Abstract
Background
Treating hyperglycemia promotes better outcomes among inpatients. Knowledge deficits about management of inpatient diabetes are prevalent among resident physicians, which may affect the care of a substantial number of these patients.
Methods
A computer-based training (CBT) curriculum on inpatient diabetes and hyperglycemia was developed and implemented for use by resident physicians and focuses on several aspects of the management of inpatient diabetes and hyperglycemia: (1) review of importance of inpatient glucose control, (2) overview of institution-specific data, (3) triaging and initial admission actions for diabetes or hyperglycemia, (4) overview of pharmacologic management, (5) insulin-dosing calculations and ordering simulations, (6) review of existing policies and procedures, and (7) discharge planning. The curriculum was first provided as a series of lectures, then formatted and placed on the institutional intranet as a CBT program.
Results
Residents began using the inpatient CBT in September 2008. By August 2009, a total of 29 residents had participated in CBT: 8 in family medicine, 12 in internal medicine, and 9 in general surgery. Most of the 29 residents confirmed that module content met stated objectives, considered the information valuable to their inpatient practices, and believed that the quality of the online modules met expectations. The majority reported that the modules took just the right amount of time to complete (typically 30 min each).
Conclusions
Improvement in inpatient diabetes care requires continuous educational efforts. The CBT format and curriculum content were well accepted by the resident physicians. Ongoing assessment must determine whether resident practice patterns are influenced by such training.
Keywords: computer-based training, hospital hyperglycemia, inpatient diabetes, resident physicians
Introduction
Effective management of inpatient hyperglycemia may improve patient outcomes in many clinical situations (e.g., by reducing mortality from acute myocardial infarction and decreasing deep sternal wound infections).1–4 Consequently, national and regional organizations5–8 and professional societies1–3,8,9 have developed guidelines and tool kits for management of inpatient hyperglycemia. The general perception of many health care providers is that inpatient diabetes care is in a state of “glycemic chaos;”10 multiple analyses have demonstrated gaps in the quality of inpatient diabetes care.11–14
Although inpatient management of hyperglycemia is often criticized, it should be acknowledged that glycemic control in the hospital poses unique challenges. The population of inpatients with hyperglycemia is diverse and often described as encompassing patients with preexisting diabetes, with previously undiagnosed diabetes, or with hyperglycemia that develops because of acute illness or specific medical therapies (e.g., high-dose glucocorticoids). There are also critically ill patients, noncritically ill patients, and others who migrate in and out of these clinical states during their hospitalization.
Adding to this complexity are other factors that create a dynamic situation: short lengths of stay, unpredictable timing of procedures, various and changing forms of nutritional support, and different levels of expertise among medical staff members. Furthermore, insulin is considered a high-risk medication, which might add to practitioner unease about inpatient use.15–17 Hospital quality improvement efforts must include all subsets of hyperglycemic patients.
Given the complex nature of inpatient hyperglycemia management, improving hospital care (i.e., creating “glycemic order” out of “glycemic chaos”)18 likely will require intensive, coordinated, prolonged, and multi-pronged educational programs reaching all types of health care practitioners. One group of practitioners that should benefit from a dedicated educational program is resident physicians, who may care for as many as 50% of our hospitalized diabetes patients.13
Our previous studies confirmed the need for a dedicated educational program on inpatient diabetes and hyper-glycemia. Our hospital data indicate an ever-increasing prevalence of inpatients with these conditions, from 14% of all 1999 discharges to 22% in 2007. Previous analyses have also shown the need for improved care: more than 40% of patients admitted with poor glucose control were discharged with poor control.13 Although nearly all admission notes appropriately acknowledged diabetes in newly admitted patients, the condition was subsequently addressed in only about 60% through daily progress notes.14 Moreover, insulin therapy was often improperly applied (i.e., overuse of sliding scale) and subject to both clinical inertia (i.e., failure to intensify therapy despite persistent hyperglycemia) and negative therapeutic momentum (i.e., deintensification of therapy despite persistent hyperglycemia).13,14,19
A survey to explore practitioner attitudes about inpatient diabetes was developed and administered to resident physicians.20 Results confirmed that residents viewed inpatient hyperglycemia as highly prevalent and glucose control as important. Although they indicated that diabetes and hyperglycemia cases composed a large proportion of their inpatient practices, these respondents expressed discomfort about management.20 Knowledge deficits were identified that pertained to insulin use and existing institutional policies on glucose management. These findings were echoed in surveys of inpatient midlevel practitioners (i.e., nurse practitioners and physician assistants)21 and residents in a training program in a different geographic area.22 Common themes in these resident surveys included lack of comfort with glucose management, low familiarity with diabetes-related institutional policies and procedures, and poor understanding of how best to apply insulin therapy.20,22
Computer-based training (CBT) is one approach to enhance clinical skills that has garnered attention for use in undergraduate and graduate medical training.23–26 General principles for the design and development of a CBT curriculum include interactivity, learner feedback, accessibility, and integration with the core curriculum.27–30
In this paper, we discuss the design and implementation of an inpatient diabetes educational curriculum crafted specifically for our resident physicians. The curriculum focuses on diabetes and hyperglycemia management in the acute care setting and was developed in three phases: (1) content development, (2) delivering content via lectures, and (3) migration of the curriculum to a Web-based CBT format. We give an overview of course content, describe the CBT format, and review preliminary data on resident satisfaction with its use.
Methods
Overview of Institution
Our tertiary care academic medical center is a facility with 200-plus beds in metropolitan Phoenix, Arizona. All adult general medical and surgical specialty services are represented; inpatient pediatric care and obstetric care are not offered. Inpatient care is provided by resident physicians, students in allied health and medical schools, physician assistants, nurse practitioners, and staff physicians.
Our institution offers numerous accredited residency and fellowship training programs. However, the inpatient diabetes curriculum was designed for resident physicians most likely to be directly involved in management of inpatient diabetes on an ongoing basis, rather than for other types of trainees with primarily consultative roles (e.g., dermatology residents, fellows in gastroenterology, hematology/oncology, or epilepsy). Prior research indicated that nearly 75% of diabetes inpatients at our facility are managed on either on the primary care services (i.e., family medicine or general internal medicine) or on the surgical services.13,14 Hence, the CBT curriculum was designed to target trainees in family medicine, general internal medicine, and general surgery. Although residents routinely attended lectures on management of several inpatient conditions, they had no access to dedicated instruction on inpatient diabetes other than on diabetic ketoacidosis and hyperglycemic crisis.
Institutional electronic educational resources are coordinated through the system-wide Education Technology Center (ETC). The ETC goals are two-fold: (1) to ensure the highest quality of patient care by capturing, indexing, storing, and delivering medical knowledge and (2) to assess and implement technology in support of an environment of lifelong learning. The ETC provides a spectrum of online education, from curriculum-based, instructor-led courseware to self-directed point-of-care learning.
Training Curriculum and Computer-Based Training Course
After a preliminary curriculum was developed, its content was initially provided as lectures during a series of family medicine and internal medicine 1 h noon conferences. The lectures were not delivered to surgical residents, but the surgical training program director reviewed lecture content and provided feedback to the curriculum developers on its relevancy to trainees. Between 2006 and 2008, the lectures were delivered twice to internal medicine and once to family medicine residents. The terms diabetes and hyperglycemia were used interchangeably, because patients with diabetes may have hyperglycemia and because hyperglycemic patients, even without a diabetes diagnosis, often require treatment and education comparable to that for patients with known diabetes.
However, delivering recurring lectures to multiple training programs was time-intensive for the presenter, which led to the design of the current seven-module CBT curriculum. In addition, a CBT approach allows for immediate interaction between learner and curriculum. After completing the lecture series and receiving informal feedback from residents, curriculum objectives were finalized, revisions made in content and format, and the curriculum imported into a CBT environment using Articulate Presenter 5.2 and Articulate Engage (Articulate Global, Inc., New York, NY); this software allows rapid development of CBT from existing lecture materials while permitting interactivity to maintain learner engagement. Case studies and computerized physician order entry (CPOE) simulations were developed using Adobe Captivate (Adobe Systems, Inc., San Jose, CA) to provide learner practice and feedback. Tracking participation and completion of the curriculum were done with a learning management system (Pathlore 6.6 Learning Management System, SumTotal Systems, Inc., Mountain View, CA).
The inpatient diabetes CBT curriculum was placed on our institutional intranet, where Web-based training is a standard method of accessing and tracking mandatory education. All family medicine (typically during their third year) and internal medicine (typically during their second year) residents rotate through the Division of Endocrinology within the Department of Internal Medicine. Hence the inpatient diabetes CBT was required as part of the endocrinology rotation, and dedicated time was built into the residents' clinical calendar so they could complete it during work hours in compliance with resident work-hour restrictions; they were scheduled to complete one module per day over seven consecutive days. For general surgery residents, the CBT curriculum was incorporated into their training requirements. The curriculum can be accessed from any computer anywhere within the institution or by remote access.
Computer-Based Training Content
The CBT curriculum consists of seven online modules. In addition to the overall curriculum objectives, which are presented at the beginning of the course, each module has its own specific objectives. Modules 1 and 2 consist of introductory material. Module 1 reviews data on the relationship between inpatient hyperglycemia and hospital outcomes;1–4 several examples of clinical studies from the surgical literature make the topic relevant to surgical trainees. Module 2 summarizes our institution-specific data on inpatient diabetes care and glycemic control.13,14
Modules 3 to 7 focus on principles of hospital management of diabetes and hyperglycemia. Although such management is a continuum (e.g., discharge planning should begin early after hospitalization and changes in therapy may occur until discharge), for the purpose of organizing the curriculum, inpatient care is conceptualized in three segments (Figure 1). A case-based approach is used throughout modules 3 to 7; residents are required to answer questions about case scenarios and are provided feedback on their responses.
Figure 1.
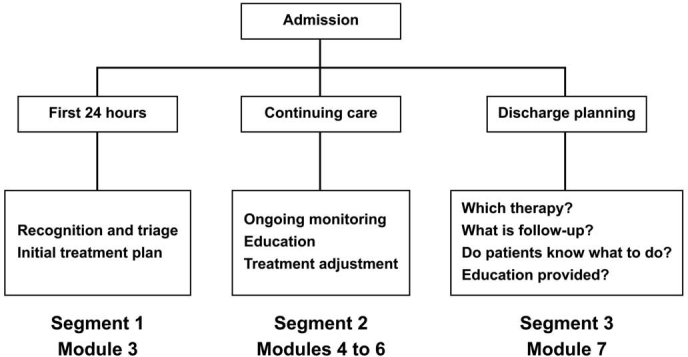
Inpatient diabetes care is conceptualized for teaching purposes as having three segments of care: (1) initial triage and assessment, (2) continuing care, and (3) discharge planning.
Segment 1 of care (Figure 1, initial recognition and triage, module 3) discusses actions required within the first 24 h after admission. The importance of recognizing the patient with diabetes or hyperglycemia early on is underscored. Likewise, the need to correctly categorize the type of diabetes (e.g., so that insulin is not withheld from patients with type 1 diabetes) is emphasized. Module 3 proposes an initial treatment scheme based on the severity of hyperglycemia (Figure 2), the type of diabetes, and the mode of outpatient therapy (Figure 3). The pathways in Figures 2 and 3 illustrate one approach on how to generate awareness about the need to recognize the presence of diabetes and/or hyperglycemia early in the hospital stay and how to individualize initial therapy. The pathway outlined in Figure 2 can be applied to individuals with or without a previous history of diabetes. Correctional insulin is recommended only with the mildest levels of hyperglycemia. Module 3 also describes four basic actions to accomplish at admission: (1) order bedside glucose monitoring, (2) measure hemoglobin A1c (HbA1c), (3) document diabetes/hyperglycemia in the admission note, and (4) outline a therapeutic strategy. The recommendation for obtaining an HbA1c value follows recent Joint Commission recommendations.7
Figure 2.
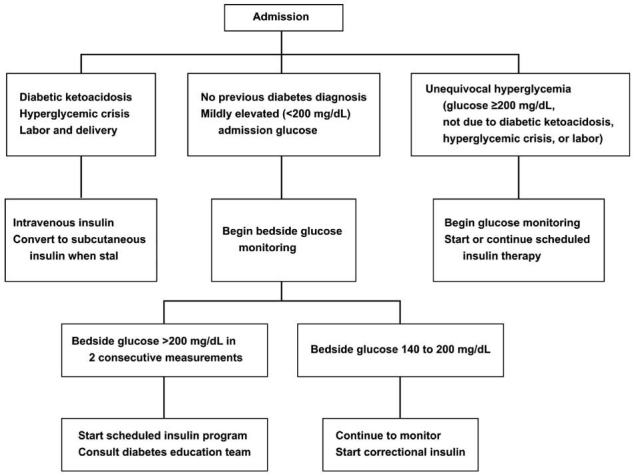
Sample hospital clinical pathway outlining an initial approach to management of hyperglycemia.
Figure 3.
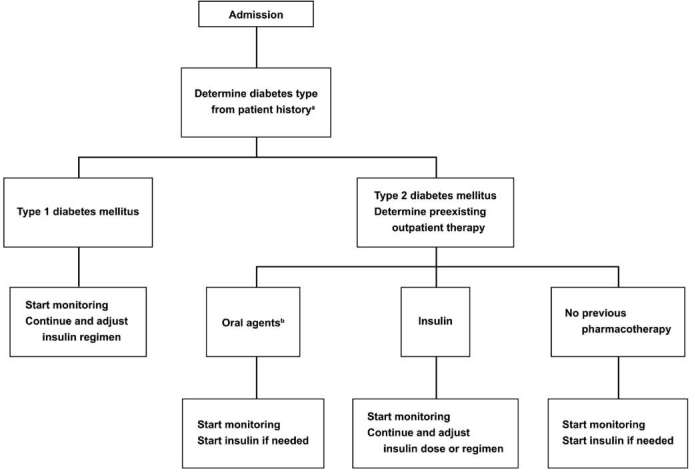
Sample hospital clinical pathway for initial management by type of diabetes and mode of outpatient therapy for hyperglycemia. a If uncertain and patient on insulin, keep on insulin. b Consider discontinuing depending on clinical situation.
Segment 2 of care (Figure 1, continuing care, modules 4 to 6) provides instruction in ongoing management, specifically pharmacologic management, during hospi-talization. The optimal use of pharmacotherapy for inpatient hyperglycemia is reviewed in modules 4 and 5. Residents are counseled against using oral hypoglycemic agents unless the patient is stable (e.g., in the inpatient rehabilitation unit).1,31 A sliding scale approach to insulin use is discouraged for severe hyperglycemia because of the proven lack of efficacy,32,33 whereas a basal-prandial-bolus approach to hyperglycemia treatment is encouraged as the principal means of providing insulin therapy because of its superior ability to control hyperglycemia.1,34 Moreover, structured insulin order sets and computer-based algorithms can lead to better application of insulin therapy.35 Instruction is provided on how to calculate doses of each component of insulin therapy. We use a weight-based formula, with 0.5 U of insulin administered per kilogram as an example of how to estimate total daily insulin dose.34–36 Cases are presented throughout the modules that require learners to practice calculating insulin doses (Figure 4). The trainee can click on a pop-up window on the computer screen that reviews insulin-dosing formulas. After completing a calculation, the resident can select “submit” to determine its correctness. Answers are acceptable if they fall within a narrow range, which accounts for possible differences in rounding during calculations (Figure 4). If necessary, the learner can make multiple attempts at the calculation. Our previous data indicated that diabetes is often “forgotten” after admission,13 hence the emphasis on daily bedside assessment of glucose values and adjustments in insulin therapy.
Figure 4.

Example of an insulin dosing simulation. A pop-up can be activated (lower right) to review formulas, with instantaneous feedback after the learner submits the calculated answer. CF, correction factor; TDD, total daily dose.
Module 6 reviews existing institutional policies and procedures for recognizing and treating hypoglycemia and for using subcutaneous insulin order sets. Although patients on insulin pump therapy are encountered infrequently, this module also reviews institutional guidelines and procedures we developed to follow up on patients already on outpatient insulin pump therapy.37 Simulations are also provided to guide residents in placing subcutaneous insulin and insulin pump orders in the institutional CPOE system.
Segment 3 of care (Figure 1, module 7) discusses discharge planning and establishes the criteria for a successful transition from inpatient to outpatient settings. Module 7 discusses effective discharge planning as a national priority7,31,38,39 and delineates the mechanisms within our institution that facilitate an effective diabetes discharge.40 Since our institution does not deploy a rapid-response diabetes education team, emphasis is placed on early identification of deficits in patient knowledge so that education can begin before discharge.
Educational Curriculum and Computer-Based Training Assessment
Residents are asked to complete an online evaluation after each training module. Each module has a set of common questions that address whether the program met stated objectives, whether the information was valuable to their inpatient practice, and whether the quality of the online modules met their expectations. Possible responses are “not applicable,” “no opinion,” “strongly disagree,” “disagree,” “agree,” and “strongly agree.” Each module also queried the residents about the time it took for completion; choices were “too long,” “too short,” and “just the right amount of time.” The actual time spent on each module was also determined by calculating the difference between the log-out and log-in time recorded in the learning system.
In addition to these universal questions, evaluative questions asked to what extent the module-specific objectives had been met. Residents can select “not applicable,” “no opinion,” “strongly disagree,” “disagree,” “agree,” or “strongly agree.” At the completion of the CBT curriculum, residents complete a cumulative assessment of how well they believe the curriculum objectives were met as a whole. Possible responses for each objective are “objective not met,” “objective partially met,” and “objective fully met.”
Results
Resident Feedback
Development of the inpatient diabetes CBT curriculum was completed by August 2008, and residents began using it in September 2008. From September 2008 to August 2009, a total of 29 residents completed all seven modules (8 from family medicine, 12 from general internal medicine, and 9 from general surgery).
Table 1 lists the number of residents completing the evaluations for each module. Of those who completed the evaluations, the majority agreed or strongly agreed that each module met its stated objectives. In addition, most (≥90%) residents agreed or strongly agreed that the information in each module was valuable to their inpatient practice, that the quality of the online modules met their expectations, and that the information would be valuable to their inpatient clinical practice (data not shown). Among the residents who completed the final summary evaluations, most indicated that the overall curriculum objectives had been fully met (Table 2).
Table 1.
Resident Opinions of Module-Specific Objectives a
| Module | Module-specific objective | Total number of responses | Strongly agree | Agree | No opinion | Disagree | Strongly disagree |
|---|---|---|---|---|---|---|---|
| 1 | Understanding the importance of inpatient hyperglycemia has been enhanced as a result of completing this module. | 28 | 13 (46) | 14 (50) | 1 (4) | 0 | 0 |
| 2 | I now have a better understanding of diabetes care at our hospital. | 13 | 8 (61) | 4 (31) | 0 | 1 (8) | 0 |
| 3 | I now have a better understanding of how to triage newly admitted patients with diabetes or hyperglycemia. | 26 | 13 (50) | 11 (42) | 1 (4) | 1 (4) | 0 |
| 4 | I now have a better understanding of how to approach pharmacologic management of inpatient hyperglycemia. | 18 | 15 (83) | 3 (17) | 0 | 0 | 0 |
| 5 | I now have a better understanding of how to calculate and adjust insulin therapy in the hospital. | 17 | 15 (88) | 2 (12) | 0 | 0 | 0 |
| 6 | I now have a better understanding of Mayo Clinic Hospital's current inpatient procedures relating to hypoglycemia. | 18 | 15 (83) | 3 (17) | 0 | 0 | 0 |
| I now have a better understanding of Mayo Clinic Hospital's current inpatient CPOE procedures relating to ordering subcutaneous insulin. | 18 | 15 (83) | 3 (17) | 0 | 0 | 0 | |
| I now have a better understanding of Mayo Clinic Hospital's current inpatient CPOE procedures relating to insulin pumps. | 17 | 15 (88) | 2 (12) | 0 | 0 | 0 | |
| 7 | I now have a better understanding of what needs to be done to get a diabetes patient ready for discharge. | 18 | 8 (44) | 9 (50) | 1 (6) | 0 | 0 |
Data are number of responses (percent).
Table 2.
Resident Opinions on Whether Overall Curriculum Objectives Were Met a
| Objective | Total number of responses | Objective not met | Objective partially met | Objective fully met |
|---|---|---|---|---|
| Discuss the importance of controlling inpatient hyperglycemia. | 17 | 0 | 1 (6) | 16 (94) |
| Describe the current state of inpatient diabetes management. | 17 | 0 | 1 (6) | 16 (94) |
| Utilize guidelines for recognition and triaging of inpatient hyperglycemia. | 17 | 0 | 1 (6) | 16 (94) |
| Demonstrate hyperglycemia management techniques, including insulin dosing. | 16 | 0 | 0 | 16 (100) |
| Access key policies related to diabetes management. | 17 | 0 | 1 (6) | 16 (94) |
| Enter insulin orders using the CPOE system. | 17 | 0 | 1 (6) | 16 (94) |
| List requirements and resources for safe discharge from the hospital. | 17 | 0 | 3 (18) | 14 (82) |
Data are number of responses (percent).
Time Spent on Modules
Most (≥92%) of residents who completed evaluations indicated that the modules took just the right amount of time. The average time residents spent on module 1 was 30 min, module 2 was 28 min, module 3 was 31 min, module 4 was 32 min, module 5 was 27 min, module 6 was 29 min, and time spent on module 7 was 27 min.
Limitations and Future Directions of Study
A future study will be needed to investigate whether the residents were able to successfully apply lessons learned from the CBT curriculum to the real-world hospital setting. Although residents indicated that they viewed the CBT curriculum and its content favorably, it is too early to determine whether this training will have any actual impact on care with improved glucose control, better application of insulin therapy, and increased provider comfort in managing patients with diabetes. The efficacy of the educational program will be included as part of a future investigation.
The goal of the CBT curriculum was to provide a high-level approach to managing diabetes and hyperglycemia cases across the hospitalization spectrum—from admission to discharge. Hence the current CBT curriculum provides only general principles of diabetes and hyperglycemia care, rather than detailed management suggestions about specific situations (e.g., the wide glucose fluctuations that may occur with rapid titration of corticosteroid therapy or use of insulin during various methods of nutritional support). However, the application of the general principles of care outlined in the curriculum should enable residents to more readily adapt to different hospital scenarios.
The CBT curriculum emphasizes instruction in subcutaneous rather than intravenous insulin therapy, and it does not address treatment of diabetic ketoacidosis or hyperglycemic crisis, because these conditions are generally covered elsewhere in the training program. Also, since our institution does not provide inpatient obstetric or pediatric care, the curriculum does not address glucose control during labor and delivery or management in children.
The content of the CBT curriculum will require periodic review and updating, as new data and recommendations for inpatient diabetes management become available from our institution or external sources. For example, national recommendations for glucose targets in critically ill patients were revised2 on the basis of findings from the NICE-SUGAR (Normoglycemia in Intensive Care Evaluation Survival Using Glucose Algorithm Regulation) trial41 and will require changes to the introductory material in module 1 to reflect the controversy of glucose targets. Moreover, our institution is transitioning to a new electronic medical record by 2010, which will require changes in the insulin-ordering simulations presented in module 6.
Finally, other health care professionals, both internal and external to our institution, may find the CBT curriculum relevant to their practice. Our previous data indicated that our own inpatient midlevel practitioners had similar knowledge deficits and expressed barriers to care comparable to those expressed by our residents.21 Offering the CBT curriculum to inpatient nurse practitioners and physician assistants might be another step toward enhancing care of hospitalized diabetes patients. In addition, residents training elsewhere also expressed barriers to inpatient diabetes and hyperglycemia management similar to those voiced by our trainees;22 hence trainees in other institutions may find the CBT curriculum helpful. Deleting our institution-specific quality-of-care data would make the CBT curriculum applicable to a wider audience of health care professionals in other clinical settings and at other institutions.
Conclusions
Multiple regional and national associations and quality improvement organizations have focused attention on inpatient diabetes care. Although treatment of hospital hyperglycemia is strongly emphasized, there is more to inpatient diabetes management than controlling glucose levels. Inpatient diabetes care must span the length of the hospitalization from admission to discharge. For the best outcomes for patients with diabetes and hyperglycemia, hospital-based care should be organized and systematic. The curriculum (and its associated CBT) reviewed here represents an attempt to teach a general set of principles to a specific group of physicians who provide care for a large number of these patients. Its continued use by residents and its implementation for use by other groups of health care professionals should facilitate further refinement of the curriculum content.
Acknowledgements
Editing, proofreading, and reference verification were provided by the Section of Scientific Publications, Mayo Clinic.
Abbreviations
- CBT
computer-based training
- CPOE
computerized physician order entry
- ETC
Education Technology Center
- HbA1c
hemoglobin A1c
References
- 1.Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB. American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27(2):553–591. doi: 10.2337/diacare.27.2.553. [DOI] [PubMed] [Google Scholar]
- 2.Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE. American Association of Clinical Endocrinologists, American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract. 2009;15(4):353–369. doi: 10.4158/EP09102.RA. [DOI] [PubMed] [Google Scholar]
- 3.American College of Endocrinology and American Diabetes Association Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control. Endocr Pract. 2006;12(4):458–468. doi: 10.4158/EP.12.4.458. [DOI] [PubMed] [Google Scholar]
- 4.Braithwaite SS, Magee M, Sharretts JM, Schnipper JL, Amin A, Maynard G. Society of Hospital Medicine Glycemic Control Task Force. The case for supporting inpatient glycemic control programs now: the evidence and beyond. J Hosp Med. 2008;3(Suppl 5):6–16. doi: 10.1002/jhm.350. [DOI] [PubMed] [Google Scholar]
- 5.Institute for Healthcare Improvement. Prevent surgical site infections. http://www.ihi.org/IHI/Programs/Campaign/SSI.htm Accessed March 19, 2009.
- 6.Institute for Healthcare Improvement. Implement effective glucose control. http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm Accessed March 19, 2009.
- 7.The Joint Commission. Inpatient diabetes certification. http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes/ Accessed April 4, 2009.
- 8.Cook CB, Stockton L, Baird M, Osburne RC, Davidson PC, Steed RD, Bode BW, Reid J, McGowan KA. Working to improve care of hospital hyperglycemia through statewide collaboration: the Georgia Hospital Association Diabetes Special Interest Group. Endocr Pract. 2007;13(1):45–50. doi: 10.4158/EP.13.1.45. [DOI] [PubMed] [Google Scholar]
- 9.Society of Hospital Medicine. Glycemic control resource room. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Search_Advanced_Search#template=/CM/HTMLDisplay.cfm#ContentID=14414. Accessed April 3, 2009.
- 10.Umpierrez G, Maynard G. Glycemic chaos (not glycemic control) still the rule for inpatient care: how do we stop the insanity? J Hosp Med. 2006;1(3):141–144. doi: 10.1002/jhm.101. [DOI] [PubMed] [Google Scholar]
- 11.Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998;21(2):246–249. doi: 10.2337/diacare.21.2.246. [DOI] [PubMed] [Google Scholar]
- 12.Schnipper JL, Barsky EE, Shaykevich S, Fitzmaurice G, Pendergrass ML. Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital. J Hosp Med. 2006;1(3):145–150. doi: 10.1002/jhm.96. [DOI] [PubMed] [Google Scholar]
- 13.Knecht LA, Gauthier SM, Castro JC, Schmidt RE, Whitaker MD, Zimmerman RS, Mishark KJ, Cook CB. Diabetes care in the hospital: is there clinical inertia? J Hosp Med. 2006;1(3):151–160. doi: 10.1002/jhm.94. [DOI] [PubMed] [Google Scholar]
- 14.Cook CB, Castro JC, Schmidt RE, Gauthier SM, Whitaker MD, Roust LR, Argueta R, Hull BP, Zimmerman RS. Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2(4):203–211. doi: 10.1002/jhm.188. [DOI] [PubMed] [Google Scholar]
- 15.Institute for Safe Medication Practices. Complexity of insulin therapy has risen sharply in the past decade. ISMP Medication Safety Alert. 2004;3:1. [Google Scholar]
- 16.Considering insulin pens for routine hospital use? Institute for Safe Medication Practices. http://www.ismp.org/Newsletters/acutecare/articles/20080508.asp. Accessed October 27, 2009.
- 17.Institute for Safe Medication Practices. ISMP's list of high-alert medications. http://www.ismp.org/Tools/highalertmedications.pdf. Accessed March 19, 2009.
- 18.Cook CB. Creating “glycemic order” out of “glycemic chaos” [letter] J Hosp Med. 2006;1:383–385. [Google Scholar]
- 19.Cook CB, Zimmerman RS, Gauthier SM, Castro JC, Jameson KA, Littman SD, Magallanez JM. Understanding and improving management of inpatient diabetes mellitus: the Mayo Clinic Arizona experience. J Diabetes Sci Technol. 2008;2(6):925–931. doi: 10.1177/193229680800200602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cook CB, McNaughton DA, Braddy CM, Jameson KA, Roust LR, Smith SA, Roberts DL, Thomas SL, Hull BP. Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians. Endocr Pract. 2007;13(2):117–124. doi: 10.4158/EP.13.2.117. [DOI] [PubMed] [Google Scholar]
- 21.Cook CB, Jameson KA, Hartsell ZC, Boyle ME, Leonhardi BJ, Farquhar-Snow M, Beer KA. Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners. Diabetes Educ. 2008;34(1):75–83. doi: 10.1177/0145721707311957. [DOI] [PubMed] [Google Scholar]
- 22.Cheekati V, Osburne RC, Jameson KA, Cook CB. Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital. J Hosp Med. 2009;4(1):E1–E8. doi: 10.1002/jhm.383. [DOI] [PubMed] [Google Scholar]
- 23.Hammoud M, Gruppen L, Erickson SS, Cox SM, Espey E, Goepfert A, Katz NT. Association of Professors of Gynecology and Obstetrics Undergraduate Medical Education Committee. To the point: reviews in medical education online computer assisted instruction materials. Am J Obstet Gynecol. 2006;194(4):1064–1069. doi: 10.1016/j.ajog.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 24.Greenhalgh T. Computer assisted learning in undergraduate medical education. BMJ. 2001;322(7277):40–44. doi: 10.1136/bmj.322.7277.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zucker S, White JA, Fabri PJ, Khonsari LS. Instructional intranets in graduate medical education. Acad Med. 1998;73(10):1072–1075. doi: 10.1097/00001888-199810000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Bell DS, Fonarow GC, Hays RD, Mangione CM. Self-study from web-based and printed guideline materials. A randomized, controlled trial among resident physicians. Ann Intern Med. 2000;132(12):938–946. doi: 10.7326/0003-4819-132-12-200006200-00003. [DOI] [PubMed] [Google Scholar]
- 27.Minasian-Batmanian LC. Guidelines for developing an online learning strategy for your subject. Med Teach. 2002;24(6):645–647. doi: 10.1080/0142159021000063998. [DOI] [PubMed] [Google Scholar]
- 28.McKimm J, Jollie C, Cantillon P. ABC of learning and teaching: web based learning. BMJ. 2003;326(7394):870–873. doi: 10.1136/bmj.326.7394.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cook DA, Dupras DM. A practical guide to developing effective web-based learning. J Gen Intern Med. 2004;19(6):698–707. doi: 10.1111/j.1525-1497.2004.30029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berman NB, Fall LH, Maloney CG, Levine DA. Computer-assisted instruction in clinical education: a roadmap to increasing CAI implementation. Adv Health Sci Educ Theory Pract. 2008;13(3):373–383. doi: 10.1007/s10459-006-9041-3. [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Association. Standards of medical care in diabetes—2009. Diabetes Care. 2009;32(Suppl 1):S13–S61. doi: 10.2337/dc09-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Queale WS, Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus. Arch Intern Med. 1997;157(5):545–552. [PubMed] [Google Scholar]
- 33.Gearhart JG, Duncan JL, 3rd, Replogle WH, Forbes RC, Walley EJ. Efficacy of sliding-scale insulin therapy: a comparison with prospective regimens. Fam Pract Res J. 1994;14(4):313–322. [PubMed] [Google Scholar]
- 34.Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, Puig A, Mejia R. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial) Diabetes Care. 2007;30(9):2181–2186. doi: 10.2337/dc07-0295. [DOI] [PubMed] [Google Scholar]
- 35.Maynard G, Lee J, Phillips G, Fink E, Renvall M. Improved inpatient use of basal insulin, reduced hypoglycemia, and improved glycemic control: effect of structured subcutaneous insulin orders and an insulin management algorithm. J Hosp Med. 2009;4(1):3–15. doi: 10.1002/jhm.391. [DOI] [PubMed] [Google Scholar]
- 36.Schnipper JL, Ndumele CD, Liang CL, Pendergrass ML. Effects of a subcutaneous insulin protocol, clinical education, and computerized order set on the quality of inpatient management of hyperglycemia: results of a clinical trial. J Hosp Med. 2009;4(1):16–27. doi: 10.1002/jhm.385. [DOI] [PubMed] [Google Scholar]
- 37.Cook CB, Boyle ME, Cisar NS, Miller-Cage V, Bourgeois P, Roust LR, Smith SA, Zimmerman RS. Use of continuous subcutaneous insulin infusion (insulin pump) therapy in the hospital setting: proposed guidelines and outcome measures. Diabetes Educ. 2005;31(6):849–857. doi: 10.1177/0145721705281563. [DOI] [PubMed] [Google Scholar]
- 38.The Joint Commission. 2008 National patient safety goals: disease-specific care program. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_dsc_npsgs.htm. Accessed April 4, 2009.
- 39.U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services. Medicare releases solicitations for quality improvement organizations' 9th statement of work. http://www.cms.hhs.gov/apps/media/press/factsheet.asp?Counter=2880&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&srchOpt=0&srchData=&keywordType=All&chkNewsType=6&intPage=&showAll=&pYear=&year=&desc=false&cboOrder=date. Accessed April 4, 2009.
- 40.Cook CB, Seifert KM, Hull BP, Hovan MJ, Charles JC, Miller-Cage V, Boyle ME, Harris JK, Magallanez JM, Littman SD. Inpatient to outpatient transfer of diabetes care: planing for an effective hospital discharge. Endocr Pract. 2009;15(3):263–269. doi: 10.4158/EP.15.3.263. [DOI] [PubMed] [Google Scholar]
- 41.NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hébert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]


