Abstract
Diverticular disease of the colon may be responsible for abdominal symptoms requiring colonoscopy, which may reveal the presence of concomitant polyps. A polyp found during colonoscopy in patients with colonic diverticular disease may be removed by endoscopic polypectomy with electrosurgical snare, a procedure associated with an incidence of perforation of less than 0.05%. The risk of such a complication may be higher in the event of an inverted colonic diverticulum, which may be misinterpreted as a polypoid lesion at colonoscopy. To date, fewer than 20 cases of inverted colonic diverticula, diagnosed at colonoscopy or following air contrast barium enema, have been reported in the literature. The present report describes a 68-year-old woman who underwent a screening colonoscopy, which revealed a voluminous pedunculated polyp that was recognized to be an inverted giant colonic diverticulum before endoscopic polypectomy.
Keywords: Colonic diverticulum, Colonic polyp, Colonoscopy, Polypectomy
Abstract
La maladie diverticulaire du colon peut être responsable de symptômes abdominaux exigeant une coloscopie, laquelle peut révéler la présence de polypes concomitants. Un polype trouvé pendant la coloscopie chez des patients ayant une maladie diverticulaire du côlon peut être extrait par polypectomie endoscopique au moyen d’une excision électrochirurgicale à l’anse, une intervention s’associant à un risque de perforation inférieur à 0,05 %. Le risque d’une telle complication peut être plus élevé en cas de diverticule colique inversé qui, à la coloscopie, peut être confondu avec une lésion polypoïde. Jusqu’à présent, moins de 20 cas de diverticule colique inversé, diagnostiqués au moment de la coloscopie ou après un lavement baryté de contraste, sont déclarés dans les publications. Le présent rapport décrit le cas d’une femme de 68 ans qui a subi une coloscopie de dépistage, laquelle a révélé un polype pédonculé volumineux diagnostiqué comme un diverticule colique géant inversé avant la polypectomie endoscopique.
Diverticular disease of the colon, a condition frequently observed in clinical practice, may be responsible for abdominal symptoms requiring colonoscopy. Colonoscopy may reveal the presence of polyps, often adenomas concomitant with diverticular disease (1–3), which may be removed by endoscopic polypectomy. This procedure has been estimated to account for approximately 50% of the cases of perforation reported during colonoscopy, the incidence of which has been reported to be less than 0.05% (4–6). The risk of such a complication is higher in the event of an inverted colonic diverticulum, which may be misinterpreted as a polypoid lesion at colonoscopy. To date, fewer than 20 cases of inverted colonic diverticula, diagnosed at colonoscopy or following air contrast barium enema, have been reported in the literature (7–14).
The present report describes a patient who underwent a screening colonoscopy, which revealed a voluminous, pedunculated polyp recognized to be an inverted giant colonic diverticulum before endoscopic polypectomy.
CASE PRESENTATION
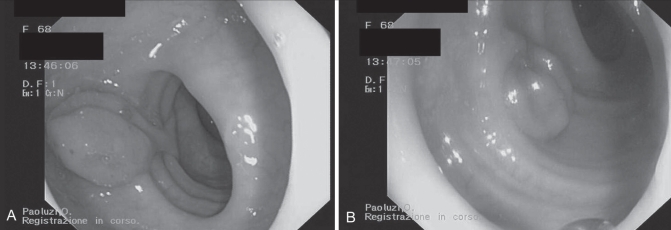
A 68-year-old woman was referred to the Department of Internal Medicine, Tor Vergata University (Rome, Italy), for a gastroenterological consult on account of abdominal pain and constipation. The patient’s symptoms persisted for approximately three months, without other relevant conditions or clinical signs in her medical history for which she would have undergone any previous digestive tract investigations. Routine hematochemical tests, including inflammatory parameters (C-reactive protein and erythrocyte sedimentation rate) as well as complete blood count, were within normal ranges. Following a standard bowel cleansing consisting of gut lavage with 4 L of polyethylene glycol, a full colonoscopy was performed, which revealed a polypoid lesion in the distal sigmoid with a head approximately 2.5 cm in size and a peduncle approximately 3 cm in length. The mucosa covering the head showed hyperemia and mild granularity (Figure 1). Multiple diverticula were also present in the left colon and in the tract where the polypoid lesion was located. Because standard assessments of coagulation and complete blood counts were within the normal ranges, removal of the polypoid lesion by means of endoscopic polypectomy with diathermal coagulation was scheduled. However, when in contact and moved with biopsy forceps, the head of the polyp appeared soft and empty (Figure 2). When delicate pressure was applied, the polypoid lesion appeared reduced in size, as if it was pushed out beyond the colonic wall. Polypectomy was abandoned and three biopsy specimens were collected from the head of the lesion to define its nature. Histology revealed the presence of hyperplastic epithelium and mild inflammatory changes in the normal colonic mucosa – a finding consistent with a diagnosis of inverted diverticulum of the colon.
Figure 1).
Two views (A and B) of a large, inverted diverticulum of the colon resembling a pedunculated polyp
Figure 2).
The lesion moved by biopsy forceps. The neck of the diverticulum resembled a long, thin stalk and the head appeared flat
DISCUSSION
The present report described endoscopic findings with regard to a colonic lesion, first diagnosed as a polyp, possibly an adenoma; however, based on macroscopic features and histological findings, the lesion was subsequently revealed to be an inverted diverticulum of the colon. The relevance of this condition seems to reside in the apparent difficulty in reaching an appropriate diagnosis in clinical practice because, to date, fewer than 20 cases have been reported in the literature (7–14). Of these, six were correctly diagnosed on radiology (11,14,15) and five at colonoscopy (11), while the remaining eight were diagnosed following histological assessment of colonic specimens after surgery in five cases and following endoscopic polypectomy in three. These data have led to speculation that there is a high possibility of missing an inverted colonic diverticulum, or misdiagnosing this condition as a polyp at radiology and colonoscopy. This outcome appears more likely when the lesion is large, such as the one described in the present case (greater than 2 cm in size), and strongly resembles a pedunculated polyp. This latter morphology has previously been observed in only two large (3 cm) inverted colonic diverticulae (10,14), one of which appeared as a pedunculated polyp (10), and is very different from most cases of inverted diverticulum described to date, which were only a few millimetres in size.
Although little data regarding the incidence of complications associated with inverted colonic diverticulum have been reported in the literature, it is tempting to hypothesize that an incorrect diagnosis of this condition, especially when resembling a polyp, may be responsible for severe complications such as perforation following endoscopic polypectomy with electrosurgical snare. Therefore, prompt diagnosis of an inverted colonic diverticulum during colonoscopy appears to be crucial. To more easily define a differential diagnosis between an inverted colonic diverticulum and common true polyps, it may be worthwhile to attempt to induce eversion of the diverticulum by air insufflation, as observed during radiological examination (11) or colonoscopy (7), or by probing the lesion with biopsy forceps and gently pushing it outside the colonic wall, as suggested by Triadafilopoulos (8). These manoeuvres seem to be more successful in cases of a small diverticulum, but may fail in cases of a large inverted colonic diverticulum as, in part, occurred in the present case. In these occurrences, collection of biopsy specimens may reveal a normal mucosa, a finding consistent with a diagnosis of diverticulum. Recognizing that the wall of a diverticulum consists only of mucosa, biopsies should be performed with considerable caution. Indeed, biopsy specimens in the present case were collected without complications, a finding consistent with other reports (7). Colonic perforation following biopsy collection from an inverted colonic diverticulum has been described in only one case (9). Thus, the risk of colonic perforation following biopsy collection from a large, inverted colonic diverticulum appears to be low.
CONCLUSION
The present report highlights the possibility of finding an inverted colonic diverticulum during colonoscopy. This possibility must be considered carefully to reach a correct diagnosis and avoid potentially dangerous procedures such as endoscopic polypectomy.
REFERENCES
- 1.Stefansson T, Ekbom A, Sparen P, Pahlman L. Increased risk of left sided colon cancer in patients with diverticular disease. Gut. 1993;34:499–502. doi: 10.1136/gut.34.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morini S, Hassan C, Zullo A, et al. Diverticular disease as a risk factor for sigmoid colon adenomas. Dig Liver Dis. 2002;34:635–9. doi: 10.1016/s1590-8658(02)80206-7. [DOI] [PubMed] [Google Scholar]
- 3.Kieff BJ, Eckert GJ, Imperiale TF. Is diverticulosis associated with colorectal neoplasia? A cross-sectional colonoscopic study. Am J Gastroenterol. 2004;99:2007–11. doi: 10.1111/j.1572-0241.2004.30332.x. [DOI] [PubMed] [Google Scholar]
- 4.Araghizadeh FY, Timmcke AE, Opelka FG, Hicks TC, Beck DE. Colonoscopic perforations. Dis Colon Rectum. 2001;44:713–6. doi: 10.1007/BF02234572. [DOI] [PubMed] [Google Scholar]
- 5.Korman LY, Overholt BF, Box T, Winker CK. Perforation during colonoscopy in endoscopic ambulatory surgical centers. Gastrointest Endosc. 2003;58:554–7. doi: 10.1067/s0016-5107(03)01890-x. [DOI] [PubMed] [Google Scholar]
- 6.Cobb WS, Heniford BT, Sigmon LB, et al. Colonoscopic perforations: Incidence, management, and outcomes. Am Surg. 2004;70:750–7. [PubMed] [Google Scholar]
- 7.Yusuf SI, Grant C. Inverted colonic diverticulum: A rare finding in a common condition? Gastrointest Endosc. 2000;52:111–5. doi: 10.1067/mge.2000.106539. [DOI] [PubMed] [Google Scholar]
- 8.Triadafilopoulos G. Images in clinical medicine. Inverted colonic diverticulum. N Engl J Med. 1999;341:1508. doi: 10.1056/NEJM199911113412005. [DOI] [PubMed] [Google Scholar]
- 9.Hollander E, David G. Inverted sigmoid diverticulum simulating polyps. Orv Hetil. 1993;134:639–40. [PubMed] [Google Scholar]
- 10.Dumas O, Jouffre C, Desportes R, Etaix JP, Barthelemy C, Audigier JC. Inverted sigmoid diverticulum: A misleading polyp. Gastrointest Endosc. 1991;37:587–8. doi: 10.1016/s0016-5107(91)70848-1. [DOI] [PubMed] [Google Scholar]
- 11.Glick SN. Inverted colonic diverticulum: Air contrast barium enema findings in six cases. Am J Roentgenol. 1991;156:961–4. doi: 10.2214/ajr.156.5.2017960. [DOI] [PubMed] [Google Scholar]
- 12.Ladas SD, Prigouris SP, Pantelidaki C, Raptis A. Endoscopic removal of inverted sigmoid diverticulum – is it a dangerous procedure? Endoscopy. 1989;21:243–4. doi: 10.1055/s-2007-1012960. [DOI] [PubMed] [Google Scholar]
- 13.Shah AN, Mazza BR. The detection of an inverted diverticulum by colonoscopy. Gastrointest Endosc. 1982;28:188–9. doi: 10.1016/s0016-5107(82)73052-4. [DOI] [PubMed] [Google Scholar]
- 14.Freeny PC, Walker JH. Inverted diverticula of the gastrointestinal tract. Gastrointest Radiol. 1979;4:57–9. doi: 10.1007/BF01887497. [DOI] [PubMed] [Google Scholar]
- 15.Posner R, Solomon A. Dilemma of an inverted cecal diverticulum simulating a pedunculated polyp: CT appearance. Abdom Imaging. 1995;20:440–1. doi: 10.1007/BF01213266. [DOI] [PubMed] [Google Scholar]