Abstract
The care of the patient with scoliosis has a history extending back over two millennia with cast and brace treatment being a relatively recent endeavor, the modern era comprising just over half a century. Much of the previous literature provides a modest overview with emphasis on the history of the operative management. To better understand the current concepts of brace treatment of scoliosis, an appreciation of the history of bracing would be helpful. As such, we review the history of the treatment of scoliosis with an emphasis on modern brace treatment, primarily from a North American perspective. Our review utilizes consideration of historical texts as well as current treatises on the history of scoliosis and includes discussion of brace development with their proponents’ rationale for why they work along with an appraisal of their clinical outcomes. We provide an overview of the current standards of care and the braces typically employed toward that standard including: the Milwaukee brace, the Wilmington brace, the Boston brace, the Charleston brace, the Providence brace and the SpineCor brace. Finally, we discuss future trends including improvements in methods of determining the critical period of peak growth velocity in children with scoliosis, the exciting promise of gene markers for progressive scoliosis and “internal bracing” options.
Introduction
“If you would understand anything, observe its beginning and its development.”—Aristotle
The care of the patient with scoliosis has a long and varied history extending over two millennia. Immobilization with a spinal cast or brace has been and remains an important treatment modality in the care of the child with scoliosis. Current bracing techniques and recommendations are well described in the literature. The history of bracing for scoliosis has received less attention but knowledge of the evolution of modern bracing improves understanding of the treatment concepts.
We therefore describe the history of bracing for scoliosis, from bracing’s earliest inception to its current manifestation, predominantly from a North American perspective and with an emphasis on the modern era of bracing. Our timeline begins with Hippocrates in the 5th century BC and culminates in the 21st century. Current standards of care along with the future of the treatment of scoliosis are discussed.
Early History
The treatment of scoliosis with longitudinal traction was first described by Hippocrates in the 5th century BC [22]. His early work was devoted to the use of traction with the Hippocratic bench or scamnum for the treatment of long bone and spinal fractures. It was not long before he applied these same techniques to the treatment of spinal deformity. Traction treatment was crude, requiring painful, prolonged sessions on the scamnum [22]. For nearly half a century there was little modification of the Hippocratic technique until the 2nd century AD, when Galen of Pergamum, a student of the Hippocratic school of thought, added direct pressure in combination with traction [31]. Galen’s contribution mirrored the modern tactic but did little to improve outcomes as treatment was, of necessity, intermittent and no bracing was utilized [40]. Despite these shortcomings, variations of these devices were used up until the 16th century as alternative modalities were limited or nonexistent [4].
The first supportive braces used to treat spinal deformity were developed by Ambrose Paré (1510–1590), a French army surgeon considered one of the “fathers” of modern surgery. Paré hypothesized spinal deformity resulted from dislocation of the spine. He described a method of reducing the “dislocation” using extension and directed pressure [30]. Afterward, patients were placed into a padded iron corset with multiple holes to reduce the weight, changed at intervals to accommodate growth. Paré’s brace was notable for being the precursor to the modern spinal orthotic brace. He apparently met with some success as he was the first to note that bracing after skeletal maturity was unsuccessful [42]. After Paré, progress in the treatment of scoliosis would not come about for another two centuries, in the late 1800’s, when the first glimpses of the modern treatment for scoliosis could be seen in the work of Lewis Albert Sayre.
Sayre, a staff physician at Bellevue Hospital in New York City, NY, was the first person to hold the title of Professor of Orthopaedic Surgery in America (he was appointed in 1861) and is considered one of the founding fathers of orthopaedic surgery in the United States [64]. Sayre was renowned for his writings on the treatment of spinal disorders, especially with regard to the study of scoliosis. During this time, the study of idiopathic scoliosis was still in its infancy and its etiology widely debated, with corset use being popularly criticized [61]. Sayre believed musculoskeletal imbalance was the primary cause and that treatment should center on “gymnastic exercises” to strengthen the muscles on the convex side of the deformity [57]. As evidence, he observed that girls of lower socioeconomic levels infrequently had abnormal spine development and he postulated their “healthy” spines related to their lack of corset use and their being forced to stand erect because of the bundles of wood they constantly carried on their head.
Sayre is best known, however, for his 1874 description of the use of traction in conjunction with a plaster cast to correct and hold spinal deformity, predating the use of this technique in the modern history of the treatment of spinal deformity [57]. Traction was applied by suspending his patient off the ground by supports at the chin and axillae and, following this, a plaster jacket was applied. The plaster jacket, though, was simply an adjunct to treatment centered on “gymnastic exercises necessary for cure of the deformity” and consequently was removed at night and during exercise. While Sayre did have some success with his approach, adequate maintenance of correction after discontinuation of the jacket was not seen [57, 58]. His method, however, formed the basis for the next generation of techniques used to treat scoliosis.
The most important development of this time related to the study and treatment of scoliosis was Wilhelm Conrad Roentgen’s 1895 discovery of an unknown type of radiation he called “x-rays” [49, 54]. With x-rays, physicians were able to study skeletal anatomy without dissection of the body, revolutionizing the study of scoliosis. In the period after Roentgen’s discovery in the early 1900’s, spinal radiographs initially required long exposure times which resulted in poor quality spinal radiographs because of excessive patient movement [43]. There was little concern regarding radiation doses at the time as the deleterious effects of x-ray radiography had not yet been discovered. Not until the development of faster radiographic films circa 1930 were good quality spinal radiographs obtainable [43]. The value of these “roentgenograms” to facilitate research and inquiry concerning scoliosis and other maladies of the spine was immeasurable.
Premodern Era
With the increasing research emphasis on scoliosis and childhood diseases, the differing etiologies of scoliosis began to be elucidated. The most common etiologies of spinal deformity in the early 20th century were tuberculous and paralytic (typically secondary to polio) [33]. In 1911, Russell Hibbs performed one of the first posterior spinal fusions for a gibbous deformity resulting from tuberculous infection of the spine at the New York Orthopaedic Dispensary and Hospital (now, a part of the New York-Presbyterian Hospital of the Columbia University College of Physicians and Surgeons) [20]. By 1914, Hibbs was using this technique to treat patients with scoliosis. Attempts were made to reduce the curvature before surgery because intraoperative methods of correction did not yet exist. These preoperative corrective measures included bed traction and later full-time plaster body jackets applied under gravity traction. For eight weeks after surgery, patients were either placed back in bed traction or were made to wear a corset, both attempts to immobilize the spine to promote fusion [21].
In 1924, Lovett and Brewster described the full-time use of a “turnbuckle” cast for the correction of scoliotic deformities [29]. The turnbuckle cast was essentially a plaster body jacket split into superior and inferior sections, which were then joined with a lateral hinge on the convex side of the deformity and a turnbuckle (a threaded screw with a wing nut) on the concave side of the deformity. Opening the hinge (ie, distracting the concave side through the turnbuckle) would result in the application of lateral bending forces to the spine [52], straightening the primary curve. No attempt at direct curve correction or derotation was made. These jackets were based on the principle that to straighten a curved rod, bending forces are more effective than traction, especially for smaller curves [59].
Joseph Risser, an orthopaedic surgeon at the New York Orthopaedic Dispensary and Hospital, along with Hibbs, pioneered the use of the turnbuckle cast in the treatment of scoliosis. In 1931, Hibbs, Risser, and Ferguson published their work on the treatment of scoliosis in 360 patients using cast immobilization with posterior spinal arthrodesis [21]. Their results were excellent in comparison to alternative treatments at that time with nearly 70% of cases resulting in improvement or maintenance of their preoperative curvature.
Although effective in the preoperative correction and postoperative immobilization of spinal deformity, there were downsides to the use of the turnbuckle cast. Early turnbuckle casts were cumbersome and quite heavy (the plaster required nearly 1 week to fully dry), making mobilization of the patient difficult. Additionally, because the turnbuckle cast relied solely on bending forces to straighten the primary curve, it was possible to inadvertently increase the secondary curves and throw the trunk out of alignment [59]. Consequently, in the early 1950’s Risser modified the concept of the turnbuckle cast, opting for a more contoured, lighter cast in which the patient would be able to walk [50]. For curve correction prior to application of the plaster cast, Risser chose to use traction on a stabilizer frame he developed. This allowed for curve reduction like the turnbuckle cast but with improved maintenance of trunk alignment and coronal balance. The patient was placed supine on a metal frame (now known as a Risser frame) that supported him or her while allowing the surgeon and assistants to apply longitudinal traction through chin and pelvic straps and localized lateral pressure at the apices of the coronal deformity. In one of the first described attempts at correction of rotational deformity, posterolateral pressure was localized to the rib hump. After achieving correction, a molded cast was applied from the chin or under the axillae to the iliac crests. The Risser localizer cast, as it came to be known, was worn full-time and was used to obtain preoperative deformity correction and for 8 to 10 months after posterior spinal arthrodesis to immobilize the spine.
The turnbuckle cast and later the localizer cast were the first widely used nonoperative methods of treatment for scoliosis [21, 50]. In patients with milder deformity nearing skeletal maturity, casts were used to prevent excessive progression of spinal curvatures. Patients would wear the cast continuously until vertebral growth was complete, only changing the cast for loss of correction, when patients outgrew their cast, or when casts were broken or soiled beyond repair. The localizer cast continued to be widely used in the operative and nonoperative treatment of scoliosis until the development of removable spinal orthoses.
While refinements in braces and brace application were certainly important in the development of bracing for scoliosis, just as important was the recognition of the importance of the timing of brace application. In 1958, Risser described the progressive lateral to medial ossification of the iliac apophysis followed by its fusion with the ilium and the correlation of this with spinal skeletal growth [51]. Because adolescent idiopathic scoliosis (AIS) progresses in children who are still rapidly growing, surgeons were then more accurately able to identify children who would benefit most from treatment. Risser staging continues to be important in the evaluation of the child with scoliosis, though its poor ability to predict the period of peak spinal growth has led to the development and use of alternative radiographic staging systems of skeletal maturity [47, 48].
Further understanding of the natural history of scoliosis from review of case series led to better understanding of the disease process and the influence of methods of intervention. In 1950, Ponseti and Friedman of the University of Iowa reported on the natural history of idiopathic scoliosis in 394 patients [45]. They found curve pattern, age at onset, and rapidity of curve progression were important factors to consider in determining prognoses of patients with scoliosis. Patients with thoracic curves in their series developed the most noteworthy deformity. Earlier onset of disease and rapid progression of curvatures were associated with the development of more severe curves that were difficult to treat. Ponseti and Friedman’s findings helped to establish treatment guidelines for the nonoperative and surgical treatment of patients with AIS. Armed with better bracing techniques and a better understanding of the natural history of idiopathic scoliosis and the risk factors for progression, surgeons began to view brace treatment as a viable treatment option for patients with specific types of scoliosis.
Modern Era
Prior to the development of the removable orthoses, nonoperative treatment of scoliosis was achieved mostly by prolonged wear of correcting casts. As it became understood that long-term bracing through to skeletal maturity was required to prevent curve progression, alternatives to correcting casts were sought. Advances in the fabrication of removable braces coupled with the development of rational treatment algorithms resulting from improved understanding of idiopathic scoliosis and its natural history marked the beginning of the modern era of brace treatment for scoliosis.
Milwaukee Brace
In 1946, Walter Blount described the use of a removable cervicothoracolumbosacral orthosis (CTLSO) as a method of postoperative immobilization after operative treatment of neuromuscular scoliosis (primarily as a result of polio) [5]. With the introduction of this orthosis, the Milwaukee brace, Blount ushered in the modern era of brace treatment for scoliosis.
In 1958, Blount and his colleagues published their experience using the Milwaukee brace in the nonoperative treatment of AIS (Fig. 1) [5]. The original Milwaukee brace consisted of a molded pelvic girdle made of leather with a metal superstructure comprised of three metal uprights designed to minimize thoracic pressure. The anterior bar was made of aluminum to enhance radiolucency and the posterior bars were made of stainless steel to enhance rigidity. A chin rest (a fixed mandibular and occipital assembly) was initially used to stabilize the head but because of later reports of orthognathic deformities from the applied pressure, the chin rest was ultimately changed to a throat pad [32]. Lateral pressure pads, trapezius pads, and axillary slings were attached to the superstructure and placed based on curve location. The axillary slings were used for counterpressure for higher thoracic curves (T5–T8). Traditionally, the pelvic portion of the Milwaukee brace was custom-molded leather made from a cast of the patient. Later, the leather was replaced by prefabricated thermoplastics that were easier and less expensive to create, first Orthoplast, then vitrothene, and finally polypropylene [28, 32]. Custom molding with thermoplastics was reserved for patients with considerable pelvic obliquity or atypical spinal deformity.
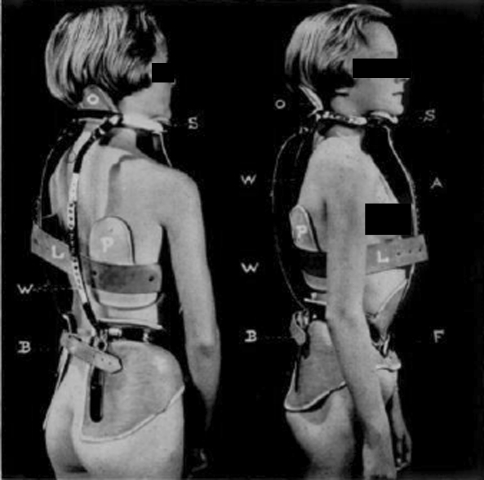
Fig. 1.
The Milwaukee brace, a cervicothoracolumosacral orthosis introduced in 1958, was the first of the modern spinal braces. (Reprinted from Blount WP, Schmidt AC, Bidwell RG. Making the Milwaukee brace. J Bone Joint Surg Am. 1958;40:526–528 with permission from Journal of Bone and Joint Surgery, Inc., Needham, MA.)
The original design of the Milwaukee brace worked by applying corrective forces to the spine in two planes: longitudinal traction through the pelvic module in conjunction with the neck ring and laterally applied corrective forces to the apex of the deformity through lateral pads [38]. The efficacy of the Milwaukee brace relied on the pelvic module being intimate with the iliac crest and lumbar spine. At the time in the United States, flattening of the lumbar lordosis was considered critical to maximize correction of scoliosis. Decreased lumbar lordosis theoretically created a more stable foundation for the brace and moved the lumbar spine posteriorly where lateral and derotational forces could be more effectively applied to the spine [26]. Correction of spinal deformity with the Milwaukee brace was theorized to occur by both passive and active forces. Passive correction was achieved by direct pressure from the pads or by traction from the brace design. Active correction was believed to occur through active movement of the body away from pressure points as the patient’s muscles fired to pull the trunk away from contact with the lateral pads or chin support. Later study of the Milwaukee brace suggested correction was largely the result of passive effects with little correction provided from active muscle action [2, 18].
Noncompliance with brace wear is an issue with the Milwaukee brace, as it is with all removable orthoses and varies from outright refusal to wear the brace, to premature discontinuation of the use of the brace, to less than full-time use of the brace [39]. Lack of compliance has been found to relate to several factors including the unacceptable appearance of the brace to the body image-conscious teenager, and the discomfort from chin and throat contact or from the pelvic portion of the brace [3]. While some studies report little variation in compliance when compared with the thoracolumbosacral orthosis (TLSO), others show substantially less compliance with the Milwaukee brace when compared to TLSO’s [28, 62].
Despite these limitations, the Milwaukee brace was the first widely used removable orthosis for the nonoperative treatment of scoliosis. Its widespread use was likely a result of several factors. First, its method of controlling spinal deformity through both longitudinal traction and lateral pressure was widely accepted. Second, the orthosis was adjustable as well as removable, important advantages over cast treatment. Last, the Milwaukee brace was promoted by Blount in the 1940’s and Moe in the 1950’s, preeminent clinicians in the field and popular lecturers who traveled extensively discussing their positive experiences with CTLSO brace treatment [34].
The Milwaukee brace remains the orthosis with the longest clinical experience and the highest reported success rate in halting progression of AIS with the caveat that because of the prior lack of standardization in bracing studies, direct comparison with studies of alternative brace designs is problematic [8, 28]. Use of the Milwaukee brace has diminished primarily because of the development of lower-profile designs with lighter-weight materials that have similar ability to prevent curve progression for certain curve types keeping the previous caveat in mind. Currently, the Milwaukee brace is primarily prescribed for patients with thoracic apices above T7, for control of upper thoracic sagittal deformities, and for other spinal deformities not amenable to treatment with lower-profile designs [37].
In an effort to make brace treatment better tolerated by patients, a variety of low-profile (underarm) designs composed of lighter-weight plastics that were more comfortable and less obtrusive to the patient were introduced at several large centers within 10 years of Blount’s work. Surgeons at the Alfred I. duPont Institute of Wilmington and Boston Children’s Hospital, among other centers, each created versions of the low-profile spinal orthosis (TLSO), commonly used in the brace management of AIS [7, 62].
Wilmington Brace
In 1969, G. Dean MacEwen, chief of service at the Alfred I. DuPont Institute, recommended treatment with the Milwaukee brace for a young girl with scoliosis. Because of her fear of ridicule, she adamantly refused treatment despite extensive counseling. An alternative option was offered, ie, bracing with a molded Risser cast, but this too was refused. The patient would only agree to a brace that was both inconspicuous and removable. In response to a seemingly unreasonable request, MacEwen and colleagues created one of the first low-profile TLSO’s, which became known as the Wilmington brace [G. Dean MacEwen, personal communication].
The Wilmington brace is a removable device constructed of durable, semirigid but moldable plastic that provides passive correction of deformities with apices at or below T7 [7]. Fabrication of the brace requires the appropriate equipment and experience to be effective. The patient is placed supine on a Risser frame and the scoliotic deformity is corrected by a combination of longitudinal traction applied by head and pelvic straps and lateral and posterolateral forces applied by hand pressure. A Risser-style plaster cast is applied while maintaining correction (Fig. 2). After the cast is dry, a supine anteroposterior radiograph of the spine is taken to determine the degree of improvement. If acceptable correction is achieved, ideally a 50% decrease in the Cobb measurement of the primary curve, the cast is removed and subsequently filled with plaster to create a replica of the patient’s torso. Thermoplastic brace material is then molded to the plaster replica. The brace is then applied to the patient and trimmed as needed to preserve comfort without compromising correction, maintaining corrective forces through molding at the curve apices, the iliac crests, greater trochanters, and symphysis pubis (Fig. 3). Finally, a standing anteroposterior radiograph of the patient in the brace is taken to confirm the degree of correction, fit, and overall spinal balance. The Wilmington brace continues to be one of the more popular TLSO’s in use today.
Fig. 2.
A Wilmington brace plaster jacket is molded to a patient placed on a Risser frame.
Fig. 3.
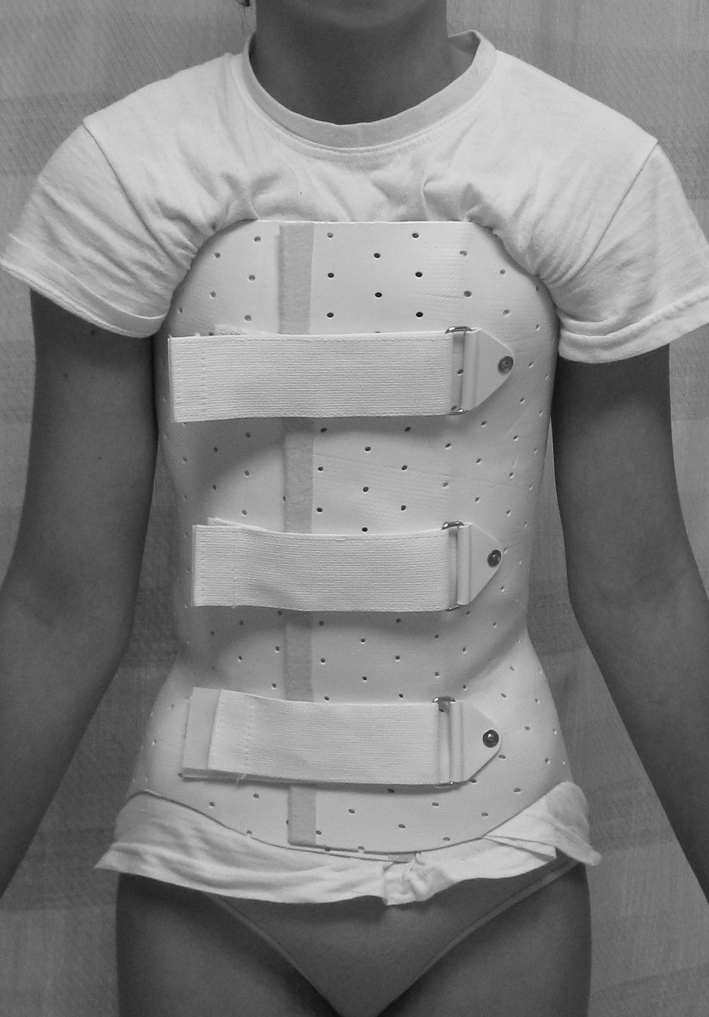
The Wilmington brace is a popular thoracolumbosacral orthosis that is custom-molded to the patient.
Boston Brace
In 1972, at Boston Children’s Hospital, John Hall and his orthotist, William Miller, jointly created a low-profile TLSO that differed from the Wilmington brace in one important aspect: it was not custom-molded and fabricated to the patient from a cast but created from prefabricated modules of different sizes that were custom-modified to achieve correction of the individual patient’s deformity [16].
Boston braces were first made from the molded plastic girdles used for Milwaukee brace superstructures [16]. Instead of custom-fitting each individual patient, a time-consuming process, Miller opted to prefabricate six standardized modules selecting a range of sizes that would fit the majority of patients seen in their clinic. These modules served as a base for the Boston modification of the Milwaukee CTLSO originally prescribed by Hall [16]. Similar to that which occurred in Wilmington, one patient requiring bracing for scoliosis refused to wear the pelvic module with the superstructure attached. The patient agreed to a lower-profile version, however, created by extending the molded plastic base to the axilla on the side of the apex. A lateral pad was then attached to this extension just below the apex of the curve to provide passive correction. Initially, a purposeful reduction in the lumbar lordosis was incorporated into the brace similar to the design of the Milwaukee brace. Design features that allowed for this included anterior abdominal molding and flattening of the posterior lumbar contours. Radiographs taken in this new brace demonstrated better deformity correction than that achieved with the superstructure in place. This method of creating a low-profile TLSO by custom modification of prefabricated plastic modules or molds is the core of the Boston brace system, one of the more popular methods of TLSO fabrication (Fig. 4).
Fig. 4.

The prefabricated Boston brace orthosis is one of the more widely used thoracolumbosacral orthoses in use today. (Photo courtesy of Boston Brace, Inc., Avon, MA. Reprinted with permission.)
Over the years, additional brace sizes were introduced and multiple variations of the original Boston brace were developed to address particular spinal curvatures, including specific versions for cervicothoracic, thoracic, thoracolumbar, and lumbar curves [16]. In the early 1990’s, the original brace design was modified to incorporate 15° of lumbar lordosis into the pelvic module in an effort to better derotate the spine. The efficacy of this modification in improving correction was confirmed by the Boston group’s observations.
The Boston bracing system, as opposed to the Wilmington brace, uses passive and active corrective forces, more similar to the Milwaukee brace in that regard [32]. The apical pads provide passive corrective forces on the convexity, whereas the open areas of the superstructure on the concavity adjacent to the pads allow active curve reduction into these openings.
The Boston bracing system is popular because its low-profile, partially open design is comfortable and well tolerated by patients. The modularity of the design requires less time and experience for fitting and is easier to modify if minor adjustments are needed compared with the Wilmington brace. These braces are some of the most widely used orthoses for full-time nonoperative brace treatment of AIS. Selection of one over another is based primarily on surgeon preference and the skills of the consulting orthotist. The Wilmington and Boston braces have yielded similar clinical outcomes when used in full-time bracing programs (23 hours per day) through skeletal maturity [1, 17, 44, 62].
Nighttime Bracing
Despite the development of the low-profile TLSO, full compliance with a brace program that demands 18 to 23 hours of daily wear through skeletal maturity is difficult for adolescents. In response to this, some surgeons have questioned the need for full-time wear, modifying designs to increase the corrective forces applied and thereby theoretically diminishing the time needed in the brace per day. Based on this principle, nighttime bracing systems were developed to improve patient compliance by reducing the total time in the brace and eliminating the social anxiety created by daytime wear.
Charleston Brace
In 1979, Frederick Reed of Charleston, SC, and his colleague, Ralph Hooper, an orthotist, collaborated to create the first “side-bending” orthosis designed for nighttime wear only, known as the Charleston brace, similar in concept to the turnbuckle cast (Fig. 5) [23]. Using a frame that maximizes correction of the curve, a plaster mold is made that holds the patient in an “overcorrected” position, theoretically stretching soft tissues and unloading the vertebral end plates on the concavity of the curve to a greater degree than a traditional TLSO [46]. The brace is then fabricated from rigid plastic from this mold. Reduction forces generated by this side-bending design result in greater in-brace correction than a traditional TLSO; consequently, brace wear of 8 to 10 hours is all that is considered necessary [47]. Despite this reduced wear schedule, patient compliance is sometimes compromised because of discomfort caused by the aggressive stretching required to achieve correction. Proponents of this brace typically use it in place of traditional TLSO bracing, although some authors are more selective in their indications [10, 19, 25, 47, 60].
Fig. 5.
The Charleston nighttime brace relies on side-bending for curve correction. (Photo courtesy of C. Ralph Hooper, Jr., CPO, Charleston Bending Brace Foundation, Charleston, SC. Reprinted with permission.)
Providence Brace
Another brace designed for nighttime use was developed in 1992 by Charles d’Amato and Barry McCoy, colleagues at the Children’s Hospital of Rhode Island in Providence (Fig. 6) [14]. While developing a standardized method to perform supine bending radiographs of the spine used in the preoperative planning of scoliosis surgery, they created an acrylic positioning board that was able to achieve considerable curve correction with minimal discomfort to the patient [14]. Their method of reduction did not rely on side-bending as did the Charleston brace. Instead, curve correction was achieved through the direct application of lateral and derotational forces, bringing the apices of the curve toward the midline. A brace incorporating this method of curve correction was then developed [13]. Initially fabricated from a mold, the modern Providence brace, as it is known, now relies on computer-assisted design and manufacturing. Because of the combination of translational and rotational forces, a well-fitted brace often leaves the patient with considerable tilt of the shoulders and truncal rotation, making standing and walking difficult. Like the Charleston brace, proponents of the Providence brace typically use it as a primary bracing option in lieu of traditional TLSO bracing [13, 24, 63].
Fig. 6.

The Providence nighttime brace works through a combination of forces: laterally applied three-point bending and rotational. (Photo courtesy of Spinal Technology, Inc., West Yarmouth, MA. Reprinted with permission.)
In appropriately selected patients, both the Charleston and Providence braces used at night only are effective and comparable to full-time TLSO use [13, 19, 47, 60, 63]. The best results have been seen in children with very flexible, single structural thoracolumbar and lumbar curves. The use of the Charleston brace in patients with considerable secondary curves has been cautioned because unbending of the primary curve can result in worsening of these compensatory curves [46]. Nighttime bracing is used by many surgeons only for specific and limited indications presently but may gain in popularity as experience with these orthoses increases and more data are accumulated to support its efficacy.
SpineCor
The most recent innovation in brace design is the use of nonrigid bracing alternatives. In 1998, Charles Rivard and Christine Coillard at Saint-Justine Hospital in Montreal, Quebec, described the use of a dynamic nonrigid bracing system for the treatment of scoliosis [36]. Development of the brace is based on the theory that scoliosis is related to three factors: postural disorganization, muscular dysfunction, and unsynchronized spinal growth that can lead to spinal deformation [11]. The authors hypothesize controlled spinal movement in their brace prevents or even improves spinal deformity by influencing these factors. The orthosis, known as the SpineCor brace, consists of a thermoplastic pelvic base, thigh and crotch bands, a cotton bolero, and four corrective elastic bands of variable sizes (Fig. 7). Placement and tensioning of the bands is curve- specific guided by a software system available to aid the clinician through the fitting process. Because movement is only partially restricted in the brace and the device is less visible under clothes, the brace is well tolerated by patients. Like traditional TLSO’s, the SpineCor brace is worn full-time through skeletal maturity. Patients are instructed to wear the brace at least 20 hours per day, allowing for two 2-hour breaks, one in the morning and one at night. Unlike traditional bracing protocols, the SpineCor brace is recommended for treatment of curves as small as 15° [53].
Fig. 7.

The SpineCor brace is a proposed flexible bracing alternative to standard rigid thoracolumbosacral orthosis braces. (Photo courtesy of Drs. Charles H. Rivard and Christine Coillard. Reprinted with permission.)
Based on preliminary work, Coillard and colleagues suggested the SpineCor brace is a reasonable option for scoliosis treatment, demonstrating less than 5 degrees of curve progression at skeletal maturity in 93% of patients in their initial series [11]. Because the SpineCor brace is used for deformities as small as 15°, these preliminary results may not be comparable to other bracing studies. More recently, Coillard et al. reported curve stabilization or improvement in 59% of patients using the new SRS Inclusion and Assessment Criteria for Bracing Studies [12]. The best results were seen in patients with single structural thoracolumbar and lumbar curves.
Although the efficacy of brace treatment has recently been called into question, most authors accept the results of the 1995 prospective, controlled (but not randomized) brace study by the Scoliosis Research Society (SRS) that showed a benefit of bracing in comparison to observation only [35, 37]. However, comparison between studies of individual brace designs remains difficult because of inconsistency of research protocols and disparity regarding the choice of outcome measures [37, 48]. For example, some studies define treatment success as curve progression < 5 degrees at skeletal maturity while others use < 10 degrees as a cutoff. In response to this, the SRS has called for standardization of the parameters used in bracing studies [48]. This work will establish new standardized protocols to guide brace treatment of AIS based on rigorous and scientifically sound clinical study. At least one bracing study [24] using these new criteria suggests lower overall success rates of orthotic management for AIS when compared to previous studies.
Standard of Care for Brace Treatment of Idiopathic Scoliosis
The goals of brace treatment for AIS are to prevent progression of deformity and to obviate the need for spinal fusion, not to improve the deformity. Brace treatment for idiopathic scoliosis is indicated for most children and adolescents with curves measuring between 25° and 40° who have at least 2 years of growth remaining based on Risser sign (Risser 0, 1, 2) and onset of menses for girls (less than 1 year postmenarche) [37]. Some important contraindications include severe hypokyphosis and severe rib deformities. A low-profile, rigid TLSO worn full-time (18–23 hours per day) through skeletal maturity is currently the standard of care for most idiopathic curve patterns with a thoracic curve apex at or below T7, ie, the majority of idiopathic curves. The Wilmington and Boston braces are used similarly. Nighttime bracing systems are more effective in patients with isolated flexible thoracolumbar and lumbar curves [25, 47, 60, 63]. Other currently used indications include patient noncompliance with a full-time wear program, patients in whom other types of orthotic management had failed, and patients nearing skeletal maturity who may not require full-time wear.
Discussion
Understanding bracing of AIS is enhanced through study of its early years and development. We described the history of bracing from its earliest underpinnings in the traction devices of ancient Greece through its earliest incarnation in the metal braces of Paré, to the methods of casting followed finally by the removable orthoses.
Because of inconsistencies in selection criteria and research protocols for most older bracing studies, we were unable to perform any direct comparisons of these braces and therefore have generalized the overall efficacy of these various brace designs based upon our interpretations of the literature. Rather than providing comparisons, our goal was to provide a comprehensive history of scoliotic bracing especially given the inclusion of a meta-analysis of bracing in this same issue. The recent standardization of inclusion criteria for bracing studies by the SRS should allow for improved appraisal of the efficacy of brace treatment for AIS.
Future considerations in the nonoperative management of idiopathic scoliosis include improvement in bracing techniques, the development and evaluation of internal bracing options (eg, vertebral stapling/tethering), and the refinement of the ability to select patients who will benefit from spinal bracing.
One of the most promising areas of research in AIS seeks to better define those patients at greatest risk for progression of scoliosis. It is known that scoliosis is most likely to progress in children in the period of peak growth velocity. Predicting curve progression has traditionally relied on assessment of certain clinical signs (eg, onset of menarche and Tanner staging) and radiographic findings (eg, the Risser sign) [27]. However, the ability to discriminate the period of peak spinal growth velocity, especially with Risser staging, has been lacking.
Newer methods are being refined to more precisely predict the peak period of spinal growth velocity. Diméglio’s modification of the Sauvegrain method and Sanders’ modification of the Tanner-Whitehouse-III RUS system both identify characteristic radiographic changes in ossification centers occurring during the critically important period of peak growth velocity (skeletal ages 11–13 in girls and 13–15 in boys) and are only recently being utilized [15, 55, 56].
Sauvegrain and colleagues, in 1962, proposed a method of determining skeletal maturity using a scoring system based on evaluation of the elbow ossification centers on anteroposterior and lateral radiographic images [56]. More recently, Diméglio and colleagues described a simplification of the Sauvegrain method to improve reliability and allow skeletal age to be assessed at 6-month intervals during the period of most rapid spinal growth [15].
The Tanner-Whitehouse-III RUS system is another method of skeletal age determination based on the characteristic progression of development of the ossification centers of the hand. In 2007, Sanders and colleagues described a simplified method of determining skeletal age based on descriptors from the Tanner-Whitehouse-III RUS system [55]. Key features of the ossification centers of the hand on anteroposterior radiographs at different levels of skeletal maturity during the period of peak growth velocity were determined.
In a preliminary study, these methods appear better able to identify patients approaching or in the earliest phases of peak spinal growth compared with traditional methods [9]. With this information, surgeons will be able to more reliably predict which patients are at greatest risk for curve progression, allowing more selective use of bracing and other methods for controlling curve progression.
Advances in genetic research have been the most exciting developments to date. James W. Ogilvie and colleagues have identified genetic markers, two major genetic loci and 12 minor loci, related to the development of scoliosis [41]. They found 95% of patients with idiopathic curves greater than 40° had these genetic markers. Using a simple genetic test, it may be possible to identify individuals at highest risk of developing severe scoliosis at the time of initial diagnosis. Armed with this information, followup care and treatment considerations can be individualized. Early bracing or minimally invasive surgical procedures may be recommended for those with a positive screen for severe scoliosis, whereas those at low risk based on DNA analysis may be spared unnecessary treatment.
There has been increasing interest in “internal bracing” or “fusionless” procedures through minimally invasive operative approaches aimed at harnessing the growth potential of the developing spine to correct spinal deformity by restricting vertebral growth on the convexity of the spinal curve. Devices currently under investigation include rigid, shape-memory alloy staples and bone screw anchors joined by a flexible, braided synthetic ligament. Both are placed across the thoracic and lumbar disc spaces on the convexity of the deformity using video-assisted thoracoscopic surgical techniques. Despite promising initial results, indications are limited because of the increased risks of operative treatment compared with bracing. Currently, fusionless surgical alternatives are recommended primarily for patients unable or unwilling to comply with standard bracing protocols. Further study will be necessary to validate the efficacy of this approach for controlling scoliosis [6] and the long-term effects of these devices on the aging spine. As previously mentioned, if accurate identification of patients at high risk for curve progression is realized, early intervention with minimally invasive fusionless procedures may find a place in the armamentarium of the scoliosis surgeon.
Although brace treatment for scoliosis has been used for centuries, the modern era of brace treatment began less than 70 years ago with the introduction of the Milwaukee brace. Improvements in materials and design and an increased understanding of the natural history of AIS over subsequent years led to the development of the removable TLSO braces, two prime examples being the Wilmington and Boston spinal orthoses. The current standard of care for nonsurgical treatment of mild and moderate AIS is full-time TLSO wear through skeletal maturity. The role of nighttime bracing options and nonrigid alternatives continues to be explored. Important considerations for the future regarding brace treatment of scoliosis are continued improvements in brace design to maximize patient comfort and compliance and being able to determine more precisely bracing’s efficacy and indications. More accurate assessment of the period of peak growth velocity will enhance our ability to individualize treatment. Fusionless surgical options for controlling progression of scoliosis are promising but remain investigational. The development of genetic testing for scoliosis is an exciting area of research because it will help us better identify those patients at most risk for developing severe scoliosis and individualize treatment protocols. Ultimately, this work may be the gateway to a broader understanding of AIS and its potential cure.
Acknowledgements
We thank G. Dean MacEwen for his commitment to education and his invaluable assistance in the preparation of the manuscript.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Allington NJ, Bowen JR. Adolescent idiopathic scoliosis: treatment with the Wilmington brace. A comparison of full-time and part-time use. J Bone Joint Surg Am. 1996;78:1056–1062. [PubMed] [Google Scholar]
- 2.Andriacchi TP, Schultz AB, Belytschko TB, Dewald R. Milwaukee brace correction of idiopathic scoliosis. A biomechanical analysis and a retrospective study. J Bone Joint Surg Am. 1976;58:806–815. [PubMed] [Google Scholar]
- 3.Apter A, Morein G, Munitz H, Tyano S, Maoz B, Wijsenbeek H. The psychosocial sequelae of the Milwaukee brace in adolescent girls. Clin Orthop Relat Res. 1978;131:156–159. [PubMed] [Google Scholar]
- 4.Bademci G, Batay F, Sabuncuoglu H. First detailed description of axial traction techniques by Serefeddin Sabuncuoglu in the 15th century. Eur Spine J. 2005;14:810–812. doi: 10.1007/s00586-005-0889-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blount W, Schmidt AC, Keever ED, Leonard ET. The Milwaukee brace in the operative treatment of scoliosis. J Bone Joint Surg Am. 1958;40:511–525. [PubMed] [Google Scholar]
- 6.Braun JT, Akyuz E, Ogilvie JW, Bachus KW. The efficacy and integrity of shape memory alloy staples and bone anchors with ligament tethers in the fusionless treatment of experimental scoliosis. J Bone Joint Surg Am. 2005;87:2038–2051. doi: 10.2106/JBJS.D.02103. [DOI] [PubMed] [Google Scholar]
- 7.Bunnell WP, MacEwen GD, Jayakumar S. The use of plastic jackets in the non-operative treatment of idiopathic scoliosis. Preliminary report. J Bone Joint Surg Am. 1980;62:31–38. [PubMed] [Google Scholar]
- 8.Carr WA, Moe JH, Winter RB, Lonstein JE. Treatment of idiopathic scoliosis in the Milwaukee brace. J Bone Joint Surg Am. 1980;62:599–612. [PubMed] [Google Scholar]
- 9.Charles YP, Diméglio A, Canavese F, Daures JP. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser grade 0. J Bone Joint Surg Am. 2007;89:2737–2744. doi: 10.2106/JBJS.G.00124. [DOI] [PubMed] [Google Scholar]
- 10.Climent JM, Sánchez J. Impact of the type of brace on the quality of life of adolescents with spine deformities. Spine. 1999;24:1903–1908. doi: 10.1097/00007632-199909150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Coillard C, Leroux MA, Zabjek KF, Rivard CH. SpineCor—a non-rigid brace for the treatment of idiopathic scoliosis: post-treatment results. Eur Spine J. 2003;12:141–148. doi: 10.1007/s00586-002-0467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coillard C, Vachon V, Circo AB, Beauséjour M, Rivard CH. Effectiveness of the SpineCor brace based on the new standardized criteria proposed by the Scoliosis Research Society for adolescent idiopathic scoliosis. J Pediatr Orthop. 2007;27:375–379. doi: 10.1097/01.bpb.0000271330.64234.db. [DOI] [PubMed] [Google Scholar]
- 13.D’Amato CR, Griggs S, McCoy B. Nighttime bracing with the Providence brace in adolescent girls with idiopathic scoliosis. Spine. 2001;26:2006–2012. doi: 10.1097/00007632-200109150-00014. [DOI] [PubMed] [Google Scholar]
- 14.D’Amato CR, McCoy B. The Providence Scoliosis System Manual. Milwaukee, WI: Scoliosis Research Society; 2003. [Google Scholar]
- 15.Diméglio A, Charles YP, Daures JP, Rosa V, Kaboré B. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am. 2005;87:1689–1696. doi: 10.2106/JBJS.D.02418. [DOI] [PubMed] [Google Scholar]
- 16.Emans JB. Reference Manual for the Boston Scoliosis Brace. Milwaukee, WI: Scoliosis Research Society; 2003. [Google Scholar]
- 17.Emans JB, Kaelin A, Bancel P, Hall JE, Miller ME. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine. 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Galante J, Schultz A, Dewald RL, Ray RD. Forces acting in the Milwaukee brace on patients undergoing treatment for idiopathic scoliosis. J Bone Joint Surg Am. 1970;52:498–506. [PubMed] [Google Scholar]
- 19.Gepstein R, Leitner Y, Zohar E, Angel I, Shabat S, Pekarsky I, Friesem T, Folman Y, Katz A, Fredman B. Effectiveness of the Charleston bending brace in the treatment of single-curve idiopathic scoliosis. J Pediatr Orthop. 2002;22:84–87. doi: 10.1097/00004694-200201000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Hibbs RA. An operation for progressive spinal deformities. New York Med J. 1911;93:1013–1016. [Google Scholar]
- 21.Hibbs RA, Risser JC, Ferguson AB. Scoliosis treated by the fusion operation: an end-result study of three hundred and sixty cases. J Bone Joint Surg Am. 1931;13:91–104. [Google Scholar]
- 22.Hippocrates. The Genuine Works of Hippocrates [translated by Adams F]. New York, NY: Wm Wood; 1849.
- 23.Hooper CR, Reed FE, Price CT. The Charleston Brace. An Orthotist’s Guide to Scoliosis Management. Milwaukee, WI: Scoliosis Research Society; 2003. [Google Scholar]
- 24.Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27:369–374. doi: 10.1097/01.bpb.0000271331.71857.9a. [DOI] [PubMed] [Google Scholar]
- 25.Katz DE, Richards BS, Browne RH, Herring JA. A comparison between the Boston brace and the Charleston bending brace in adolescent idiopathic scoliosis. Spine. 1997;22:1302–1312. doi: 10.1097/00007632-199706150-00005. [DOI] [PubMed] [Google Scholar]
- 26.Lindh M. The effect of sagittal curve changes on brace correction of idiopathic scoliosis. Spine. 1980;5:26–36. doi: 10.1097/00007632-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66:1061–1071. [PubMed] [Google Scholar]
- 28.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76:1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Lovett RH, Brewster AH. The treatment of scoliosis by a different method from that usually employed. J Bone Joint Surg Am. 1924;6:847–857. [Google Scholar]
- 30.Lovett RW. Lateral Curvature of the Spine and Round Shoulders. Philadelphia, PA: P. Blackiston’s Son & Co; 1916. History of scoliosis; pp. 1–7. [Google Scholar]
- 31.Marketos SG, Skiadas PK. Galen: a pioneer of spine research. Spine. 1999;24:2358–2362. doi: 10.1097/00007632-199911150-00012. [DOI] [PubMed] [Google Scholar]
- 32.Moe JH. The Milwaukee brace in the treatment of scoliosis. Clin Orthop Relat Res. 1971;77:18–31. [PubMed] [Google Scholar]
- 33.Moen KY, Nachemson AL. Treatment of scoliosis. An historical perspective. Spine. 1999;24:2570–2575. doi: 10.1097/00007632-199912150-00003. [DOI] [PubMed] [Google Scholar]
- 34.Mostofi SB, editor. Who’s Who in Orthopedics. New York, NY: Springer; 2005. [Google Scholar]
- 35.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:815–822. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 36.National Scoliosis Foundation. A new alternative treatment for idiopathic scoliosis. Available at: www.scoliosis.org/resources/medicalupdates/spinecor.php. Accessed July 29, 2008.
- 37.Newton P. Idiopathic scoliosis. In: Morrissey RT, Weinstein SL, editors. Lovell & Winter’s Pediatric Orthopaedics. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 693–762. [Google Scholar]
- 38.Noonan KJ. Nonsurgical techniques in adolescent idiopathic scoliosis. In: Weinstein SL, editor. The Pediatric Spine: Principles and Practice. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. pp. 371–383. [Google Scholar]
- 39.Noonan KJ, Weinstein SL, Jacobson WC, Dolan LA. Use of the Milwaukee brace for progressive idiopathic scoliosis. J Bone Joint Surg Am. 1996;78:557–567. doi: 10.2106/00004623-199604000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Ogilvie JW. Historical aspects of scoliosis. In: Lonstein J, Winter R, Bradford D, Ogilvie J, editors. Moe’s Textbook of Scoliosis and Other Spinal Deformities. Philadelphia, PA: WB Saunders; 1995. pp. 1–5. [Google Scholar]
- 41.Ogilvie JW, Braun J, Argyle V, Nelson L, Meade M, Ward K. The search for idiopathic scoliosis genes. Spine. 2006;31:679–681. doi: 10.1097/01.brs.0000202527.25356.90. [DOI] [PubMed] [Google Scholar]
- 42.Paré A. The Works of that Famous Churugion Ambrose Paré [translated by Johnson T, Cotes T, Young R]. London, UK: Clark J; 1634.
- 43.Peltier LF, editor. Orthopaedics: A History and Iconography. Novato, CA: Norman Publishing; 1993. [Google Scholar]
- 44.Piazza MR, Bassett GS. Curve progression after treatment with the Wilmington brace for idiopathic scoliosis. J Pediatr Orthop. 1990;10:39–43. [PubMed] [Google Scholar]
- 45.Ponseti IV, Friedman B. Prognosis in idiopathic scoliosis. J Bone Joint Surg Am. 1950;32:381–395. [PubMed] [Google Scholar]
- 46.Price CT, Scott DS, Reed FE, Jr, Riddick MF. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace. Preliminary report. Spine. 1990;15:1294–1299. doi: 10.1097/00007632-199012000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Price CT, Scott DS, Reed FR, Jr, Sproul JT, Riddick MF. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace: long-term follow-up. J Pediatr Orthop. 1997;17:703–707. doi: 10.1097/00004694-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 49.Riesz PB. The life of Wilhelm Conrad Roentgen. AJR Am J Roentgenol. 1995;165:1533–1537. doi: 10.2214/ajr.165.6.7484601. [DOI] [PubMed] [Google Scholar]
- 50.Risser JC. The application of body casts for the correction of scoliosis. Instr Course Lect. 1955;12:255. [PubMed] [Google Scholar]
- 51.Risser JC. The iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop Relat Res. 1958;11:111–119. [PubMed] [Google Scholar]
- 52.Risser JC. Scoliosis: past and present. J Bone Joint Surg Am. 1964;46:167–199. [PubMed] [Google Scholar]
- 53.Rivard CH, Coillard C. SpineCor System Bracing Manual. Milwaukee, WI: Scoliosis Research Society; 2002. [Google Scholar]
- 54.Röntgen WC. Ueber eine neue Art von Strahlen. Annalen der Physik. 1895;300:12–17. doi: 10.1002/andp.18983000103. [DOI] [Google Scholar]
- 55.Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90:540–553. doi: 10.2106/JBJS.G.00004. [DOI] [PubMed] [Google Scholar]
- 56.Sauvegrain J, Nahum H, Bronstein H. Study of bone maturation of the elbow [in French] Ann Radiol (Paris) 1962;5:542–550. [PubMed] [Google Scholar]
- 57.Sayre LA, Yale LM, George WA. Lectures on Orthopedic Surgery and Disease of the Joints. New York, NY: D. Appleton & Colleagues; 1892. [Google Scholar]
- 58.Sayre JW. Lewis Albert Sayre. Spine. 1995;20:1091–1096. doi: 10.1097/00007632-199505000-00019. [DOI] [PubMed] [Google Scholar]
- 59.Smith AD. Scoliosis. J Bone Joint Surg Am. 1958;40:505–507. [PubMed] [Google Scholar]
- 60.Trivedi JM, Thomson JD. Results of Charleston bracing in skeletally immature patients with idiopathic scoliosis. J Pediatr Orthop. 2001;21:277–280. doi: 10.1097/00004694-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 61.University of Iowa Hospitals and Clinics. The Debate on Clothing as a Cause of Scoliosis. Available at: www.uihealthcare.com/depts/medmuseum/wallexhibits/scoliosis/history/scolhistory.html. Accessed February 1, 2009.
- 62.Watts HG, Hall JE, Stanish W. The Boston brace system for the treatment of low thoracic and lumbar scoliosis by the use of a girdle without superstructure. Clin Orthop Relat Res. 1977;126:87–92. [PubMed] [Google Scholar]
- 63.Yrjönen T, Ylikoski M, Schlenzka D, Kinnunen R, Poussa M. Effectiveness of the Providence nighttime bracing in adolescent idiopathic scoliosis: a comparative study of 36 female patients. Eur Spine J. 2006;15:1139–1143. doi: 10.1007/s00586-005-0049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zampini JM, Sherk HH, Lewis A. Sayre: the first Professor of Orthopaedic Surgery in America. Clin Orthop Relat Res. 2008;466:2263–2267. doi: 10.1007/s11999-008-0349-6. [DOI] [PMC free article] [PubMed] [Google Scholar]