Abstract
Dengue virus (DENV) pathogenesis is related to the host responses to viral infection within target cells, and therefore, this study assessed intracellular changes in host proteins following DENV infection. Two-dimensional gel electrophoresis and mass spectrometry identified upregulation of the host endoplasmic reticulum (ER) chaperone GRP78 in K562 cells following DENV infection, in the absence of virus-induced cell death. Upregulation of GRP78 in DENV-infected cells was confirmed by immunostaining and confocal microscopy and by Western blot analysis and was also observed in DENV-infected primary monocyte-derived macrophages, a natural target cell type for DENV infection. GRP78 was upregulated in both DENV antigen-positive and -negative cells in the DENV-infected culture, suggesting a bystander effect, with the highest GRP78 levels coincident with high-level DENV antigen production and infectious-virus release. Transfection of target cells to express GRP78 prior to DENV challenge did not affect subsequent DENV infection, but cleavage of GRP78 with the SubAB toxin, during an established DENV infection, yielded a 10- to 100-fold decrease in infectious-virus release, loss of intracellular DENV particles, and a dramatic decrease in intracellular DENV antigen. However, DENV RNA levels were unchanged, indicating normal DENV RNA replication but altered DENV antigen levels in the absence of GRP78. Thus, GRP78 is upregulated by DENV infection and is necessary for DENV antigen production and/or accumulation. This may be a common requirement for viruses such as flaviviruses that depend heavily on the ER for coordinated protein production and processing.
The pathogenesis of dengue virus (DENV) disease is multifactorial, and many of the clinical manifestations of the disease, including the life-threatening DENV-induced hemorrhage, may be mediated by the host responses to infection. Many studies have defined altered host responses during DENV infection, including activation of T cells (19) and altered levels of circulating factors in patients (13) and altered release of cytokines and chemokines from DENV-infected cells (8). Transcriptome analyses of DENV-infected endothelial cells (23, 45), HepG2 cells (9), circulating patient cells (39), or peripheral blood mononuclear cells from DENV-infected macaque monkeys (37) have identified alterations in transcripts involved in a variety of cellular processes, including the innate immune response, cell signaling, and metabolic processes. A recent study examined proteomic changes in DENV-infected HepG2 cells and identified 17 altered cellular proteins, including 2 proteins for which the changes were confirmed (32). In the current study, we performed a proteomic analysis of changes due to DENV infection in a target cell population that is relevant to a natural DENV infection and in which DENV-induced cytopathic effect (CPE) and the cellular death response are absent. Two-dimensional gel electrophoresis (2DGE) identified upregulation of glucose-regulated protein 78 (GRP78), otherwise known as heat shock protein A5 or the immunoglobulin heavy chain binding protein (BiP), in DENV-infected cells. GRP78 is an endoplasmic reticulum (ER)-associated member of the HSP70 family of chaperone proteins. GRP78 is part of the cell's response to ER stress and is a major regulator of the cell's unfolded-protein response (UPR). Sequestration of GRP78 to unfolded proteins releases three cellular factors, protein kinase-like ER-resident kinase, activating transcription factor 6, and inositol-requiring enzyme 1, which induces a cascade of activation of proteins that can inhibit protein translation and assist protein refolding (2, 18, 41). While GRP78 itself is protective against cell death (35), prolonged and extensive UPR and ER stress can induce CHOP-mediated cell death (2, 18, 41). Induction of the UPR accompanied by GRP78 upregulation and cell death has been described for a number of viruses, including bovine viral diarrhea virus (16), Tula virus (21), West Nile virus (28), and Japanese encephalitis virus (40), the last two of which are flaviviruses related to DENV. With hepatitis C virus (HCV), also a member of the family Flaviviridae and related to DENV, the GRP78 promoter and GRP78 mRNA levels are induced in cells expressing the HCV subgenomic replicon (43) or HCV envelope (22). Additionally, expression of the HCV core protein can induce GRP78 protein, ER stress, and CHOP-mediated apoptosis (1). Recently, GRP78 has been shown to be upregulated in HCV-infected cells in an in vivo mouse model of HCV infection in association with ER stress and hepatocyte apoptosis (17). This study investigated the characteristics of GRP78 upregulation in DENV-infected cells and the potential role that GRP78 may play in a DENV infection model that is not associated with extensive CPE. The results show for the first time that GRP78 is upregulated in DENV-infected cells coincident with high-level intracellular viral-antigen production and infectious-virus release. Knockdown of GRP78 resulted in a dramatic reduction in infectious-DENV production that was mediated by a severe reduction in intracellular DENV antigen accumulation but without altering RNA replication, suggesting that GRP78 may act as a chaperone for viral-protein production during DENV infection. This contrasts with the previously described roles for GRP78 in human cytomegalovirus (HCMV) and rotavirus infections and highlights diversity in viral subversion of host cell proteins.
MATERIALS AND METHODS
Cells and virus stocks.
Vero African Green monkey cells, K562 human erythroleukemic cells, HEK-293 human embryonic kidney cells (293 cells), and primary monocyte-derived macrophages (MDM) generated from peripheral blood mononuclear cells by adherence, as previously described (6), were used for DENV infection studies. The DENV stock was MON601, a laboratory clone of the DENV type 2 strain New Guinea C (10), which was produced from in vitro-transcribed RNA transfected into BHK-21 cells and amplified in C6/36 insect cells and whose titer was determined in Vero cells, as described below.
DENV infection and plaque assay.
Cells were infected at a multiplicity of infection (MOI) of 1 to 5 for 90 min at 37°C, as described previously (34, 46). Control mock infections were performed with an equal volume of heat-inactivated virus (80°C for 20 min). The cell culture supernatants were collected, clarified by centrifugation, and frozen at −80°C prior to plaque assay for infectious DENV. The plaque assay was performed in Vero cells, and levels of infectious virus were quantitated as PFU per milliliter.
Cell lysis and 2DGE.
K562 cells were DENV or mock infected as described above, and at 72 h postinfection (p.i.), total cell lysates were collected in 10 mM Tris-HCl, pH 7.4, 5 mM MgCl2, 0.5% Triton X-100 (vol/vol) (Sigma), 20 μg/ml aprotinin (Sigma), and 1 mM dithiothreitol (DTT) (Sigma). Nucleic acids were digested with 0.2 mg/ml of DNase I and RNase A on ice for 20 min, the mixture was sonicated, and the proteins were precipitated by the addition of 4 volumes of ice-cold acetone. The protein precipitate was collected by centrifugation (13,000 × g; 30 min at 4°C) and dissolved in rehydration buffer (5 M urea, 2 M thiourea, 40 mM DTT, 2% [vol/vol] CHAPS {3-[(3-cholamidopropyl)-dimethylammonio]-1-propanesulfonate}, 2% (vol/vol) SB 3-10 [3-decyldimethylammonio-propanesulfonate] (Fluka), 40 mM Tris base, 0.0002% bromophenol blue, 0.2% [wt/vol] ampholytes 3 to 10 [Bio-Rad]). Samples were clarified by centrifugation (13,000 × g; 15 min at 20°C), and the total protein concentration was determined by RC/DC protein assay (Bio-Rad). The cell lysates were then subjected to isoelectric focusing (IEF) on 11-cm precast immobilized pH gradient (IPG) strips with a pH range of 3 to 10 using a Protean IEF cell (Bio-Rad). Briefly, 0.7 mg protein in 0.185 ml of rehydration solution was used to passively rehydrate each IPG strip overnight. IEF was run using a linear voltage that increased to 8,000 V over 2.5 h. Focusing occurred for 35,000 V/h with a 50-μA per strip current limit, with the temperature maintained at 20°C. After IEF, the IPG strips were subjected to a two-step equilibration, 20 min for each step, in 2% DTT in equilibration buffer (6 M urea, 2% [wt/vol] sodium dodecyl sulfate [SDS], 0.05 M Tris-HCl, pH 8.8, 20% [vol/vol] glycerol) with gentle agitation, followed by incubation in 2.5% iodoacetamide in equilibration buffer. Separation of proteins in the second dimension was performed using 12% precast criterion gels (Bio-Rad), and the gels were stained with Biosafe Coomassie G250 stain (Bio-Rad).
PD-Quest analysis of 2DGE spot patterns.
The stained gels were scanned using a GS-800 densitometer and analyzed using PD-Quest software v7.2 (Bio-Rad). Following spot detection, a match set containing six gels (three independent DENV infections and three mock infections) was analyzed to reproducibly identify up- or downregulated proteins. The spot density was normalized within each gel with respect to the total spot density across all gels. The difference in the mean spot density for individual protein spots was then compared between DENV-infected and mock-infected groups using Student's t test. Protein spots showing a statistically significant (P < 0.05) and >2-fold density difference between DENV-infected and mock-infected samples were identified, excised from the gel, and identified by mass spectrometry (MS).
MS.
Excised protein spots were trypsin digested in gel and subjected to MS using matrix-assisted laser desorption ionization-time of flight MS (Bruker ultraflex III). The spectra and mass lists were exported into BioTools (version 3.0; Bruker Daltonik GmbH) and submitted to the Mascot database search engine (Matrix Science). The MOWSE and probability scores calculated by Mascot were used as the criteria for protein identification.
SDS-PAGE and Western blotting.
Proteins in approximately 5 × 106 cell equivalents of whole-cell lysate were separated by SDS-polyacrylamide gel electrophoresis (PAGE) on a 10% gel with a 29:1 ratio of acrylamide to bis-acrylamide. The proteins were then transferred to polyvinylidene difluoride membranes (GE Healthcare) and subjected to Western blotting with rabbit anti-GRP78 (H-12a) against the C-terminal 525 to 638 amino acids of GRP78 (sc-13968; 1:800 dilution; Santa Cruz Biotechnology). Antibody complexes were detected with goat anti-rabbit immunoglobulin G (IgG)-horseradish peroxidase (HRP) conjugate (Pierce) and chemiluminescence (Pierce; WestDura Extend). Membranes were reprobed with mouse anti-actin (1/1,000 dilution; Chemicon International) and visualized with goat anti-mouse IgG-HRP conjugate (Pierce) and chemiluminescence.
Immunostaining and confocal microscopy for GRP78 and DENV.
Cells were spotted or grown on glass slides, fixed in 1% (vol/vol) cold formaldehyde for 30 min, and stored at −20°C until they were analyzed. The slides were washed in phosphate-buffered saline, permeabilized with 0.05% (vol/vol) Igepal (Sigma), and blocked in 4% (vol/vol) goat serum, 5% (vol/vol) fetal calf serum, 0.4% (wt/vol) bovine serum albumin in Hanks buffered salt solution (Gibco BRL). The cells were stained with mouse anti-DENV, raised against DENV1 to -4 proteins and cross-reacting with a 61-kDa DENV protein (D1 to -11; sc-65659; 1/100; Santa Cruz Biotechnology Inc.) and rabbit anti-GRP78 (as described above; 1/100), with detection of antibody complexes with goat anti-mouse IgG-Alexa 488 or 647 and goat anti-rabbit IgG-Alexa 647 or 488 (Molecular Probes). Nuclei were stained with 5 μg/ml Hoescht stain (Molecular Probes) prior to being mounted (Prolong Gold antifade; Invitrogen). Fluorescence was visualized by laser scanning confocal microscopy (Bio-Rad; Radiance 2100). Negative control assays of mock-infected cells or cells with no primary antibodies added were performed concurrently. All data were analyzed using CAS40 Confocal Assistant version 4.02 and LaserSharp 2000 version 5.2 (Bio-Rad).
Overexpression of GRP78 and DENV infection.
293 cells were transfected with pEFIRES-P-BiP (30) or pEGFP (Clontech) to express GRP78 or an irrelevant protein (green fluorescent protein [GFP]), respectively, using Superfect (Qiagen), following the manufacturers' instructions. At 48 h posttransfection, the cells were infected with DENV (MOI = 3) as described above, and the supernatants were sampled for infectious-virus release and quantitated by plaque assay.
SubAB knockdown of GRP78.
Recombinant SubAB and SubAA272B mutant toxins were produced in Escherichia coli and purified by Ni-nitrilotriacetic acid chromatography, as previously described (31, 42). The 293 cells were either left uninfected, mock infected with heat-inactivated virus, or DENV infected, as described above. At 12 h p.i., the cells were either mock treated or treated with SubAB or SubAA272B mutant toxin at an initial concentration of 100 ng/ml in complete medium, followed by incubation at 37°C for 30 min. The toxin-containing medium was then diluted with complete medium to a final concentration of 25 ng/ml toxin, and incubation at 37°C continued. After 12 h of treatment, the supernatants were harvested for analysis of infectious-virus release (plaque assay; 24 h p.i.), and cells were spotted onto glass slides for immunostaining and confocal analysis of DENV antigens or fixed for transmission electron microscopy (TEM). Cell lysates were collected for Western analysis, and RNA was extracted to quantitate intracellular DENV negative-strand RNA.
Analysis of DENV-infected cells by TEM.
Following infection and treatment as described above, cells were harvested, washed, and fixed in 2% osmium tetroxide (OsO4) for 45 min on a rotator. The samples were then dehydrated by serial increments through ethanol from 70 to 100% (vol/vol) and then treated with propylene oxide prior to being embedded in resin blocks. Ultrathin (90-nm) sections were cut and stained with lead citrate (BDH) and uranyl citrate (BDH) in the presence of sodium hydroxide (ProSciTech), and the sections were viewed using a Phillips CM 100 transmission electron microscope. All data were analyzed using the Universal TEM Imaging Platform Software System.
Quantitation of intracellular DENV negative-strand RNA.
RNA was extracted from cell lysates using a QIAamp Viral RNA Kit (Qiagen), heat denatured, and reverse transcribed at 37°C for 1 h with 20 pmol of DENV-specific primer attached to a 19-mer-long sequence (tag) (33), 10 U Moloney murine leukemia virus reverse transcriptase (RT) (New England Biolabs), 10 U RNase inhibitor, and 0.5 mM of each deoxynucleotide triphosphate (Promega) in 1× Moloney murine leukemia virus buffer (New England Biolabs). Known amounts of in vitro-transcribed DENV negative-strand RNA was reverse transcribed in parallel. The tagged DENV cDNA was then subjected to real-time PCR with Quantitect SYBER Green PCR mix (Qiagen) and 0.5 μM of each primer, tag, and DENV3.2, as previously described (46). The data were analyzed using Rotor-Gene DNA sample analysis system software version 4.6. The real-time RT-PCR was normalized against cyclophilin A mRNA, which was reverse transcribed from total RNA as described above with 0.5 μg oligo(dT)15 (Promega), and real-time PCR was performed using primers cyclophilin (F) and cyclophilin (R), as previously described (46).
RESULTS
DENV infection upregulates GRP78.
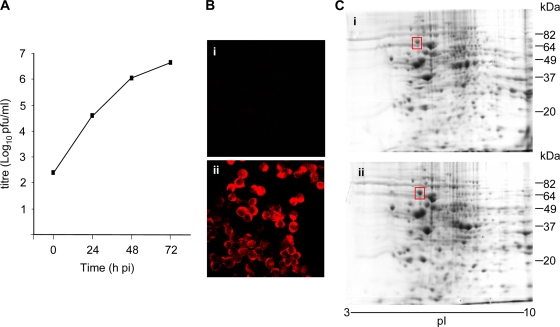
Cells of the monocyte/macrophage lineage are primary sites for DENV infection and replication in vivo (11, 12, 38). However, it is difficult to achieve infection levels higher than 20 to 30% of the total cell population in primary MDM in vitro (5, 34), and thus, we used the Fc receptor-bearing K562 erythroleukemic cell line as a model monocyte-like cell type. Additionally, K562 cells support high levels of DENV infection (20, 25) without associated virus-induced CPE or cell death, and thus, proteomic analysis in this cell type would not include changes in host proteins associated with a cell death response. K562 cells were DENV or mock infected with heat-inactivated virus, and viral replication was monitored by plaque assay, immunostaining, and confocal microscopy. At 72 h p.i., DENV-infected K562 cells produced high levels of infectious virus (Fig. 1A), and 100% of the cell population was DENV antigen positive (Fig. 1B) in the absence of any visible CPE (data not shown). At this time point, the cells were lysed and proteins were separated by 2DGE and visualized by Coomassie blue staining (Fig. 1C). From six member gels, a match set master gel was created using the PD-Quest software (Bio-Rad), and 344 protein spots detected in all gels were used to find reproducible differences between mock- and DENV-infected cells. Using a cutoff value of >2-fold change in spot intensity and a P value of <0.05 (Student's t test) for significance, one protein spot with a mass of approximately 70 kDa and a pI of approximately 6.0 was identified as upregulated (2.4- ± 0.4-fold) in all three DENV-infected cell lysates compared with mock-infected cell lysates (Fig. 1C). This protein spot was excised and subjected to in-gel trypsin digestion and MS. A Mascot database search identified a single highly significant match (MOWSE score:cutoff, 242:54), and MS identified peptides mapping to 52% of the sequence for the human ER chaperone, GRP78. The predicted molecular mass of GRP78 (78 kDa) matched that estimated by 2DGE (Fig. 1C), thus confirming the protein spot identity as GRP78.
FIG. 1.
Proteomic analysis of DENV-infected K562 cells. K562 cells were mock (i) or DENV (ii) infected at an MOI of 5. (A) Supernatant was sampled at the indicated time point p.i. and assayed for infectious-virus release by plaque assay. (B) At 72 h p.i., cells were fixed and immunostained for mouse anti-DENV and visualized with goat anti-mouse Alexa546 and confocal microscopy. (C) At 72 h p.i., cells were lysed, the lysates were subjected to 2DGE, and the proteins were visualized with Coomassie blue staining. The boxed protein spot was upregulated in DENV-infected cell lysates and was identified by MS analysis as GRP78. The results are representative of three independent infections.
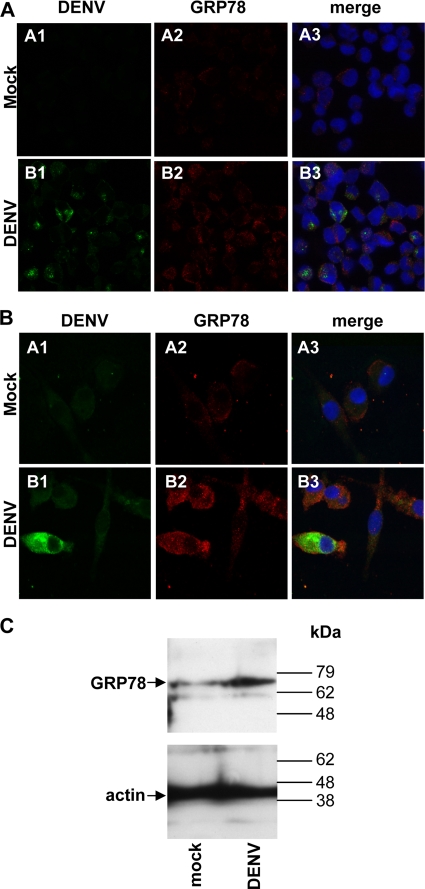
The predicted upregulation of GRP78 in DENV-infected cells was further validated by immunostaining and confocal microscopy. K562 cells or primary MDM, a natural cell target for DENV infection, were DENV or mock infected as described above. At 72 h p.i. for K562 and 48 h p.i. for MDM, infectious-virus release was quantitated at 4 × 106 ± 0.2 × 106 PFU/ml and 4.95 × 105 ± 0.9 × 105 PFU/ml, respectively, and cells were analyzed for DENV antigens and GRP78. Upregulation of GRP78 was seen in DENV-infected but not in mock-infected K562 cells (Fig. 2A) and MDM (Fig. 2B). Notably, upregulation of GRP78 was observed in both DENV antigen-positive and antigen-negative cells of the DENV-challenged population (Fig. 2A and B), suggesting induction of GRP78 via a bystander effect. Cell lysates from DENV-infected K562 cells were also subjected to SDS-PAGE and Western blotting for GRP78. The results again confirmed upregulation of GRP78 in DENV-infected compared with mock-infected cell lysates (Fig. 2C), estimated to be on the order of two- to threefold, consistent with that determined from the above-mentioned proteomic analysis.
FIG. 2.
GRP78 is upregulated in DENV-infected K562 cells and MDM. (A) K562 cells were mock or DENV infected at an MOI of 3, and at 72 h p.i., the cells were fixed and immunostained for mouse anti-DENV and anti-mouse Alexa488 (column 1) or rabbit anti-GRP78 and goat anti-rabbit Alexa647 (column 2), and images were collected by confocal microscopy. (B) MDM were generated from peripheral blood mononuclear cells derived from healthy donor blood by adherence and mock or DENV infected at an MOI of 1, and at 48 h p.i., the cells were fixed and immunostained as for panel A. (C) K562 cells were infected as for panel A, and at 72 h p.i., the cells were lysed and subjected to one-dimensional SDS-PAGE and Western analysis with rabbit anti-GRP78 with detection of complexes with goat anti-rabbit IgG-HRP conjugate and chemiluminescence. The Western blots were reprobed with mouse anti-actin and visualized with goat anti-mouse IgG-HRP and chemiluminescence.
DENV upregulates GRP78 in both antigen-positive and antigen-negative bystander cells at the time of high-level DENV antigen production.
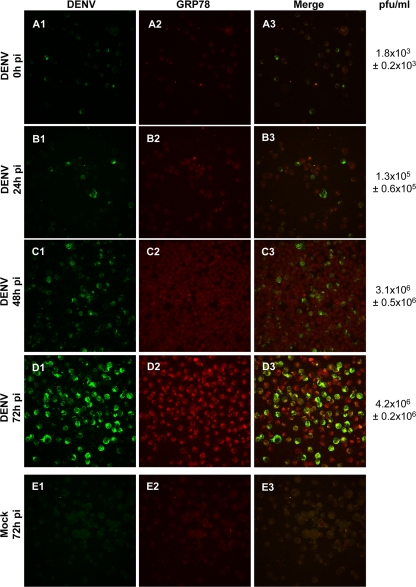
Next, the timing of GRP78 upregulation in relation to viral replication was analyzed. K562 cells were infected at a lower MOI to allow visualization of both infected and any uninfected bystander cells, and the cells were fixed, permeabilized, and immunostained for DENV and GRP78 (Fig. 3). Upregulation of GRP78 coincided with high-level viral-antigen production, and again, this was evident in both DENV antigen-positive and antigen-negative bystander cells. The highest GRP78 levels corresponded to high-level DENV antigen expression at 72 h p.i. (Fig. 3), and quantitation of the fluorescent image intensity at this time point (n = 6) showed significantly greater GRP78 staining in DENV-infected cells (45.9 ± 2.5) than in mock-infected (19.5 ± 0.8) or uninfected cell cultures (25 ± 1.5) (P < 0.05; Student's unpaired t test), again consistent with the two- to threefold upregulation observed by proteomic analysis (Fig. 1C) and Western blotting (Fig. 2C). Thus, DENV infection upregulates GRP78 in K562 cells and primary MDM, in both DENV antigen-positive and antigen-negative bystander cells, with the highest levels of GRP78 observed coincident with high-level DENV antigen production.
FIG. 3.
GRP78 is upregulated coincident with high-level viral-protein production. K562 cells were DENV or mock infected at an MOI of 1, and at the indicated times p.i., they were fixed, permeabilized, and costained for mouse anti-DENV (column 1) and rabbit anti-GRP78 (column 2), with detection using goat anti-mouse IgG-Alexa488 and goat anti-rabbit IgG-Alexa647, respectively, and analysis by confocal microscopy. Cumulative infectious-virus release was determined by plaque assay of cell supernatants (n = 2). The results represent means ± standard deviations.
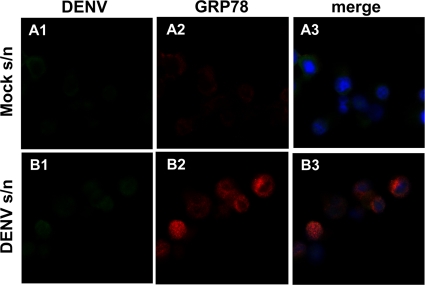
To investigate the mechanisms of upregulation of GRP78 in DENV antigen-negative bystander cells, K562 cells were treated with supernatants from DENV- or mock-infected K562 cells. After 1 h or 10 h of exposure, the cells were fixed, costained for DENV antigens and GRP78, and analyzed by confocal microscopy. One hour of exposure of the cells to DENV- or mock-infected cell supernatants did not result in DENV antigen-positive cells or any change in GRP78 staining (data not shown). In contrast, 10-h exposure of the cells to DENV-infected cell supernatants yielded a strong upregulation of GRP78 in comparison to that seen in cells treated with supernatants from mock-infected cells (Fig. 4). Upregulation of GRP78 was observed without accompanying productive DENV infection, as indicated by the absence of DENV antigen-positive cells (Fig. 4). Given that GRP78 induced by a single-round DENV infection is not apparent until 72 h p.i., this suggests the action of soluble factors released from DENV-infected cells that can upregulate GRP78 independently of productive DENV infection.
FIG. 4.
Supernatant from DENV-infected cells induces GRP78 in the absence of productive DENV infection. K562 cells were incubated for 10 h with supernatant (s/n) from mock-infected (A) or DENV-infected (B) K562 cells. The cells were washed, spotted onto glass slides, fixed, and costained for mouse anti-DENV (column 1) and rabbit anti-GRP78 (column 2), with detection using goat anti-mouse IgG-Alexa488 and goat anti-rabbit IgG-Alexa647, respectively, and analysis by confocal microscopy.
DENV replication requires GRP78 to assist viral-protein production.
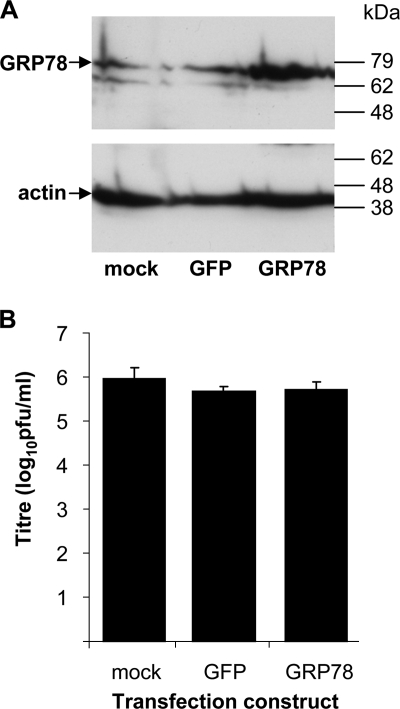
GRP78 is a known protein chaperone and thus may act to chaperone newly produced viral protein or particles, but GRP78 has additionally been reported as part of a DENV receptor complex (15) and thus may act to enhance DENV uptake. We therefore assessed the role of GRP78 during DENV infection by DENV challenge of cells overexpressing GRP78 at the time of infection and knockdown of GRP78 in DENV-infected cells at the time of peak virus production. For these experiments, we utilized 293 cells, since they can be readily transfected and can replicate DENV to high titers by 24 h p.i. (S. Wati, R. A. Ivanov, and J. M. Carr, unpublished data). 293 cells were transfected to express GRP78 or GFP as a control, and expression of GRP78 was confirmed by Western blot analysis (Fig. 5A). At 48 h posttransfection, the cells were challenged with DENV, and infectious-virus release was analyzed at 24 h p.i. The results showed no difference in infectious-virus release from cells expressing GRP78 or GFP or untransfected control cells (Fig. 5B). Thus, high levels of GRP78 in DENV target cells prior to infection do not affect subsequent DENV entry or virus production.
FIG. 5.
Overexpression of GRP78 does not affect DENV production. (A) 293 cells were transiently transfected with pEFIRES-P-BiP to express GRP78 or pEGFP. At 48 h posttransfection, the cells were lysed and the lysates were subjected to Western blotting with rabbit anti-GRP78 and detection of complexes with goat anti-rabbit IgG-HRP conjugate and chemiluminescence. The Western blots were reprobed with mouse anti-actin and visualized with goat anti-mouse IgG-HRP and chemiluminescence. (B) At 48 h posttransfection, the cells were infected with DENV at an MOI of 1 or mock infected. At 24 h p.i., the supernatant was sampled and assayed for infectious virus by plaque assay. The results represent means plus standard errors of the mean from three independent transfection/infection experiments.
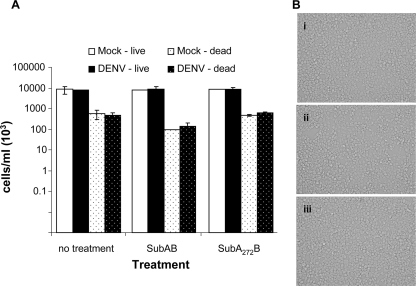
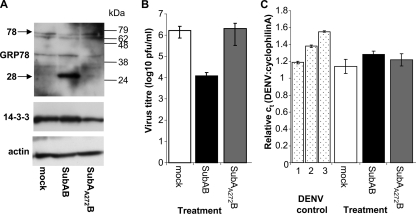
Next, the effect of reduction of GRP78 levels on DENV infection was assessed. Eighty to 90% knockdown of GRP78 protein can be achieved using short hairpin RNA, but a more complete and rapid knockdown can be achieved using the SubAB toxin (3). SubAB is an AB5 toxin derived from Shiga-toxigenic E. coli strains, and its catalytic A subunit can cleave GRP78 into 44-kDa and 28-kDa fragments, corresponding to the N- and C-terminal regions of GRP78, respectively (30). The SubAA272B mutant is a point mutant that lacks the catalytic ability of SubAB to cleave GRP78 (30). Based on previous literature (3), 293 cells were mock treated or treated with 100 ng/ml SubAB or the SubAA272B mutant for 30 min, and then the toxin was diluted to 25 ng/ml and incubated for 12 h. SubAB or SubAA272B treatment had no major cytotoxic effect with no change in cell viability as determined by trypan blue staining (Fig. 6A) or cell morphology as viewed by light microscopy (Fig. 6B). Following 12 h of SubAB treatment, the cells were lysed and the lysates were subjected to Western blotting using an antibody specific for the C-terminal region of GRP78 and thus the 28-kDa SubAB-cleaved fragment. The results showed the presence of the 28-kDa GRP78 cleavage product in SubAB-treated but not mock- or SubAA272B-treated cells, which represented the major form of GRP78 protein in these cells (Fig. 7A). We next assessed the effects of SubAB cleavage and knockdown of GRP78 on infectious DENV production and DENV RNA replication. 293 cells were DENV infected and at 12 h p.i. were treated with SubAB or the SubAA272B mutant or mock treated as described above. Following 12 h of treatment, the supernatants (24 h p.i.) were harvested for analysis of infectious-DENV release by plaque assay, and the cells were lysed and RNA was extracted for analysis of DENV negative-strand RNA, which is a marker of active DENV replication (46). The results showed a reproducible 10- to 100-fold decrease in production of infectious DENV (Fig. 7B) in the SubAB-treated culture without an accompanying change in the level of intracellular RNA (Fig. 7C). Thus, GRP78 does not affect DENV RNA replication but is required for efficient production of infectious DENV virions.
FIG. 6.
SubAB treatment does not affect cell viability. 293 cells were mock or DENV infected, and then at 12 h p.i. they were mock (i), SubAB (ii), or SubA272B mutant toxin (iii) treated for a further 12 h. (A and B) Live and dead cells were enumerated with trypan blue (A), and the visible morphology was assessed by light microscopy (B).
FIG. 7.
SubAB treatment cleaves GRP78 and reduces infectious-DENV production. (A) 293 cells were mock, SubAB, or SubA272B mutant toxin treated for 12 h, and then the cells were lysed and subjected to Western analysis against the C-terminal region of GRP78 (rabbit anti-GRP78 [525 to 638]). Antibody complexes were detected with anti-rabbit IgG-HRP conjugate and chemiluminescence. The filters were reprobed with rabbit anti-14-3-3 zeta, and mouse anti-actin and antibody complexes were detected with anti-rabbit or anti-mouse IgG-HRP conjugate and chemiluminescence. (B and C) 293 cells were mock or DENV infected at an MOI of 3, and at 12 h p.i., they were mock, SubAB, or SubA272B mutant toxin treated. At 24 h p.i. (after 12 h of mock, SubAB, or SubA272B mutant toxin treatment), the supernatants were assayed for infectious-virus release by plaque assay (B), and RNA was extracted and subjected to real-time RT-PCR for DENV negative-strand RNA (C). DENV controls (bars 1 to 3) were serial 1/10 dilutions of in vitro-transcribed DENV negative-strand RNA. The results are representative of three independent infections.
Importantly, GRP78 knockdown with SubAB toxin has the potential to reduce global protein synthesis. Our previous published data had shown by [35S]methionine protein labeling and detection of phosphorylated eIF2α (the α subunit of eukaryotic initiation factor 2) that global protein synthesis is reduced following as little as 0.5 h of SubAB treatment of cells, but this response is transient and protein synthesis recovers by 4 h of SubAB treatment (47). Under the conditions used here, we observed cleavage of GRP78 without an associated decrease in the levels of the abundant cellular 14-3-3 protein (Fig. 7A). Additionally, control cells were transfected to express a GFP reporter construct and then, at 36 h posttransfection, were mock, SubAB, or SubAA272B treated for 12 h, as described above. Analysis of GFP-positive cells by flow cytometry showed no change in the number or intensity of GFP-expressing cells (data not shown). Therefore, treatment with SubAB for 12 h specifically cleaved GRP78 but did not significantly affect cell viability or morphology and did not reduce the total levels of major host cell proteins or the expression of an exogenous transfected protein. Thus, under these conditions, SubAB toxin treatment is not cytotoxic and does not reduce global cellular protein levels.
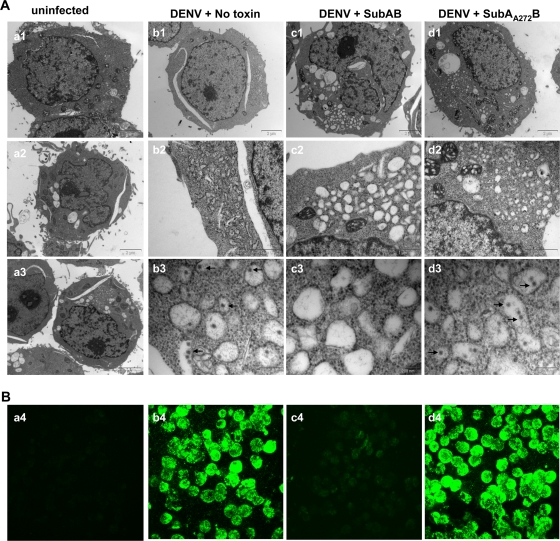
For HCMV infection, GRP78 knockdown similarly leads to reduced virion production and is accompanied by accumulation of intracellular virions (3). We thus assessed whether the decreased levels of infectious DENV in supernatant from cells lacking GRP78 was due to a block in DENV virion production or at virus release. 293 cells were infected with DENV and mock, SubAB, or SubAA272B mutant treated for 12 h, and the cells were then fixed and analyzed by TEM (Fig. 8A). Cells were also fixed, immunostained for DENV antigens, and analyzed by confocal microscopy (Fig. 8B). EM analysis showed normal cellular morphology in uninfected SubAB-treated cells, confirming the lack of major CPE of SubAB treatment (Fig. 8A, a1 to a3). ER proliferation, characteristic of flavivirus and DENV infection, was present in all DENV-infected cells, regardless of SubAA272B or SubAB treatment (Fig. 8A, b to d). In DENV-infected cells that were mock treated or treated with the SubAA272B mutant toxin, viral particles measured at 35.8 ± 0.5 nm (n = 51), consistent with the reported size of DENV particles, were present within membranous structures (Fig. 8A, b3 and d3). In contrast, there was a substantial reduction in the number of DENV particles visualized in SubAB-treated cells (Fig. 8A, c3). Immunostaining for DENV antigen and analysis by confocal microscopy clearly showed high-level DENV antigen in mock- and SubAA272B mutant-treated DENV-infected cells but a dramatic reduction in DENV antigen reactivity in SubAB-treated cells (Fig. 8B). Together, these results show that GRP78 protein knockdown by SubAB treatment had no gross detrimental effect on the cell and did not affect DENV RNA replication or DENV induction of ER proliferation but reduced DENV antigen levels, resulting in reduced numbers of intracellular virions and reduced production of infectious DENV particles. Thus, DENV infection induces GRP78 protein levels, which the virus utilizes to assist DENV antigen production.
FIG. 8.
SubAB knockdown of GRP78 reduces intracellular DENV virion and viral-antigen levels. 293 cells were mock or DENV infected at an MOI of 3, and at 12 h p.i., they were mock, SubAB, or SubA272B mutant toxin treated. (A) At 24 h p.i., uninfected cells or DENV-infected cells were treated for 12 h with SubAB or SubA272B mutant toxin or mock treated and then harvested, fixed, and subjected to TEM. a1, uninfected, no toxin; a2, uninfected, SubAB toxin; a3, uninfected, SubA272B mutant toxin treated; b1 to d3, DENV-infected cells. Row 1, original field; rows 2 and 3, enlargement of the field shown in row 1. The arrows indicate examples of viral particles. (B) Immunostaining against mouse anti-DENV and visualization of complexes with goat anti-mouse Alexa488. a4, uninfected cells; b4 to d4, DENV-infected cells.
DISCUSSION
The clinical outcome of DENV infection in humans is variable and is believed to be determined by the host responses to infection. Many studies have characterized circulating changes or altered cellular release of cytokines and chemokines (8, 13, 19) or altered mRNA transcripts during DENV infection (9, 23, 37, 39, 45). DENV infection has also been associated with upregulation of the UPR and activation of its downstream components (eIF2α phosphorylation, CHOP, and XBP-1) that can be associated with induction of cell death (44, 50). In this study, we performed a proteomic analysis to assess changes at the intracellular-protein level in a cell model that avoids the major cellular changes associated with a cytopathic UPR and cell death. To this end, the study utilized K562 cells, which support high-level DENV infection (20, 25) without cell death and also have been shown to lack a UPR-mediated cell death response during Japanese encephalitis virus infection (40). K562 cells also have some properties reflecting the natural monocyte/macrophage DENV target cell type, including the presence of Fc receptors. Proteomic analysis identified 344 unique protein spots and 1 protein spot that was significantly altered, approximately two- to threefold, by DENV infection. The total number of spots detected was low and could be improved technically by cup loading rather than passive rehydration of IEF strips, use of a more sensitive protein stain, and fractionation of cell lysates to reduce protein complexity. A proteomic study of DENV-infected HepG2 cells identified 800 protein spots and 17 differentially expressed proteins, only 7 of which were altered by >2-fold, the cutoff used in our proteomic study (32). Of these seven proteins, altered protein expression was confirmed by Western analysis for two proteins; elongation factor Tu (EF-Tu) mitochondrial precursor and vinculin. Altered GRP78 protein levels were not identified in this study (32). Using 2DGE and MS analysis, we successfully identified GRP78 as significantly upregulated in DENV-infected cells. Upregulation of GRP78 was confirmed by Western blotting, immunostaining, and confocal microscopy in K562 cells and also in MDM, a relevant natural target cell type. Additionally, upregulation of GRP78 was observed in both DENV antigen-positive and -negative bystander cells within the DENV-infected cell culture, and GRP78 could be upregulated by exposure of cells to cell culture supernatants from DENV-infected cells in the absence of a productive DENV infection. The observed timing of upregulation of GRP78 coincided with high-level DENV antigen production. DENV infection induces the release of a variety of chemokines and cytokines and factors such as nitric oxide (26, 29, 49) that are well described as inducing the expression of GRP78 (48). Taken together, these data suggest that GRP78 could be upregulated in DENV-infected cultures by two mechanisms: (i) as a direct response to productive infection in DENV-infected cells and (ii) as a secondary consequence, in both DENV-infected and bystander cells, of the release of factors from DENV-infected cells that can induce GRP78 expression.
The literature has suggested a role for GRP78 in hepatocytes (4, 15), and for HSP70 in monocytic cell types (36), as part of a receptor complex for DENV entry. Additionally, heat shock treatment of cells prior to DENV challenge, which would be expected to upregulate both GRP78 and HSP70, enhances DENV entry and replication (7). However, in this study, transfection of 293 cells to express high levels of GRP78 at the time of DENV challenge did not affect the subsequent production of infectious virus, and these results thus do not support a role for GRP78 alone in 293 cells as a rate-limiting factor for DENV entry or virus production.
Additionally, GRP78 is known to function as a major ER chaperone and can bind to many unfolded proteins, including viral proteins (14). Recently, using a yeast two-hybrid screen, it has been shown that GRP78 can interact with the DENV E protein, and consistent with the results of our study, small interfering RNA knockdown of BiP (GRP78) in DENV-infected Vero cells decreased infectious-virus production (24). This study extends this observation by showing that when GRP78 is cleaved by SubAB toxin treatment, which effectively reduces functional GRP78 chaperone levels in the cell, release of infectious DENV is dramatically reduced with an accompanying reduction in intracellular virion particles and DENV antigen levels but without any effect on DENV RNA production. This suggests that GRP78 may function in its traditional role in binding and chaperoning proper DENV protein folding and/or protein production and accumulation in the cell. Further experiments are needed to determine if this role for GRP78 is specific for particular DENV proteins or is a more generalized requirement for DENV polyprotein production. This role for GRP78 in chaperoning DENV protein production contrasts with the lack of a requirement for HMCV protein production for GRP78 (3, 27). Knockdown of GRP78 in HCMV infection leads to intracellular viral-particle accumulation, and thus, HCMV needs GRP78 to chaperone virion particle egress but not HCMV protein production itself. During rotavirus infection, knockdown of GRP78 impairs the specific cleavage of the oligosaccharide chains of NSP4 and thus reduces the infectivity of the released virion (25). These contrasting viral requirements for GRP78 are summarized in Table 1, suggesting that GRP78 may be utilized as a chaperone in different ways by different viruses: by HMCV for virion egress, by rotavirus for infectious-virion maturation, and by DENV for viral-antigen production. These differing requirements for GRP78 highlight the diverse ways in which viruses may utilize the same host factors for replication. In addition to an essential role in DENV antigen production, GRP78 may also assist DENV virion assembly, but a role in this specific step cannot be delineated from the current experiments.
TABLE 1.
Summary of actions of GRP78 in different virus infections
| Virus | Production of virala: |
GRP78 chaperone role | |||||
|---|---|---|---|---|---|---|---|
| RNA | Intracellular protein | Protein maturation and structure | Intracellular particles | Extracellular particles | Extracellular infectious virus | ||
| DENV | √ | X | ND | X | ND | X | Protein production |
| HCMVb | ND | √ | ND | √ | X | X | Particle egress |
| Rotavirusc | ND | √ | X | ND | √d | X | Correct protein structure and maturation |
In summary, we have shown for the first time that the host ER chaperone GRP78 is upregulated in DENV-infected cells that are not undergoing viral CPE or a cell death response. Furthermore, bystander cells also showed an increase in GRP78, and this could prime neighboring cells for subsequent DENV production. The timing of GRP78 upregulation coincides with high-level viral-antigen production, and knockdown of GRP78 severely reduces the production of infectious virus, intracellular viral particles, and intracellular viral antigen. This occurs without any change to viral-RNA replication and is consistent with a requirement for GRP78 to chaperone DENV antigen production during DENV infection. These results demonstrate the importance of the ER and its associated host cell machinery for productive DENV infection.
Acknowledgments
We thank Adrian Purins for maintenance of cell stocks and Chris Bagley at the Adelaide Proteomics Centre, School of Molecular and Biomedical Science, University of Adelaide, for MS analysis.
This project was supported by the Royal Adelaide Hospital/IMVS Research Committee Bridging Grant fund.
Footnotes
Published ahead of print on 30 September 2009.
REFERENCES
- 1.Benali-Furet, N. L., M. Chami, L. Houel, F. De Giorgi, F. Vernejoul, D. Lagorce, L. Buscail, R. Bartenschlager, F. Ichas, R. Rizzuto, and P. Paterlini-Brechot. 2005. Hepatitis C virus core triggers apoptosis in liver cells by inducing ER stress and ER calcium depletion. Oncogene 24:4921-4933. [DOI] [PubMed] [Google Scholar]
- 2.Bertolotti, A., Y. Zhang, L. M. Hendershot, H. P. Harding, and D. Ron. 2000. Dynamic interaction of BiP and ER stress transducers in the unfolded-protein response. Nat. Cell Biol. 2:326-332. [DOI] [PubMed] [Google Scholar]
- 3.Buchkovich, N. J., T. G. Maguire, Y. Yu, A. W. Paton, J. C. Paton, and J. C. Alwine. 2008. Human cytomegalovirus specifically controls the levels of the endoplasmic reticulum chaperone BiP/GRP78, which is required for virion assembly. J. Virol. 82:31-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cabrera-Hernandez, A., C. Thepparit, L. Suksanpaisan, and D. R. Smith. 2007. Dengue virus entry into liver (HepG2) cells is independent of hsp90 and hsp70. J. Med. Virol. 79:386-392. [DOI] [PubMed] [Google Scholar]
- 5.Carr, J. M., H. Hocking, K. Bunting, P. J. Wright, A. Davidson, J. Gamble, C. J. Burrell, and P. Li. 2003. Supernatants from dengue virus type-2 infected macrophages induce permeability changes in endothelial cell monolayers. J. Med. Virol. 69:521-528. [DOI] [PubMed] [Google Scholar]
- 6.Carr, J. M., H. Hocking, P. Li, and C. J. Burrell. 1999. Rapid and efficient cell-to-cell transmission of human immunodeficiency virus infection from monocyte-derived macrophages to peripheral blood lymphocytes. Virology 265:319-329. [DOI] [PubMed] [Google Scholar]
- 7.Chavez-Salinas, S., I. Ceballos-Olvera, J. Reyes-Del Valle, F. Medina, and R. M. Del Angel. 2008. Heat shock effect upon dengue virus replication into U937 cells. Virus Res. 138:111-118. [DOI] [PubMed] [Google Scholar]
- 8.Chen, Y. C., and S. Y. Wang. 2002. Activation of terminally differentiated human monocytes/macrophages by dengue virus: productive infection, hierarchical production of innate cytokines and chemokines, and the synergistic effect of lipopolysaccharide. J. Virol. 76:9877-9887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekkapongpisit, M., T. Wannatung, T. Susantad, K. Triwitayakorn, and D. R. Smith. 2007. cDNA-AFLP analysis of differential gene expression in human hepatoma cells (HepG2) upon dengue virus infection. J. Med. Virol. 79:552-561. [DOI] [PubMed] [Google Scholar]
- 10.Gualano, R. C., M. J. Pryor, M. R. Cauchi, P. J. Wright, and A. D. Davidson. 1998. Identification of a major determinant of mouse neurovirulence of dengue virus type 2 using stably cloned genomic-length cDNA. J. Gen. Virol. 79:437-446. [DOI] [PubMed] [Google Scholar]
- 11.Halstead, S. B. 1989. Antibody, macrophages, dengue virus infection, shock, and hemorrhage: a pathogenetic cascade. Rev. Infect Dis 11(Suppl. 4):S830-S839. [DOI] [PubMed] [Google Scholar]
- 12.Halstead, S. B., E. J. O'Rourke, and A. C. Allison. 1977. Dengue viruses and mononuclear phagocytes. II. Identity of blood and tissue leukocytes supporting in vitro infection. J. Exp. Med. 146:218-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hober, D., L. Poli, B. Roblin, P. Gestas, E. Chungue, G. Granic, P. Imbert, J. L. Pecarere, R. Vergez-Pascal, and P. Wattre. 1993. Serum levels of tumor necrosis factor-alpha (TNF-alpha), interleukin-6 (IL-6), and interleukin-1 beta (IL-1 beta) in dengue-infected patients. Am. J. Trop. Med. Hyg. 48:324-331. [DOI] [PubMed] [Google Scholar]
- 14.Hurtley, S. M., D. G. Bole, H. Hoover-Litty, A. Helenius, and C. S. Copeland. 1989. Interactions of misfolded influenza virus hemagglutinin with binding protein (BiP). J. Cell Biol. 108:2117-2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jindadamrongwech, S., C. Thepparit, and D. R. Smith. 2004. Identification of GRP 78 (BiP) as a liver cell expressed receptor element for dengue virus serotype 2. Arch. Virol. 149:915-927. [DOI] [PubMed] [Google Scholar]
- 16.Jordan, R., L. Wang, T. M. Graczyk, T. M. Block, and P. R. Romano. 2002. Replication of a cytopathic strain of bovine viral diarrhea virus activates PERK and induces endoplasmic reticulum stress-mediated apoptosis of MDBK cells. J. Virol. 76:9588-9599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joyce, M. A., K. A. Walters, S. E. Lamb, M. M. Yeh, L. F. Zhu, N. Kneteman, J. S. Doyle, M. G. Katze, and D. L. Tyrrell. 2009. HCV induces oxidative and ER stress, and sensitizes infected cells to apoptosis in SCID/Alb-uPA mice. PLoS Pathog. 5:e1000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim, I., W. Xu, and J. C. Reed. 2008. Cell death and endoplasmic reticulum stress: disease relevance and therapeutic opportunities. Nat. Rev. Drug Discov. 7:1013-1030. [DOI] [PubMed] [Google Scholar]
- 19.Kurane, I., B. L. Innis, S. Nimmannitya, A. Nisalak, A. Meager, J. Janus, and F. A. Ennis. 1991. Activation of T lymphocytes in dengue virus infections. High levels of soluble interleukin 2 receptor, soluble CD4, soluble CD8, interleukin 2, and interferon-gamma in sera of children with dengue. J. Clin. Investig. 88:1473-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurane, I., U. Kontny, J. Janus, and F. A. Ennis. 1990. Dengue-2 virus infection of human mononuclear cell lines and establishment of persistent infections. Arch. Virol. 110:91-101. [DOI] [PubMed] [Google Scholar]
- 21.Li, X. D., H. Lankinen, N. Putkuri, O. Vapalahti, and A. Vaheri. 2005. Tula hantavirus triggers pro-apoptotic signals of ER stress in Vero E6 cells. Virology 333:180-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liberman, E., Y. L. Fong, M. J. Selby, Q. L. Choo, L. Cousens, M. Houghton, and T. S. Yen. 1999. Activation of the grp78 and grp94 promoters by hepatitis C virus E2 envelope protein. J. Virol. 73:3718-3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liew, K. J., and V. T. Chow. 2006. Microarray and real-time RT-PCR analyses of a novel set of differentially expressed human genes in ECV304 endothelial-like cells infected with dengue virus type 2. J. Virol. Methods 131:47-57. [DOI] [PubMed] [Google Scholar]
- 24.Limjindaporn, T., W. Wongwiwat, S. Noisakran, C. Srisawat, J. Netsawang, C. Puttikhunt, W. Kasinrerk, P. Avirutnan, S. Thiemmeca, R. Sriburi, N. Sittisombut, P. Malasit, and P. T. Yenchitsomanus. 2009. Interaction of dengue virus envelope protein with endoplasmic reticulum-resident chaperones facilitates dengue virus production. Biochem. Biophys. Res. Commun. 379:196-200. [DOI] [PubMed] [Google Scholar]
- 25.Littaua, R., I. Kurane, and F. A. Ennis. 1990. Human IgG Fc receptor II mediates antibody-dependent enhancement of dengue virus infection. J. Immunol. 144:3183-3186. [PubMed] [Google Scholar]
- 26.Marianneau, P., A. M. Steffan, C. Royer, M. T. Drouet, D. Jaeck, A. Kirn, and V. Deubel. 1999. Infection of primary cultures of human Kupffer cells by Dengue virus: no viral progeny synthesis, but cytokine production is evident. J. Virol. 73:5201-5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maruri-Avidal, L., S. Lopez, and C. F. Arias. 2008. Endoplasmic reticulum chaperones are involved in the morphogenesis of rotavirus infectious particles. J. Virol. 82:5368-5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medigeshi, G. R., A. M. Lancaster, A. J. Hirsch, T. Briese, W. I. Lipkin, V. Defilippis, K. Fruh, P. W. Mason, J. Nikolich-Zugich, and J. A. Nelson. 2007. West Nile virus infection activates the unfolded protein response, leading to CHOP induction and apoptosis. J. Virol. 81:10849-10860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neves-Souza, P. C., E. L. Azeredo, S. M. Zagne, R. Valls-de-Souza, S. R. Reis, D. I. Cerqueira, R. M. Nogueira, and C. F. Kubelka. 2005. Inducible nitric oxide synthase (iNOS) expression in monocytes during acute Dengue Fever in patients and during in vitro infection. BMC Infect. Dis. 5:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paton, A. W., T. Beddoe, C. M. Thorpe, J. C. Whisstock, M. C. Wilce, J. Rossjohn, U. M. Talbot, and J. C. Paton. 2006. AB5 subtilase cytotoxin inactivates the endoplasmic reticulum chaperone BiP. Nature 443:548-552. [DOI] [PubMed] [Google Scholar]
- 31.Paton, A. W., P. Srimanote, U. M. Talbot, H. Wang, and J. C. Paton. 2004. A new family of potent AB(5) cytotoxins produced by Shiga toxigenic Escherichia coli. J. Exp. Med. 200:35-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pattanakitsakul, S. N., K. Rungrojcharoenkit, R. Kanlaya, S. Sinchaikul, S. Noisakran, S. T. Chen, P. Malasit, and V. Thongboonkerd. 2007. Proteomic analysis of host responses in HepG2 cells during dengue virus infection. J. Proteome Res. 6:4592-4600. [DOI] [PubMed] [Google Scholar]
- 33.Peyrefitte, C. N., B. Pastorino, M. Bessaud, H. J. Tolou, and P. Couissinier-Paris. 2003. Evidence for in vitro falsely-primed cDNAs that prevent specific detection of virus negative strand RNAs in dengue-infected cells: improvement by tagged RT-PCR. J. Virol. Methods 113:19-28. [DOI] [PubMed] [Google Scholar]
- 34.Pryor, M. J., J. M. Carr, H. Hocking, A. D. Davidson, P. Li, and P. J. Wright. 2001. Replication of dengue virus type 2 in human monocyte-derived macrophages: comparisons of isolates and recombinant viruses with substitutions at amino acid 390 in the envelope glycoprotein. Am. J. Trop. Med. Hyg. 65:427-434. [DOI] [PubMed] [Google Scholar]
- 35.Rao, R. V., A. Peel, A. Logvinova, G. del Rio, E. Hermel, T. Yokota, P. C. Goldsmith, L. M. Ellerby, H. M. Ellerby, and D. E. Bredesen. 2002. Coupling endoplasmic reticulum stress to the cell death program: role of the ER chaperone GRP78. FEBS Lett. 514:122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reyes-Del Valle, J., S. Chavez-Salinas, F. Medina, and R. M. Del Angel. 2005. Heat shock protein 90 and heat shock protein 70 are components of dengue virus receptor complex in human cells. J. Virol. 79:4557-4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sariol, C. A., J. L. Munoz-Jordan, K. Abel, L. C. Rosado, P. Pantoja, L. Giavedoni, I. V. Rodriguez, L. J. White, M. Martinez, T. Arana, and E. N. Kraiselburd. 2007. Transcriptional activation of interferon-stimulated genes but not of cytokine genes after primary infection of rhesus macaques with dengue virus type 1. Clin. Vaccine Immunol. 14:756-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott, R. M., A. Nisalak, U. Cheamudon, S. Seridhoranakul, and S. Nimmannitya. 1980. Isolation of dengue viruses from peripheral blood leukocytes of patients with hemorrhagic fever. J. Infect. Dis. 141:1-6. [DOI] [PubMed] [Google Scholar]
- 39.Simmons, C. P., S. Popper, C. Dolocek, T. N. Chau, M. Griffiths, N. T. Dung, T. H. Long, D. M. Hoang, N. V. Chau, T. T. Thao Le, T. T. Hien, D. A. Relman, and J. Farrar. 2007. Patterns of host genome-wide gene transcript abundance in the peripheral blood of patients with acute dengue hemorrhagic fever. J. Infect. Dis. 195:1097-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Su, H. L., C. L. Liao, and Y. L. Lin. 2002. Japanese encephalitis virus infection initiates endoplasmic reticulum stress and an unfolded protein response. J. Virol. 76:4162-4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szegezdi, E., S. E. Logue, A. M. Gorman, and A. Samali. 2006. Mediators of endoplasmic reticulum stress-induced apoptosis. EMBO Rep. 7:880-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Talbot, U. M., J. C. Paton, and A. W. Paton. 2005. Protective immunization of mice with an active-site mutant of subtilase cytotoxin of Shiga toxin-producing Escherichia coli. Infect. Immun. 73:4432-4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tardif, K. D., K. Mori, and A. Siddiqui. 2002. Hepatitis C virus subgenomic replicons induce endoplasmic reticulum stress activating an intracellular signaling pathway. J. Virol. 76:7453-7459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Umareddy, I., O. Pluquet, Q. Y. Wang, S. G. Vasudevan, E. Chevet, and F. Gu. 2007. Dengue virus serotype infection specifies the activation of the unfolded protein response. Virol. J. 4:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Warke, R. V., K. Xhaja, K. J. Martin, M. F. Fournier, S. K. Shaw, N. Brizuela, N. de Bosch, D. Lapointe, F. A. Ennis, A. L. Rothman, and I. Bosch. 2003. Dengue virus induces novel changes in gene expression of human umbilical vein endothelial cells. J. Virol. 77:11822-11832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wati, S., P. Li, C. J. Burrell, and J. M. Carr. 2007. Dengue virus (DV) replication in monocyte-derived macrophages is not affected by tumor necrosis factor alpha (TNF-α), and DV infection induces altered responsiveness to TNF-α stimulation. J. Virol. 81:10161-10171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wolfson, J. J., K. L. May, C. M. Thorpe, D. M. Jandhyala, J. C. Paton, and A. W. Paton. 2008. Subtilase cytotoxin activates PERK, IRE1 and ATF6 endoplasmic reticulum stress-signalling pathways. Cell Microbiol. 10:1775-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu, W., L. Liu, I. G. Charles, and S. Moncada. 2004. Nitric oxide induces coupling of mitochondrial signalling with the endoplasmic reticulum stress response. Nat. Cell Biol. 6:1129-1134. [DOI] [PubMed] [Google Scholar]
- 49.Yen, Y. T., H. C. Chen, Y. D. Lin, C. C. Shieh, and B. A. Wu-Hsieh. 2008. Enhancement by tumor necrosis factor alpha of dengue virus-induced endothelial cell production of reactive nitrogen and oxygen species is key to hemorrhage development. J. Virol. 82:12312-12324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu, C. Y., Y. W. Hsu, C. L. Liao, and Y. L. Lin. 2006. Flavivirus infection activates the XBP1 pathway of the unfolded protein response to cope with endoplasmic reticulum stress. J. Virol. 80:11868-11880. [DOI] [PMC free article] [PubMed] [Google Scholar]