psychological distress in the context of serious illness, such as hypertension.32
In this study, the five main classes of antihypertensive drugs available were: Antihypertensives (ACT-code C02), Diuretics (C03), Beta blocking agents (C07), Calcium channel blockers (C08) and Agents acting on the renin-angiotensin system (C09). The different classes may have distinct side effects and thus could potentially be differently related to psychological attributes. However, our results suggest that high sense of coherence was associated with better adherence in relation to most of the antihypertensive drugs. The results for Diuretics (C03) slightly differed, but small numbers prevent any definite conclusions.
Our findings should be interpreted in light of some limitations. First, although pharmacy refill records are objective measures and collected routinely, they do not represent a measure of whether the participants actually took the medications. It is possible that some of the participants characterized as totally adherent did not actually take their medication despite of filling their prescriptions, leading to overestimation of adherence in this study. Future research with alternative measures of adherence, such as pill counters, would provide an interesting comparison to the present results. Secondly, our sample of public sector employees did not include unemployed individuals and is thus not representative of the general population, which may limit the generalizability of our findings. Third, the SOC scale was included only in the survey for employees in the service of towns but not those working for hospitals; thus we had data only for 53% of the 1, 021 hypertensive participants identified. This limited statistical power in our analysis.
Implications of findings
The prevalence of full adherence to antihypertensive medication measured using pharmacy refill records in our sample of hypertensive patients was about 60% and the prevalence of those who really take their medication might be even lower. This confirms the fact that poor adherence to antihypertensive medication remains a major problem among patients with hypertension.2 Hypertension accounts for a significant cost burden through avoidable hospital admissions, premature deaths, work absenteeism, and reduced productivity. 33
In the WHO report 4 on adherence to long-term therapy, it has been recognized that patient’s behaviour is the critical link between a prescribed regimen and treatment outcome. The most effective regimen will fail if the patient does not take the medication as prescribed or refuses to take it. The relationship between sense of cohort and medication-adherence behaviour observed in this study suggests that knowledge (comprehensibility), capacity (manageability), and motivation (meaningfulness) may be important determinants of adherence behaviour in a context of asymptotic illness in which patients often do not feel or perceive the immediate consequences of skipping medication doses. Our results suggest that global messages on adherence to patients might benefit from emphasis on the importance of adherence (knowledge or comprehensibility), of their ability to achieve it (capacity or manageability), and focus on factors that influence their willingness to take the prescribed antihypertensive drugs (motivation or meaningfulness).
We assessed sense of cohort with a 13-item measure, but a validated brief 6-item scale also exists 34. Although we acknowledge the high workload of clinicians, we believe that a brief assessment of sense of coherence could (in certain cases) provide clinicians with insight into patient behaviour and foster a more directed discussion regarding medication adherence with patients particularly low on sense of coherence. As adherence to medication is behaviour that is self-managed, interventions to promote better adherence to antihypertensive medication might benefit from input from the sense of coherence model because it provides specific aspects (meaningfulness, comprehensibility, manageability) that could be targeted in education programs 31. Therapeutic education programs could be an important strategy to improve adherence by informing patients about hypertension, benefits of the treatment, and serious complications associated with non-adherence and by motivating and encouraging them to adhere to treatment. Education is also needed for self-management since most of the care provided for chronic conditions such as hypertension requires the patients to be involved in their own self care. 35
Acknowledgments
The Finnish Public Sector cohort study is supported by the Academy of Finland (projects 117604, 124271, 124322); The Finnish Work Environment Fund; The Social Insurance Institution of Finland; The Local Government Pensions Institution, Finland; the participating towns and hospitals. AS-M is supported by a “Chaire d’excellence” award from the French Ministry of Research and a “European Young Investigator Award” from the European Science Foundation.
Footnotes
Disclosures: None to declare
References
- 1.Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 2.De Geest S, Sabate E. Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs. 2003;2:323. doi: 10.1016/S1474-5151(03)00091-4. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart PV, Sabate E. Adherence to long-term therapies: evidence for action. J Nurs Scholarsh. 2003;35:207. [PubMed] [Google Scholar]
- 4.Sabatâe E World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. [Google Scholar]
- 5.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–794. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 6.Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens. 1999;12:548–554. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- 7.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 8.Schnall PL, Pieper C, Schwartz JE, Karasek RA, Schlussel Y, Devereux RB, Ganau A, Alderman M, Warren K, Pickering TG. The relationship between ‘job strain,’ workplace diastolic blood pressure, and left ventricular mass index. Results of a case-control study. Jama. 1990;263:1929–1935. [PubMed] [Google Scholar]
- 9.Spiro A, 3rd, Aldwin CM, Ward KD, Mroczek DK. Personality and the incidence of hypertension among older men: longitudinal findings from the Normative Aging Study. Health Psychol. 1995;14:563–569. doi: 10.1037//0278-6133.14.6.563. [DOI] [PubMed] [Google Scholar]
- 10.Steptoe A, Cropley M. Persistent high job demands and reactivity to mental stress predict future ambulatory blood pressure. J Hypertens. 2000;18:581–586. doi: 10.1097/00004872-200018050-00011. [DOI] [PubMed] [Google Scholar]
- 11.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 12.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120:26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 14.Hassan NB, Hasanah CI, Foong K, Naing L, Awang R, Ismail SB, Ishak A, Yaacob LH, Harmy MY, Daud AH, Shaharom MH, Conroy R, Rahman AR. Identification of psychosocial factors of noncompliance in hypertensive patients. J Hum Hypertens. 2006;20:23–29. doi: 10.1038/sj.jhh.1001930. [DOI] [PubMed] [Google Scholar]
- 15.Lee D, Mendes de Leon CF, Jenkins CD, Croog SH, Levine S, Sudilovsky A. Relation of hostility to medication adherence, symptom complaints, and blood pressure reduction in a clinical field trial of antihypertensive medication. J Psychosom Res. 1992;36:181–190. doi: 10.1016/0022-3999(92)90027-y. [DOI] [PubMed] [Google Scholar]
- 16.Vahtera J, Kivimaki M, Pentti J, Linna A, Virtanen M, Virtanen P, Ferrie JE. Organisational downsizing, sickness absence, and mortality: 10-town prospective cohort study. Bmj. 2004;328:555. doi: 10.1136/bmj.37972.496262.0D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kivimaki M, Lawlor DA, Davey Smith G, Kouvonen A, Virtanen M, Elovainio M, Vahtera J. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector study. Am J Public Health. 2007;97:874–879. doi: 10.2105/AJPH.2005.078691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antonovsky A. Unraveling the mystery of health: how people manage stress and stay well. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 19.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 20.Koskenvuo M, Kaprio J, Rose RJ, Kesaniemi A, Sarna S, Heikkila K, Langinvainio H. Hostility as a risk factor for mortality and ischemic heart disease in men. Psychosom Med. 1988;50:330–340. doi: 10.1097/00006842-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Spielberger CD, Gorsuch RL. Manual for the State-Trait Anxiety Inventory (Form Y): (“self-evaluation questionnaire”) Palo Alto, CA: Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- 22.Martikainen T, Pirinen E, Alhava E, Poikolainen E, Paakkonen M, Uusitupa M, Gylling H. Long-term results, late complications and quality of life in a series of adjustable gastric banding. Obes Surg. 2004;14:648–654. doi: 10.1381/096089204323093435. [DOI] [PubMed] [Google Scholar]
- 23.Lau HS, de Boer A, Beuning KS, Porsius A. Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol. 1997;50:619–625. doi: 10.1016/s0895-4356(97)00040-1. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–197. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 25.Kouvonen A, Kivimaki M, Elovainio M, Vaananen AK, De Vogli R, Heponiemi T, Linna A, Pentti J, Vahtera J. Low organisational justice and heavy drinking: a prospective cohort study. Occup Environ Med. 2007 doi: 10.1136/oem.2007.032755. [DOI] [PubMed] [Google Scholar]
- 26.Kujala UM, Kaprio J, Sarna S, Koskenvuo M. Relationship of leisure-time physical activity and mortality: the Finnish twin cohort. Jama. 1998;279:440–444. doi: 10.1001/jama.279.6.440. [DOI] [PubMed] [Google Scholar]
- 27.Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145:762–769. doi: 10.1093/aje/145.8.762. [DOI] [PubMed] [Google Scholar]
- 28.Tsasis P. Adherence assessment to highly active antiretroviral therapy. AIDS Patient Care STDS. 2001;15:109–115. doi: 10.1089/108729101750123544. [DOI] [PubMed] [Google Scholar]
- 29.Matsui D, Joubert GI, Dykxhoorn S, Rieder MJ. Compliance with prescription filling in the pediatric emergency department. Arch Pediatr Adolesc Med. 2000;154:195–198. doi: 10.1001/archpedi.154.2.195. [DOI] [PubMed] [Google Scholar]
- 30.Cohen M, Kanter Y. Relation between sense of coherence and glycemic control in type 1 and type 2 diabetes. Behav Med. 2004;29:175–183. doi: 10.3200/BMED.29.4.175-185. [DOI] [PubMed] [Google Scholar]
- 31.Cederfjall C, Langius-Eklof A, Lidman K, Wredling R. Self-reported adherence to antiretroviral treatment and degree of sense of coherence in a group of HIV-infected patients. AIDS Patient Care STDS. 2002;16:609–616. doi: 10.1089/108729102761882143. [DOI] [PubMed] [Google Scholar]
- 32.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36:725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- 33.Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–1196. doi: 10.1016/j.amjhyper.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Kivimaki M, Feldt T, Vahtera J, Nurmi JE. Sense of coherence and health: evidence from two cross-lagged longitudinal samples. Soc Sci Med. 2000;50:583–597. doi: 10.1016/s0277-9536(99)00326-3. [DOI] [PubMed] [Google Scholar]
- 35.Williams AB. Adherence to HIV regimens: 10 vital lessons. Am J Nurs. 2001;101:37–43. doi: 10.1097/00000446-200106000-00019. quiz 44. [DOI] [PubMed] [Google Scholar]


