Abstract
Context
Racial differences in survival have not been previously studied after in-hospital cardiac arrest, an event for which access to care is not likely to influence treatment.
Objectives
To estimate racial differences in survival for patients with in-hospital cardiac arrests and examine the association of sociodemographic and clinical factors and the admitting hospital with racial differences in survival.
Design, Setting, and Patients
Cohort study of 10 011 patients with cardiac arrests due to ventricular fibrillation or pulseless ventricular tachycardia enrolled between January 1, 2000, and February 29, 2008, at 274 hospitals within the National Registry of Cardiopulmonary Resuscitation.
Main Outcome Measures
Survival to hospital discharge; successful resuscitation from initial arrest and postresuscitation survival (secondary outcome measures).
Results
Included were 1883 black patients (18.8%) and 8128 white patients (81.2%). Rates of survival to discharge were lower for black patients (25.2%) than for white patients (37.4%) (unadjusted relative rate [RR], 0.73; 95% confidence interval [CI], 0.67–0.79). Unadjusted racial differences narrowed after adjusting for patient characteristics (adjusted RR, 0.81 [95% CI, 0.75–0.88]; P<.001) and diminished further after additional adjustment for hospital site (adjusted RR, 0.89 [95% CI, 0.82–0.96]; P=.002). Lower rates of survival to discharge for blacks reflected lower rates of both successful resuscitation (55.8% vs 67.4% for whites; unadjusted RR, 0.84 [95% CI, 0.81–0.88]) and postresuscitation survival (45.2% vs 55.5% for whites; unadjusted RR, 0.85 [95% CI, 0.79–0.91]). Adjustment for the hospital site at which patients received care explained a substantial portion of the racial differences in successful resuscitation (adjusted RR, 0.92 [95% CI, 0.88–0.96]; P<.001) and eliminated the racial differences in postresuscitation survival (adjusted RR, 0.99 [95% CI, 0.92–1.06]; P=.68).
Conclusions
Black patients with in-hospital cardiac arrest were significantly less likely to survive to discharge than white patients, with lower rates of survival during both the immediate resuscitation and postresuscitation periods. Much of the racial difference was associated with the hospital center in which black patients received care.
Survival Following In-hospital cardiac arrest represents a unique opportunity to examine racial disparities in medical care and outcomes. In-hospital cardiac arrest is an emergency condition tightly linked to processes of care and for which there is little debate regarding clinical appropriateness of treatment in eligible patients.1 Furthermore, because patients are already in the hospital, potential racial differences in access to care or medical compliance are not likely to confound the association between the care delivered and patients’ outcomes.
To date, potential disparities in survival outcomes after in-hospital cardiac arrest have not been systematically described. If differences in survival by race exist and are mediated primarily by lower quality care and survival at hospitals with a higher concentration of cardiac arrest patients who are black, these findings would provide a conceptual framework for targeting interventions to improve resuscitation quality and reduce racial disparities in cardiac outcomes.
We used data from the National Registry of Cardiopulmonary Resuscitation (NRCPR) to examine whether racial differences exist in survival for patients with in-hospital cardiac arrest due to ventricular arrhythmia, and if so, to estimate the relative role of the hospital in explaining these differences. We also explored whether differences in survival by race were associated with differences in successful resuscitation immediately at the time of cardiac arrest or during postresuscitation phases of care.
METHODS
Study Design
The NRCPR is a large prospective registry of patients with in-hospital cardiac arrest, and its study design has been previously described in detail.2 Briefly, cardiac arrest is defined as the absence of a palpable central pulse, apnea, and unresponsiveness. Consecutive patients with cardiac arrests and without do-not-resuscitate (DNR) orders are screened by specially trained quality-improvement personnel at participating hospitals. To ensure adequate capture, cases are identified by multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for use of resuscitation medications.1,2
Data on cardiac arrests are collected using standardized Utstein-style definitions to ensure uniform reporting.3–7 Data accuracy in the NRCPR is ensured by rigorous certification of research staff to ensure operational definition compliance prior to data acceptance, a periodic reabstraction process, 2 and use of standardized software to ensure data completeness and accuracy.2,8
NRCPR Study Population
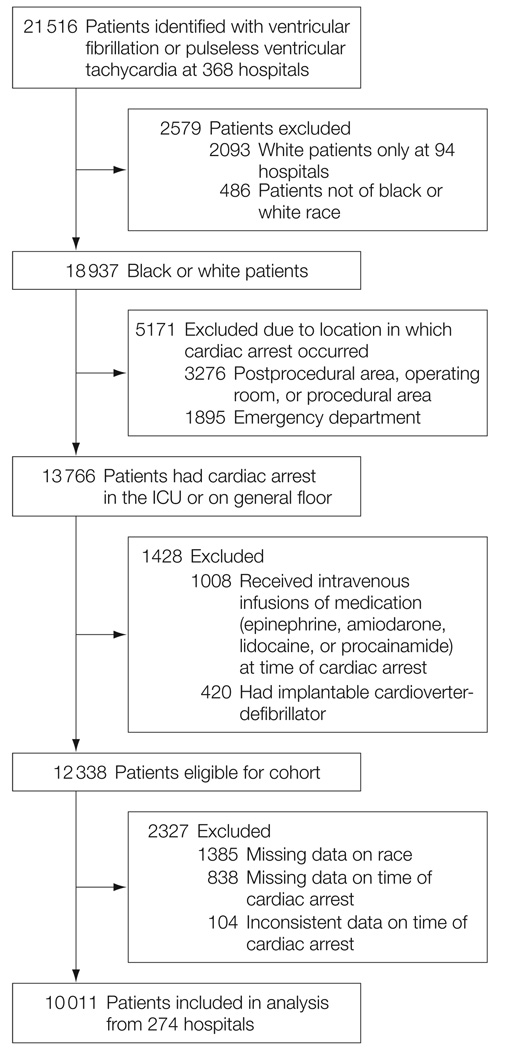
Our analyses included acute care hospitals that provided at least 6 months of data between January 1, 2000, and February 29, 2008. Within these hospitals, we identified 21 516 patients aged 18 years or older with an index in-hospital cardiac arrest for which the first identifiable rhythm was ventricular fibrillation or pulseless ventricular tachycardia (FIGURE). Patient race was self-identified and was abstracted from the medical records by NRCPR staff. We limited our study analyses to comparisons between patients of black and white race because of the small proportion of patients represented by other races (n=486 [2.3%] who were excluded).
Figure. Study Cohort.
ICU indicates intensive care unit.
Study Outcomes
There were 3 survival outcomes of interest in this study. The primary outcome was survival to hospital discharge. To better understand which phase of resuscitation care was associated with racial differences in survival to discharge, the secondary outcomes were return of spontaneous circulation (ROSC) for at least 20 minutes during the acute resuscitation and postresuscitation survival among those patients with ROSC. For each of these 3 survival outcomes, the degree to which patient factors, the hospital to which a patient was admitted, and hospital process measures were associated with observed racial differences in survival was examined.
In addition, neurological status was assessed among patients surviving to hospital discharge using cerebral performance category (CPC) scores.9 For our analyses, CPC scores were dichotomized into those with and without major neurological disability. The CPC data were available in 86% of survivors, with no racial bias in rates of missingness (14% for both blacks and whites; P=.70).
Study Variables
The primary independent variable was patient race. Patient factors collected other than race included demographics (age and sex), initial cardiac rhythm, and comorbidities or medical conditions present prior to cardiac arrest (congestive heart failure, myocardial infarction, or diabetes mellitus; renal, hepatic, or respiratory insufficiency; baseline evidence of motor, cognitive, or functional deficits [central nervous system depression]; acute stroke; pneumonia; hypotension; sepsis; major trauma; and requirement for hemodialysis).
Hospital factors collected included the hospital’s geographic region, licensed bed volume (<250, 250–499, ≥500 inpatient beds), and academic training program status (no training program, residency program only, residency and fellowship programs). Hospital process variables included the use of a hospitalwide cardiopulmonary arrest alert, use of an organized hospital code team, defibrillation time, time of cardiac arrest (work hours: 8 am to 5 pm; after hours: 5 pm to 8 am or weekend), and cardiac arrest location (not monitored, telemetry, or intensive care unit [ICU]). Time to defibrillation was evaluated as both a continuous and categorical variable (delayed, >2 minutes vs not delayed, ≤2 minutes) based on current guidelines.10,11
Statistical Analyses
Baseline differences between black and white patients were evaluated using t tests for continuous variables and χ2 tests for categorical variables. To examine the extent to which racial differences in rates of survival to discharge were attenuated by patient and hospital factors, we constructed a sequence of multivariable models to cumulatively adjust for study covariates and to quantify the incremental contribution of each class of variables as follows: (1) demographics other than race, (2) clinical characteristics, (3) hospital factors, (4) hospital site, and (5) hospital process variables with a potential effect on the resuscitation process.
The initial steps of adjustment (steps 1–3) were performed using generalized estimating equations, which accounts for clustering of outcomes within hospital but estimates population-average effects across all hospitals in the study. Following these steps, we then explicitly adjusted for the hospital site (step 4) and hospital process variables (step 5) using 2-level hierarchical models. In these models, hospital site and the proportion of cardiac arrest patients who were black at each hospital were evaluated as random effects, and their estimates represent within-hospital differences by race, fully adjusting for all observable and unobservable between-hospital differences.12 Because survival rates exceeded 10%, we used log-binomial or modified Poisson regression models at all steps, which estimate a relative rate (RR) directly.13,14
A priori secondary analyses examined whether differences in survival to discharge by race were associated with racial differences in ROSC, postresuscitation survival (as determined by survival to discharge among those with ROSC), or both. To accomplish this, separate sequential multivariable models for each were constructed in a similar fashion to those described above. As an additional exploratory analysis, the total number of attempted defibrillations and the duration of resuscitation were compared between black and white patients who died during the initial resuscitation (ie, no ROSC). These outcomes were evaluated as surrogate measures of treatment intensity.
For each analysis, the null hypothesis was evaluated at a 2-sided significance level of .05 and 95% confidence intervals (CIs) were calculated. Given the sample size of 10 011 patients, of whom 19% were black and 35% survived to hospital discharge, this study had 90% power to detect, at a 2-sided significance level of .05, a minimum crude RR difference between black and white patients of 0.91. All statistical analyses were performed with SAS version 9.1 (SAS Institute Inc, Cary, North Carolina) and R version 2.7.0.15 The institutional review board of Saint Luke’s Mid America Heart Institute approved this study and waived the requirement for informed consent.
RESULTS
Sample Characteristics
The cohort included 10 011 patients from 274 hospitals who underwent defibrillation for a cardiac arrest. The mean (SD) age in the study population was 66.6 (14.5) years, 6021 were men (60.1%), and 1883 were black (18.8%). Ventricular fibrillation was the first identified rhythm in nearly two-thirds of cases, and 5 in 6 patients were monitored in the ICU or on a telemetry unit at the time of cardiac arrest. Nearly 4 in 5 patients had a cardiac arrest in a hospital with an academic training program, and 2 in 5 patients had a cardiac arrest in a hospital with fewer than 250 beds.
Several patient and hospital factors differed by race (TABLE 1). White cardiac arrest patients were older, were more likely to be male, were more likely to be admitted with a cardiac admitting diagnosis (especially congestive heart failure or myocardial infarction), and were more likely to be admitted at a nonacademic hospital. Black patients were more likely to have ventricular fibrillation as their initial presenting arrest rhythm, were sicker at the time of cardiac arrest (higher rates of renal insufficiency, diabetes mellitus, baseline central nervous system depression, acute stroke, pneumonia, sepsis, major trauma, and requirement for hemodialysis), and were more likely to be admitted to a hospital unit not monitored, to a hospital with greater than 500 beds, and in the south-eastern United States.
Table 1.
Description of Study Population by Racea
| Total (N = 10 011) |
White (n = 8128) |
Black (n = 1883) |
P Value |
||
|---|---|---|---|---|---|
| Demographic Characteristics | |||||
| Age, mean (SD), y | 66.6 (14.5) | 67.8 (13.9) | 61.2 (16.5) | <.001 | |
| Male sex | 6021 (60.1) | 5057 (62.2) | 964 (51.2) | <.001 | |
| Clinical Characteristics | |||||
| Cardiac admitting diagnosis | 5907 (59.0) | 5046 (62.1) | 861 (45.7) | <.001 | |
| Ventricular fibrillation | 6515 (65.1) | 5246 (64.5) | 1269 (67.4) | .02 | |
| Characteristics Prior to Cardiac Arrest | |||||
| CHF during admission | 2503 (25.0) | 2082 (25.6) | 421 (22.4) | .003 | |
| Prior CHF before admission | 2676 (26.7) | 2192 (27.0) | 484 (25.7) | .26 | |
| MI during admission | 2783 (27.8) | 2456 (30.2) | 327 (17.4) | <.001 | |
| Prior MI before admission | 2473 (24.7) | 2180 (26.8) | 293 (15.6) | <.001 | |
| Hypotension | 2448 (24.5) | 2014 (24.8) | 434 (23.0) | .12 | |
| Respiratory insufficiency | 3571 (35.7) | 2881 (35.4) | 690 (36.6) | .33 | |
| Renal insufficiency | 3074 (30.7) | 2270 (27.9) | 804 (42.7) | <.001 | |
| Hepatic insufficiency | 593 (5.9) | 467 (5.7) | 126 (6.7) | .12 | |
| Diabetes mellitus | 3115 (31.1) | 2438 (30.0) | 677 (36.0) | <.001 | |
| Baseline CNS depression | 1082 (10.8) | 821 (10.1) | 261 (13.9) | <.001 | |
| Acute stroke | 388 (3.9) | 286 (3.5) | 102 (5.4) | <.001 | |
| Acute pneumonia | 1050 (10.5) | 829 (10.2) | 221 (11.7) | .05 | |
| Sepsis | 1159 (11.6) | 834 (10.3) | 325 (17.3) | <.001 | |
| Major trauma | 230 (2.3) | 173 (2.1) | 57 (3.0) | .02 | |
| History of pacemaker | 968 (9.7) | 857 (10.5) | 111 (5.9) | <.001 | |
| Hemodialysis | 398 (4.0) | 285 (3.5) | 113 (6.0) | <.001 | |
| Process Factors | |||||
| Level of monitoring | |||||
| Intensive care unit | 6270 (62.6) | 5123 (63.0) | 1147 (60.9) | <.001 | |
| Telemetry | 2197 (22.0) | 1842 (22.7) | 355 (18.9) | ||
| Not monitored | 1544 (15.4) | 1163 (14.3) | 381 (20.2) | ||
| Arrest response | |||||
| Hospitalwide code-blue alert | 8372 (83.6) | 6828 (84.0) | 1544 (82.0) | .03 | |
| After hours cardiac arrest | 7161 (71.5) | 5809 (71.5) | 1352 (71.8) | .77 | |
| Cardiac arrests in hospital with code team |
9762 (97.5) | 7905 (97.3) | 1857 (98.6) | <.001 | |
| Hospital Factors | |||||
| Geographic location | |||||
| Northeast | 1378 (13.8) | 1138 (14.0) | 240 (12.7) | <.001 | |
| Southeast | 3921 (39.2) | 3006 (37.0) | 915 (48.6) | ||
| Midwest | 2839 (28.4) | 2359 (29.0) | 480 (25.5) | ||
| Southwest | 964 (9.6) | 794 (9.8) | 170 (9.0) | ||
| West | 909 (9.1) | 831 (10.2) | 78 (4.1) | ||
| Total hospital beds | |||||
| <250 | 4178 (41.7) | 3391 (41.7) | 787 (41.8) | <.001 | |
| 250–499 | 3628 (36.2) | 3042 (37.4) | 586 (31.1) | ||
| ≥500 | 2205 (22.0) | 1695 (20.9) | 510 (27.1) | ||
| Academic hospital program | |||||
| Fellowship training | 6293 (62.9) | 4966 (61.1) | 1327 (70.5) | <.001 | |
| Residency training | 1559 (15.6) | 1313 (16.2) | 246 (13.1) | ||
| No training | 2159 (21.6) | 1849 (22.7) | 310 (16.5) | ||
Abbreviations: CHF, congestive heart failure; CNS, central nervous system; MI, myocardial infarction.
Values are expressed as number (percentage) unless otherwise indicated.
Survival to Discharge
Black patients had lower overall rates of survival to discharge compared with white patients (25.2% vs 37.4%; unadjusted RR, 0.73 [95% CI, 0.67–0.79]; P<.001), and lower rates of survival when stratified by hospital unit type (ICU, telemetry, not monitored) (TABLE 2). These differences narrowed after adjusting for differences in patient characteristics (adjusted RR, 0.81 [95% CI, 0.75–0.88]; P<.001; TABLE 3). Additional adjustment for the hospital to which the patient was admitted further attenuated racial differences in rates of survival to discharge (adjusted RR, 0.89 [95% CI, 0.82–0.96]; P=.002). However, further adjustment for hospital process variables did not meaningfully attenuate residual differences, and black patients remained 10% less likely to survive to hospital discharge.
Table 2.
Study Outcomes by Racea
| White (n = 8128) |
Black (n = 1883) |
P Value |
|
|---|---|---|---|
| Overall survival to discharge | 3043 (37.4) | 475 (25.2) | <.001 |
| By hospital unit | |||
| ICU | 1902/5123 (37.1) | 266/1147 (23.2) | <.001 |
| Telemetry unit | 858/1842 (46.6) | 134/355 (37.7) | .002 |
| Unit not monitored | 283/1163 (24.3) | 75/381 (19.7) | .06 |
| Favorable neurological outcomesb | 1543/2606 (59.2) | 213/410 (52.0) | .02 |
| Acute resuscitation outcomes | |||
| Return of spontaneous circulation | 5478 (67.4) | 1051 (55.8) | <.001 |
| Delayed defibrillation (>2 min) | 1415 (17.4) | 414 (22.0) | <.001 |
| Aggressiveness of resuscitation, median (IQR)c | |||
| No. of defibrillations | 3 (2–6) | 4 (2–6) | .28 |
| Duration of resuscitation | 23 (15–33) | 22 (15–32) | .42 |
| Postresuscitation survivald | 3041/5478 (55.5) | 475/1051 (45.2) | <.001 |
Abbreviations: ICU, intensive care unit; IQR, interquartile range.
Values are expressed as number (percentage) or number/total (percentage) unless otherwise indicated.
Among 3016 patients surviving to discharge with available cerebral performance category assessments and defined as discharge without major neurological deficits.
Assessed among the 3482 patients who died during resuscitation (no return of spontaneous circulation).
Assessed among the 6529 patients who survived initial resuscitation (return of spontaneous circulation).
Table 3.
Association Between Black Race and Likelihood of Survival and Favorable Neurological Outcome in Patients With Cardiac Arrest
| RR (95% CI) | P Value | Survival Difference Explained, %a | |
|---|---|---|---|
| Survival to discharge | |||
| Unadjustedb | 0.73 (0.67–0.79) | <.001 | NA |
| Adjusted for age and sexb | 0.70 (0.64–0.76) | <.001 | 0 |
| Plus clinical characteristicsb | 0.81 (0.75–0.88) | <.001 | 30 |
| Plus hospital characteristicsb | 0.82 (0.76–0.89) | <.001 | 33 |
| Adjusted for age, sex, clinical characteristics, and hospitalc | 0.89 (0.82–0.96) | .002 | 59 |
| Plus processes of care and time to defibrillationc,d | 0.90 (0.83–0.96) | .004 | 63 |
| Survival without major neurological deficite | |||
| Unadjustedb | 0.88 (0.78–0.98) | .02 | NA |
| Adjusted for age and sexb | 0.85 (0.76–0.95) | .006 | 0 |
| Plus clinical characteristicsb | 0.91 (0.82–1.02) | .09 | 25 |
| Plus hospital characteristicsb | 0.91 (0.81–1.01) | .08 | 25 |
| Adjusted for age, sex, clinical characteristics, and hospitalc | 0.94 (0.83–1.06) | .35 | 50 |
| Plus processes of care and time to defibrillationc,d | 0.94 (0.83–1.06) | .35 | 50 |
| Return of spontaneous circulation | |||
| Unadjustedb | 0.84 (0.81–0.88) | <.001 | NA |
| Adjusted for age and sexb | 0.84 (0.80–0.87) | <.001 | 0 |
| Plus clinical characteristicsb | 0.88 (0.84–0.92) | <.001 | 25 |
| Plus hospital characteristicsb | 0.89 (0.85–0.93) | <.001 | 31 |
| Adjusted for age, sex, clinical characteristics, and hospitalc | 0.92 (0.88–0.96) | <.001 | 50 |
| Plus processes of care and time to defibrillationc,d | 0.92 (0.88–0.97) | <.001 | 50 |
| Postresuscitation survival | |||
| Unadjustedb | 0.85 (0.79–0.91) | <.001 | NA |
| Adjusted for age and sexb | 0.83 (0.77–0.89) | <.001 | 0 |
| Plus clinical characteristicsb | 0.90 (0.84–0.96) | .002 | 33 |
| Plus hospital characteristicsb | 0.91 (0.85–0.97) | .007 | 40 |
| Adjusted for age, sex, clinical characteristics, and hospitalc | 0.99 (0.92–1.06) | .77 | 93 |
| Plus processes of care and time to defibrillationc,d | 0.99 (0.92–1.06) | .68 | 93 |
Abbreviations: CI, confidence interval; NA, data not applicable; RR, rate ratio.
Determined using the formula: 100×([RR of adjusted model−RR of unadjusted model]/[1−RR of unadjusted model]).
Indicates population–average estimates using generalized estimating equations.
Indicates hospital–specific estimates using hierarchical models.
Time to defibrillation as a continuous variable. Results were similar when time to defibrillation was evaluated as a categorical variable (≤2 vs >2 minutes).
Favorable neurological status was defined as a cerebral performance category score of 1 (ie, without major neurological deficits) among patients surviving to hospital discharge.
To examine the association between hospital site and racial differences, hospitals were stratified into quintiles by their proportion of black cardiac arrest patients. Most black cardiac arrest patients were concentrated in hospitals with the lowest overall rates of survival to discharge (TABLE 4). We also examined racial differences in survival to discharge over time and in favorable neurological outcomes. Notably, racial differences did not decrease over time during the 8 years of this study (P=.65 for trend). However, there were racial differences in favorable neurological outcomes among patients surviving to discharge (Table 2), which were partly attenuated after adjusting for patient and hospital factors (Table 3).
Table 4.
Survival to Discharge After In-Hospital Cardiac Arresta
| No. | Patient Survival to Discharge, % (95% CI) | ||||||
|---|---|---|---|---|---|---|---|
| Hospital Quintile | Hospitals | Patients | Black Patients | Mean % (Range)b |
All | Blacks | Whites |
| Lowest | 50 | 2957 | 93 | 3.4 (0.9–5.8) | 41.2 (39.4–42.9) | 29.0 (19.6–38.4) | 41.6 (39.7–43.4) |
| Second | 54 | 1838 | 167 | 8.9 (5.9–11.9) | 37.2 (35.0–39.4) | 31.1 (24.0–38.2) | 37.8 (35.5–40.1) |
| Third | 60 | 1891 | 314 | 16.5 (12.5–20.3) | 35.7 (33.5–37.9) | 30.3 (25.1–35.4) | 36.8 (34.4–39.2) |
| Fourth | 56 | 1815 | 524 | 28.8 (20.5–38.8) | 29.5 (27.4–31.6) | 22.3 (18.8–25.9) | 32.5 (29.9–35.0) |
| Highest | 54 | 1510 | 785 | 55.4 (39.7–87.5) | 26.9 (24.6–29.1) | 23.4 (20.5–26.4) | 30.6 (27.3–34.0) |
| Total | 274 | 10 011 | 1883 | 22.8 (0.9–87.5) | 35.1 (34.2–36.1) | 25.2 (23.3–27.2) | 37.4 (36.4–38.5) |
Abbreviation: CI, confidence interval.
Although racial differences in survival were seen within each hospital quintile, black patients were primarily concentrated in hospitals with the lowest rates of survival to discharge for cardiac arrests (P<.001 for trend comparing mean hospital survival rate for all cardiac arrests across quintiles).
Indicates average hospital percentage of cardiac arrest patients who were black.
Acute Resuscitation Outcomes
Rates of delayed defibrillation were higher for black patients (22.0%) than for white patients (17.4%). In contrast, among patients who did not survive the initial resuscitation, the number of attempted defibrillations and the median resuscitation duration did not differ by race (Table 2). Rates of ROSC were lower among black patients (55.8% vs 67.4% for whites). These differences were attenuated after adjusting for patient factors (adjusted RR, 0.88 [95% CI, 0.84–0.92]; Table 3). Adjustment for the hospital to which the patient was admitted led to a further attenuation of racial differences in rates of ROSC (adjusted RR, 0.92; 95% CI, 0.88–0.96), while additional adjustment for hospital process variables did not further diminish racial differences.
Postresuscitation Survival
Among the 6529 patients who survived the initial resuscitation, black patients had lower rates of survival to hospital discharge (45.2% vs 55.5% for whites; unadjusted RR, 0.85 [95% CI, 0.79–0.91]). The racial difference in postresuscitation survival was eliminated after multivariable adjustment (adjusted RR, 0.99 [95% CI, 0.92–1.06]), and was largely explained by the hospital site at which patients received postresuscitation care (Table 3).
COMMENT
In this large, multisite registry of in-hospital cardiac arrests, black patients had a 27% lower RR and a 12% lower absolute rate of survival to hospital discharge than white patients. These unadjusted survival differences by race were, in large part, attributable to black patients being more likely to receive treatment at hospitals with worse outcomes. In addition, we found that survival differences by race were associated with disparities in care during both the acute resuscitation phase and after resuscitation. Collectively, these findings suggest that strategies to eliminate racial disparities in survival after in-hospital cardiac arrest are not likely to succeed unless they are accompanied by successful identification and implementation of interventions that improve resuscitation survival in those poorly performing hospitals in which black patients are more likely to receive care.
While prior studies have demonstrated racial differences in use and treatment outcomes for a variety of nonemergency procedures and conditions,16–20 the source of these differences have been rarely identified. Although underuse of services in blacks may account for racial differences in these studies, overuse in whites and patient preferences also have been postulated to account for these differences, particularly in areas in which clinical appropriateness is unclear.21–23
These issues are less relevant for patients with cardiac arrest who are eligible for resuscitation, leading our findings to raise particularly unique concerns. Additionally, we describe the role of the hospital providing resuscitation care in explaining these differences and identified differences in both the acute resuscitation phase—which is not likely to be due to overuse of treatment or patient preferences during an emergency response—and during postresuscitation care.
For the acute resuscitation phase, although black race has previously been shown to be a predictor of delays in defibrillation response time,1 we did not find that additional within-hospital adjustment for defibrillation response time attenuated racial differences in ROSC after adjusting for the hospital to which a patient was admitted. This suggests that black patients were more likely to have cardiac arrests in hospitals with higher rates of delays in defibrillation time. Importantly, there was no evidence of significant racial differences in available measures of resuscitation aggressiveness, such as the number of attempted defibrillations and total treatment time, to suggest a source of clinician bias during the acute resuscitation phase.
There were also large observed differences by race in postresuscitation survival. The hospital center effect accounted for 65% of the explained variation (60% of 93%), with no meaningful residual racial differences after adjustment. Unlike the outcome of ROSC, for which patient preferences and appropriateness of care are not likely to influence treatment decisions during an emergency resuscitation, postresuscitation survival may be affected by these factors.
However, racial differences in postresuscitation survival are not likely to be explained by higher rates of newly initiated DNR status in black patients in the postcardiac arrest setting because prior studies have found that hospitalized black patients are actually less likely to choose DNR status than nonwhite patients24,25 and are more likely to continue terminal end-of-life care in the ICU.26 Yet, significant hospital variation in mortality exists for ICU patients.27–29 Therefore, whether lower rates of postresuscitation survival in blacks are due to lower quality ICU expertise, less aggressive use of postresuscitation therapies (eg, hypothermia, cardiac catheterization),30 or other characteristics of the hospital to which they are more likely to be admitted, requires further study.
Nonetheless, there remained a substantial and unexplained lower rate of survival to hospital discharge among black patients. These residual differences were associated with unexplained racial differences in rates of ROSC because residual differences in postresuscitation survival were minimal. Because previously established mediators of ROSC, including defibrillation time,1 did not account for residual racial differences, further research is needed to determine which other factors may be responsible, such as unmeasured hospital resuscitation process variables (time to subsequent defibrillations, quality of chest compressions and ventilation, and number and timing of resuscitation medications), physiological responses to cardiac arrest that differ by race, or clinician and/or institutional bias. In addition, although our use of hierarchical models accounted for between-hospital differences in rates of DNR status on admission, potential within-hospital differences by race may exist,31 which could yield a sicker, older black population for each hospital in our analyses.
There are several issues to consider in interpreting the results of our findings. While we found that the hospital effect for racial differences for in-hospital cardiac arrests was explained by a greater proportion of black patients receiving care at hospitals with lower rates of survival, this observation may not apply to other health conditions and warrants further study. Because race was abstracted from medical records, there is the potential for misclassification bias, which would likely have been nondifferential and underestimated observed racial differences. The NRCPR does not collect data on a hospital’s postresuscitation resources, such as ICU staffing and expertise. However, our use of hierarchical models controlled for between-hospital effects.
We also did not have data on other resuscitation measures (eg, time to successive shocks and resuscitation medications) and the use of many potential postresuscitation care interventions (eg, hypothermia). Furthermore, we did not assess for clinician bias, which may account for racial differences in treatment, and we were unable to determine whether DNR status varied by race because the NRCPR does not enroll patients with DNR status. Finally, our study population was enrolled from US hospitals that participated in a quality-improvement resuscitation registry and represents about 15% of large hospitals in the United States; therefore, our study findings may not represent cardiac arrest outcomes by race in non-NRCPR hospitals.
In conclusion, we found large racial differences in survival after in-hospital cardiac arrest, with a substantial portion of this racial disparity associated with lower resuscitation and postresuscitation survival in hospitals with high concentrations of black cardiac arrest patients. Strategies to eliminate racial disparities in survival are not likely to succeed unless they improve resuscitation survival and the quality of postresuscitation care in hospitals that are poor performers and in which black patients are more likely to receive care.
Acknowledgments
Funding/Support: The American Heart Association provided funding for the collection and management of the data and reviewed and approved the final manuscript.
Role of the Sponsor: The American Heart Association had no role in the design and conduct of this study, in the analysis or interpretation of the data, or the preparation of the manuscript.
Footnotes
Author Contributions: Dr Chan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Chan, Nallamothu.
Acquisition of data: Chan, Nichol.
Analysis and interpretation of data: Chan, Nichol, Krumholz, Spertus, Jones, Peterson, Rathore, Nallamothu.
Drafting of the manuscript: Chan, Nallamothu.
Critical revision of the manuscript for important intellectual content: Chan, Nichol, Krumholz, Spertus, Jones, Peterson, Rathore, Nallamothu.
Statistical analysis: Chan, Jones.
Obtained funding: Chan.
Study supervision: Chan, Nichol, Krumholz, Spertus, Peterson, Rathore, Nallamothu.
Financial Disclosures: Dr Nichol reported having served as a consultant to Northfield Laboratories; having received travel compensation from INNERcool Inc and Radiant Medical Inc; having received research grant funding from Medtronic and the National Heart, Lung, and Blood Institute; having received equipment donations for overseas medical missions from Medtronic Physio-Control and Laerdal Inc; and having served on advisory boards with the American Heart Association and the Medic One Foundation. Drs Chan, Krumholz, Spertus, Peterson, and Nallamothu and Messrs Jones and Rathore did not report any financial disclosures.
American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators: E. Allen, R. Berg, S. Braithwaite, P. Chan (study author), B. Eigel, R. Geocadin, E. Hunt, K. Kern, T. Mader, D. Magid, M. Mancini, V. Nadkarni, G. Nichol (study author), T. Noel, J. Ornato, M. Peberdy, J. Potts, T. Truitt, and S. Warren.
Disclaimer: Dr Peterson, a JAMA contributing editor, was not involved in the editorial review of or decision to publish this article.
REFERENCES
- 1.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 2.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs I, Nadkarni V, Bahr J, et al. International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110(21):3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 4.Cummins RO, Chamberlain D, Hazinski MF, et al. American Heart Association. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ’Utstein style’. American Heart Association. Circulation. 1997;95(8):2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 5.Cummins RO, Sanders A, Mancini E, Hazinski MF. In-hospital resuscitation: executive summary. Ann Emerg Med. 1997;29(5):647–649. doi: 10.1016/s0196-0644(97)70255-5. [DOI] [PubMed] [Google Scholar]
- 6.Writing Group. Zaritsky A, Nadkarni V, Hazinski MF, et al. Recommended guidelines for uniform reporting of pediatric advanced life support: the pediatric Utstein Style: a statement for healthcare professionals from a task force of the American Academy of Pediatrics, the American Heart Association, and the European Resuscitation Council Writing Group. Circulation. 1995;92(7):2006–2020. doi: 10.1161/01.cir.92.7.2006. [DOI] [PubMed] [Google Scholar]
- 7.Zaritsky A, Nadkarni V, Hazinski MF, et al. Recommended guidelines for uniform reporting of pediatric advanced life support: the pediatric Utstein style: a statement for healthcare professionals from a task force of the American Academy of Pediatrics, the American Heart Association, and the European Resuscitation Council. Resuscitation. 1995;30(2):95–115. doi: 10.1016/0300-9572(95)00884-v. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Ornato JP, Larkin GL, et al. National Registry of Cardiopulmonary Resuscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 9.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 10.Ewy GA, Ornato JP. 31st Bethesda Conference, Emergency Cardiac Care, task force 1: cardiac arrest; J Am Coll Cardiol; 2000. pp. 832–846. [DOI] [PubMed] [Google Scholar]
- 11.Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the “chain of survival” concept: a statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation. 1991;83(5):1832–1847. doi: 10.1161/01.cir.83.5.1832. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein H. Multilevel Statistical Models. London, England: Edward Arnold; 1995. [Google Scholar]
- 13.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 14.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160(4):301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 15.R Development Core Team. R Foundation for Statistical Computing V. R: A language and environment for statistical computing. http://www.R-project.org.
- 16.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 17.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001;135(5):352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 18.Escarce JJ, Epstein KR, Colby DC, Schwartz JS. Racial differences in the elderly’s use of medical procedures and diagnostic tests. Am J Public Health. 1993;83(7):948–954. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaccarino V, Rathore SS, Wenger NK, et al. National Registry of Myocardial Infarction Investigators. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353(7):671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298(13):1525–1532. doi: 10.1001/jama.298.13.1525. [DOI] [PubMed] [Google Scholar]
- 21.Schneider EC, Leape LL, Weissman JS, Piana RN, Gatsonis C, Epstein AM. Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135(5):328–337. doi: 10.7326/0003-4819-135-5-200109040-00009. [DOI] [PubMed] [Google Scholar]
- 22.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation–clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–1544. doi: 10.1056/NEJM200011233432106. 2, 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rathore SS, Krumholz HM. Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med. 2004;141(8):635–638. doi: 10.7326/0003-4819-141-8-200410190-00011. [DOI] [PubMed] [Google Scholar]
- 24.Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE. Racial variation in the use of donot-resuscitate orders. J Gen Intern Med. 1999;14(1):15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders: disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155(19):2056–2062. [PubMed] [Google Scholar]
- 26.Robert Wood Johnson Foundation ICU End-of-Life Peer Group. Barnato AE, Berhane Z, Weissfeld LA, Chang CC, Linde-Zwirble WT, Angus DC. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006;41(6):2219–2237. doi: 10.1111/j.1475-6773.2006.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knaus WA, Wagner DP, Zimmerman JE, Draper EA. Variations in mortality and length of stay in intensive care units. Ann Intern Med. 1993;118(10):753–761. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- 28.Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80(1):30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177(3):279–284. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neumar RW, Nolan JP, Adrie C, et al. Postcardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118(23):2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 31.Degenholtz HB, Arnold RA, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. J Am Geriatr Soc. 2002;50(2):378–381. doi: 10.1046/j.1532-5415.2002.50073.x. [DOI] [PubMed] [Google Scholar]