Abstract
Introduction
To assess potential metabolic and microcirculatory alterations in critically ill patients, near-infrared spectroscopy (NIRS) has been used, in combination with a vascular occlusion test (VOT), for the non-invasive measurement of tissue oxygen saturation (StO2), oxygen consumption, and microvascular reperfusion and reactivity. The methodologies for assessing StO2 during a VOT, however, are very inconsistent in the literature and, consequently, results vary from study to study, making data comparison difficult and potentially inadequate. Two major aspects concerning the inconsistent methodology are measurement site and probe spacing. To address these issues, we investigated the effects of probe spacing and measurement site using 15 mm and 25 mm probe spacings on the thenar and the forearm in healthy volunteers and quantified baseline, ischemic, reperfusion, and hyperemic VOT-derived StO2 variables.
Methods
StO2 was non-invasively measured in the forearm and thenar in eight healthy volunteers during 3-minute VOTs using two InSpectra tissue spectrometers equipped with a 15 mm probe or a 25 mm probe. VOT-derived StO2 traces were analyzed for base-line, ischemic, reperfusion, and hyperemic parameters. Data were categorized into four groups: 15 mm probe on the forearm (F15 mm), 25 mm probe on the forearm (F25 mm), 15 mm probe on the thenar (T15 mm), and 25 mm probe on the thenar (T25 mm).
Results
Although not apparent at baseline, probe spacing and measurement site significantly influenced VOT-derived StO2 variables. For F15 mm, F25 mm, T15 mm, and T25 mm, StO2 ownslope was -6.4 ± 1.7%/minute, -10.0 ± 3.2%/minute, -12.5 ± 3.0%/minute, and -36.7 ± 4.6%/minute, respectively. StO2 upslope was 105 ± 34%/minute, 158 ± 55%/minute, 226 ± 41%/minute, and 713 ± 101%/minute, and the area under the hyperemic curve was 7.4 ± 3.8%·minute, 10.1 ± 4.9%·minute, 12.6 ± 4.4%·minute, and 21.2 ± 2.7%·minute in these groups, respectively. Furthermore, the StO2 parameters of the hyperemic phase of the VOT, such as the area under the curve, significantly correlated to the minimum StO2 during ischemia.
Conclusions
NIRS measurements in combination with a VOT are measurement site-dependent and probe-dependent. Whether this dependence is anatomy-, physiology-, or perhaps technology-related remains to be elucidated. Our study also indicated that reactive hyperemia depends on the extent of ischemic insult.
Introduction
It is now well established that tissue oxygen utilization and regional microcirculatory oxygen transport properties are severely affected during sepsis and shock [1-9]. To assess and identify these metabolic and microcirculatory alterations non-invasively, near-infrared spectroscopy (NIRS) has recently been applied to measure the behavior of tissue oxygen saturation (StO2). Besides observation of steady-state values, a vascular occlusion test (VOT) has been introduced for the measurement of tissue oxygen consumption and of microvascular reperfusion and reactivity [9-14].
The VOT seems to be sensitive to the progress and outcome of sepsis in critical illness [9,12]. A large number of variables exist in the performance of this maneuver, however, yielding apparently conflicting results and uncertainty as to the significance of the various VOT-derived StO2 parameters [11]. The analysis, interpretation, and understanding of VOT-derived StO2 traces, although being widely employed in septic and trauma patients, is limited, especially for the post-occlusion phase of the VOT. Consequently, identification of which StO2 parameters are most appropriate for scoring (micro)vascular reperfusion and reactivity remains to be determined. Proper characterization of VOT-derived StO2 parameters in health is hence needed to allow translation of results obtained in patients to pathophysiological phenomena.
The main problem with the interpretation of StO2 data in the literature is the diversity of methodologies used for assessing StO2 during a VOT. Results vary from study to study, making data comparison and interpretation difficult and possibly inadequate. Two major aspects regarding the inconsistent methodology are the measurement site and probe spacing (that is, the spatial separation between the illumination and detection fibers of the NIRS probe). The measurement site is important because differences may exist in the sensitivity of muscle groups and/or other anatomical structures to the VOT during health and/or pathophysiological conditions. Probe spacing, on the other hand, will determine the depth of measurement within the respective muscle group. To study the roles of both variables, we performed 3-minute VOTs in healthy volunteers and measured using 15 mm and StO2 25 mm probe spacings on the thenar and the forearm. VOT-derived StO2 traces were quantified for baseline, ischemic, reperfusion, and hyperemic StO2 parameters. We expect these results to provide an essential frame of reference for conducting StO2 measurements in future clinical studies.
Materials and methods
Subjects
The study protocol was approved by the Medical Ethics Committee of the Erasmus Medical Center Rotterdam. Eight healthy volunteers (Table 1) who were not receiving any vaso-active medication were requested to refrain from consuming caffeine-containing beverages prior to the experiments. The subjects were comfortably seated in the experimental room (mean ± standard deviation room temperature was 21 ± 1°C) 1 hour before measurements and were requested not to perform any physical labor (for example, lifting and writing).
Table 1.
Demographic characteristics of the studied subjects
| Demographic characteristic | Mean ± standard deviation |
|---|---|
| Age (years) | 28 ± 6 |
| Gender (%) | |
| Female | 25 |
| Male | 75 |
| Dominant hand (%) | |
| Right | 87.5 |
| Left | 12.5 |
| Weight (kg) | 78 ± 10 |
| Height (cm) | 178 ± 8 |
| Tympanic temperature (°C) | 36.6 ± 0.5 |
| Systolic blood pressure (mmHg) | 112 ± 9 |
| Diastolic blood pressure (mmHg) | 73 ± 7 |
| Mean arterial pressure (mmHg) | 91 ± 8 |
| Heart rate (beats/minute) | 69 ± 8 |
Near-infrared spectroscopy
StO2 was continuously and non-invasively measured using two InSpectra tissue spectrometers (Model 325; Hutchinson Technology, Hutchinson, MN, USA). The spectrometers use reflectance mode probes that have a 1.5 mm optical fiber to illuminate the tissue and a 0.4 mm optical fiber to collect the backscattered light from the tissue. Two types of probes were used for this study: one with 15 mm spacing between the illumination and the collecting optical fibers, and one with 25 mm spacing. Both probes have been used in various studies with varying results [9-12].
The relative optical attenuation of the backscattered light at four wavelengths (680 nm, 720 nm, 760 nm, and 800 nm) is measured to calculate two second-derivative attenuation values, one centered at 720 nm and the other at 760 nm [15]. The ratio of the 720 nm to 760 nm second-derivative values is directly extrapolated to StO2, defined as [HbO2]/([Hb] + [HbO2]), via a calibration table. The calibration table relating StO2 to the second-derivative attenuation ratio is stored permanently within the NIRS device and is common to each device and probe used [15]. The NIRS devices were calibrated before the first measurement in each subject using a light-scatter calibrator.
Vascular occlusion test
One NIRS probe was placed on the skin of the thenar eminence and another NIRS probe was placed on the lateral side of the anterior surface of the forearm for simultaneous measurement of thenar StO2 and forearm StO2 during the VOTs. Both the hand and the forearm were kept at heart level with the palms up. The subjects were instructed not to move their hand or arm, or to change their sitting position during measurements.
Baseline arterial pressure was measured using a manual sphygmomanometer. After a 3-minute stabilization period (baseline measurement), stagnant ischemia was induced for 3 minutes by rapidly inflating a pneumatic cuff (within 5 seconds), placed around the upper arm, to 50 mmHg above systolic blood pressure. The cuff was subsequently deflated (within 1 second) and StO2 measurements were continued up to 5 minutes post ischemia.
StO2 curve characteristics
StO2 data from the two devices were continuously saved (one sample every 3.5 seconds) on two computers and were retrospectively analyzed using InSpectra Analysis V3.3 software (Hutchinson Technology). The VOT-derived StO2 traces were divided into four phases: baseline, ischemia, reperfusion, and hyperemia (Figure 1).
Figure 1.
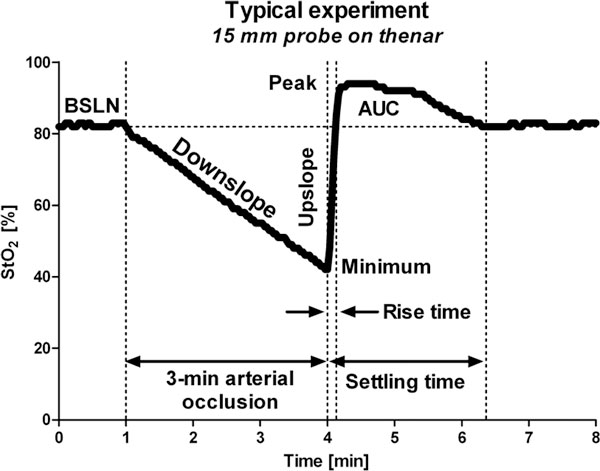
Vascular occlusion test-derived tissue oxygen saturation phases and parameters. The vascular occlusion test-derived tissue oxygen saturation (StO2) traces were divided into four phases (baseline, ischemia, reperfusion, and hyperemia) and were analyzed for baseline StO2 (BSLN), StO2 downslope, minimum StO2, StO2 upslope, rise time, peak StO2, area under the hyperemic curve (AUC), and settling time.
The ischemic phase was analyzed for StO2 downslope (%/minute), minimum StO2 after 3 minutes of ischemia (%), and ΔStO2 (%; that is, the difference between baseline and minimum StO2). The StO2 downslope is generally considered to reflect muscle metabolism and the minimum StO2 is considered to indicate the extent of ischemia.
The reperfusion phase was analyzed for two parameters: upslope (%/minute) and rise time (minutes), both StO2 measured over the interval from minimum StO2 to baseline (Figure 1). Although these parameters are directly StO2 related (StO2 upslope = ΔStO2/Rise time), the StO2 upslope is metabolism-dependent as it is based on ΔStO2 after a fixed time of occlusion (that is, 3 minutes), while the rise time solely represents the time required to wash out the stagnantly deoxygenated blood by oxygenated arterial blood during reperfusion. These two parameters were therefore measured and analyzed separately.
The hyperemic phase of the VOT was analyzed for peak StO2 during reperfusion (%), for StO2 overshoot (that is, difference between peak StO2 and baseline StO2), for the area under the hyperemic curve (AUC; %·minute), and for the settling time from release of the cuff to recovery to baseline StO2 (minutes).
Measurement protocol
Three measurement variables were investigated and compared for the assessment of VOT-derived StO2 parameters: dominant arm versus nondominant arm, forearm versus thenar, and superficial tissue versus deep tissue (as measured by the different probe spacings). For this purpose, four measurements were performed per subject: two on the dominant side and two on the nondominant side. Although good reproducibility of NIRS measurements during sequential VOTs has been demonstrated by Gómez and colleagues [11], the side and probes were switched after every VOT. Additionally, to avoid any effect of starting conditions, the first measurement in four subjects was performed on the dominant side with the 15 mm probe on the forearm and the 25 mm probe on the thenar, whereas in the other four subjects the first measurement was performed on the nondominant side with the 15 mm probe on the thenar and the 25 mm probe on the forearm.
Statistical analysis
First, differences between the dominant arm and the nondominant arm were analyzed and data were subsequently categorized into four groups: 15 mm probe on the forearm (F15 mm), 25 mm probe on the forearm (F25 mm), 15 mm probe on the thenar (T15 mm), and 25 mm probe on the thenar (T25 mm). Statistical analysis was performed in GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Normal distribution of the data within all groups (dominant, nondominant, F15 mm, F25 mm, T15 mm, and T25 mm) was confirmed for each StO2 parameter using the D'Agostino and Pearson omnibus normality test. Comparative analysis between groups was performed using analysis of variance with a Bonferroni post-hoc test. Correlation analysis was performed by Pearson's analysis for normally distributed datasets. All data are presented as the mean ± standard deviation. Differences between groups with P < 0.05 were considered statistically significant.
Results
No differences between the dominant and nondominant sides were found and data could therefore be categorized into four groups: F15 mm, F25 mm, T15 mm, and T25 mm. Baseline StO2 was similar in all groups and independent of probe spacing and measurement site: 81 ± 10% for F15 mm, 85 ± 7% for F25 mm, 87 ± 4% for T15 mm, and 87 ± 3% for T25 mm. Occlusion of the upper arm by a pneumatic cuff resulted in an immediate decrease in StO2. Release of the occlusion after 3 minutes was followed by a rapid increase in StO2 and a StO2 overshoot relative to baseline. Less than 3 minutes post-ischemia, StO2 values were restored to baseline level.
Ischemic phase
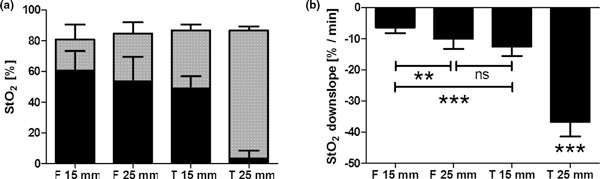
The downslopes during ischemia were measured using linear regression analysis over the linear part (that is, R2 > 0.95) of the StO2 curve. For the first three groups (F15 mm, F25 mm, and T15 mm), the downslopes were linear over the entire 3-minute period of ischemia. The downslopes measured in the T25 mm group, in contrast, were linear over a time interval of 2.34 ± 0.38 minutes. For F15 mm, F25 mm, T15 mm, and T25 mm, StO2 down-slopes were -6.4 ± 1.7%/minute, -10.0 ± 3.2%/minute, -12.5 ± 3.0%/minute, and -36.7 ± 4.6%/minute, respectively (Figure 2). Hence, during 3 minutes of ischemia, StO2 decreased significantly (P < 0.001) by 20 ± 5%, 31 ± 11%, 38 ± 9%, and 84 ± 6% for F15 mm, F25 mm, T15 mm, and T25 mm, respectively, which resulted in a minimum StO2 of 60 ± 13%, 54 ± 16%, 49 ± 8%, and 3 ± 5% in these groups (Figure 2).
Figure 2.
Tissue oxygen saturation at baseline and after ischemia, and the corresponding downslopes. (a) Measured tissue oxygen saturation (StO2) baseline values and minima after 3 minutes of ischemia. (b) Corresponding StO2 downslopes (right). ns = not significant (P > 0.05), **P < 0.01, ***P < 0.001. F, forearm; T, thenar.
For all groups, minimum StO2 values were significantly lower than baseline values (P < 0.001). For the downslopes and ΔStO2 during ischemia, values for F15 mm differed significantly from values for F25 mm (P < 0.01), for T15 mm (P < 0.001), and for T25 mm (P < 0.001). The minimum StO2 was significantly higher in the F15 mm group with respect to T15 mm (P < 0.05) and to T25 mm (P < 0.001). No significant differences between F25 mm and T15 mm were found for these parameters. Downslopes, ΔStO2, measured in the and minimum StO2 T25 mm group were significantly different from those measured in the other groups (P < 0.001).
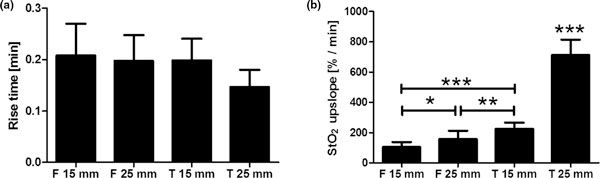
Reperfusion phase
After release of the cuff pressure, StO2 rapidly increased to (and above) baseline StO2. In F15 mm, F25 mm, T15 mm, and T25 mm, StO2 rise times (that is, time from minimum StO2 to baseline StO2) were 0.208 ± 0.062 minutes, 0.198 ± 0.050 minutes, 0.198 ± 0.042 minutes, and 0.147 ± 0.033 minutes, respectively. None of these results were significantly different between groups (Figure 3).
Figure 3.
Measured rise times and the corresponding tissue oxygen saturation upslopes. (a) Measured rise times. (b) Corresponding tissue oxygen saturation (StO2) upslopes. *P < 0.05, **P < 0.01, ***P < 0.001. F, forearm; T, thenar.
In contrast to the rise times, differences between the StO2 upslopes (calculated over the same interval as the rise time) were found between groups due to differences in baselines and minima (StO2 upslope = (StO2 baseline - StO2 minimum)/Rise time). Upslopes were 105 ± 34%/minute, 158 ± 55%/minute, 226 ± 41%/minute, and 713 ± 101%/minute for F15 mm, F25 mm, T15 mm, and T25 mm, respectively. The upslopes in the thenar were significantly higher than the upslopes in the forearm, and the upslopes measured with the 25 mm probe were significantly higher than those measured with the 15 mm probe (Figure 3).
Although the rise time and StO2 upslope both describe (micro)vascular reperfusion following ischemia, apparently these parameters are sensitive to different variables. Hence, where the rise time is similar for the forearm and the thenar and is independent of the applied probe, the StO2 upslope depends significantly on both the muscle and the probe type.
Hyperemic phase
Peak StO2 following release of the upper arm occlusion was 88 ± 7%, 93 ± 5%, 95 ± 3%, and 98 ± 0% for F15 mm, F25 mm, T15 mm, and T25 mm, respectively, Only the peak in the F15 mm group differed significantly from the thenar (P < 0.001 with respect to T15 mm and T25 mm). No significant differences were found for the StO2 overshoot (that is, peak StO2 - Baseline StO2): 6.9 ± 3.8%, 8.6 ± 3.7%, 8.7 ± 3.2%, and 11.3 ± 2.7% for F15 mm, F25 mm, T15 mm, and T25 mm, respectively.
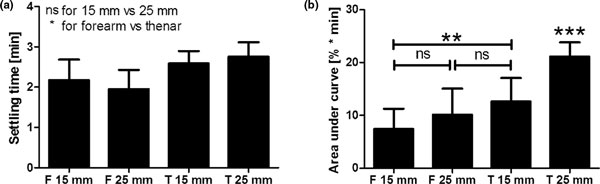
The settling time, defined as the time required for the StO2 to completely restore to baseline (Figure 4), was 2.170 ± 0.511 minutes, 1.950 ± 0.475 minutes, 2.588 ± 0.306 minutes, and 2.755 ± 0.360 minutes for F15 mm, F25 mm, T15 mm, and T25 mm, respectively. No significant differences were found with respect to the probe spacing (that is, F15 mm versus F25 mm (P > 0.05) and T15 mm versus T25 mm (P > 0.05)), but significant differences existed between measurement sites (that is, F15 mm versus T15 mm and T25 mm (P < 0.05), and F25 mm versus T15 mm and T25 mm (P < 0.01)).
Figure 4.
Measured settling times and the corresponding areas under the hyperemic curves. (a) Measured settling times. (b) Corresponding areas under the curves. ns = not significant (P > 0.05), *P < 0.05, **P < 0.01, ***P < 0.001. F, forearm; T, thenar.
The AUC was 7.4 ± 3.8%·minute, 10.1 ± 4.9%·minute, 12.6 ± 4.4%·minute, and 21.2 ± 2.7%·minute for F15 mm, F25 mm, T15 mm, and T25 mm, respectively (Figure 4). No significant differences were found between the 15 mm probe and the 25 mm probe on the forearm. Using the 15 mm probe, the AUC in the thenar was significantly higher (P < 0.01) than in the forearm. AUCs measured in the T25 mm group were significantly higher than those measured in the other groups (P < 0.001).
Correlation analysis
To investigate the relationship between the extent of ischemia and the parameters of reperfusion and hyperemia, StO2 correlation analysis (Pearson's analysis) was performed for minimum StO2 versus reperfusion parameters (StO2 upslope and rise time) and hyperemic parameters (peak StO2, StO2 overshoot, AUC, and settling time) from combined data of F15 mm, F25 mm, and T15 mm. T25 mm data were excluded from the analysis because StO2 downslopes were not linear over the entire 3-minute period of ischemia, which would affect the consistency in the correlation analysis.
StO2 upslope correlated significantly with minimum StO2 (r = 0.81, P < 0.001), while the rise time did not (r = 0.12, P > 0.05). The peak StO2 (r = 0.3, P < 0.05), StO2 overshoot (r = 0.44, P < 0.001), and AUC (r = 0.45, P < 0.01) exhibited a weak positive correlation with minimum StO2, whereas a correlation was absent with respect to settling time (r = 0.16, P > 0.05).
To illustrate why the rise time and StO2 upslope behave differently in relation to the measurement site and probe spacing, two individual measurements are described in detail. One measurement was performed with the 15 mm probe on the forearm and the other with the 15 mm probe on the thenar, both with a baseline StO2 of 88%. The StO2 downslope during ischemia was -8%/minute in the forearm and -16%/minute in the thenar. This resulted in different StO2 minima for the two curves: 64% in the forearm and 40% in the thenar. After release of the occlusion, both curves restored back to their baseline level in 0.233 minutes. The rise times, and thus the reperfusion dynamics, for both curves were therefore equal. The StO2 upslopes, in contrast, were very different: 103%/minute in the forearm and 206%/minute in the thenar. This suggests that the StO2 upslope does not solely reflect post-ischemia reperfusion dynamics, but is also strongly influenced by the extent of StO2 decrease during ischemia.
Discussion
The primary finding of this study was that, although not apparent at baseline, the probe spacing and measurement site significantly influenced VOT-derived StO2 variables. The upslope in the reperfusion phase of the VOT was StO2 shown to depend on the minimum StO2 after 3 minutes of ischemia, while the rise time was not. Furthermore, the StO2 parameters of the hyperemic phase of the VOT were shown to significantly correlate to the minimum StO2 value after 3 minutes of ischemia.
Among the investigations employing a NIRS device identical to the ones used in the present study, some studies have used 15 mm probe spacing [10,11,14] while others have used 25 mm probe spacing [9,12,16-18]. In healthy volunteers, all of these studies - including ours - have shown that baseline StO2 values were similar, independent of the applied probe. The VOT-derived StO2 variables as reported in the literature, however, varied widely between the studies using a 15 mm probe and the studies using a 25 mm probe [9-12,14,16-18]. The values obtained in the present study are comparable to those obtained in the above-referenced studies. In the present study we quantitatively compared the VOT-derived StO2 variables obtained using both probes and confirmed the hypothesis that this difference in StO2 downslopes is indeed caused by the use of different probe spacings. In the thenar, the 15 mm probe provided a longer time interval of linear StO2 decay during ischemia than the 25 mm probe, which could make the estimation of the ischemic insult and muscle metabolism inaccurate and possibly inadequate when using the 25 mm probe.
The potential mechanisms by which the VOT-derived StO2 traces might be different when measured by the 15 mm or 25 mm probes could be anatomy-related, physiology-related, or even technology-related. It is well established that muscle cells consume much more oxygen per unit time compared with skin and adipose tissue. Additionally, if the ischemic stimulus is more extensive in the muscle compared to the more superficial layer of (sub)dermal tissue, the reactive hyperemia is probably also of a larger extent in the deeper, muscular, layer. In this light, the probe dependence, and thus the measurement depth dependence, of the StO2 downslope and hyperemic parameters could therefore be explained by variable relative contributions of (sub)dermal tissue and muscular tissue to the NIRS signal for the different probing depths. Another option that might explain the probe dependence of the StO2 traces, however, is that the number of photons that reach the detection fiber of the NIRS probe decreases with increasing probe spacing, which, in turn, could decrease the accuracy of the StO2 calculation. This could be especially true at low microcirculatory oxygenation, as occurs during ischemia, where the optical absorbance of blood is much higher compared to at high oxygenation. This, however, is purely suggestive and no evidential data are present to support this speculation.
In the present article we provide a frame of reference for comparison of data measured in the thenar and forearm using the 15 mm probe and the 25 mm probe for a very broad spectrum of VOT-derived StO2 parameters; that is, baseline parameters, ischemic parameters, reperfusion parameters, and hyperemic parameters.
An important conceptual issue that is addressed in the present study is the difference between StO2 upslope and the rise time in the reperfusion phase of the VOT. First, it was shown that StO2 upslopes were different between the experimental groups while rise times were similar in these groups. Second, the correlation analysis performed on the minimum StO2 values after 3 minutes of ischemia versus the StO2 upslopes and rise times showed that the StO2 upslope correlated significantly with the minimum StO2 while the rise time did not. From a physiological point of view, the rise time represents the time it takes to wash out (or replace) the stagnantly deoxygenated blood in the measurement volume of the NIRS probe by oxygenated arterial blood. The StO2 upslope, on the other hand, has no single physiological meaning as it is the product of multiple variables, such as the baseline StO2, minimum StO2, and rise time. Hence, the use of rise time seems to be a more representative measure of (micro)vascular reperfusion than StO2 upslope.
Another pertinent result from the correlation analysis was the significant positive correlation between the hyperemic parameters and the minimum StO2, indicating that the extent of hyperemia is related to the extent of ischemia. This suggests that the use of a target or threshold StO2 might be more appropriate for standardization of the hyperemic phase of the VOT. After 3 minutes of ischemia, however, StO2 decreased to a minimum of 60% in the forearm and 49% in the thenar when one uses the 15 mm probe and to 54% in the forearm and 1% in the thenar if one uses the 25 mm probe. The probe type should therefore be taken into account when one uses a defined StO2 threshold value of 30 or 40%. Moreover, the occlusion time might exceed 3 minutes when using the 15 mm probe, which could be uncomfortable for the studied subject.
Conclusively, the data from this study support the hypothesis that the NIRS measurements in combination with a VOT are measurement site-dependent and probe-dependent. The present study showed that the use of upslope is StO2 sensitive to the minimum StO2 after 3 minutes of ischemia and does not solely reflect the (micro)vascular reperfusion rate. Although the rise time seems a better measure for (micro)vascular reperfusion following ischemia, this study could not determine whether the use of the rise time can distinguish healthy (micro)vasculature from nonhealthy (micro)vasculature. Our study also indicated that reactive hyperemia depends on the extent of ischemic insult and supports the use of a target StO2 over the use of a fixed time of occlusion for a metabolism-independent analysis of (micro)vascular reactivity, whereby the type of probe should be taken into account. Whether the observed measurement site dependence and probe dependence is anatomy-related, physiology-related, or perhaps technology-related remains to be elucidated.
Abbreviations
NIRS: near-infrared spectroscopy; StO2: tissue oxygen saturation; VOT: vascular occlusion test.
Competing interests
The NIRS devices were provided by Hutchinson Technologies.
Acknowledgements
This article is part of Critical Care Volume 13 Supplement 5: Tissue oxygenation (StO2) in healthy volunteers and critically-ill patients. The full contents of the supplement are available online at http://ccforum.com/supplements/13/S5. Publication of the supplement has been supported with funding from Hutchinson Technology Inc.
References
- Fink MP. Cytopathic hypoxia. Mitochondrial dysfunction as mechanism contributing to organ dysfunction in sepsis. Crit Care Clin. 2001;17:219–237. doi: 10.1016/S0749-0704(05)70161-5. [DOI] [PubMed] [Google Scholar]
- Boerma EC, Mathura KR, Voort PH van der, Spronk PE, Ince C. Quantifying bedside-derived imaging of microcirculatory abnormalities in septic patients: a prospective validation study. Crit Care. 2005;9:R601–R606. doi: 10.1186/cc3809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ince C, Sinaasappel M. Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med. 1999;27:1369–1377. doi: 10.1097/00003246-199907000-00031. [DOI] [PubMed] [Google Scholar]
- Ince C. The microcirculation is the motor of sepsis. Crit Care. 2005;9(Suppl 4):S13–S19. doi: 10.1186/cc3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL. Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med. 2002;166:98–104. doi: 10.1164/rccm.200109-016OC. [DOI] [PubMed] [Google Scholar]
- Astiz ME, DeGent GE, Lin RY, Rackow EC. Microvascular function and rheologic changes in hyperdynamic sepsis. Crit Care Med. 1995;23:265–271. doi: 10.1097/00003246-199502000-00011. [DOI] [PubMed] [Google Scholar]
- Kirschenbaum LA, Astiz ME, Rackow EC, Saha DC, Lin R. Microvascular response in patients with cardiogenic shock. Crit Care Med. 2000;28:1290–1294. doi: 10.1097/00003246-200005000-00005. [DOI] [PubMed] [Google Scholar]
- Trzeciak S, McCoy JV, Phillip Dellinger R, Arnold RC, Rizzuto M, Abate NL, Shapiro NI, Parrillo JE, Hollenberg SM. Microcirculatory Alterations in Resuscitation and Shock Investigators. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med. 2008;34:2210–2217. doi: 10.1007/s00134-008-1193-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL. The prognostic value of muscle StO2 in septic patients. Intensive Care Med. 2007;33:1549–1556. doi: 10.1007/s00134-007-0739-3. [DOI] [PubMed] [Google Scholar]
- Skarda DE, Mulier KE, Myers DE, Taylor JH, Beilman GJ. Dynamic near-infrared spectroscopy measurements in patients with severe sepsis. Shock. 2007;27:348–353. doi: 10.1097/01.shk.0000239779.25775.e4. [DOI] [PubMed] [Google Scholar]
- Gómez H, Torres A, Polanco P, Kim HK, Zenker S, Puyana JC, Pinsky MR. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O2 saturation response. Intensive Care Med. 2008;34:1600–1607. doi: 10.1007/s00134-008-1145-1. [DOI] [PubMed] [Google Scholar]
- Pareznik R, Knezevic R, Voga G, Podbregar M. Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Med. 2006;32:87–92. doi: 10.1007/s00134-005-2841-8. [DOI] [PubMed] [Google Scholar]
- De Blasi RA, Palmisani S, Alampi D, Mercieri M, Romano R, Collini S, Pinto G. Microvascular dysfunction and skeletal muscle oxygenation assessed by phase-modulation near-infrared spectroscopy in patients with septic shock. Intensive Care Med. 2005;31:1661–1668. doi: 10.1007/s00134-005-2822-y. [DOI] [PubMed] [Google Scholar]
- Doerschug KC, Delsing AS, Schmidt GA, Haynes WG. Impairments in microvascular reactivity are related to organ failure in human sepsis. Am J Physiol Heart Circ Physiol. 2007;293:H1065–H1071. doi: 10.1152/ajpheart.01237.2006. [DOI] [PubMed] [Google Scholar]
- Myers DE, Anderson LD, Seifert RP, Ortner JP, Cooper CE, Beilman GJ, Mowlem JD. Noninvasive method for measuring local hemoglobin oxygen saturation in tissue using wide gap second derivative near-infrared spectroscopy. J Biomed Opt. 2005;10:034017. doi: 10.1117/1.1925250. [DOI] [PubMed] [Google Scholar]
- Strahovnik I, Podbregar M. Measurement of skeletal muscle tissue oxygenation in the critically ill. Signa Vitae. 2008;3:43–50. [Google Scholar]
- Nanas S, Gerovasili V, Dimopoulos S, Pierrakos C, Kourtidou S, Kaldara E, Sarafoglou S, Venetsanakos J, Roussos C, Nanas J, Anastasiou-Nana M. Inotropic agents improve the peripheral microcirculation of patients with end-stage chronic heart failure. J Card Fail. 2008;14:400–406. doi: 10.1016/j.cardfail.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Siafaka A, Angelopoulos E, Kritikos K, Poriazi M, Basios N, Gerovasili V, Andreou A, Roussos C, Nanas S. Acute effects of smoking on skeletal muscle microcirculation monitored by near-infrared spectroscopy. Chest. 2007;131:1479–1485. doi: 10.1378/chest.06-2017. [DOI] [PubMed] [Google Scholar]