Introduction
During normal aging, there is a decrease in maximal urine concentrating ability [1-3]. This physiological change was clearly demonstrated by the Baltimore Longitudinal Study of Aging [1]. Rowe and colleagues measured maximal urine concentrating ability in healthy individuals in three age groups: 20−39, 40−59, and 60−79. Individuals aged 60−79 had approximately a 20% reduction in maximum urine osmolality, a 50% decrease in the ability to conserve solute, and a 100% increase in minimal urine flow rate, when compared to the two younger age groups [1]. The change in urine concentrating ability could not be explained by a decrease in glomerular filtration rate [1]. Aged individuals do have a diminished thirst response, but the relationship between vasopressin (also named antidiuretic hormone) secretion and plasma osmolality is preserved and may even be enhanced [3]. Thus, neither a reduction in renal function, as measured by glomerular filtration rate, nor an abnormality in vasopressin secretion, appears to be the mechanism that explains the decrease in urine concentrating ability during aging [1;3;4]. The cloning (reviewed in [5-7]) of many of the key renal medullary water (aquaporins) and solute (sodium and urea) transport proteins that are involved in the urine concentrating mechanism, and the type 2 vasopressin receptor, have resulted in studies into the molecular mechanisms underlying the reduction in urine concentrating ability that occurs during aging.
Urine Concentrating Mechanism
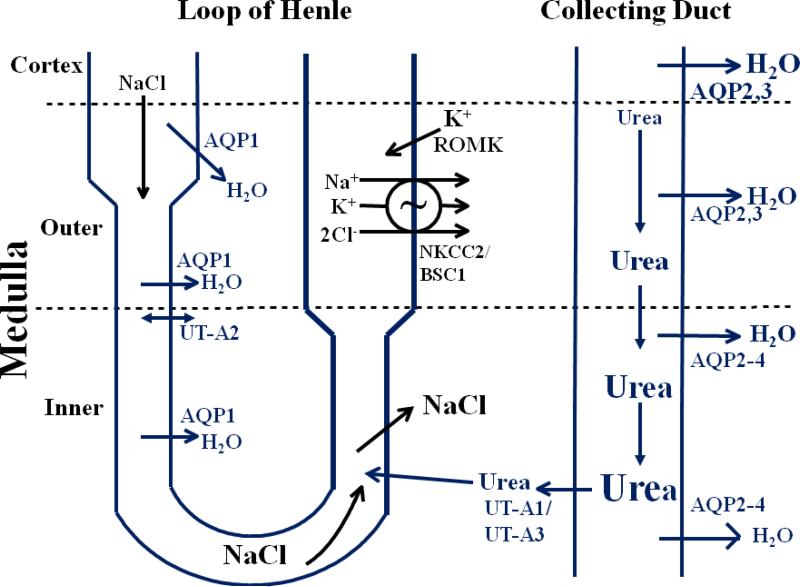
The region of the kidney that is responsible for the generation of concentrated or dilute urine is the medulla (figure 1). To produce a concentrated urine, the collecting duct must be permeable to water and a hypertonic medullary interstitium must be generated by the nephron segments located in the loops of Henle (reviewed in [8;9]). To generate a hypertonic medullary interstitium, a small osmotic gradient is generated at each level of the medulla and then magnified down its length by countercurrent multiplication. In the thick ascending limb of the loop of Henle (in the outer medulla): the NKCC2/BSC1 cotransporter actively reabsorbs Na+, K+, and Cl− across the apical membrane; the K+ that is reabsorbed is secreted back into the lumen via the K+ secretory channel ROMK; resulting in net NaCl reabsorption.
1.
Transport proteins involved in the urinary concentrating mechanism. In the outer medulla, active NaCl reabsorption via NKCC2/BSC1 in the thick ascending limb of the loop of Henle generates a hypertonic medullary interstitium. This concentrates NaCl in the lumen of the thin descending limb of the loop of Henle by osmotically removing water via AQP1 water channels. In the inner medulla, passive NaCl reabsorption exceeds urea secretion. Water is reabsorbed from the collecting duct, in the presence of vasopressin via AQP2 in the apical plasma membrane and AQP3 and AQP4 in the basolateral plasma membrane. Urea is concentrated in the collecting duct lumen until the fluid reaches the urea-permeable terminal inner medullary collecting duct where urea is reabsorbed into the inner medullary interstitium via the UT-A1 and UT-A3 urea transporters.
In contrast to the outer medulla, NaCl is passively reabsorbed in the inner medulla across the thin ascending limb of the loop of Henle (reviewed in [8;9]). The thin ascending limb luminal fluid has a higher concentration of NaCl and a lower concentration of urea than inner medullary interstitial fluid, thereby establishing chemical gradients that favor NaCl reabsorption and urea secretion, provided that the interstitial urea concentration is sufficiently high. NaCl reabsorption exceeds urea secretion in the thin ascending limb, as it has a higher permeability to NaCl than urea, thereby resulting in dilution of the thin ascending limb luminal fluid as it ascends towards the outer medulla.
NaCl reabsorption in both ascending limb portions of the loop of Henle results in both: a hypertonic medullary interstitium; and delivery of a dilute fluid (relative to plasma) to the distal tubule since both ascending limb segments are water impermeable. The collecting duct is impermeable to water in the absence of vasopressin, resulting in excretion of this dilute fluid as dilute urine. However, the collecting duct becomes highly permeable to water in the presence of vasopressin, and if a hypertonic medulla is present, water is reabsorbed resulting in excretion of a concentrated urine (reviewed in [8;9]).
Vasopressin Receptors
There are two types of vasopressin receptors: type 1 and type 2 (reviewed in [10]). The V2-receptor is involved in urinary concentration. It is expressed in the collecting duct, is a G-protein coupled 7 transmembrane spanning receptor, and its activation results in the generation of the second messenger cyclic AMP. The V1-receptor is involved in increasing systemic blood pressure and has two subtypes: V1a and V1b (also called V3). It is expressed in vasculature, liver, and brain, and its activation results in the generation of the second messenger intracellular calcium.
Water reabsorption along the entire collecting duct is regulated by vasopressin binding to the V2-receptor and stimulating cAMP production (reviewed in [5;9;11]). When blood plasma osmolality becomes elevated by water deprivation (or other causes), hypothalamic osmoreceptors, which can sense an increase of as little as 2 mOsm/kg H2O, stimulate vasopressin secretion from the posterior hypothalamus. Vasopressin binds to V2-receptors in the basolateral plasma membrane of collecting duct principal cells and IMCD cells, which stimulates adenylyl cyclase to produce cAMP and in turn activates protein kinase A.
One potential mechanism for the aging-related decrease in urine concentrating ability would be a reduction in V2-receptors in the aged kidney. In rat, a decrease in V2-receptor mRNA abundance has been detected in one study [12] but no effect on V2-receptor mRNA abundance or vasopressin-stimulated cAMP production was detected in other studies [13-15]. Thus, there is conflicting data on the effect of aging on V2-receptor mRNA abundance (and no data on V2-receptor protein abundance).
Aquaporins
At present, there are 13 cloned water channels or aquaporins (AQPs), 6 of which are expressed in the kidney (reviewed in [5;9]). AQP1 is expressed in the proximal tubule and descending limb of the loop of Henle; AQP7 is also expressed in the proximal tubule. AQP2 is expressed in the apical plasma membrane and sub-apical vesicles of the collecting duct and is the “vasopressin-regulated” water channel. AQP3 and APQ4 are expressed in the basolateral plasma membrane of the collecting duct. AQP6 is expressed in intracellular vesicles in the collecting duct in association with H+-ATPase.
The primary mechanism by which vasopressin rapidly regulates water reabsorption in the collecting duct is by regulating the accumulation of AQP2 in the apical plasma membrane (reviewed in [5;9]). Vasopressin regulation involves both AQP2 phosphorylation at serines 256, 261, 264, and 269 [16-19], and regulated trafficking of AQP2 between sub-apical vesicles and the apical plasma membrane (reviewed in [5]). Wade and colleagues [20] originally proposed the “membrane shuttle hypothesis” in 1979, at a time when water channels had not been cloned or identified. They proposed that the (putative) water channels were stored in vesicles and inserted exocytically into the apical plasma membrane in response to vasopressin. After AQP2 was cloned, the “membrane shuttle hypothesis” was confirmed experimentally by Knepper and colleagues in rat inner medullary collecting ducts (reviewed in [5]). The water that is reabsorbed through AQP2 exits the collecting duct principal cells through AQP3 and AQP4. Water reabsorption is stopped when vasopressin-stimulation ends by endocytosing AQP2 back into the cell, where it is recycled into endosomes until the next stimulation by vasopressin (reviewed in [5;9]).
Several studies show that the protein abundance of some AQPs is reduced in the aged rat kidney [13;21], which could contribute to the reduction in concentrating ability during aging. These studies show that AQP2 protein abundance is reduced in 24−30 month-old rats (which are very old rats), when compared to 10 month-old rats, in both the outer and inner medulla [12;13;21]. The abundance of AQP2 that is phosphorylated at serine 256 is also markedly reduced in the older rats [21]; phosphorylation of serines 261, 264, and 269 has not been studied to date. AQP3 protein abundance is also reduced in the inner medulla of 30 month-old rats, compared to 10 month-old rats, but not in the outer medulla [13;21]. Transepithelial water reabsorption across the collecting duct of aged rats is likely to be reduced by the reductions in AQP2 and AQP3 protein abundances. These changes appear to be specific for AQP2 and AQP3 since neither AQP4 nor AQP1 protein abundances differ between 30 and 10 month-old rats [13;21;22].
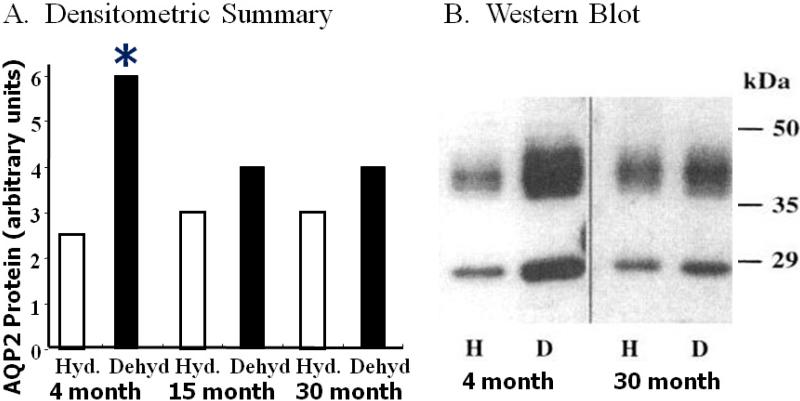
The preceding studies pertain to the basal state, ie. rats receiving food and water ad libitum. An important clinical issue is the response of aged people to dehydration, as elderly individuals are more susceptible to dehydration than younger individuals. To model this situation in rats, we compared the ability of 30 month-old rats to respond to 3 days of water restriction, as compared to the response of 4 month-old rats [23]; 4 month-old rats are young adult animals (figure 2). Both the 30 and 4 month-old rats lost 8% of their body weight and had similar increases in hematocrit, but only the older rats became hypernatremic [23]. AQP2 protein abundance and urine osmolality increased significantly in the 4 month-old rats but not in the 30 month-old rats [12;23;24]. Somewhat surprisingly, AQP2 protein abundance did not increase in dehydrated 15 month-old rats, similar to the response in the 30 month-old rats [24]. AQP2 mRNA abundance also increased in dehydrated 2 month-old rats but not in dehydrated 7 month-old rats [14]. Thus, the age at which concentrating ability is lost in rats may be significantly younger than 24−30 months.
2.
Water restriction does not increase AQP2 protein abundance in 30 or 15 month-old rats. Panel A: densitometic summary. There was no significant difference between hydrated (Hyd.) vs. dehydrated (Dehyd) in the 30 or 15 month-old rats. Asterisk indicates a significant difference between hydrated (Hyd.) vs. dehydrated (Dehyd) 4 month-old rats. Panel B: western blot showing that AQP2 protein (a non-glycosylated 29 kDa band and a glycosylated smear from 35−45 kDa) abundance is not different between hydrated (h) and dehydrated (D) 30 month-old rats but is increased significantly increased in dehydrated (D) vs. hydrated (H) 4 month-old rats. Data from references [23;24].
The preceding studies suggest that an important mechanism that contributes to the reduction in urine concentrating ability in aging is a failure to increase AQP2 protein abundance in the collecting duct in response to vasopressin. To determine whether this defect could be corrected pharmacologically, supra-physiologic concentrations of dDAVP (Desmopressin), a selective V2-receptor agonist that does not increase blood pressure, were administered to 30 and 10 month-old rats [25]. dDAVP administration caused similar increases in urine osmolality and decreases in urine flow rate in 30 and 10 month-old rats, although the maximum urine osmolality in the older rats was lower than in the younger rats [25]. dDAVP administration also increased the protein abundances of both AQP2 and AQP3 [25], suggesting that the reduced maximal urine osmolality in the aged rats is related, at least in part, to the reduced level of these AQP proteins.
Sodium Transporters
NaCl reabsorption through the Na+-K+-2Cl− cotransporter NKCC2/BSC1 is critical for the establishment of the hypertonic medullary interstitium that is needed to concentrate urine (reviewed in [8;9]). NKCC2/BSC1 protein abundance is reduced in older rats in the outer medulla [26]. NKCC2/BSC1 protein abundance is increased by water restriction, but the increase is less than in younger rats [22;26]. The decrease in NKCC2/BSC1 protein will reduce active NaCl reabsorption across the thick ascending limb of the loop of Henle, thereby reducing the generation of a hypertonic medulla and urine concentrating ability.
The protein abundances of the Ǝ and subunits of the epithelial sodium channel ENaC are also reduced [26]. Water restriction resulted in either no increase, or a reduced increase, in the protein abundances of ENaC, the sodium-protein exchanger 3 (NHE3), the Na+-Cl− cotransporter (NCC/TSC), and the sodium pump Na+-K+-ATPase [22;26]. Thus, the reduced maximal urine osmolality in aged rats may also be related, at least in part, to the reduced level of these sodium transporter proteins.
Urea Transporters
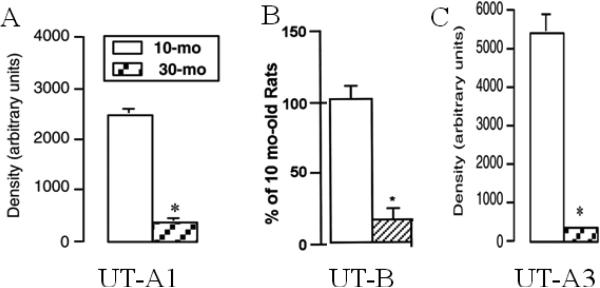
Urea is the second major solute that contributes to medullary interstitial hyperosmolality, and hence to urine concentrating ability [27-29]. Protein malnutrition reduces urine concentrating ability [30-34]. Elderly individuals may be at risk for protein malnutrition, especially those on fixed incomes. Two human (and two rat) urea transporter genes have been cloned: UT-A, which has 6 protein isoforms; and UT-B, which has 2 protein isoforms (reviewed in [6;8;9;35]). UT-A1 protein is expressed in the apical plasma membrane of the inner medullary collecting duct [36]. UT-A3 protein is expressed in the same segment of the collecting duct as UT-A1 [37]. Vasopressin increases urea permeability in the perfused terminal inner medullary collecting duct by increasing UT-A1 and UT-A3 phosphorylation and UT-A1 and UT-A3 accumulation in the apical plasma membrane [37-41]. Vasopressin phosphorylates UT-A1 at serines 486 and 499 [42]. The abundance of both UT-A1 and UT-A3 proteins is significantly reduced in 30 month-old vs. 10 month-old rats [21;43]; phosphorylation of serines 486 and 499 has not been studied to date (figure 3).
3.
Urea transporters are reduced in 30 month-old rats compared to 10 month-old rats. Panel A: UT-A1 protein abundance. Panel B: UT-B protein abundance. Panel C: UT-A3 protein abundance. Asterisk indicates a significant difference between 30 and 10 month-old rats. Data from references [21;43].
Administering a supra-physiologic concentration of dDAVP increases UT-A1 protein abundance in the 30 month-old rats, but to a lesser degree than in the 10 month-old rats [25]. Inner medullary interstitial urea concentration is increased by water restricting the 30 month-old rats, but to a lesser degree than in the 10 month-old rats [43]. The reduced levels of UT-A1 and UT-A3 proteins will decrease urea reabsorption and inner medullary interstitial urea accumulation, thereby reducing the hyperosmolality of the inner medulla and urine concentrating ability. Thus, the reductions in UT-A1 and UT-A3 protein abundances, along with the reductions in AQP and sodium transporter protein abundances (discussed above), likely contribute to the reduced urine concentrating ability in the aged rats.
Glucocorticoids may be a mechanism that contributes to the decrease in UT-A1 abundance in aged rats. Older (30 month-old) rats have elevated plasma corticosterone levels as compared to 10 month-old rats [25]. Glucocorticoids decrease UT-A1 transcription, mRNA abundance, and protein abundance [44;45]. These findings suggest the hypothesis that increased glucocorticoids in aged rats may contribute to the reduction in UT-A1 protein.
UT-B protein is expressed on erythrocytes and in the descending vasa recta. A reduction in UT-B would reduce urine concentrating ability by reducing the efficiency of counter-current exchange and/or decreasing intra-renal urea recycling. People who lack the Kidd blood group antigen, which is also UT-B, and knock-out mice lacking UT-B, are unable to concentrate their urine to normal levels [46;47]. Thus, UT-B protein expression on erythrocytes and/or in the descending vasa recta is necessary to produce maximally concentrated urine [46;48-50].
UT-B protein abundance is significantly reduced in aged rats [21;43], and administration of supra-physiological amounts of dDAVP increases it [25]. Thus, another factor that may contribute to reduced urine concentrating ability in aged rats is the reduced level of UT-B protein.
Summary
Aged people and rats have a reduced ability to maximally concentrate their urine. Many of the key transport proteins that contribute to urine concentrating ability, namely AQP2, serine-256-phosphorylated AQP2, AQP3, NKCC2/BSC1, UT-A1, UT-B, and the V2-receptor, are reduced in the medulla of aged rats. The reductions in the abundances of proteins, and their reduced response to administration of a supra-physiologic dose of dDAVP or water restriction, contributes to the reduced ability of aged rats to concentrate their urine and conserve water. If similar mechanisms occur in human kidneys, it would provide a molecular explanation for the reduced concentrating ability in aging and may provide opportunities for novel therapeutic approaches to improve urine concentrating ability.
ACKNOWLEDGMENT
This work was supported by National Institutes of Health grants R01-DK41707 and P01-DK61521.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Rowe JW, Shock NW, DeFronzo RA. The influence of age on the renal response to water deprivation in man. Nephron. 1976;17:270–278. doi: 10.1159/000180731. [DOI] [PubMed] [Google Scholar]
- 2.Sporn IN, Lancestremere RG, Papper S. Differential diagnosis of oliguria in aged patients. N Engl J Med. 1962;267:130–132. doi: 10.1056/NEJM196207192670304. [DOI] [PubMed] [Google Scholar]
- 3.O'Neill PA, McLean KA. Water homeostasis and ageing. Medical Laboratory Sciences. 1992;49:291–298. [PubMed] [Google Scholar]
- 4.Geelen G, Corman B. Relationship between vasopressin and renal concentrating ability in aging rats. Am J Physiol Regul Integr Comp Physiol. 1992;262:R826–R833. doi: 10.1152/ajpregu.1992.262.5.R826. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen S, Frokiaer J, Marples D, Kwon ED, Agre P, Knepper M. Aquaporins in the Kidney: From Molecules to Medicine. Physiol Rev. 2002;82:205–244. doi: 10.1152/physrev.00024.2001. [DOI] [PubMed] [Google Scholar]
- 6.Bagnasco SM. Gene structure of urea transporters. Am J Physiol Renal Physiol. 2003;284:F3–F10. doi: 10.1152/ajprenal.00260.2002. [DOI] [PubMed] [Google Scholar]
- 7.Knepper MA, Kim GH, Fernández-Llama P, Ecelbarger CA. Regulation of thick ascending limb transport by vasopressin. J Am Soc Nephrol. 1999;10:628–634. doi: 10.1681/ASN.V103628. [DOI] [PubMed] [Google Scholar]
- 8.Sands JM, Layton HE. The urine concentrating mechanism and urea transporters. In: Alpern RJ, Hebert SC, editors. The Kidney: Physiology and Pathophysiology. Vol. 1. Academic Press; San Diego: 2008. pp. 1143–1178. [Google Scholar]
- 9.Sands JM, Layton HE. The physiology of urinary concentration: an update. Semin Nephrol. 2009;29:178–195. doi: 10.1016/j.semnephrol.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bankir L. Antidiuretic action of vasopressin: quantitative aspects and interaction between V1a and V2 receptor-mediated effects. Cardiovasc Res. 2001;51:372–390. doi: 10.1016/s0008-6363(01)00328-5. [DOI] [PubMed] [Google Scholar]
- 11.Brown D. The ins and outs of aquaporin-2 trafficking. Am J Physiol Renal Physiol. 2003;284:F893–F901. doi: 10.1152/ajprenal.00387.2002. [DOI] [PubMed] [Google Scholar]
- 12.Tian Y, Serino R, Verbalis JG. Downregulation of renal vasopressin V2 receptor and aquaporin-2 expression parallels age-associated defects in urine concentration. Am J Physiol Renal Physiol. 2004;287:F797–F805. doi: 10.1152/ajprenal.00403.2003. [DOI] [PubMed] [Google Scholar]
- 13.Preisser L, Teillet L, Aliotti S, Gobin R, Berthonaud V, Chevalier J, Corman B, Verbavatz JM. Downregulation of aquaporin-2 and-3 in aging kidney is independent of V2 vasopressin receptor. Am J Physiol Renal Physiol. 2000;279:F144–F152. doi: 10.1152/ajprenal.2000.279.1.F144. [DOI] [PubMed] [Google Scholar]
- 14.Terashima Y, Kondo K, Inagaki A, Yokoi H, Arima H, Murase T, Iwasaki Y, Oiso Y. Age-associated decrease in response of rat aquaporin-2 gene expression to dehydration. Life Sci. 1998;62:873–882. doi: 10.1016/s0024-3205(98)00004-6. [DOI] [PubMed] [Google Scholar]
- 15.Klingler C, Preisser L, Barrault MB, Lluel P, Horgen L, Teillet L, Ancellin N, Corman B. Vasopressin V2 receptor mRNA expression and cAMP accumulation in aging rat kidney. Am J Physiol Regul Integr Comp Physiol. 1997;272:R1775–R1782. doi: 10.1152/ajpregu.1997.272.6.R1775. [DOI] [PubMed] [Google Scholar]
- 16.Hoffert JD, Fenton RA, Moeller HB, Simons B, Tchapyjnikov D, McDill BW, Yu MJ, Pisitkun T, Chen F, Knepper MA. Vasopressin-stimulated Increase in Phosphorylation at Ser269 Potentiates Plasma Membrane Retention of Aquaporin-2. J Biol Chem. 2008;283:24617–24627. doi: 10.1074/jbc.M803074200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffert JD, Pisitkun T, Wang GH, Shen RF, Knepper MA. Dynamics of aquaporin-2 serine-261 phosphorylation in response to short-term vasopressin treatment in collecting duct. Am J Physiol Renal Physiol. 2007;292:F691–F700. doi: 10.1152/ajprenal.00284.2006. [DOI] [PubMed] [Google Scholar]
- 18.Hoffert JD, Pisitkun T, Wang G, Shen R-F, Knepper MA. Quantitative phosphoproteomics of vasopressin-sensitive renal cells: regulation of aquaporin-2 phosphorylation at two sites. Proc Natl Acad Sci USA. 2006;103:7159–7164. doi: 10.1073/pnas.0600895103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fenton RA, Moeller HB, Hoffert JD, Yu MJ, Nielsen S, Knepper MA. Acute regulation of aquaporin-2 phosphorylation at Ser-264 by vasopressin. PNAS. 2008;105:3134–3139. doi: 10.1073/pnas.0712338105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wade JB, Stetson DL, Lewis SA. ADH action: evidence for a membrane shuttle mechanism. Annals NY Acad Sci. 1981;372:106–117. doi: 10.1111/j.1749-6632.1981.tb15464.x. [DOI] [PubMed] [Google Scholar]
- 21.Combet S, Teillet L, Geelen G, Pitrat B, Gobin R, Nielsen S, Trinh-Trang-Tan MM, Corman B, Verbavatz JM. Food restriction prevents age-related polyuria by vasopressin-dependent recruitment of aquaporin-2. Am J Physiol Renal Physiol. 2001;281:F1123–F1131. doi: 10.1152/ajprenal.0139.2001. [DOI] [PubMed] [Google Scholar]
- 22.Amlal H, Wilke C. Resistance of mTAL Na+-dependent transporters and collecting duct aquaporins to dehydration in 7-month-old rats. Kidney Int. 2003;64:544–554. doi: 10.1046/j.1523-1755.2003.00110.x. [DOI] [PubMed] [Google Scholar]
- 23.Swenson KL, Sands JM, Jacobs JD, Sladek CD. Effect of aging on the vasopressin and aquaporin responses to dehydration in Fischer 344/Brown-Norway F1 rats. Am J Physiol. 1997;273:R35–R40. doi: 10.1152/ajpregu.1997.273.1.R35. [DOI] [PubMed] [Google Scholar]
- 24.Catudioc-Vallero J, Sands JM, Sidorowicz HE, Klein JD, Sladek CD. Effect of age and testosterone in the vasopressin response to dehydration in F344BNF1 male rats. Adv Exp Med Biol. 1998;449:183–185. doi: 10.1007/978-1-4615-4871-3_22. [DOI] [PubMed] [Google Scholar]
- 25.Combet S, Geffroy N, Berthonaud V, Dick B, Teillet L, Verbavatz J-M, Corman B, Trinh-Trang-Tan M-M. Correction of age-related polyuria by dDAVP: molecular analysis of aquaporins and urea transporters. Am J Physiol Renal Physiol. 2003;284:F199–F208. doi: 10.1152/ajprenal.00167.2002. [DOI] [PubMed] [Google Scholar]
- 26.Tian Y, Riazi S, Khan O, Klein JD, Sugimura Y, Verbalis JG, Ecelbarger CA. Renal ENaC subunit, Na-K-2Cl and Na-Cl cotransporter abundances in aged, water-restricted F344 × Brown Norway rats. Kidney Int. 2006;69:304–312. doi: 10.1038/sj.ki.5000076. [DOI] [PubMed] [Google Scholar]
- 27.Gamble JL, McKhann CF, Butler AM, Tuthill E. An economy of water in renal function referable to urea. Am J Physiol. 1934;109:139–154. [Google Scholar]
- 28.Kokko JP, Rector FC. Countercurrent multiplication system without active transport in inner medulla. Kidney Int. 1972;2:214–223. doi: 10.1038/ki.1972.97. [DOI] [PubMed] [Google Scholar]
- 29.Stephenson JL. Concentration of urine in a central core model of the renal counterflow system. Kidney Int. 1972;2:85–94. doi: 10.1038/ki.1972.75. [DOI] [PubMed] [Google Scholar]
- 30.Levinsky NG, Berliner RW. The role of urea in the urine concentrating mechanism. J Clin Invest. 1959;38:741–748. doi: 10.1172/JCI103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peil AE, Stolte H, Schmidt-Nielsen B. Uncoupling of glomerular and tubular regulations of urea excretion in rat. Am J Physiol Renal,Fluid Electrolyte Physiol. 1990;258:F1666–F1674. doi: 10.1152/ajprenal.1990.258.6.F1666. [DOI] [PubMed] [Google Scholar]
- 32.Epstein FH, Kleeman CR, Pursel S, Hendrikx A. The effect of feeding protein and urea on the renal concentrating process. J Clin Invest. 1957;36:635–641. doi: 10.1172/JCI103463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klahr S, Alleyne GAO. Effects of chronic protein-calorie malnutrition on the kidney. Kidney Int. 1973;3:129–141. doi: 10.1038/ki.1973.21. [DOI] [PubMed] [Google Scholar]
- 34.Hendrikx A, Epstein FH. Effect of feeding protein and urea on renal concentrating ability in the rat. Am J Physiol. 1958;195:539–542. doi: 10.1152/ajplegacy.1958.195.3.539. [DOI] [PubMed] [Google Scholar]
- 35.Sands JM. Molecular mechanisms of urea transport. J Membr Biol. 2003;191:149–163. doi: 10.1007/s00232-002-1053-1. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen S, Terris J, Smith CP, Hediger MA, Ecelbarger CA, Knepper MA. Cellular and subcellular localization of the vasopressin-regulated urea transporter in rat kidney. Proc Natl Acad Sci USA. 1996;93:5495–5500. doi: 10.1073/pnas.93.11.5495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blount MA, Klein JD, Martin CF, Tchapyjnikov D, Sands JM. Forskolin stimulates phosphorylation and membrane accumulation of UT-A3. Am J Physiol Renal Physiol. 2007;293:F1308–F1313. doi: 10.1152/ajprenal.00197.2007. [DOI] [PubMed] [Google Scholar]
- 38.Bagnasco SM, Peng T, Janech MG, Karakashian A, Sands JM. Cloning and characterization of the human urea transporter UT-A1 and mapping of the human Slc14a2 gene. Am J Physiol Renal Physiol. 2001;281:F400–F406. doi: 10.1152/ajprenal.2001.281.3.F400. [DOI] [PubMed] [Google Scholar]
- 39.Sands JM, Nonoguchi H, Knepper MA. Vasopressin effects on urea and H20 transport in inner medullary collecting duct subsegments. Am J Physiol. 1987;253:F823–F832. doi: 10.1152/ajprenal.1987.253.5.F823. [DOI] [PubMed] [Google Scholar]
- 40.Zhang C, Sands JM, Klein JD. Vasopressin rapidly increases the phosphorylation of the UT-A1 urea transporter activity in rat IMCDs through PKA. Am J Physiol Renal Physiol. 2002;282:F85–F90. doi: 10.1152/ajprenal.0054.2001. [DOI] [PubMed] [Google Scholar]
- 41.Klein JD, Froehlich O, Blount MA, Martin CF, Smith TD, Sands JM. Vasopressin increases plasma membrane accumulation of urea transporter UT-A1 in rat inner medullary collecting ducts. J Am Soc Nephrol. 2006;17:2680–2686. doi: 10.1681/ASN.2006030246. [DOI] [PubMed] [Google Scholar]
- 42.Blount MA, Mistry AC, Froehlich O, Price SR, Chen G, Sands JM, Klein JD. Phosphorylation of UT-A1 urea transporter at serines 486 and 499 is important for vasopressin-regulated activity and membrane accumulation. Am J Physiol Renal Physiol. 2008;295:F295–F299. doi: 10.1152/ajprenal.00102.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trinh-Trang-Tan MM, Geelen G, Teillet L, Corman B. Urea transporter expression in aging kidney and brain during dehydration. Am J Physiol Regul Integr Comp Physiol. 2003;285:R1355–R1365. doi: 10.1152/ajpregu.00207.2003. [DOI] [PubMed] [Google Scholar]
- 44.Peng T, Sands JM, Bagnasco SM. Glucocorticoids inhibit transcription and expression of the rat UT-A urea transporter gene. Am J Physiol Renal Physiol. 2002;282:F853–F858. doi: 10.1152/ajprenal.00262.2001. [DOI] [PubMed] [Google Scholar]
- 45.Naruse M, Klein JD, Ashkar ZM, Jacobs JD, Sands JM. Glucocorticoids downregulate the rat vasopressin-regulated urea transporter in rat terminal inner medullary collecting ducts. J Am Soc Nephrol. 1997;8:517–523. doi: 10.1681/ASN.V84517. [DOI] [PubMed] [Google Scholar]
- 46.Sands JM, Gargus JJ, Fröhlich O, Gunn RB, Kokko JP. Urinary concentrating ability in patients with Jk(a-b-) blood type who lack carrier-mediated urea transport. J Am Soc Nephrol. 1992;2:1689–1696. doi: 10.1681/ASN.V2121689. [DOI] [PubMed] [Google Scholar]
- 47.Yang B, Bankir L, Gillespie A, Epstein CJ, Verkman AS. Urea-selective concentrating defect in transgenic mice lacking urea transporter UT-B. J Biol Chem. 2002;277:10633–10637. doi: 10.1074/jbc.M200207200. [DOI] [PubMed] [Google Scholar]
- 48.Macey RI, Yousef LW. Osmotic stability of red cells in renal circulation requires rapid urea transport. Am J Physiol. 1988;254:C669–C674. doi: 10.1152/ajpcell.1988.254.5.C669. [DOI] [PubMed] [Google Scholar]
- 49.Edwards A, Pallone TL. Facilitated transport in vasa recta: Theoretical effects on solute exchange in the medullary microcirculation. Am J Physiol Renal Physiol. 1997;272:F505–F514. doi: 10.1152/ajprenal.1997.272.4.F505. [DOI] [PubMed] [Google Scholar]
- 50.Edwards A, Pallone TL. A multiunit model of solute and water removal by inner medullary vasa recta. Am J Physiol Heart Circ Physiol. 1998;274:H1202–H1210. doi: 10.1152/ajpheart.1998.274.4.H1202. [DOI] [PubMed] [Google Scholar]