Abstract
After the spontaneous relief of initial symptoms by traumatic carotid-cavernous fistula (CCF), paradoxical worsening of patient's condition can be followed. We present a case of a 60-yr-old man whose audible bruit from a traumatic CCF had completely disappeared. A few days later, however, the patient had spontaneous intracerebral hematoma with cortical venous drainage. Complete obliteration of the fistula was achieved after embolization. When initial audible bruit in traumatic CCF disappears suddenly, cerebral angiography should be performed to differentiate venous hypertension by the hemodynamic changes of the cavernous sinus channels from spontaneous resolution of CCF.
Keywords: Carotid-Cavernous Sinus Fistula, Cerebral Hemorrhage, Cerebral Angiography
INTRODUCTION
Spontaneous closure of traumatic carotid-cavernous fistulas (CCFs) by thrombosis of the cavernous sinus is quite rare since these are high-flow fistulas. We recently observed a traumatic CCF that had rapid improvement of symptoms after the event, but it recurred shortly after the resolution of symptoms. The mechanism for paradoxical worsening of the patient's condition is discussed by reviewing literature.
CASE REPORT
A 60-yr-old man fell down from a ladder on 11 August 2002, suffering mental deterioration to a Glasgow Coma Scale of 10 and mild left hemiparesis. Brain computed tomography (CT) scan showed a massive right epidural hematoma. The hematoma was evacuated with right fronto-temporoparietal craniotomy. On August 17, he was improved to the extent that he complained a headache. Proptosis and conjunctival chemosis of left eye was observed with edema of the eyelid. A bruit was heard over the left orbital and periorbital regions. The left eye was fixed with a sluggish light reflex. Brain magnetic resonance imaging (MRI) showed dilated superior ophthalmic vein in the left orbit (Fig. 1), suggesting a traumatic CCF. While in the hospital waiting for a cerebral angiography, the bruit disappeared with improvement of other ocular signs. We thought the spontaneous resolution of traumatic CCF had occured with thrombus formation of cavernous sinus. Four days later, however, the patient suddenly became semicomatose with a palsy of the left third cranial nerve and an audible bruit of left eye. A brain CT scan revealed a large amount of hematoma in left frontal base (Fig. 2). A left carotid angiogram demonstrated direct CCF with drainage into sigmoid sinus via inferior petrosal sinus, superior ophthalmic vein and inferior ophthalmic vein, and showed dilated subfrontal pial veins (Fig. 3). During the operation to evacuate the spontaneous intracerebral hematoma (ICH), bleeding appeared to be originated from ruptured subfrontal pial veins. The left CCF was occluded by the transarterial embolization with platinum coil. On September 29, ocular signs and bruit were no longer present. A follow-up left carotid angiogram showed a complete occlusion of fistula (Fig. 4).
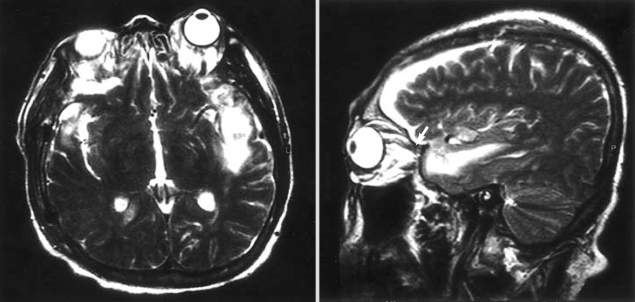
Fig. 1.
T2-weighted axial and sagittal magnetic resonance images show a dilated superior ophthalmic vein (arrows).
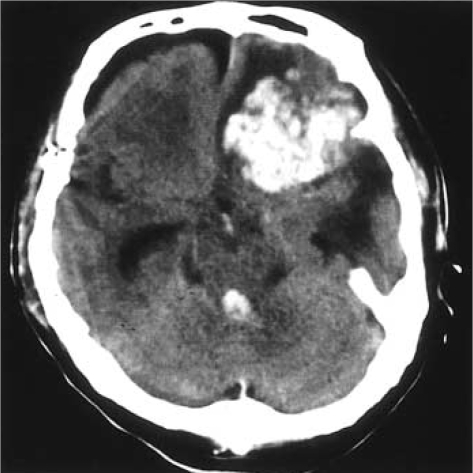
Fig. 2.
Non contrast-enhanced computed tomography scan shows a large amount of hematoma in the left frontal base.
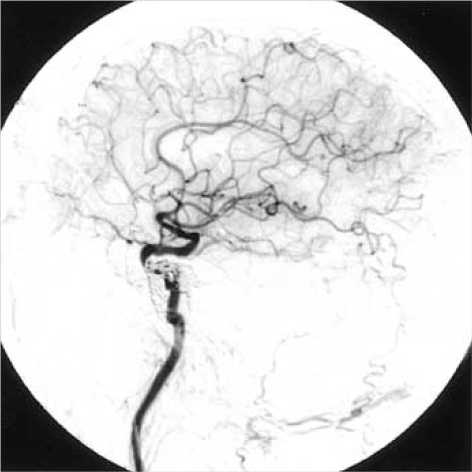
Fig. 3.
Left internal carotid artery angiogram in lateral projection, showing direct CCF with drainage into sigmoid sinus (short arrow), superior ophthalmic vein (long arrow) and inferior ophthalmic vein (arrowhead), and dilated subfrontal pial veins (open arrow).
Fig. 4.
Follow-up angiogram after the transarterial embolization shows a complete occlusion of CCF.
DISCUSSION
CCFs typically produce symptoms in two ways: cerebral arterial steal and venous hypertension. The back-flow with venous hypertension resulting from the CCFs is much more threatening. Multiple routes of drainage from the cavernous sinus provide the basis for the varied modes of presentation of CCFs. If the venous drainage is via sphenoparietal sinus, cortical venous hypertension may result, placing the patient at risk for ICH (1-3), which is extremely uncommon in traumatic CCF.
The spontaneous occlusion of a CCF has been reported to occur in about 10% of all reported cases (4-6), but the spontaneous resolution of symptomatic traumatic CCF is quite rare. As a mechanism of spontaneous occlusion of traumatic CCFs, carotid angiography played an important role in most reported cases. It is thought that formation of a thrombus is induced due to vascular contraction caused by the contrast medium, or due to the decrease in blood flow passing through the fistula (7, 8). The possibility that a dissecting aneurysm (7) or false aneurysm (9) formed in the cavernous internal carotid artery was obliterated has also been suggested.
Lin et al. (10) presented a case of traumatic CCF that had completely resolved after the initial event, but recurred 4 yr later, causing ICH during pregnancy and puerperium. They suggested that the hemodynamic change and the hormonal effects due to the patient's subsequent pregnancy further aggravated the venous engorgement and finally caused rupture. Muraine et al. (11) also reported that a case of spontaneous thrombosis of CCF was preceded by paradoxical worsening of initial ocular symptoms.
We speculated that spontaneous closure occurred probably from thrombotic occlusion of most of the cavernous sinus channels. Partial thrombosis of the cavernous sinus, especially the superior ophthalmic vein, gave rise to the resolution of the patient's eye signs and the bruit. Nevertheless, this also rendered the subfrontal cortical vessels, which were the preserved drainage routes of the occult CCF, more dilated and engorged. This process was followed by paradoxical worsening of the patient's condition.
In conclusion, even if initial audible bruit abruptly disappears or eye signs improve in direct CCF, cerebral angiography should be performed to confirm the true closure of CCF, in consideration of the fact that not only spontaneous resolution of CCF but also diversion of drainage channels may result in symptom improvement.
ACKNOWLEDGMENT
This paper was supported by Wonkwang University in 2004.
References
- 1.d'Angelo VA, Monte V, Scialfa G, Fiumara E, Scotti G. Intracerebral venous hemorrhage in "high-risk" carotid cavernous fistula. Surg Neurol. 1988;30:387–390. doi: 10.1016/0090-3019(88)90202-9. [DOI] [PubMed] [Google Scholar]
- 2.Halbach VV, Higashida RT, Hieshima GB, Reiche M, Norman D, Newton TH. Dural fistulas involving the cavernous sinus : results of treatment in 30 patients. Radiology. 1987;163:437–442. doi: 10.1148/radiology.163.2.3562823. [DOI] [PubMed] [Google Scholar]
- 3.Turner DM, Vangilder JC, Mojtahedi S, Pierson EW. Spontaneous intracerebral hematoma in carotid-cavernous fistula. Report of three cases. J Neurosurg. 1983;59:680–686. doi: 10.3171/jns.1983.59.4.0680. [DOI] [PubMed] [Google Scholar]
- 4.Dandy WE. Carotid-cavernous aneurysms (pulsating exophthalmos) Zentralbl Neurochir. 1937;2:77–113. 165–206. [Google Scholar]
- 5.Locke CE. Intracranial arterio-venous aneurysm or pulsating exophthalmos. Ann Surg. 1924;80:1–24. doi: 10.1097/00000658-192480010-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin JD, Mabson RF. Pulsating exophthalmos, review of all reported cases. JAMA. 1943;121:330–335. [Google Scholar]
- 7.van der Drift JH, Sparling CM, Berg D, Magnus O. Spontaneous occlusion of a carotid-cavernous shunt. Neurology. 1967;17:187–193. doi: 10.1212/wnl.17.2.187. [DOI] [PubMed] [Google Scholar]
- 8.Isofort A. Spontangeilung einer trumatischen Carotissinus cavernousus-Fistel bei einem kind unter der Angiographue. Klin Mbl Augenhk. 1967;150:821–823. [PubMed] [Google Scholar]
- 9.Stenbens WE. The pathogenesis of intracranial aneurysms. In: Tindall G, Cooper PR, Barrow DL, editors. The practice of neurosurgery. Vol 2. Baltimore: Williams & Wilkins; 1996. pp. 1941–1952. [Google Scholar]
- 10.Lin TK, Chang CN, Wai YY. Spontaneous intracerebral hematoma from occult carotid-cavernous fistula during pregnancy and puerperium. J Neurosurg. 1992;76:714–717. doi: 10.3171/jns.1992.76.4.0714. [DOI] [PubMed] [Google Scholar]
- 11.Muraine M, de Bokay E, Clavier E, Brasseur G. Paradoxical aggravation of carotid cavernous fistula. J Fr Ophthalmol. 1996;19:51–54. [PubMed] [Google Scholar]