Abstract
OBJECTIVE
We have already reported that A1C is elevated because of iron deficiency in late pregnancy among nondiabetic pregnant women. This report examined whether the same phenomenon is observed in pregnant women with diabetes.
RESEARCH DESIGN AND METHODS
This longitudinal study was conducted in 17 pregnant women with diabetes (20–35 weeks of pregnancy). A1C, serum glycated albumin, erythrocyte indexes, and iron metabolism indexes were measured.
RESULTS
A1C levels were significantly increased in late pregnancy, whereas serum glycated albumin showed no significant changes. Glycated albumin/A1C ratio, mean corpuscular hemoglobin, serum transferrin saturation, and serum ferritin were significantly decreased in late pregnancy. Serum transferrin saturation showed a significant positive correlation with glycated albumin/A1C ratio.
CONCLUSIONS
A1C levels, but not serum glycated albumin levels, are elevated in late pregnancy because of iron deficiency in diabetic women. Serum glycated albumin may offer an adequate marker for glycemic control during pregnancy.
In pregnant women with diabetes, namely women with gestational diabetes, type 2 diabetes, or type 1 diabetes, tight glycemic control during pregnancy is essential to reduce the risk of intrauterine fetal death, fetal growth abnormalities, and maternal complications (1). In patients with diabetes, several glycated proteins can be used as markers to evaluate glycemic control. Among them, A1C is currently in wide use as the standard marker for clinical management of diabetes (2).
A1C is influenced not only by blood glucose levels, but also by conditions that affect erythrocyte survival (3). Although in patients with iron deficiency anemia, A1C is known to be elevated (4), we recently found that A1C levels are also elevated in iron deficiency states without anemia (5). Furthermore, a study in nondiabetic pregnant women on correlations between glycemic control markers (A1C and serum glycated albumin) and iron deficiency status reported that in late pregnancy, A1C levels were increased because of iron deficiency, but serum glycated albumin levels were not influenced by such conditions (6).
Accordingly, we believed that a similar study on glycemic control markers in pregnant women with diabetes would be clinically important. We therefore conducted this study in pregnant women with diabetes.
RESEARCH DESIGN AND METHODS
This longitudinal study was conducted in 17 Japanese pregnant women with diabetes who were evaluated between January 2007 and August 2009 at Aizenbashi Hospital or Osaka Medical Center and Research Institute for Maternal and Child Health. Mean age of the women was 30.5 ± 4.1 years. Category of diabetes for the study patients was gestational diabetes in 6, type 2 diabetes in 4, and type 1 diabetes in 7. Diabetes treatment was dietary therapy alone in 4 and insulin therapy in 13. During the observation period, iron and vitamin supplements were not permitted. The pregnancy period was divided into four terms of 4 weeks each, starting at gestational week 20: Term I, 20–23 weeks; term II, 24–27 weeks; term III, 28–31 weeks; and term IV, 32–35 weeks. In each term, A1C, serum glycated albumin, erythrocyte (red blood cell) count, hematocrit, hemoglobin mean corpuscular hemoglobin, serum transferrin saturation, and serum ferritin were measured. A1C was measured by high-performance liquid chromatography (ADAMS-A1C HA-8160; Arkray, Kyoto, Japan) (7) with calibration using Japan Diabetes Society (JDS) Lot 2 (8). Serum glycated albumin was determined by enzymatic methods using albumin-specific protease, ketoamine oxidase, and albumin assay reagent (Lucica GA-L; Asahi Kasei Pharma, Tokyo, Japan) (9). Blood cell counts, hematocrit, hemoglobin, and mean corpuscular hemoglobin were measured using an automated hematology system. Serum ferritin concentrations were measured by chemiluminescent immunoassay. Serum transferrin saturation was calculated by dividing serum iron by total iron binding capacity determined by the calorimetric method.
RESULTS
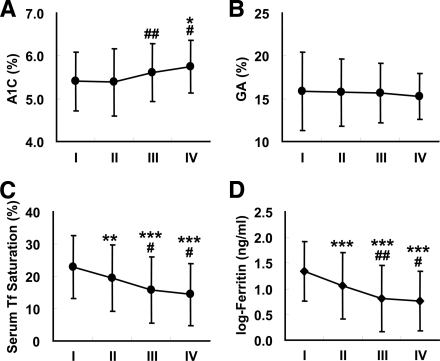
Figure 1 shows A1C levels and serum glycated albumin levels in the four terms during pregnancy. A1C levels increased as pregnancy progressed, with a significant increase in late pregnancy (term I, 5.4 ± 0.7%; term II, 5.4 ± 0.8%; term III, 5.6 ± 0.7%; term IV, 5.7 ± 0.6%; P < 0.05 for each of term I versus IV and term II versus IV; P < 0.01 for term II versus III). By contrast, serum glycated albumin levels did not change significantly during the four terms. Glycated albumin/A1C ratio decreased as pregnancy progressed, with a significant decrease in late pregnancy (term I, 2.91 ± 0.47; term II, 2.90 ± 0.36; term III, 2.78 ± 0.36; term IV, 2.65 ± 0.30; P < 0.05 for term I versus term III; P < 0.01 for each of term I versus IV, term II versus III and term III versus IV; P < 0.001 for term II versus IV).
Figure 1.
Changes in A1C (A), serum glycated albumin (GA) (B), serum transferrin (Tf) saturation (C), and serum ferritin (log transformation) (D) during pregnancy. Term I, 20–23 weeks; term II, 24–27 weeks; term III, 28–31 weeks; term IV, 32–35 weeks. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. term I; #P < 0.05 and ##P < 0.01 vs. term II.
Red blood cell count did not change during pregnancy, but mean corpuscular hemoglobin in term IV was significantly decreased (term I, 29.9 ± 1.8 pg; term II, 29.9 ± 2.0 pg; term III, 29.6 ± 2.3 pg; term IV, 28.7 ± 2.7 pg; P < 0.01 for term I versus IV, P < 0.001 for each of term II versus IV and term III versus IV). Also, serum transferrin saturation (term I, 22.8 ± 9.7%; term II, 19.4 ± 10.2%; term III, 15.8 ± 10.3%; term IV, 14.4 ± 9.6%; P < 0.05 for each of term II versus III and term II versus IV; P < 0.01 for term I versus II; P < 0.001 for each of term I versus III and term I versus IV) and log-ferritin (term I, 1.35 ± 0.58; term II, 1.06 ± 0.64; term III, 0.81 ± 0.64; term IV, 0.76 ± 0.58; P < 0.05 for term II versus IV; P < 0.01 for term II versus III; P < 0.001 for term I versus II, term I versus III and term I versus IV) decreased as pregnancy progressed, with a significant decrease in late pregnancy (Fig. 1).
Analysis of the correlation between glycated albumin/A1C ratio and iron metabolism indexes using univariate analysis showed that serum transferrin saturation showed a significant positive correlation with glycated albumin/A1C ratio (R = 0.297, P = 0.0214).
CONCLUSIONS
In normal pregnancy, A1C shows biphasic changes with a nadir in mid-pregnancy (10,11). The decrease in A1C levels until mid-pregnancy is thought to be due to a decline in blood glucose levels from early to mid-pregnancy. Conversely, Nielsen et al. (12) have reported that A1C levels begins to decline from early pregnancy and is further decreased in late pregnancy. In their study, whether pregnant women had iron deficiency was not investigated.
In patients with gestational diabetes during treatment or with a previous history of diabetes during pregnancy, some discrepancies between A1C levels and changes in blood glucose levels have been reported (13).
Given hemodilution seen in pregnancy, serum protein concentration decreases, and thus fructosamine levels can be influenced during pregnancy. Serum glycated albumin measures glycated albumin as a ratio of serum albumin and is therefore unaffected by the serum albumin concentration. During pregnancy, glycated albumin levels have been reported to decrease slightly from early to mid-pregnancy (14). In our study, from mid-pregnancy to late pregnancy, no significant change in serum glycated albumin levels was identified. Similar results were also reported by Abe et al. (15).
Based on our findings, not only in nondiabetic pregnant women, but also in pregnant women with diabetes, it is important to keep in mind that iron deficiency and an increase in A1C levels can occur in late pregnancy. By contrast, serum glycated albumin levels are unaffected by iron deficiency and thus may offer an adequate marker for monitoring glycemic control during pregnancy.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Lauenborg J, Mathiesen E, Ovesen P, Westergaard JG, Ekbom P, Mølsted-Pedersen L, Damm P: Audit on stillbirths in women with pregestational type 1 diabetes. Diabetes Care 2003;26:1385–1389 [DOI] [PubMed] [Google Scholar]
- 2. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 2004;27 (Suppl. 1):S15–S35 [DOI] [PubMed] [Google Scholar]
- 3. Fitzgibbons JF, Koler RD, Jones RT: Red cell age-related changes of hemoglobins AIa+b and AIc in normal and diabetic subjects. J Clin Invest 1976;58:820–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coban E, Ozdogan M, Timuragaoglu A: Effect of iron deficiency anemia on the levels of hemoglobin A1c in nondiabetic patients. Acta Haematol 2004;112:126–128 [DOI] [PubMed] [Google Scholar]
- 5. Koga M, Morita S, Saito H, Mukai M, Kasayama S: Association of erythrocyte indices with glycated haemoglobin in pre-menopausal women. Diabet Med 2007;24:843–847 [DOI] [PubMed] [Google Scholar]
- 6. Hashimoto K, Noguchi S, Morimoto Y, Hamada S, Wasada K, Imai S, Murata Y, Kasayama S, Koga M: A1C but not serum glycated albumin is elevated in late pregnancy owing to iron deficiency. Diabetes Care 2008;31:1945–1948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Davis JE, McDonald JM, Jarett L: A high-performance liquid chromatography method for hemoglobin A1C. Diabetes 1978;27:102–107 [DOI] [PubMed] [Google Scholar]
- 8. Tominaga M, Makino H, Yoshino G, Kuwa K, Takei I, Aono Y, Hoshino T, Umemoto M, Shimatsu A, Sanke T, Kuwashima M, Taminato T, Ono J: Japanese standard reference material for JDS Lot 2 haemoglobin A1c. I: Comparison of Japan Diabetes Society-assigned values to those obtained by the Japanese and USA domestic standardization programmes and by the International Federation of Clinical Chemistry reference laboratories. Ann Clin Biochem 2005;42:41–46 [DOI] [PubMed] [Google Scholar]
- 9. Kouzuma T, Usami T, Yamakoshi M, Takahashi M, Imamura S: An enzymatic method for the measurement of glycated albumin in biological samples. Clin Chim Acta 2002;324:61–71 [DOI] [PubMed] [Google Scholar]
- 10. Phelps RL, Honig GR, Green D, Metzger BE, Frederiksen MC, Freinkel N: Biphasic changes in haemoglobin A1c concentrations during normal human pregnancy. Am J Obstet Gynecol 1983;147:651–653 [DOI] [PubMed] [Google Scholar]
- 11. Worth R, Potter JM, Drury J, Fraser RB, Cullen DR: Glycosylated haemoglobin in normal pregnancy: a longitudinal study with two independent methods. Diabetologia 1985;28:76–69 [DOI] [PubMed] [Google Scholar]
- 12. Nielsen LR, Ekbom P, Damm P, Glümer C, Frandsen MM, Jensen DM, Mathiesen ER: HbA1C levels are significantly lower in early and late pregnancy. Diabetes Care 2004;27:1200–1201 [DOI] [PubMed] [Google Scholar]
- 13. Griffiths RJ, Vinall PS, Stickland MH, Wales JK: Haemoglobin A1c levels in normal and diabetic pregnancies. Eur J Obstet Gynecol Reprod Biol 1987;24:195–200 [DOI] [PubMed] [Google Scholar]
- 14. Kurishita M, Nakashima K, Kozu H: Glycosylated haemoglobin of fractionated erythrocytes, glycated albumin, and plasma fructosamine during pregnancy. Am J Obstet Gynecol 1992;167:1372–1378 [DOI] [PubMed] [Google Scholar]
- 15. Abe F, Miyamoto N, Tahara Y, Takahashi J, Shima K: Serum glycated albumin concentrations during pregnancy. Ann Clin Biochem 1993;30:198–200 [DOI] [PubMed] [Google Scholar]