Figure 1. Elements involved in innate immunity.
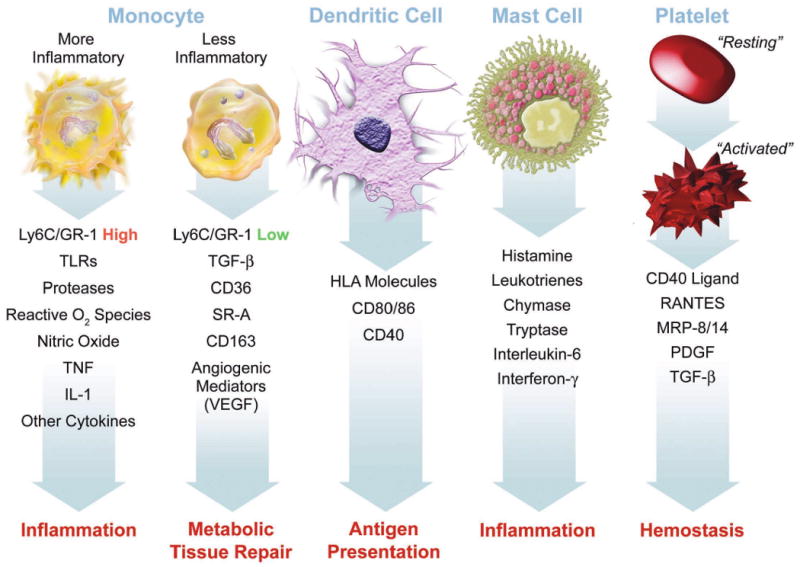
This figure summarizes some of the functions ascribed to various cellular participants in atherosclerosis that may participate in the disease and its complication when dysregulated. Mononuclear phagocytes represent the bulwark of the innate immune defenses in mammals. Monocytes give rise to macrophages, which in the arterial intima form foam cells, the hallmark of the arterial fatty streak. Recent work has focused on heterogeneity of mononuclear phagocytes. We now recognize a pro-inflammatory subset distinct from a less inflammatory population of monocytes. The inflammatory subset expresses high levels of the cell-surface marker Ly6c (also known as GR-1) in the mouse. These inflammatory monocytes express higher levels of Toll-like receptors (TLR), and the other functions indicated, including elaboration of high levels of the cytokines tumor necrosis factor (TNF) and interleukin-1 (IL–1). The less inflammatory subset of monocytes express higher levels of transforming growth factor beta (TGF-beta), the scavenger receptors CD36 and scavenger receptor – A (SR-A), and angiogenic mediators including vascular endothelial growth factor (VEGF). Dendritic cells express human leukocyte antigen (HLA) molecules among the other indicated structures. Dendritic cells present antigens to T cells, linking innate to adaptive immunity. Mast cells elaborate many mediators as shown. Recent data support a causal role for mast cells in mouse atherosclerosis. Platelets also participate in adaptive immunity. When activated, platelets exteriorize CD40 ligand (CD40L or CD154) and release mediators including RANTES (regulated and T cell expressed secreted), myeloid related protein – 8/14 (MRP-8/14), platelet-derived growth factor (PDGF), and TGF-beta.
