Abstract
Background:
Surgical residency training is evolving, and trainees who wish to practice hepato-pancreato-biliary (HPB) surgery in the future will be required to obtain advanced training. As this paradigm evolves, it is crucial that HPB fellowship incorporation into an established surgical residency programme does not diminish surgical residents' exposure to complex HPB procedures. We hypothesized that incorporation of a HPB fellowship in a high-volume clinical training programme would not detract from residents' HPB experience.
Methods:
Resident operative case logs and HPB fellow case logs were reviewed. Resident exposure to complex HPB procedures for 3 years prior to and 3 years after fellowship incorporation were compared.
Results:
No significant changes in surgical resident exposure to liver and pancreatic resection were seen between the two time periods. Surgical resident exposure to complex biliary procedures decreased in the 3 years after HPB fellowship incorporation (P= 0.003); however, exceeded the national average in each year except 2006. Graduating residents' overall HPB experience was unchanged in the 3 years prior to and after incorporating an HPB fellow. Expansion of HPB volume was a critical part of successful HPB fellowship implementation.
Discussion:
An HPB fellowship programme can be incorporated into a high-volume clinical training programme without detracting from resident HPB experience. Individual training programmes should carefully assess their capability to provide an adequate clinical experience for fellows without diminishing resident exposure to complex HPB procedures.
Keywords: resident education, hepato-pancreato-biliary surgery fellowship, fellowship training, hepato-pancreato-biliary surgery, hepato-pancreato-biliary
Introduction
In the United States, residency training in general surgery is currently undergoing a major paradigm shift. Restructuring of surgical education programmes around the Accreditation Council for Graduate Medical Education (ACGME) core competencies, the challenge of operating within duty hour restrictions and external pressure for increased resident supervision all contribute to this change.1,2
The Surgical Council on Resident Education (SCORE), created in 2004, is a voluntary consortium of six organizations invested in surgical residency training, including the American Board of Surgery, the American College of Surgeons, the American Surgical Association, the Residency Review Committee for Surgery (of the ACGME), the Association of Program Directors in Surgery and the Association for Surgical Education. The SCORE consortium has defined competencies expected of a general surgery residency graduate, including a list of diseases and conditions that a general surgeon should be competent in caring for and a list of operations and procedures they should be competent in performing.3 Implicit in these SCORE recommendations are the diseases and procedures that require additional training to achieve competence.
Specific surgical procedures have been defined by SCORE as essential (common and uncommon), in which specific procedural competency is required by the end of general surgery residency training, and complex, in which generic experience is required, but not competence in specific procedures. Notably, virtually all elective liver, pancreas and complex biliary procedures fall under the SCORE category complex (Table 1). This categorization suggests that trainees who wish to focus their practice around hepato-pancreato-biliary (HPB) surgery will require further training.
Table 1.
Score definition of operative procedures for general surgery trainees
| ESSENTIAL – COMMON: Frequently performed operations in general surgery; specific procedure competency is required by end of training (and should be attainable primarily by case volume). |
| LIVER: needle/wedge biopsy (open or laparoscopic) |
| PANCREAS: none |
| BILIARY: cholecystectomy with/without cholangiography (open or laparoscopic) |
| ESSENTIAL – UNCOMMON: Rare, often urgent, operations seen in general surgery practice and not typically done in significant numbers by trainees; specific procedure competency required by end of training (but cannot be attained by case volume alone) |
| LIVER: drainage liver abscess |
| PANCREAS: none |
| BILIARY: cholecystostomy; common bile duct exploration (open); cholodochoenteric anastomosis; operation for gallbladder cancer (when found incidentally); repair acute bile duct injury. |
| COMPLEX: Not consistently performed by general surgeons in training and not typically performed in general surgery practice. Generic experience in complex procedures in residency is required but not competence in individual procedures. Some residency programmes may provide sufficient experience for competence in some specific procedures. |
| LIVER: segmentectomy/lobectomy (open and laparoscopic); intra-operative ultrasound of the liver; portal-systemic shunt |
| PANCREAS: pancreaticoduodenectomy; total pancreatectomy; ampullary resection for tumour; distal pancreatectomy; longitudinal pancreaticojejunostomy; Frey procedure; Beger procedure; intraoperative pancreatic ultrasound; pancreatic debridement for necrosis (open/laparoscopic/endoscopic); drainage pancreatic pseudocyst. |
| BILIARY: laparoscopic common bile duct exploration; operation for gallbladder cancer (planned); operation for bile duct cancer; excision choledochal cyst; transduodenal sphincteroplasty. |
The number of surgical residents seeking advanced fellowship training in various subspecialties has increased. In fact, current data show that nearly 80% of graduating surgical residents will go on to fellowship training in some form.4,5 This trend includes residents entering advanced training in complex gastrointestinal (GI) surgery. Over the 5-year time frame spanning 2004–08, the number of general surgery residency graduates entering fellowship training in GI surgery (excluding colorectal) has increased by more than 50%.2
Historically, surgical residents interested in acquiring formal advanced training in HPB surgery have sought fellowships in either surgical oncology or transplantation. More recently, however, the number of fellowships focusing specifically on advanced GI and HPB surgery has grown rapidly. The Fellowship Council is responsible for accreditation of and administrating the match process for approximately 125 advanced general surgery fellowships in minimally invasive, bariatric, upper GI and endoscopic surgery. Currently, the Fellowship Council recognizes 11 programmes offering advanced HPB training (7 accredited and 4 pending), and several other institutions are offering HPB fellowships outside of the Fellowship Council umbrella. Currently all HPB programmes accredited through the Fellowship Council must meet specific criteria to be Accredited as an HPB programme.
Guidelines for what constitutes appropriate standards for HPB fellowship training are in evolution. The education and training committee of the International Hepato-Pancreato-Biliary Association has proposed objectives and programme requirements (available at http://www.ihpba.org/hpb-training-standards.html), but formalized accreditation in HPB surgery is not yet universally standardized. A critical consideration for any institution wishing to provide advanced HPB training is preserving general surgery trainees' HPB experience.
With this background firmly in mind, in 2005 our institution formally incorporated an HPB fellowship into the surgical training programme. Factors that went into this decision were (i) the fact that our residents were already above the 90th percentile in HPB operations, and (ii) the expectation that HPB volumes would increase with the addition of a new faculty. The aim of the current study was therefore to critically evaluate our surgical residents' exposure to complex HPB procedures over the 3 years prior to and following the start of the HPB fellowship. We hypothesized that incorporating an HPB fellowship into our high-volume clinical training programme (with the anticipation of increased HPB case volume) would not detract from surgical residents' HPB experience.
Materials and methods
A formal HPB fellowship was instituted at Indiana University during the educational year 2005–06. Records from the 3 years prior to and the 3 years after this time were acquired for comparison.
Resident and Fellow HPB operative experience
During this 6-year period, the surgery training programme graduated 8–10 chief residents per year; one HPB fellow per year participated in the training programme during the latter 3 years. Senior residents in our programme have 6-week long rotations, and are exposed to HPB operations primarily while rotating through two HPB services at the Indiana University Hospital, a 350-bed tertiary care facility. Additional resident HPB exposure is provided at three other facilities: the Methodist Hospital (a 620-bed private hospital), Wishard Memorial Hospital (a 300-bed county hospital) and the Roudebush Veteran's Administration (VA) Hospital (a 190-bed tertiary VA hospital). The HPB fellow's primary responsibility is to serve as the team leader of one HPB service at Indiana University Hospital, with occasional participation in HPB operations on the other University Hospital HPB service.
Resident and Fellow operative case logs
Operative case experience for graduating chief residents is provided to the programme yearly by the ACGME. Each HPB fellow is responsible for maintaining an individual operative log. National resident operative data are in the public domain, and were obtained by accessing the ACGME website (http://www.acgme.org/residentdatacollection/documentation/statistical_reports.asp).
Definitions of HPB procedures
HPB procedures are categorized under the Residency Review Committee area ‘Abdomen.’ Liver procedures include the subcategories lobectomy or segmentectomy, wedge resection/open biopsy and other major liver. Pancreatic procedures are categorized as pancreas resection – distal, pancreas resection – Whipple/total, drainage pseudocyst (all types) and pancreaticojejunostomy and other major pancreas. Biliary procedures are categorized as cholecystostomy/cholecystectomy, common bile duct exploration – open, common bile duct exploration – laparoscopic, choledochoenteric anastomosis, sphinteroplasty (Oddi) and other major biliary. For this analysis, we were interested in complex biliary procedures, and therefore excluded cholecystostomy/cholecystectomy. This subgroup analysis prohibited accurate calculation of the standard deviation from national data regarding complex biliary procedures. We used the numbers reported as ‘Total surgeon’ in each category.
Statistical analysis
Data are presented as mean ± standard deviation. Student's t-test and anova were applied where appropriate, and a P-value < 0.05 was accepted as statistically significant.
Results
Consolidated data regarding IU resident, HPB fellow and national resident average HPB operative experience during the years 2003–08 are shown in Table 2. During this time period, the ACGME required graduating chief residents to have exposure to a minimum of four liver and three pancreas cases; mandatory requirements for complex biliary procedures were not subdivided from the category ‘Abdomen – biliary.’ The IHPBA guidelines for HPB fellowship training call for exposure to 25 liver, 30 pancreas and 20 complex biliary cases.
Table 2.
Consolidated US graduating surgery resident, Indiana University graduating surgery resident and Indiana University HPB fellow HPB experience, 2003–08
|
Liver |
Pancreas |
Complex biliary |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| US Avg | Resident | Fellow | US Avg | Resident | Fellow | US Avg | Resident | Fellow | |
| 2003 | 8 ± 5 | 20 ± 9 | – | 9 ± 6 | 20 ± 10 | – | 5 | 7 ± 4 | – |
| 2004 | 8 ± 5 | 22 ± 9 | – | 10 ± 7 | 22 ± 5 | – | 6 | 11 ± 6 | – |
| 2005 | 8 ± 5 | 8 ± 4 | – | 10 ± 7 | 23 ± 7 | – | 6 | 11 ± 7 | – |
| 2006 | 9 ± 5 | 14 ± 4 | 40 | 10 ± 7 | 23 ± 9 | 100 | 5 | 4 ± 3a | 38 |
| 2007 | 9 ± 5 | 16 ± 5 | 42 | 11 ± 8 | 24 ± 8 | 109 | 5 | 9 ± 2a | 44 |
| 2008 | 9 ± 5 | 13 ± 5 | 40 | 11 ± 8 | 19 ± 6 | 114 | 2 | 5 ± 2a | 56 |
US Avg, average cases by graduating United States surgery residents.
P= 0.003 vs. 2003–05.
Liver resection
The Indiana University graduating chief resident, HPB fellow and national graduating chief resident's average experience with liver resection over the time period 2003–08 is illustrated in Fig. 1. No significant change was observed in chief resident exposure to liver resection between the time periods before and after incorporation of the HPB fellowship (P= 0.11); graduating chief resident exposure to liver resection was greater than the national average in each of these 6 years. The HPB fellow performed an average of 41 liver resections yearly.
Figure 1.
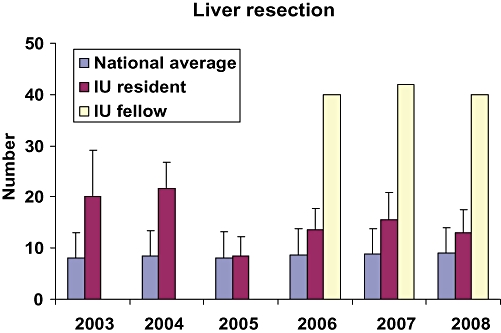
Liver resection experience of United States residents, Indiana University residents and Indiana University hepato-pancreato-biliary (HPB) fellow, 2003–08
Pancreatic resection
Graduating chief resident and HPB fellow exposure to pancreatic operations is shown in Fig. 2. Similar to the liver resection experience, no significant difference was seen in graduating chief resident exposure to pancreatic operations before and after HPB fellowship incorporation (P= 0.7), and the number of pancreatic operations performed by chief residents was greater than the national average in each year. The HPB fellow performed an average of 108 pancreatic operations yearly.
Figure 2.
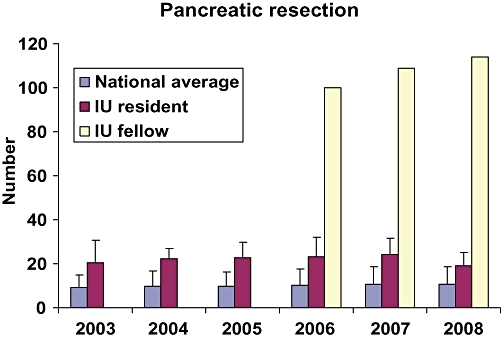
Pancreatic resection experience of United States residents, Indiana University residents and Indiana University hepato-pancreato-biliary (HPB) fellow, 2003–08
Complex biliary procedures
Graduating chief resident and HPB fellow exposure to complex biliary operations is demonstrated in Fig. 3. Graduating chief residents were exposed to fewer complex biliary operations over the 3-year time frame after incorporation of the HPB fellowship (P= 0.003). Despite this decrease, graduating chief residents performed more than the national average complex biliary procedure in each year except 2006. While the national average graduating resident exposure to complex biliary procedures was not significantly different between the two 3-year time points 2003–05 vs. 2006–08 (5.6 ± 1.3 vs. 4.3 ± 2.7; P= 0.11), a steep decrease occurred in the calendar year 2008 (to a national average experience of 2.4 cases). The HPB fellow performed an average of 46 complex biliary procedures each year.
Figure 3.
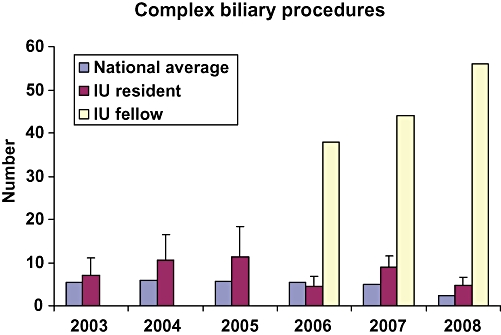
Complex biliary procedure experience of United States residents, Indiana University residents and Indiana University hepato-pancreato-biliary (HPB) fellow, 2003–08
Total resident and fellow HPB operative experience
The total number of HPB procedures performed by Indiana University graduating chief residents and HPB fellows during the time period 2003–08 is shown in Fig. 4. Graduating chief resident's overall HPB experience was not changed in the 3 years prior to and after incorporation of the HPB fellowship. However, as anticipated, the total number of HPB operations increased as the new faculty were recruited.
Figure 4.
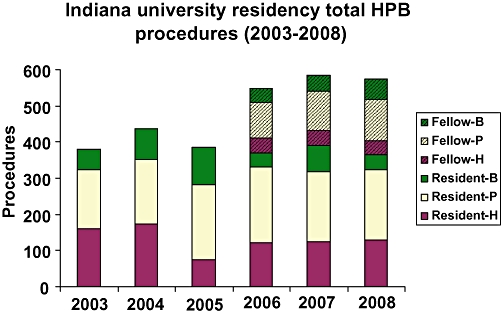
Indiana University General Surgery Residency total HPB procedural experience, 2003–08
Discussion
These data demonstrate that an HPB fellowship programme can be successfully incorporated into a high-volume clinical training programme without significantly detracting from surgical resident HPB experience. Compared with the years immediately prior to incorporating the HPB fellowship, our graduating residents performed similar numbers of major liver and pancreatic operations. Graduating resident exposure to complex biliary procedures decreased slightly after HPB fellowship incorporation; however, resident exposure to these rare cases was still greater than the national norm. Overall graduating resident experience with HPB procedures did not change during the time periods before and after incorporating the HPB fellowship.
Advanced training in HPB surgery is a topic of great current interest, as reflected by recent presidential addresses to the American Hepato-Pancreato-Biliary Association. In 2006, president Theodore N. Pappas used nationwide inpatient sample data to extrapolate the future need for HPB surgeons, and concluded that the current training paradigm, including surgical oncology, transplant and HPB programmes, will result in nearly twice as many HPB surgeons as are needed by the year 2020.6 Last year, president Bruce Schirmer cited decreased surgical resident exposure to complex HPB procedures and the changing face of resident education as evidenced by SCORE definitions to make the point that advanced training in HPB surgery will be mandatory in the future, and thus the next important step will be identifying appropriate centres to support this endeavour (B. Schirmer, personal communication; manuscript in submission).
Surgical residents' experience with complex HPB procedures such as common bile duct exploration and choledochoenteric anastomosis is decreasing.7,8 Similarly, while the average number of liver and pancreas operations performed by graduating surgery residents are 9 and 10, respectively, the mode (most commonly reported number) are 0 and 1.7 This experience is clearly not enough to support independent HPB practice, with its documented steep learning curve.9 Indeed, with the current training milieu of resident work hour restrictions and decreased emphasis on exposure to complex HBP procedures emphasized by the SCORE definitions, advanced fellowship training is the logical approach for residents wishing to practice HPB surgery in the future. Two important questions necessarily follow: what are the fundamental concepts and operative experience required to achieve competence in this complex discipline, and which programmes have the necessary substrate to provide this intellectual and clinical exposure (particularly without degrading surgery resident experience)?
The IHPBA Education and Training Committee have provided a strong framework to answer the first question, including definitions, objectives, and programme requirements for advanced HPB training. In addition to technical skills, these training objectives and programme requirements emphasize the need for knowledge, clinical experience, training in research and education, and leadership in HPB disease as integral to the core of HPB training. Other national and regional societies such as the AHPBA have developed and are currently developing similar guidelines, with the ultimate goal of standardizing the structured educational and training experience necessary to achieve expertise in HPB surgery.
A somewhat more difficult challenge lies in identifying which training programmes have the ability to support a fellowship in HPB surgery, particularly without detracting significantly from general surgery resident HPB experience. Our data suggest that at least from the operative standpoint, centres supporting a high-volume clinical HPB practice are well positioned in this respect. In our situation, assigning the HPB fellow's responsibility primarily to one clinical service permitted residents' HPB exposure to other services to remain intact. In addition, increased overall HPB volumes also cushioned the impact of the fellow. During the time period of this study, one HPB surgeon retired and four new HPB faculty were added (KDL, AN, HAP, NJZ).
As illustrated by the IHPBA guidelines, operative experience represents only one piece of the training puzzle. Equally important (yet a bit more difficult to quantify) is how to provide clinical education outside of the operating room. Team ward rounds (both ‘work’ and ‘teaching’) have traditionally played a prominent role in surgical education, and remain important today. In addition, small group and multidisciplinary educational conferences such as tumour boards offer excellent mechanisms to assure ‘generic competence’ in complex pathological processes and operative strategy.
As an example, we offer a weekly, hour-long GI surgery conference for all residents and medical students rotating on the Indiana University Hospital surgical services. This case-based conference is led by several faculty members; questions regarding the management of a patient with a complex GI problem are directed towards the senior residents. A loose schedule rotates cases in foregut, liver, biliary, pancreas and hindgut, ensuring that each of these topics is covered during every resident rotation block. In addition, the HPB fellow and residents rotating on GI surgery services routinely participate in ‘working’ multidisciplinary conferences including the GI/pancreas, liver tumour and GI oncology groups.
It is not uncommon that initiation of a new fellowship is met with some reluctance from the resident staff, who fear that the fellow will ‘steal’ all of the complex cases. Our experience highlights some of the positive aspects of a fellowship – that a fellow can actually enhance resident (and medical student) education. A fellow by definition has completed general surgery training and commonly functions as junior faculty. This advanced experience, in conjunction with an extended close relationship with faculty supervisors, makes the fellow an excellent liaison between the faculty and resident staff. In addition, the fellow has an intense interest and advanced knowledge of specific complex disease processes and procedures. In this capacity, the fellow functions as an instructor in day-to-day interaction with residents – on rounds, providing off-the-cuff ‘chalk talks’ and in the operating room. In fact, residents' initial reluctance but ultimate overall satisfaction with a new fellow has been documented in a wide spectrum of medical specialties ranging from gynaecological oncology to orthopaedics to urology.10–12
Advanced training in HPB surgery will be necessary for surgeons wishing to practice HPB surgery in the future. Our data show that an HPB fellowship programme can be incorporated into a high-volume clinical training programme without detracting from resident HPB experience. As HPB fellowships evolve, individual training programmes should carefully assess their capability to provide an adequate clinical experience for fellows without diminishing resident exposure to complex HPB procedures.
Conflict of interest
None declared.
References
- 1.Sachdeva AK, Bell RH, Jr, Britt LD, Tarpley JL, Blair PG, Tarpley MJ. National efforts to reform residency education in surgery. Acad Med. 2007;82:1200–1210. doi: 10.1097/ACM.0b013e318159e052. [DOI] [PubMed] [Google Scholar]
- 2.Bell RH., Jr Graduate education in general surgery and its related specialties and subspecialties in the United States. World J Surg. 2008;32:2178–2184. doi: 10.1007/s00268-008-9658-x. [DOI] [PubMed] [Google Scholar]
- 3.General Surgery Residency Patient Care Curriculum Outline 2008–2009. http://home.absurgery.org/xfer/patientcareoutline408.pdf; Accessed 12 January 2010.
- 4.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206:782–788. doi: 10.1016/j.jamcollsurg.2007.12.012. discussion 788–9. [DOI] [PubMed] [Google Scholar]
- 5.Stitzenberg KB, Sheldon GF. Progressive specialization within general surgery: adding to the complexity of workforce planning. J Am Coll Surg. 2005;201:925–932. doi: 10.1016/j.jamcollsurg.2005.06.253. [DOI] [PubMed] [Google Scholar]
- 6.Scarborough JE, Pietrobon R, Bennett KM, Clary BM, Kuo PC, Tyler DS, et al. Workforce projections for hepato-pancreato-biliary surgery. J Am Coll Surg. 2008;206:678–684. doi: 10.1016/j.jamcollsurg.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12:153–158. doi: 10.1007/s11605-007-0378-6. [DOI] [PubMed] [Google Scholar]
- 8.Chang YJ, Mittal VK. Hepato-pancreato-biliary training in general surgery residency: is it enough for the real world? Am J Surg. 2009;197:291–295. doi: 10.1016/j.amjsurg.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Tseng JF, Pisters PW, Lee JE, Wang H, Gomez HF, Sun CC, et al. The learning curve in pancreatic surgery. Surg. 2007;141:694–701. doi: 10.1016/j.surg.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Cohn DE, Roney JD, O'Malley DM, Valmadre S. Residents' perspectives on surgical training and the resident-fellow relationship: comparing residency programs with and without gynecological oncology fellowships. Int J Gynecol Cancer. 2008;18:199–204. doi: 10.1111/j.1525-1438.2007.00986.x. [DOI] [PubMed] [Google Scholar]
- 11.Duffy JW, 3rd, Thomas JC, Makari JH, Gold DG, Demarco RT, Adams MC, et al. The impact of a fellowship on resident training in an academic pediatric urology practice. J Urol. 2008;179:720–723. doi: 10.1016/j.juro.2007.09.104. discussion 723. [DOI] [PubMed] [Google Scholar]
- 12.Perler BA, Zuidema GD. The effect of vascular fellowships on general surgical residency training. Ann Surg. 1984;200:247–254. doi: 10.1097/00000658-198409000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]


