Abstract
Recent research on the relationship between child health and income in developed countries reveals a positive gradient that is more pronounced for older children, suggesting that the impact of income upon health accumulates. This article examines whether the same is true in a developing country. Using data from the Indonesian Family Life Survey on children aged 0 to 14 years, we find that although low income adversely affects health, its impact does not differ by age. This finding is robust to the use of both subjective and objective health measures, controlling for selective mortality, the use of alternative measures of households’ resources, and the inclusion of indicators of health at birth and parental health. One explanation for the constancy of the health-income relationship that we explore is the dominant role played by acute illness in determining the general health status of children in a developing-country context compared with the more central role played by chronic conditions in developed countries.
That better health is associated with higher income is well established. Recent research by Case, Lubotsky, and Paxson (2002) in the United States and Currie and Stabile (2003) in Canada has further revealed that the impact of income on health is greater for older children, implying that the effect of income on health accumulates as one ages. This means that, not only are poorer children in worse health from birth, but their health falls further behind as they age, with likely adverse consequences for educational attainment and earnings.
A number of mechanisms may underlie the relationship between parental income and child health. Higher household income allows parents to provide better nutrition for their children, to purchase medical care and health insurance, and possibly also to provide access to a safer environment. Children’s health is also likely to be determined at least in part by parental characteristics that are correlated with parental income. These “third factors” could give rise to an association between child health and parental income that is not causal. Such factors include poor genetics and health-related behavior. Case et al. (2002) explored these mechanisms and found no evidence that parental income affects child health through the ability to purchase medical care, nor that the gradient can be explained by either genetics or poor health at birth. They did, however, find that the arrival of chronic health conditions in childhood plays a pivotal role and suggested that higher-income parents may be better able to manage chronic health problems by seeking and adhering to appropriate medical treatment. This point was further pursued by Currie and Stabile (2003). They used panel data to examine whether the child health-income gradient increases with age because children from wealthier households are better able to respond to a given health shock or because they are subject to fewer shocks. The authors found no difference in the long-term impact of health shocks between children from rich and poor households and concluded that the gradient can be attributed to high-income-family children being subject to fewer health shocks.
That these studies are based on developed countries raises the question of whether the effect of poverty on health might also increase with age in developing countries. Given that the marginal product of health is likely to be higher in developing countries compared with developed countries (Strauss and Thomas 1998), the accumulative health effect of income might also be expected to be larger.1 Thus, health may be an important link in intergenerational cycles of poverty. Also, the mechanisms relating income to health may differ between developed and less-developed countries. For example, the ability to purchase better nutrition and better quality medical care may play a greater role in countries where many children go hungry and the quality of basic medical care is much lower. Although clearly important, these issues have been relatively underexplored in developing countries to date.2
This article is the first to investigate explicitly whether the health-income gradient is more pronounced for older children in a developing country. We are able to do so by using the rich set of child health measures in the 2000 wave of the Indonesian Family Life Survey (IFLS3). The IFLS3 collects parents’ (subjective) evaluations of their children’s general health status and a wide array of other health measures, including both nurse assessments of health and anthropometric measures. We examine the gradient for children younger than 15 years.3 The previous literature on child health in developing countries has focused on the determinants of anthropometric measures, such as height-for-age, weight-for-height, and mortality rates. Measures of height, weight, and mortality have been invaluable in assembling robust evidence of a positive association between households’ resources and health outcomes (Strauss and Thomas 1995); however, they provide only limited insight into the functioning of individuals who are not at the low end of the distribution: stunted, wasted, or deceased. Moreover, these measures are unsuitable for an examination of accumulated health effects: height largely reflects nutritional intake in early childhood, after which growth trajectories tend to proceed in parallel; weight largely reflects short-term deficiencies in nutritional intake; and mortality risk is highest among younger cohorts.4 In addition to facilitating an examination of accumulative health effects, an indicator of general health status provides a more encompassing measure of health than anthropometric measures, or even of reports of morbidity or symptoms suffered, and has been found to be a good predictor of subsequent mortality in adults (Idler and Benyamini 1997).5 However, because of its subjectivity, parent-reported health status may suffer from measurement error, and this measurement error is potentially nonrandom (Case and Deaton 2003; O’Donnell, Rosati, and Van Doorslaer 2002; Strauss and Thomas 1998).
Because the IFLS is unusual in its inclusion of a nurse’s ordinal assessment of individuals’ health status in addition to its collection of anthropometric information, we can determine the extent to which biases associated with the subjective nature of parent-reported health are driving our results. The IFLS data also allow us to investigate other important conceptual and measurement issues that may affect the estimated health-income gradients that have not been addressed in the previous literature. For example, because all births and deaths in households are captured by the IFLS panel, we can account for child mortality. We can also explore the robustness of the results to alternative measures of households’ financial resources. In addition to information on contemporaneous income used in the previous studies, the IFLS provides data on household consumption and wealth, which are longer-term indicators of households’ resources.6 The distinction between current income and permanent income is particularly important in a developing-country context. The use of measures that better reflect permanent income should permit more reliable estimates of the relationship between household resources and child health.
The evidence from our investigation confirms that the general health status of children from poor families is compromised by their families’ circumstances. However, in contrast to studies based on developed countries cited above, we find no evidence that this disadvantage is greater among older children. This suggests that the health effects of income do not accumulate with age in this developing-country setting. A possible explanation for this may lie in a difference between developed and developing countries in the nature of illnesses that threaten child health. For example, although chronic conditions have been found to be important determinants of parent-assessed child health in developed countries, we show that acute conditions are important determinants of Indonesian parents’ assessments of their children’s health. Given the prevalence and severity of acute conditions in developing countries, this result is not surprising. Nonetheless, the fact that acute illnesses are less common and less severe among older children, whereas chronic conditions tend to be revealed as children age, provides a potential explanation for why the health-income gradient steepens in developed countries but not in developing countries.
We begin by describing the IFLS data. We then estimate the child health-income gradient. We follow the literature and begin by focusing on the subjective parent-reported health measure. We examine the robustness of our results to controlling for selective mortality and using alternative subjective and objective measures of child health. We then explore the importance of acute conditions in parent-reported child health as an explanation for why the results we obtain for Indonesia differ from those found for the United States and Canada. The final section concludes.
DATA
The IFLS
The IFLS is a panel survey that was conducted in 1993 (IFLS1), 1997 (IFLS2), and 2000 (IFLS3) with a stratified random sample of more than 7,000 households. The sampling scheme stratified on provinces and urban/rural location. Provinces were selected to maximize the representation of the population, to capture the cultural and socioeconomic diversity of Indonesia, and to be cost effective given the size and terrain of the country. The sample includes 321 enumeration areas (EAs) in 13 provinces, with oversampling of urban EAs and EAs in smaller provinces to facilitate urban/rural and Javanese/non-Javanese comparisons. Households were randomly selected within EAs, using a representative sampling frame from the Indonesian Central Bureau of Statistics, which was based on the 1990 census. A household response rate for IFLS1 in excess of 90% was attained. The IFLS has been very successful in tracking households over time, with 92.3% of the original IFLS1 households reinterviewed for IFLS3. For more information on the sample design, see Strauss et al. (2004).
The 13 provinces sampled by the IFLS cover about 83% of the Indonesian population. The 2000 wave contains 11,686 children younger than 15. This article uses the health status data from the third wave and supplements it with data from the earlier waves of the survey.7
Measuring Health
We use both the parent-reported and nurse-assessed measures of health status collected in the IFLS3. Parent-reported child health status is constructed from the question, “In general, how is the child’s health now?” Possible responses are (1) very healthy (10.48%); (2) somewhat healthy (80.47%); (3) somewhat unhealthy (8.93%); and (4) unhealthy (0.11%). Because of the very small number of “unhealthy” responses, we collapse somewhat unhealthy and unhealthy in the analysis that follows.
Each IFLS household was visited by a nurse who measured individuals’ height, weight, and hemoglobin. Nurses were also asked, “How does the health of this person compare, in general, to the health status of other people of the same age and sex?” Possible responses ranged from 1 (much worse) to 9 (very good). Because very few children were ranked as a 1, 2, 3, or 9, we combined categories 8 and 9 and also categories 1, 2, and 3. To make interpretation of the parent-reported and nurse-assessed evaluations consistent, we reversed the scale of the nurse evaluations so that better health status is associated with a smaller number. Table 1 shows the resulting distribution of responses for both the parent-reported and nurse-assessed measures.
Table 1.
Distribution of Child Health Status
| Measure | Number | Percentage | Percentage by Age Category |
|||
|---|---|---|---|---|---|---|
| 0–3 Years | 4–7 Years | 8–11 Years | 12–14 Years | |||
| Parent-Reported Child Health | ||||||
| 1. Very healthy | 1,084 | 10.58 | 9.12 | 9.29 | 11.58 | 13.10 |
| 2. Somewhat healthy | 8,249 | 80.52 | 76.75 | 82.79 | 81.50 | 81.74 |
| 3. Somewhat unhealthy/unhealthy | 912 | 8.90 | 14.13 | 7.92 | 6.91 | 5.17 |
| Totala | 10,245 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| Nurse-Assessed Child Health | ||||||
| 1. Healthier than average | 186 | 1.87 | 1.54 | 2.16 | 2.03 | 1.76 |
| 2 | 3,881 | 39.01 | 36.10 | 40.18 | 39.44 | 41.17 |
| 3 | 2,591 | 26.04 | 27.51 | 23.99 | 25.98 | 26.67 |
| 4 | 2,651 | 26.65 | 26.36 | 26.89 | 27.20 | 26.00 |
| 5 | 505 | 5.08 | 6.13 | 5.45 | 4.63 | 3.63 |
| 6. Less healthy than average | 135 | 1.36 | 2.35 | 1.33 | 0.73 | 0.78 |
| Totala | 9,949 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
Some totals do not sum exactly to 100.00 because of rounding.
Measuring Household Resources
The IFLS’s detailed data on contemporaneous household income, household consumption, and the value of household assets allows us to examine the robustness of the results to different measures of family economic status. Annual household income is calculated as the sum of earnings, asset income, transfers, and other income (which includes pensions, scholarships, insurance payments, and winnings). Annual household consumption is the sum of food and nonfood consumption, both bought and self-produced. This includes a component for imputed rent.8 Household wealth is the sum of the current value of household assets and business assets, including houses, land, livestock, vehicles, household appliances and furniture, savings deposits, receivables and jewelry, crops, heavy equipment, and tools. In the case in which the household owns a share of an asset, the appropriate percentage is applied.
Other Determinants of Child Health
Although the focus of our analysis is on the relationship between child health, household resources, and age, we control for other factors previously found to be important determinants of child health. These factors include household size, gender of child, presence of parents in the household, age of parents, education of parents, the relationship to the child of the respondent to questions about the child,9 the household’s religion, and whether the household lives in a rural or urban setting. Variables used in some of our sensitivity analyses include parental health and birth weight of the child as well as symptoms of acute illness displayed by the child in the four weeks prior to survey. Summary statistics of all variables are found in Appendix Table A1.
RESULTS
The Child Health-Income Gradient
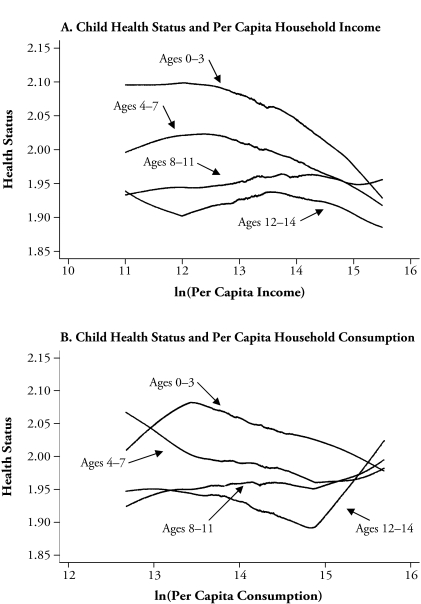
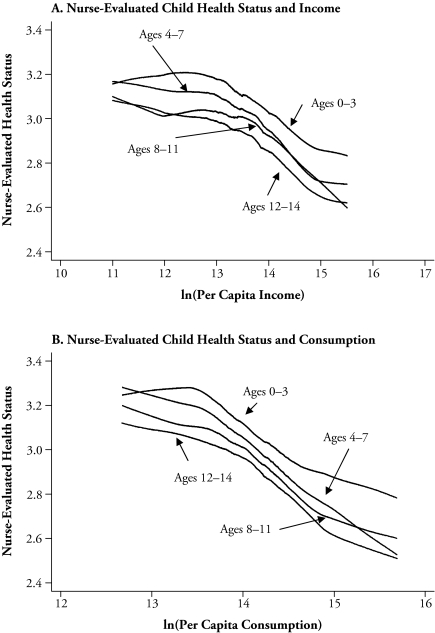
Figure 1 presents nonparametric, locally weighted regressions of parent-reported health status on per capita household income (Panel A), per capita household consumption (Panel B), and per capita household wealth (Panel C), for children up to the age of 14. All three measures of household resources produce similar results. Noting that better health is indicated by a smaller number, the protective effect of household resources is clearly indicated by the negative gradient of the majority of the lines in this figure. For example, the conditional expectation of parent-reported health status is 2.10 among 0- to 3-year-olds at the 10th percentile of the per capita income distribution but is 1.97 for those at the 90th percentile of the income distribution (indicating better health). The general health status of children improves with age in Indonesia. This is in contrast to developed-country results, which show that children’s health declines as they age.10 This is likely attributable to the differing nature of disease in the two sets of countries. Whereas in developed countries, chronic conditions are important determinants of children’s general health status, acute illnesses—such as diarrhea and acute respiratory infections (involving a cough, nasal discharge, and fever)—are the most serious threats to child health and life in developing countries. Filmer and Pritchett (2004) reported that 28% of all deaths in developing countries are due to infections and parasitic diseases among children under 5. Unlike chronic disease, these acute diseases are more prevalent at young ages.11 The implications of the higher prevalence of acute illnesses in developing countries will be discussed in more detail later.
Figure 1.
The Relationship Between Child Health Status and Household Resources
A further feature of the relationship between parent-reported health status and the household resource variables displayed in Figure 1 is that there is no evidence that the health-income gradient is steeper for older age groups. This is in contrast with the U.S. and Canadian studies discussed earlier.12 In fact, especially in the case of per capita income (the measure used in developed country studies), the gradients for Indonesia seem to flatten with age. We next examine whether the health-income relationship is robust to controlling for characteristics of the child, family structure, characteristics of the parents, and geographic location; and whether the differences across age categories are statistically significant.
Parametric Regressions
Table 2 reports the coefficients on the household resource variables from ordered probit models for child health status (1 = very healthy, 2 = somewhat healthy, 3 = somewhat unhealthy or unhealthy) for all children younger than 15, and for separate age groups.13 We estimate separate regressions with income, consumption, and wealth, respectively, as the household resource variable and report z scores based on robust standard errors that allow for correlation between unobservables for children from the same household. In addition to the natural logarithm of the household resource variable, the results in the top panel control for other variables that may affect child health, some of which are likely to be correlated with household income. These variables include household size; the child’s age and gender; whether the child’s parents live in the household, and if so, their ages; the household’s religion (Muslim, Protestant, Catholic, Hindu, or Buddhist); rural residence; and provincial location. We also control for whether the person who assessed the child’s health (the respondent) was the child, child’s mother, child’s father, or another adult household member (the omitted category). These variables are also chosen for comparability with previous studies.
Table 2.
Health Status and Household Resources at Different Ages
| All Ages | Ages 0–3 | Ages 4–7 | Ages 8–11 | Ages 12–14 | |
|---|---|---|---|---|---|
| Controls 1a | |||||
| Log of household income | −0.059 (−4.35) |
−0.104 (−4.65) |
−0.095 (−3.86) |
0.005 (0.20) |
−0.032 (−1.18) |
| Log of household consumption | −0.101 (−3.82) |
−0.16 (−3.59) |
−0.083 (−1.68) |
−0.025 (−0.55) |
−0.149 (−2.68) |
| Log of household wealth | −0.036 (−3.73) |
−0.045 (−2.96) |
−0.041 (−2.26) |
−0.025 (−1.38) |
−0.035 (−1.71) |
| Controls 2b | |||||
| Log of household income | −0.058 (−4.13) |
−0.085 (−3.68) |
−0.103 (−4.10) |
0.002 (0.07) |
−0.035 (−1.25) |
| Mother completed primary school | −0.011 (−0.30) |
−0.195 (−3.08) |
0.093 (1.36) |
0.029 (0.45) |
0.039 (0.54) |
| Log of household consumption | −0.098 (−3.61) |
−0.125 (−2.73) |
−0.09 (−1.83) |
−0.033 (−0.69) |
−0.162 (−2.81) |
| Mother completed primary school | −0.016 (−0.45) |
−0.215 (−3.44) |
0.059 (0.88) |
0.041 (0.69) |
0.069 (0.95) |
| Log of household wealth | −0.035 (−3.50) |
−0.031 (−1.93) |
−0.046 (−2.42) |
−0.030 (−1.61) |
−0.038 (−1.77) |
| Mother completed primary school | −0.014 (−0.40) |
−0.228 (−3.56) |
0.08 (1.16) |
0.06 (0.97) |
0.047 (0.65) |
| N | 10,245 | 2,938 | 2,638 | 2,676 | 1,993 |
Notes: The dependent variable is child health status (1 = very healthy, 2 = somewhat healthy, 3 = unhealthy/very unhealthy). Asymptotic z scores are in parentheses.
Controls 1 includes the natural log of household size; a set of dummy variables for each age in years; gender; the presence of the child’s mother in the household; the presence of the child’s father in the household; the mother’s age interacted with an indicator for mother’s presence; the father’s age interacted with an indicator for father’s presence; indicators for the religion of the head of the household, rural residence, and the province of residence; and indicators for who reported the child’s health status (mother, father, child, or another adult household member).
Controls 2 adds an indicator for mother’s education (at least primary school) to Controls 1.
The first observation that can be drawn from the results in Table 2 is that the previous section’s finding—that the health-income gradient for Indonesian children is not steeper for older age groups—is robust to the inclusion of these controls. The coefficient on household resources is generally statistically significant except for the 8- to 11-year-old age group and, in the specification based on household income, for the 12- to 14-year-old age group. When we test the hypothesis of equality of coefficients on the household resource variable for adjacent age groups, we find no significant difference for the models based on household wealth, suggesting a common gradient across age groups. The model based on consumption also shows no evidence of a steeper gradient for older children. The point estimates decline from ages 0–3 through to ages 8–11 and then increase for the 12–14 age group. However, the coefficient for the 12–14 age group (−0.149) is not significantly different from that for 0- to 3-year-olds (−0.16). For income, we even find some evidence that the health-income gradient is smaller for older children, with a p value for the test statistic comparing the coefficient for the 0- to 3-year-old and 12- to 14-year-old age groups of 0.04.
The top panel of Table 2 does not control for maternal education. Mothers’ education has been the focus of much attention in the developing-country literature on the relationship between socioeconomic status and child health, and has been found to be an important determinant of height, weight, and mortality (Skoufias 1999; Strauss and Thomas 1995; Van der Klaaw and Wang 2004). Indeed, there has been some debate as to whether household income affects health after mothers’ education has been accounted for (Wolfe and Behrman 1982). For example, education may impart health knowledge and confidence to deal with health professionals, and it may be this knowledge and not income per se that has a positive impact on child health. To investigate this, the bottom panel of Table 2 adds to the control variables an indicator for whether the mother has completed primary school.14
We find that the indicator of maternal education is an important determinant of general health status, but only for children younger than 3. This is consistent with the findings of Sahn and Alderman (1997) and Lavy et al. (1996). Accounting for mothers’ education reduces the impact of household resources on child health for this youngest age group, suggesting an indirect effect of education operating through household income, but does not alter the findings regarding the constancy of the gradient with respect to age.15
ROBUSTNESS CHECKS
Issues in the Measurement of Child Health
A potential explanation for finding no significant increase in the health-income gradient for older children is that measurement issues are obscuring our ability to detect such an increase. In this section, we investigate whether our finding of a constant health income gradient across age groups is robust to accounting for (1) differences in how parents and children report on child health, (2) sample selection bias arising from high infant mortality, and (3) measurement error in parent-reported child health.
Child-Reported Versus Adult-Reported Child Health
The IFLS allows children to report on their own health status if they are between 11 and 14 years of age. The results presented in Table 2 show that none of the coefficients on the household resource variables reach statistical significance for the 8- to 11-year-old age group. Self-reporting of health by some children may have led to these coefficients being imprecisely estimated. Child reports may reflect a different perspective on health than adult reports. It may also be that children, especially those at the younger end of the self-reporting spectrum, are not well placed to assess their own health, producing a noisier measure of health and diminishing our ability to identify a steepening gradient. We investigate this issue by excluding all child-reported health observations from our sample.16 The top panel in Table 3 contains results based on adult reporting only.17 Because most children in the 12–14 age group reported for themselves, the sample size for this group is greatly reduced (N = 486). Excluding the child-reported observations results in most of the coefficients on the household resources variables becoming more negative for the upper two age categories. However, our finding with regard to the gradient being constant across age groups is unaffected. Subsequent reported results continue to restrict the sample to adult-reported child health.
Table 3.
Robustness to Issues in the Measurement of Child Health Status
| All Ages | Ages 0–3 | Ages 4–7 | Ages 8–11 | Ages 12–14 | |
|---|---|---|---|---|---|
| Parent-Reported Health Status Only | |||||
| Log of household incomea | −0.064 (−4.35) [0.011] |
−0.085 (−3.68) [0.013] |
−0.094 (−3.84) [0.015] |
−0.018 (−0.68) [0.003] |
−0.058 (−1.00) [0.010] |
| Log of household consumption | −0.098 (−3.33) |
−0.125 (−2.73) |
−0.084 (−1.69) |
−0.066 (−1.25) |
−0.249 (−2.42) |
| Log of household wealth | −0.033 (−3.17) |
−0.031 (−1.93) |
−0.04 (−2.16) |
−0.038 (−1.95) |
−0.032 (−0.74) |
| N | 8,111 | 2,938 | 2,624 | 2,067 | 486 |
| Accounting for Child Mortality (parent-reported only) | |||||
| Log of household income | −0.063 (−4.67) |
−0.077 (−3.44) |
−0.100 (−4.26) |
−0.051 (−2.10) |
0.012 (0.27) |
| Log of household consumption | −0.109 (−3.87) |
−0.109 (−2.47) |
−0.125 (−2.65) |
−0.110 (−2.33) |
−0.172 (−2.12) |
| Log of household wealth | −0.03 (−3.20) |
−0.034 (−2.17) |
−0.035 (−2.11) |
−0.048 (−2.86) |
0.002 (0.05) |
| N | 8,695 | 3,068 | 2,741 | 2,240 | 654 |
| Nurse-Assessed Health Status | |||||
| Log of household income | −0.077 (−5.17) |
−0.069 (−3.33) |
−0.096 (−4.17) |
−0.056 (−2.18) |
−0.086 (−3.26) |
| Log of household consumption | −0.148 (−5.25) |
−0.112 (−2.70) |
−0.190 (−4.28) |
−0.127 (−2.97) |
−0.198 (−3.88) |
| Log of household wealth | −0.065 (−6.10) |
−0.066 (−4.37) |
−0.07 (−4.25) |
−0.059 (−3.47) |
−0.067 (−3.35) |
| N | 9,949 | 2,853 | 2,551 | 2,614 | 1,931 |
Notes: The dependent variable is child health status (1 = very healthy, 2 = somewhat healthy, 3 = unhealthy/very unhealthy). Asymptotic z scores are in parentheses. The models in the first two panels include the explanatory variables in “Controls 1” in Table 2. In addition, the model for ages 0–3 includes an indicator for mother’s education. An interaction term between mother’s education and the child being aged 0–3 is included in the model for children of all ages. Models in the last panel include the explanatory variables in “Controls 2” in Table 2, with the exception of the set of indicators for who reported the child’s health status.
Numbers in square brackets show the change in the probability of reporting very healthy (relative to somewhat healthy or very unhealthy) associated with a 1-log-point increase in household income.
In terms of the magnitude of the effect of income on child health, the estimates in the top panel of Table 3 imply that a doubling of household income is associated with an average increase in the probability of reporting being very healthy by 1.1 percentage points, or 10.4%.
Mortality
A second potential explanation for the lack of evidence of a steepening of the health-income gradient for older age groups is selective mortality—that is, the fact that mortality rates are higher among poor children than rich children. The UN’s World Development Indicators (World Bank 2003) estimate Indonesia’s under-5 child mortality rate to be 45 per 1,000 children in 1999. Among the cohort of children from IFLS households who were 5 years old in 2000 (or would have been), 4.1% died. Child mortality was 6.0% for households in the lowest quintile of the income distribution while only 2.9% for families in the highest-income quintile. This selection bias artificially flattens the health-income gradient because it raises the average health of surviving children from poor families relative to those from richer families. Further, infant and child mortality will flatten the health-income gradient more for older cohorts because a cohort’s mortality rate increases with age. This effect is exacerbated if mortality rates have declined over time. There is some evidence of this in the IFLS3 data, with infant mortality at around 5.5 per 100 live births for the cohort born in 1986 compared with about 3.5 per 100 live births in more recent years.
Because a complete history of births and deaths in households is recorded by the IFLS panel, we are able to address the issue of child mortality in our analysis. We do so by adding in those who died and attributing to them (1) the age they would have been in 2000 had they survived, and (2) the lowest health status. This approach is biased in favor of finding an increasing gradient because children who died as infants 10 years ago, for example, are now being treated as 10-year-olds with poor health (whereas if they had survived, their health may have improved). Ignoring the generally insignificant estimates for the 12- to 14-year-old age group, we find that 7 of the 12 estimates in the second panel of Table 3 are now greater in absolute magnitude and that all but two of the z scores are now higher. This indicates a stronger relationship between household resources and health after mortality is accounted for. However, testing for the equality of the impact of household resources across adjacent age groups again revealed no significant differences, indicating that the health-income profile remains flat across age groups. Thus, selective mortality does not account for the constancy of the gradient across age groups.18
Parent-Reported Versus Nurse-Assessed and Objective Measures of Child Health
As mentioned earlier, parent-reported health status may suffer from nonrandom measurement error. For example, respondents from higher-income households may be more critical of their child’s health because of greater exposure to health services.19 This would bias our coefficients on the household resource variables toward zero (they will underpredict the effect of resources on health), but it is not clear how this would affect the differences in coefficients across age categories.20 To investigate the extent to which our results reflect parental reporting bias, we make use of the nurse-assessed health measure collected as part of the IFLS.21
Each household in the IFLS was visited by a nurse who conducted physical assessments, and who, after a brief discussion with the respondent, gave a health rating. The nurse’s visit was separate from the household survey interviewer’s visit (within a day or two of the survey team), and so the nurse was not aware of the parent-reported assessments of child health provided to the interviewers. The nurse ratings are, thus, largely independent from the parental reports. This is confirmed by the low correlation between the two measures of .08.22
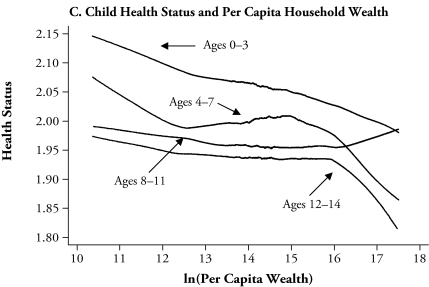
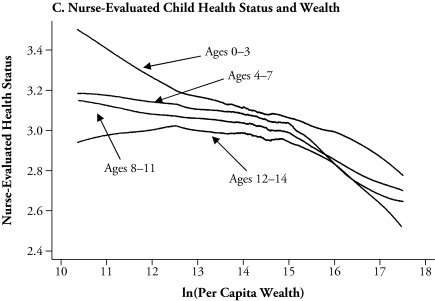
Figure 2 shows the results of nonparametric regressions of nurse-evaluated health on the three alternative measures of household resources. As with parent-assessed health, nurse-assessed health is shown to improve with greater household resources, and there is no evidence of the gradients steepening with age. Ordered probit models of the relationship between nurse-assessed health and household resources were run separately for each of the three measures of household resources, and the results are reported in the bottom panel of Table 3. The coefficients on the household resource variables are significant and remarkably constant across age groups (e.g., using wealth as the measure of household resources yields coefficients of −0.066 for 0- to 3-year-olds, −0.07 for 4- to 7-year-olds, −0.059 for 8- to 11-year-olds, and −0.067 for 12- to 14-year-olds). Testing for the equality of the impact of household resources across adjacent age groups revealed no significant differences, and this was the case for income, consumption, and wealth.
Figure 2.
The Relationship Between Nurse-Evaluated Child Health Status and Household Resources
As a further check on the existence of an increasing gradient, we examined the relationship between health as measured by standardized height-for-age, weight-for-height, and hemoglobin levels, as well as household resources.23 Iron-deficiency anemia (as indicated by low hemoglobin levels) is a serious nutritional problem in Indonesia and has detrimental effects on energy levels, intellectual development of children, and resistance to disease. The results in Table 4 confirm that, on average, children from wealthier families are taller than children from poorer families and have higher hemoglobin counts for the 0- to 3-year-old and the 4- to 7-year-old age groups. There is no evidence, however, that household resources have a greater impact on the hemoglobin levels or standardized height of older children. The coefficients on household income in the standardized height regressions are slightly larger for older children, but the differences across age groups are not statistically significant. Consistent with Lavy et al. (1996), we find no evidence of a significant relationship between standardized weight-for-height and household resources.24
Table 4.
Objective Health Measures: Coefficients on Household Income (t statistics in parentheses)
| Dependent Variable | All Ages | Ages 0–3 | Ages 4–7 | Ages 8–11 | Ages 12–14 |
|---|---|---|---|---|---|
| Standardized Height-for-Age | 0.094 (5.60) |
0.086 (2.45) |
0.081 (3.07) |
0.096 (4.31) |
0.116 (4.32) |
| Standardized Weight-for-Height | −0.021 (−1.13) |
−0.010 (−0.36) |
−0.012 (−0.46) |
−0.073 (−2.14) |
NA |
| Hemoglobin Levels | 0.035 (2.40) |
0.075 (2.37) |
0.050 (2.05) |
0.003 (0.10) |
0.031 (1.09) |
Notes: The NCHS/WHO reference data for standardizing weight-for-height are available only up to age 10. The regressions control for all the variables in “Controls 2” in Table 2. In addition, the standardized height regression controls for the height of the mother and father (if present) and the standardized weight regression controls for the body mass index (BMI) of the parents.
UNDERSTANDING THE GRADIENT
The preceding results provide evidence that children who belong to households with more economic resources are in better health and that this relationship is unchanging across age groups. As noted by Case et al. (2002), these associations do not establish a causal relationship running from household income to child health. For example, the relationship between income and child health may reflect unobserved “third factors,” such as a lasting effect of poor health at birth or the inheritance of poor health from parents, that are positively associated with low household income. We next investigate whether these factors account for the relationship between household resources and child health.25
Health at Birth
The relationship between health and income may be attributable to children from poorer families being born with poor health. Household income in childhood may thus only appear to be a determinant of child health because of serial correlation in income. We investigate this by controlling for poor health at birth using an indicator for low birth weight, defined as a weight of less than 2,500 grams (7.6% of our sample). Low-birth-weight babies are more likely to have serious health problems, including respiratory distress syndrome, bleeding in the brain, and heart and intestinal problems. Information on birth weight is available for only about one-half of our sample, so there are insufficient observations to estimate models for each age group. For this reason, we follow Case et al. (2002) and pool observations across age groups but allow income to have a differential impact by age by including an interaction term between income and (a continuous measure of) age in the regression models. Missing information on birth weight, however, is more common for children from poorer households, and this is likely to lead to an underestimate of the impact of birth weight on child health. For this reason, the results should be treated with caution.
The top panel of Table 5 contains the ordered probit results. They show that current parent-reported child health is not significantly related to low birth weight. This result is not sensitive to differences in household income or age of the child. Household resources (whether measured by income, consumption, or wealth) remain a significant determinant of health status, the effect of which does not vary with age.26
Table 5.
Robustness to Possible Third Factors: Birth Weight and Parents’ Health Status
| Controlling for Birth Weight (all ages) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Log of Household Income | −0.100 (−3.45) |
−0.100 (−3.44) |
−0.099 (−3.39) |
−0.100 (−3.45) |
−0.104 (−3.46) |
| Age | −0.111 (−1.44) |
−0.108 (−1.40) |
−0.108 (−1.41) |
−0.117 (−1.49) |
−0.126 (−1.57) |
| Income × Age | 0.005 (0.97) |
0.005 (0.96) |
0.005 (0.96) |
0.005 (1.05) |
0.006 (1.14) |
| Low Birth Weight | 0.129 (1.04) |
0.198 (0.21) |
0.127 (1.03) |
−0.962 (−0.60) |
|
| Low Birth Weight × Age | −0.027 (−1.19) |
−0.027 (−1.19) |
0.065 (0.43) |
0.224 (0.83) |
|
| Low Birth Weight × Income | −0.004 (−0.08) |
0.070 (0.68) |
|||
| Low Birth Weight × Age × Income | −0.006 (−0.60) |
−0.016 (−0.93) |
|||
| N | 4,862 | 4,862 | 4,862 | 4,862 | 4,862 |
| Controlling for Parent’s Health Status (parent-reported health status only) | All Ages | Ages 0–3 | Ages 4–7 | Ages 8–11 | Ages 12–14 |
| Log of Household Income | −0.054 (−3.74) |
−0.069 (−3.00) |
−0.087 (−3.60) |
−0.011 (−0.43) |
−0.054 (−0.90) |
| Mother: Very Healthy | −0.791 (−8.76) |
−0.933 (−7.12) |
−0.654 (−4.28) |
−0.769 (−4.65) |
−0.832 (−2.12) |
| Mother: Somewhat Healthy | −0.150 (−2.60) |
−0.271 (−3.22) |
−0.077 (−0.75) |
−0.064 (−0.57) |
−0.26 (−1.02) |
| Father: Very healthy | −0.669 (−7.02) |
−0.674 (−5.11) |
−0.747 (−4.61) |
−0.531 (−2.91) |
−0.935 (−2.72) |
| Father: Somewhat Healthy | −0.219 (−3.67) |
−0.201 (−2.15) |
−0.272 (−2.69) |
−0.238 (−2.17) |
−0.196 (−1.04) |
| N | 8,351 | 3,032 | 2,690 | 2,128 | 505 |
Notes: The dependent variable is child health status (1 = very healthy, 2 = somewhat healthy, 3 = unhealthy/very unhealthy). Asymptotic z scores are in parentheses. The models controlling for birth weight include the explanatory variables in “Controls 1” in Table 2, with the exception of the set of indicators for age. The models controlling for parent’s health status include the same controls as in the first two panels of Table 3.
Parents’ Health as a Determinant of Children’s Health
Parents’ health may be correlated with their children’s health through several avenues. For example, children may inherit their parents’ genetic predisposition for illness, or parents and children may be exposed to common, yet unobserved, environmental risk factors. Parents in poor health are likely to have reduced income-producing capacity, and failure to account for parents’ health in the preceding models could result in attributing the effect of these omitted variables to household income. Although less than a perfect solution, we follow Case et al. (2002) and address this issue by including indicators for the parents’ health in the models for children’s parent-reported health.27 The results from doing so are reported in the second panel of Table 5. They show that although the impact of parental health on the health status of the child is large and significant (e.g., if a child has a mother who is very healthy, his or her chance of also being very healthy increases by about 19 percentage points), the coefficients on income are largely unaffected by the inclusion of parental health.28 Table 5 reports results in which household income is used as the measure of household resources. The results for specifications that measure household resources using consumption or wealth are similar. From this, we conclude that the relationship between child health and income does not solely reflect unmeasured genetic or environmental factors that affect parental health, and hence, family income.
In summary, we find that child health is a function of the economic resources at a household’s command but that the strength of this relationship does not change with the age of the child. The finding of a constant gradient is robust to different measures of household resources; controls for selective mortality; and the inclusion of the possible confounding third factors, birth weight, and parental health. The parent-assessed health measure, the nurse-assessed measure, and the objective measures all generate the same result.
WHY IS THE INCOME-HEALTH GRADIENT CONSTANT ACROSS AGE GROUPS?
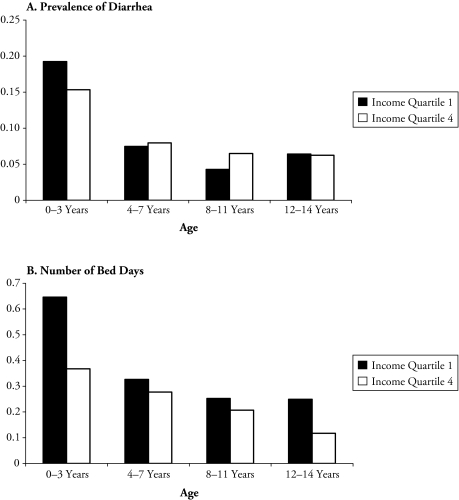
As we mention earlier, in developing countries, acute illness is often life threatening. Consequently, measures of general health status may place a greater weight on these acute conditions than is the case in a developed country. Although more common among children from poorer households, acute illnesses are—because of their short-term nature—less likely than chronic conditions to have an accumulative negative health effect.29 Indeed, cumulative exposure to pathogens may even build resistance to acute conditions (Strauss and Thomas 1995).30 Moreover, in contrast to chronic conditions, whose prevalence tends to increase with age, acute conditions are less prevalent and less severe at older ages. This explanation for why the health-income gradient is not steeper for older children in Indonesia is supported by Figure 3. It shows that among the youngest children, those from the poorest households are much more likely to report having diarrhea and spending more days in bed because of illness in the four weeks prior to survey; however, the protective effect of income diminishes with age. Therefore, a potential explanation for finding that the income health gradient is constant across age groups in a developing country may be the greater importance of acute conditions in children’s general health status.
Figure 3.
Prevalence of Diarrhea and Number of Days Spent in Bed, by Age and Income Quartile
The IFLS data allow a closer investigation of this issue. We estimate ordered probit models of parent-reported child health status as a function of symptoms of acute illness suffered in the four weeks prior to the survey. These symptoms include headache, runny nose, cough, difficulty breathing, fever, nausea, diarrhea, skin infection, eye infection, toothache, earache, worms, injury, and “other” symptoms. We also include the number of days the child spent in bed because of illness, the number of days of missed activity because of illness in the four weeks prior to the survey, and the objective measures of health: standardized height-for-age, standardized weight-for-height, and hemoglobin levels.
Table 6 presents the findings. As hypothesized, the symptoms data (which mostly reflect acute conditions) are important correlates of parents’ assessments, as are the number of days of missed activity. The physical measures of health are also statistically significant, although of lesser importance. The pseudo-R2 is .083 when all covariates are included. It drops to only .007 when just the objective measures are included. Although parent-reported health status is found to be correlated with acute morbidities, one would also expect that if a child had a chronic disease (such as epilepsy), this, too, would be reflected in the parent reports. Unfortunately, the IFLS does not provide information on these conditions, so we cannot empirically verify the role of chronic conditions in parent reports of child health.31 Overall, Table 6 demonstrates that parent assessments of their children’s health status is correlated with acute illnesses, which, given the potentially serious consequences of these conditions in developing countries, seems appropriate. The strength of the correlation between acute conditions and health status suggests that the dominant role of acute health conditions provides an explanation for why the health-income gradient does not become steeper with age in Indonesia.32
Table 6.
Correlates of Parent-Reported Health Status
| Parent-Reported Health |
||
|---|---|---|
| Coefficient | z Score | |
| Days of Missed Activity Due to Illness | 0.078 | 4.12 |
| Number of Days in Bed Due to Illness | 0.018 | 0.75 |
| Symptom | ||
| Headache | 0.089 | 1.89 |
| Runny nose | 0.214 | 4.66 |
| Cough | 0.034 | 0.73 |
| Difficulty breathing | 0.394 | 3.67 |
| Fever | 0.152 | 3.23 |
| Nausea | 0.151 | 1.93 |
| Diarrhea | 0.091 | 1.39 |
| Skin infection | 0.157 | 2.52 |
| Eye infection | 0.128 | 1.18 |
| Toothache | −0.012 | −0.19 |
| Earache | 0.133 | 1.69 |
| Worms | 0.476 | 1.22 |
| Injury | 0.735 | 2.11 |
| Other | 0.576 | 3.12 |
| Standardized Height-for-Age | −0.034 | −2.12 |
| Standardized Weight-for-Height | −0.057 | −3.27 |
| Hemoglobin Levels | −0.018 | −1.40 |
| Pseudo-R2 | .083 | |
| N | 5,616 | |
Notes: The dependent variable is child health status (1 = very healthy, 2 = somewhat healthy, 3 = unhealthy/very unhealthy). The sample size is smaller than in previous tables because standardized height and weight are available only for children 10 years old and younger.
CONCLUSIONS
Our investigation confirms that, as with developed countries, the general health status of children from poor families in developing countries is compromised by their families’ circumstances. However, unlike studies based on U.S. and Canadian data, we find no evidence that this disadvantage is greater for older children in Indonesia. Moreover, this finding is robust to accounting for selective mortality and the inclusion of indicators of health at birth and parental health; it is also robust to alternative measures of child health, including the nurse-assessed measure of general health status and the objective measures of height-for-age, weight-for-height, and hemoglobin levels. This raises the question of why household resources do not have a more pronounced effect on older children’s general health status in a developing-country context. We argue that this is because in the developing world, acute illnesses—such as diarrhea and fever—are a major cause of ill health. Therefore, despite the shorter-term nature of acute illnesses, they are significantly correlated with parental assessments of children’s health. These illnesses, unlike chronic health conditions that are a more important determinant of children’s general health status in developed countries, do not have a negative accumulating effect and are less prevalent and less severe at older ages.
Although the health effects of living in a poorer household in a developing country are not greater for older children, we still find strong evidence that living in a poorer household has a robust negative effect on health. Poor health can negatively affect children’s academic achievements. Lower academic achievement lowers potential labor market earnings. Hence, health remains an important pathway by which poverty can be transmitted across generations.
Acknowledgments
The authors gratefully acknowledge financial support for this research from the Australian Research Council.
Appendix Table A1.
Summary Statistics
| Variable | Number of Observations | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Parent-Reported Health Status | 10,245 | 1.983 | 0.441 | 1 | 3 |
| Nurse-Assessed Health Status | 9,937 | 2.982 | 1.028 | 1 | 6 |
| Log of Household Income | 10,245 | 15.396 | 1.152 | 6.81 | 20.91 |
| Log of Household Wealth | 10,245 | 15.915 | 0.625 | 14.13 | 17.70 |
| Log of Household Consumption | 10,245 | 16.548 | 1.595 | 9.21 | 21.23 |
| Log of Household Size | 10,245 | 1.787 | 0.402 | 0.69 | 3.61 |
| Age | 10,245 | 6.822 | 4.410 | 0 | 14 |
| Female | 10,245 | 0.490 | 0.500 | 0 | 1 |
| Mother Present | 10,245 | 0.937 | 0.243 | 0 | 1 |
| Father Present | 10,245 | 0.875 | 0.331 | 0 | 1 |
| Age of Mother | 10,245 | 31.422 | 10.998 | 0 | 67 |
| Age of Father | 10,245 | 33.762 | 15.250 | 0 | 83 |
| Respondent to Questions About Child Health | |||||
| Father | 10,245 | 0.152 | 0.359 | 0 | 1 |
| Mother | 10,245 | 0.583 | 0.493 | 0 | 1 |
| Child | 10,245 | 0.208 | 0.406 | 0 | 1 |
| Religion | |||||
| Protestant | 10,245 | 0.047 | 0.212 | 0 | 1 |
| Catholic | 10,245 | 0.016 | 0.125 | 0 | 1 |
| Hindu | 10,245 | 0.045 | 0.207 | 0 | 1 |
| Buddhist | 10,245 | 0.003 | 0.056 | 0 | 1 |
| Rural | 10,245 | 0.572 | 0.495 | 0 | 1 |
| Low Birth Weight | 4,949 | 0.075 | 0.264 | 0 | 1 |
| Mother’s Highest Level of Education | |||||
| Primary school | 10,245 | 0.475 | 0.499 | 0 | 1 |
| Lower secondary school | 10,245 | 0.147 | 0.354 | 0 | 1 |
| Upper secondary school | 10,245 | 0.171 | 0.376 | 0 | 1 |
| Tertiary | 10,245 | 0.049 | 0.216 | 0 | 1 |
| Father’s Highest Level of Education | |||||
| Primary school | 10,240 | 0.408 | 0.491 | 0 | 1 |
| Lower secondary school | 10,240 | 0.137 | 0.343 | 0 | 1 |
| Upper secondary school | 10,240 | 0.196 | 0.397 | 0 | 1 |
| Tertiary | 10,240 | 0.077 | 0.266 | 0 | 1 |
| Days of Missed Activity Due to Illness | 10,244 | 1.171 | 2.699 | 0 | 31 |
| Number of Days in Bed Due to Illness | 10,242 | 0.324 | 1.358 | 0 | 30 |
| Symptom | |||||
| Headache | 10,245 | 0.292 | 0.455 | 0 | 1 |
| Runny nose | 10,245 | 0.505 | 0.500 | 0 | 1 |
| Cough | 10,245 | 0.379 | 0.485 | 0 | 1 |
| Difficulty breathing | 10,245 | 0.039 | 0.193 | 0 | 1 |
| Fever | 10,245 | 0.343 | 0.475 | 0 | 1 |
| Nausea | 10,245 | 0.078 | 0.268 | 0 | 1 |
| Diarrhea | 10,245 | 0.098 | 0.297 | 0 | 1 |
| Skin infection | 10,245 | 0.105 | 0.306 | 0 | 1 |
| Eye infection | 10,245 | 0.045 | 0.206 | 0 | 1 |
| Toothache | 10,245 | 0.102 | 0.303 | 0 | 1 |
| Earache | 10,245 | 0.001 | 0.028 | 0 | 1 |
| Worms | 10,245 | 0.001 | 0.031 | 0 | 1 |
| Injury | 10,245 | 0.001 | 0.028 | 0 | 1 |
| Other | 10,245 | 0.014 | 0.117 | 0 | 1 |
| Standardized Height-for-Age | 6,183 | −1.542 | 1.303 | −6.47 | 5.13 |
| Standardized Weight-for-Height | 6,183 | −0.523 | 1.148 | −3.82 | 5.10 |
| Hemoglobin Levels | 8,584 | 11.758 | 1.499 | 3 | 29.10 |
| Mother’s Self-reported Health Status | |||||
| Very healthy | 10,167 | 0.071 | 0.257 | 0 | 1 |
| Somewhat healthy | 10,167 | 0.751 | 0.432 | 0 | 1 |
| Father’s Self-reported Health Status | |||||
| Very healthy | 10,148 | 0.068 | 0.252 | 0 | 1 |
| Somewhat healthy | 10,148 | 0.715 | 0.451 | 0 | 1 |
Footnotes
Note that although the literature refers to the “accumulative” effect of income on health, the process may actually be a combination of development and measurement, with income effects simply being revealed in later development when certain capabilities are supposed to emerge and fail to do so.
One might also expect the labor market consequences of the relative decline in health of poor children to be greater in developing countries because of the greater reliance on physical labor (Strauss and Thomas 1998).
Currie and Stabile (2003) used data on Canadian children younger than 12 years. Case et al. (2002) used three data sets on American children younger than 18, 17, and 13 years. Focusing on children under age 15 also limits the potential endogeneity of household income because most children under age 15 in Indonesia do not work.
Low height-for-age (stunting) generally occurs in the first three years of life, after which the child’s body, through reduced growth, has “adjusted” to low nutrient intake and needs fewer nutrients.
Idler and Benyamini (1997) reviewed studies that link adult self-reported general health status to subsequent mortality. We are unaware of any studies that have done this for child general-health status. However, the IFLS allows us to examine the predictive power of children being in poor health in 1997 (IFLS2) on mortality in the next three years (IFLS3). Such an examination reveals that being in poor health or being very unhealthy significantly increases the probability of death in the next three years (relative to being very healthy). Results are available from the authors upon request.
Studies that have used general health status indicators for developing countries, albeit in different contexts to that proposed here, include Kassouf, McKee, and Mossialos (2001) and Diaz (2002) for Brazil; Liu and Zhang (2004) for China; Lavy, Palumbo, and Stern (1995) for Jamaica; and Case (2001) for South Africa. Self-reported morbidity suffers from the same reporting biases as general health status, although possibly more serious. It is not uncommon for high-income individuals to report greater morbidity than those that are less well off. See Cameron (2001) for an example in the context of Indonesia.
Household consumption is commonly used as a measure of households’ permanent income. Currie and Stabile (2003) used the average of three years of household income. Case et al. (2002) also used average income to examine the effect of permanent versus current income and concluded that children’s health status is most closely associated with permanent income.
IFLS3 was a collaborative effort of RAND and the Center for Population and Policy Studies (CPPS) of the University of Gadjah Mada. Funding for IFLS3 was provided by the National Institute on Aging (NIA) and the National Institute for Child Health and Human Development (NICHD). The parent-reported and nurse-assessed health status questions were not asked in the first wave. Nurse-assessed health data collected in the second wave have not been publicly released.
For those households that do not report the value of their home, we calculate predicted values from a hedonic housing model. Similarly, for those households that own houses and did not report imputed rent or whose imputed rent reports were outliers, we predicted rent from the value of the house and district of residence.
The respondent is most often a parent (72% of cases). Children older than 10 were allowed to report their own health if they wished (21%). In the remaining cases, when parents were not household members or were not available, the respondent could be another household member, typically an aunt or uncle, a grandparent, or a sibling.
We also explored the relationship between self-reported health and income for adults and found that self-reported health starts to decrease beginning at age 15. We also found little relationship between self-reported health and income for all but the oldest category (age 65 and older) for adults. These results are not reported here but are available from the authors upon request. We limit our attention to children under the age of 15 because household income becomes endogenous after children start to work. Only a small percentage of Indonesian children under the age of 15 work, and their income does not constitute a large percentage of household income.
Cebu Study Team (1992) found that the incidence of diarrhea peaks at 9.5 months of age in the Philippines and that febrile respiratory infection also rises after birth, peaks, and then decreases. Strauss and Thomas (1998:767) noted that the difference in incidence and nature of disease in developing countries tends to “tilt the age distribution of ill health to infants and preschool children.”
Currie, Shields, and Wheatley Price (2007) found that the health-income gradient does not increase with age in the United Kingdom. They attribute this to the existence of the United Kingdom’s National Health Service.
This is the most flexible formulation and allows all control variables to affect child health differently at different ages. The results from the more restrictive formulation, in which we interact age with the resource variable, produce similar results.
We originally included a full set of indicators for mothers’ and fathers’ education. The set of indicators for fathers’ education were individually and jointly insignificant. The effect of mothers’ education above primary level did not significantly differ from that of primary level.
In disentangling nature and nurture effects of parents’ education on the schooling of their children, Plug and Vijverberg (2003) attributed about one-half of the impact of parents’ income to parental ability and education.
The characteristics of youth health may differ from that of younger children. For example, drugs, alcohol, risky sex, and other factors may begin to play a role in adolescence. This is, however, less often the case in a country like Indonesia than in developed countries. For example, the Indonesian National Household Health Survey estimates that only 5% (0.6%) of males (females) aged 15–24 drink any alcohol. Data for children younger than 14 are not available but would be expected to be considerably lower. For more information on the key features of youth health, see World Bank (2007).
These models include the same control variables as does the top panel of Table 1. In addition, mother’s education is included in the model for 0- to 3-year-olds, and an interaction term between mother’s education and the child being 0–3 years of age is included in the model for children of all ages. Unless otherwise noted, these controls are included in all subsequent regressions.
It is noteworthy that accounting for mortality did not produce the expected larger estimates on income and consumption for the 0- to 3-year-old age group. For this age group, accounting for mortality produced a larger estimated impact of mother’s education on child health.
Dow et al. (1997) provided some experimental evidence in line with this in the context of Indonesia.
Bago d’Uva et al. (2006) did find evidence of heterogeneity in reporting of health by socioeconomic and demographic characteristics for Indonesia, China, and India, but concluded that the size of the reporting bias was not large. Lindeboom and Van Doorslaer (2004) found no evidence of differential reporting by income using Canadian data but did find some evidence that reporting differs by age, with those aged 20–35 tending to report lower values of health status (conditional on an objective measure of health) than those aged 35–70.
Whether nurse-assessed or parent-reported health is likely to be a better indicator of general health status is a matter of debate. It may be argued that parents are better placed to rank the overall health of their children because they have a greater knowledge of the child’s health history and current functioning. Nurses, however, probably have greater knowledge of what is “average” health status and do collect the objective health indicators—including height, weight, and hemoglobin levels—before giving their overall assessment. At a practical level, nurse-assessed health has the advantage of providing a larger sample size for the analysis of the 12- to 14-year-old age group.
Case et al. (2002) reported a correlation coefficient of .05 between parent- and doctor-assessed child health for the National Health and Nutrition Examination Survey data they used in their analysis.
We standardized by using the NCHS/WHO reference data. Note that the weight-for-height reference data were available only for children aged 10 years and younger.
This is true regardless of whether we included parents’ BMI as an explanatory variable. We also examined the relationship between the other household resource measures and these objective measures of health. They also showed no evidence of an increasing gradient.
Another potential explanation for the association between poor child health and low income is that mothers of less-healthy children reduce their labor supply and thus have lower family income. To investigate the empirical support for this explanation, we exploited the panel nature of the IFLS and examined the impact of having a child in poor health in 1997 on mother’s employment status, hours worked per week, and weeks worked per year reported in the 2000 wave of the survey. We found that having a child in poor health in 1997 had no significant impact on maternal labor supply (controlling for household size, father’s presence, age and educational attainment of each parent, the religion of the head of household, province of residence, and an indicator for living in a rural area). This finding suggests that the relationship between income and child health is not attributable to the effect of having a child in poor health on family income. For the sake of brevity, these results are not reported here but are available from the authors upon request.
Case et al. (2002) found that poor health at birth has a large adverse effect on children’s current health, particularly at low income levels; they also found that although the effect of poor health at birth on current health dissipates with age, improvements with age are slower for poor children. Currie and Stabile (2003) found a negative effect only of very low birth weight (less than 1,500 grams) on child health. This is also true in our sample, but the impact is estimated from a very small number of observations and does not affect the coefficients on the household resource variables. Sahn and Alderman (1997) found that low birth weight has a negative effect on subsequent height in Mozambique.
Because in most cases, a parent reports on the child’s health status, the coefficients on parent’s health status will also absorb any correlation between reporting error in the child and parent’s health status variables. To address the issue of reporting bias more closely, we also estimated regressions in which we controlled specifically for the health status of the household member who assessed the child’s health. This variable was statistically significant for all age categories except 8- to 11-year-olds but did not markedly change the coefficients on household resources.
We are not attributing any behavioral or causal interpretation to the mother’s (or father’s) health status. Rather, we include it to account for any unmeasured genetic or environmental factors that affect the health of both parent and child. In a related literature, Behrman and Rosenzweig (2002) and Plug (2004) found that for developed countries, the correlation between the educational attainment of mothers and their children largely reflects genetic factors and assortative mating. In contrast, Behrman et al. (1999) found that for rural India, maternal literacy leads to increased child schooling.
Kimhi (2003) suggested that health should be viewed as comprising both stock and flow components, with acute morbidity being viewed as a flow.
Diaz (2002) also discussed preliminary medical research of the possibility that the higher prevalence of parasitic infections among the poor at young ages may protect them against chronic conditions.
The objective measures of health (height, weight, and hemoglobin) reflect nutritional intake and the body’s ability to absorb nutrients. They thus reflect both chronic and acute conditions (e.g., diarrhea and nausea).
A similar regression for nurse-assessed health shows that it is a function of days of missed activity and the objective health measures. The equation explains only a very small percentage of the variation in nurses’ evaluations (pseudo-R2 = .016). We also estimated the income gradients net of the effect of reported acute conditions. That is, we regressed parent-reported general health status on the acute conditions and then used the residuals as the dependent variable in the gradient equations. The income gradient does decrease as a result. There is still, however, no evidence of a steepening gradient with age. The remaining portion reflects the combined effect of chronic conditions and acute symptoms that are not correlated with the reported symptoms (e.g., a parent may consider a child to be in somewhat poor health because s/he often has acute illnesses, but the child has not experienced any of the symptoms in the past 4 weeks). Hence, the lack of a gradient in the residual regressions may reflect the remaining impact of acute illness or that there is no gradient even in chronic conditions in developing countries.
References
- Bago d’Uva T, Van Doorslaer E, Lindebloom M, O’Donnell O, Chatterji S.2006“Does Reporting Heterogeneity Bias the Measurement of Health Disparities?”University of York Health and Econometrics Data Group Working Paper 06/03. Department of Economics, University of York; Heslington, York, United Kingdom: [DOI] [PubMed] [Google Scholar]
- Behrman JR, Foster AD, Rosenzweig MR, Vashishtha P. “Women’s Schooling, Home Teaching and Economic Growth”. Journal of Political Economy. 1999;107:682–714. [Google Scholar]
- Behrman JR, Rosenzweig MR. “Does Increasing Women’s Schooling Raise the Schooling of the Next Generation?”. American Economic Review. 2002;92:323–34. [Google Scholar]
- Cameron LA. “The Impact of the Indonesian Financial Crisis on Children: An Analysis Using the 100 Villages Data”. Bulletin of Indonesian Economic Studies. 2001;37(1):43–64. [Google Scholar]
- Case A.2001“Does Money Protect Health Status? Evidence From South African Pensions”Working Paper 268 Woodrow Wilson School of Public and International Affairs, Center for Health and Wellbeing, Princeton University; Princeton, NJ [Google Scholar]
- Case A, Deaton A.2003“Consumption, Health, Gender and Poverty”World Bank Policy Research Working Paper Series No. 3020.World Bank; Washington, DC [Google Scholar]
- Case A, Lubotsky D, Paxson C. “Economic Status and Health in Childhood: The Origins of the Gradient”. American Economic Review. 2002;92:1308–34. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Cebu Study Team “A Child Health Production Function Estimated From Longitudinal Data”. Journal of Development Economics. 1992;38:323–51. [PubMed] [Google Scholar]
- Currie A, Shields M, Wheatley Price S. “The Child Health/Family Income Gradient: Evidence From England”. Journal of Health Economics. 2007;26:213–32. doi: 10.1016/j.jhealeco.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Currie J, Stabile M. “Socioeconomic Status and Child Health: Why Is the Relationship Stronger for Older Children?”. American Economic Review. 2003;93:1813–23. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- Diaz MDM. “Socio-economic Health Inequalities in Brazil: Gender and Age Effects”. Health Economics. 2002;11:141–54. doi: 10.1002/hec.649. [DOI] [PubMed] [Google Scholar]
- Dow W, Gertler P, Schoeni RF, Strauss J, Thomas D.1997“Health Care Prices, Health and Labor Outcomes: Experimental Evidence.”Labor and Population Program Working Paper No. 97-01.RAND; Santa Monica, CA [Google Scholar]
- Filmer D, Pritchett L.2004“Child Mortality and Public Spending on Health: How Much Does Money Matter?”World Bank Policy Research Working Paper No. 1864.World Bank; Washington, DC [Google Scholar]
- Idler EL, Benyamini Y. “Self-rated Health and Mortality: A Review of Twenty-Seven Community Studies”. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Kassouf AL, McKee M, Mossialos E. “Early Entrance to the Job Market and Its Effect on Adult Health: Evidence From Brazil”. Health Policy and Planning. 2001;16:21–28. doi: 10.1093/heapol/16.1.21. [DOI] [PubMed] [Google Scholar]
- Kimhi A. “Socio-Economic Determinants of Health and Physical Fitness in Southern Ethiopia”. Economics and Human Biology. 2003;1:55–75. doi: 10.1016/s1570-677x(02)00007-2. [DOI] [PubMed] [Google Scholar]
- Lavy V, Strauss J, Thomas D, de Vreyer P. “Quality of Health Care, Survival and Health Outcomes in Ghana”. Journal of Health Economics. 1996;15:333–57. doi: 10.1016/0167-6296(95)00021-6. [DOI] [PubMed] [Google Scholar]
- Lavy V, Palumbo M, Stern S.1995“Health Care in Jamaica: Quality, Outcomes, and Labor Supply”Living Standards Measurement Study Working Paper No. 116.World Bank; Washington, DC [Google Scholar]
- Lindeboom M, Van Doorslaer E. “Cut-point Shift and Index Shift in Self-reported Health”. Journal of Health Economics. 2004;23:1083–99. doi: 10.1016/j.jhealeco.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Liu G, Zhang Z. “Sociodemographic Differential of the Self-Rated Health of the Oldest-Old Chinese”. Population Research and Policy Review. 2004;23:117–33. [Google Scholar]
- O’Donnell O, Rosati F, Van Doorslaer E.2002“Child Labour and Health: Evidence and Research Issues.”Understanding Children’s Work Working Paper 1. Innocenti Research Centre, Florence.
- Plug E. “Estimating the Effect of Mother’s Schooling on Children’s Schooling Using a Sample of Adoptees”. American Economic Review. 2004;94:358–68. [Google Scholar]
- Plug E, Vijverberg W. “Schooling, Family Background, and Adoption: Is It Nature or Is It Nurture?”. Journal of Political Economy. 2003;111:611–41. [Google Scholar]
- Sahn D, Alderman H. “On the Determinants of Nutrition in Mozambique: The Importance of Age-Specific Effects”. World Development. 1997;25:577–88. [Google Scholar]
- Skoufias E. “Parental Education and Child Nutrition in Indonesia”. Bulletin of Indonesian Economic Studies. 1999;35:99–119. doi: 10.1080/00074919912331337717. [DOI] [PubMed] [Google Scholar]
- Strauss J, Beegle K, Sikoki B, Dwiyanto A, Herawati Y, Witoelar F. RAND; Santa Monica, CA: 2004. “The Third Wave of the Indonesian Family Life Survey: Overview and Field Report.”. [Google Scholar]
- Strauss J, Thomas D.1995“Human Resources: Empirical Modeling of Household and Family.” 1883–2023.in theHandbook of Development Economics Behrman J, Srinivasan TN.Amsterdam: North-Holland [Google Scholar]
- Strauss J, Thomas D. “Health, Nutrition and Economic Development”. Journal of Economic Literature. 1998;36:766–817. [Google Scholar]
- Van der Klaaw B, Wang L.2004“Child Mortality in Rural India”World Bank Policy Research Working Paper No. 3281.
- Wolfe B, Behrman J. “Determinants of Child Mortality, Health and Nutrition in a Developing Country”. Journal of Development Economics. 1982;11:163–93. doi: 10.1016/0304-3878(82)90002-5. [DOI] [PubMed] [Google Scholar]
- World Bank . World Development Indicators. Washington, DC: World Bank; 2003. [Google Scholar]
- World Bank . World Development Report: Development and the Next Generation. Washington, DC: World Bank; 2007. [Google Scholar]