Abstract
Clinical features and treatment outcome were compared in depressed outpatients with and without a history of emotional and physical abuse (EPA), including childhood maltreatment. Patients were initially randomized to IPT or SSRI and then augmented with the second treatment if they did not remit with monotherapy. Assessments included the SCID-I, the SCID-II for DSM-IV diagnoses, the HRSD, the QIDS and the Mood Spectrum Self-Report (MOODS-SR). Seventy-eight (25%) patients reported a history of EPA; 60 (76.9%) were women. Patients with a history of EPA did not differ from those without on HRSD scores at baseline, but showed an earlier age at onset of depression and a longer duration of illness. The two groups differed on several mood spectrum factors, namely: ‘depressive mood’ (15.6±4.9 vs. 13.5±5.4; p<0.004), ‘psychomotor retardation’ (11.7±4.5 vs. 9.6±4.7; p<0.001), ‘drug and illness-related depression’ (1.3±1.3 vs. 0.6±1.0; p<0.0001), and ‘neurovegetative symptoms’ (8.3±2.6 vs. 6.9±2.9; p<0.0001). Patients with EPA had also a significantly longer time to remission (89 vs. 67 days, log-rank test, p=0.035). The need for augmentation treatment was significantly more frequent among patients with EPA than in those without. The present study suggests that patients with a history of EPA show a subtype of depression characterized by poor treatment response and more severe neurovegetative and psychomotor symptoms.
Keywords: Life events, emotional abuse, physical abuse, sexual abuse, depression, mood, spectrum
1. Introduction
Childhood maltreatment and abuse are risk factors for the onset of depression in the adulthood, according to a large number of retrospective and prospective studies (Bifulco et al., 1994; Boudewyn & Liem, 1995; Bifulco et al., 1998; Gibb et al., 2001; Hankin, 2005; McNally et al., 2006). Childhood maltreatment may be related to the subsequent occurrence of depressive symptoms through multiple mechanisms, including actual physical changes (e.g., impaired brain development, poor physical health), psychological sequelae (e.g., low self-esteem, sense of powerlessness, social isolation), or behavioral consequences (e.g., delinquency, teen pregnancy, low academic achievement) (Chalk et al., 2002; Colman & Widom, 2004; Nemeroff, 2004). The development of an ‘insecure attachment style’, extremely frequent among maltreated children (Toth et al., 1992; Cicchetti, Rogosch, & Toth, 1994), is considered a potent risk factor for depression among adults (Carnelley et al., 1994; Roberts et al., 1996). However, attachment style is only one of multiple processes that might mediate the maltreatment-depression link, and other possible mediating factors have been suggested. For example, the ‘integrative etiological model’ of depression, and the ‘cognitive vulnerability transactional stress model’, by Hankin & Abramson (2001), postulated a classification of ‘distal risk factors’ for depression, including a childhood history of maltreatment and adversity. According to this approach, childhood maltreatment contributes to the development of depression through the induction of elevated levels of cognitive vulnerability to negative life events. This leads to negative inferences about the cause, consequence, and meaning of the event as interpreted by the individual.. Following the ‘negative cognitive style’ model (Ingram et al., 1998; Abramson et al., 2002), individuals who experienced adversity or maltreatment as children are more prone to understand and explain why the aversive events occurred. This inferential process may lead to the formation of a negative cognitive style that, in turn, predisposes the individual to depression. Furthermore, the model postulates that childhood maltreatment leads to an increased likelihood of experiencing a greater number of stressful life events later in life, consistent with the interpersonal approaches to depression (Hammen, 1991; Joiner & Coyne, 1999). In a large community study the relationship between childhood maltreatment and depression has been investigated from a different perspective: the authors examined whether a history of physical or sexual abuse in childhood was associated with the development of particular neurovegetative symptom clusters of depression in adulthood (Levitan et al., 1998). They found an association between a history of sexual/physical abuse in childhood and major depression with reverse neurovegetative features, namely increased appetite, weight gain, and hypersomnia.
Another line of research has addressed the relationship between experiences of abuse in adulthood and depression, with a special focus on intimate-partner violence in women (Al Modallal et al., 2008). Fogarty et al. (2008) reported that child abuse and intimate partner violence have a synergistic effect on depressive symptoms in women and Bernazzani and Bifulco (2003) found that adverse non-live pregnancy/births together with marital adversity and childhood neglect/abuse are the best predictors of lifetime depression. Moreover, Brown et al. (2008) documented an indirect link between parental maltreatment and adult chronic depression mediated by aversive sexual relationships and single parent status. These findings postulate a model of depression that links difficult environments, close relationships and issues of loss.
New research has found an association between sensitivity to traumatic experiences, in childhood and in adulthood, and/or to adverse environments, and genetic polymorphisms of the serotonin transporter gene promoter region (5-HTTLPR) locus of the serotonin transporter (5-HTT) gene (Cervilla et al., 2007; Stein et al., 2008). Furthermore, the combination of polymorphisms of brain derived neurotrophic factor (BDNF), 5-HTTLPR, and maltreatment/stressful life events has been associated with increased risk of depression in both child (Wichers et al., 2007) and adult populations (Kim et al., 2007). Given the variety of genetic and environmental factors influencing brain systems that are crucial for the development of depression (Pezawas et al., 2005), it is not surprising that a history of maltreatment have been shown to modulate the expression of different clinical phenotypes of depression. It remains unclear, therefore, whether these events have a specific role as risk factors beyond a ‘general adverse background’ effect for onset, severity and other clinical parameters of depression (Gladstone et al., 2004). In the effort to contribute to the scientific discourse in this area, we compared the clinical features and treatment outcome of outpatients with major depression with and without a history of EPA in childhood and/or adulthood. We hypothesized that patients with such events would have more severe depressive symptoms, higher levels of comorbidity with Axis-I and II disorders and poorer treatment outcome.
2. Methods
2a. Participants
The study sample consists of 312 outpatients with a current major depression who participated in either the pilot or the full phase of the study “Depression: The Search for Treatment-relevant Phenotypes.” (Frank et al., 2008). Patients were recruited between February 2002 and March 2007 at the outpatient clinics of the Departments of Psychiatry of the Universities of Pisa and Pittsburgh. The investigation was carried out in accordance with the latest version of the Declaration of Helsinki. The Ethical Committees of the University of Pittsburgh and Pisa approved the study design and procedures. All subjects entering the protocol provided written informed consent after receiving a complete description of the study and having the opportunity to ask questions.
2b. Study design and treatment protocol
Inclusion criteria were: age between 18 and 66, being able and willing to give informed consent, currently being in an episode of non-psychotic major depression as defined by the Structured Clinical Interview for Axis-I DSM-IV Disorders (SCID-I), a rating of ≥15 on the 17-item Hamilton Rating Scale for Depression (HRSD-17), and not currently receiving effective treatment. Females of childbearing potential had to practice an acceptable form of birth control. Subjects with suicidal ideation were eligible as long as outpatient treatment was deemed safe. Exclusion criteria were: a history of manic or hypomanic episodes, a history of schizophrenia or schizoaffective disorder, current primary diagnosis of eating disorder, drug and/or alcohol dependence or abuse, current psychosis, antisocial personality disorder, organic affective syndrome, kidney or liver disease, epilepsy, severe and untreated cardiovascular disease and any uncontrolled illness. Patients with a well-documented history of an inability to tolerate one of the study treatments or currently receiving treatment with an effective antidepressant were also excluded. In the initial phase of treatment, subjects were randomly assigned to pharmacotherapy with SSRI (citalopram or escitalopram) or psychotherapy (interpersonal psychotherapy - IPT) (Klerman & Weissman, 1987). The acute treatment phase of the study involved three assessment and triage points, at weeks 6, 12, and 20. Those patients assigned to pharmacotherapy who did not evidence a response, defined as a 50% reduction of baseline score on the HRSD first were increased from the initial daily dose of citalopram (20 mg) or escitalopram (10 mg) to a dose of 40 or 20 mg, respectively, at week 3. If patients could not tolerate an initial dose of 10 mg of escitalopram, the dose could temporarily be reduced to 5 mg and titrated up from that point. If patients did not evidence a response by Week 6, they were given psychotherapy in addition to pharmacotherapy. IPT was added by Week 12 if they did not meet stabilization criteria (as in the case of initial improvement followed by worsening). Those patients assigned to psychotherapy that did not evidence a response after 6 weeks of acute treatment (week 6) had pharmacotherapy added to their treatment. Patients who showed an initial response at week 6 but who later worsened had a second opportunity to receive pharmacotherapy augmentation at week 12. All patients still on monotherapy at week 12 who had not met the criteria for remission (average HRS-D < 7 over 3 weeks) had the other treatment (pharmacotherapy or psychotherapy) added to their treatment regimen. Patients who had not remitted with combined psychotherapy and pharmacotherapy at week 20 continued IPT and switched from citalopram or escitalopram to a second antidepressant, following the guidelines provided by the Texas Medication Algorithm Project (Trivedi et al., 2004). Patients who relapsed were offered additional or alternative treatment and continued to be followed in the study for up to 6 months of continuation treatment.
2.c Clinical Assessments
EPA Assessment
At the Pittsburgh site, patients were asked at baseline about any sexual, emotional or physical abuse experienced in childhood and/or adulthood, using a grid in which information was collected on the identity of the perpetrator and the type of event. At the Pisa site no grid was used. Information, including the age of onset of the event, was obtained only from patients (without external evidence) during the clinical interview. Events were categorized as emotional, sexual or physical, were coded as ‘present’ or ‘absent’, and not characterized in terms of their severity, duration or frequency. Sexual abuse was defined as any unwanted sexual experience (also involving parents). Physical abuse was defined as any physical aggression or violence. Emotional neglect was defined as perceived emotional rejection by parents or significant ones. If experiences of childhood abuse were reported, permission was asked to proceed with further questioning, only when it was deemed useful for the clinical management of patient’s symptomatology. At the end of the study, at both sites a chart review was carried out to search for instances of EPA reported spontaneously to clinicians after the baseline assessment. The list described by patients encompassed a number of events, including: being the victim of verbal, physical or sexual abuse by parents, other relatives, partners, husband, ex-husband, or friends; being bullied at school; being the witness of an abuse, or violence; being raped; being threatened with weapon. Clinical Interviews At Pisa and Pittsburgh sites, the diagnostic assessment was conducted using the SCID-I for DSM-IV diagnoses by clinicians trained and certified to the use of the interviews when high levels (>0.90) of inter-rater reliability of their diagnoses with the trainer were achieved. All interviewers had long-standing experience in the administration of standardized interviews. The assessment of Axis-II Personality Disorders was conducted using the SCID-II for DSM-IV diagnoses. Other study assessments included established interview-based assessments of the severity of depressive symptoms, namely the Hamilton Rating Scale for Depression (HRSD) (Hamilton, 1960). Self-Report Questionnaires The Quick Inventory of Depressive Symptomatology (QIDS) (Rush et al., 2003), and the more recently developed and validated assessment of mood spectrum, the MOODS-R, were administered. The MOODS-SR was derived from the corresponding structured interview (Fagiolini et al., 1998), and focuses on the presence of manic and depressive symptoms, traits and lifestyles that may characterize both the symptomatic and ‘temperamental’ affective dysregulations that make up both fully syndromal and subthreshold mood disturbances. These include symptoms that are either isolated or clustered in time and temperamental traits that are present throughout an individual’s lifetime. The MOODS-SR consists of 161 items coded as present or absent for one or more periods of at least 3–5 days in the time frame investigated (the subject’s lifetime or the last-month, according to the version of the instrument). The instrument can be downloaded from the web site www.spectrum-project.net where it is available in the lifetime and in the last-month version. In the present study, we administered the lifetime version of the MOODS-SR at baseline. Using exploratory factor analysis, 6 depressive factors were extracted, accounting overall for 48.3% of the variance of the 74 items (Cassano et al., 2008): 1. Depressive mood, including a number of symptoms and temperamental features that span depressed mood, loss of interests and loneliness; 2. Psychomotor retardation, including impairment in different areas of daily activities, physical weakness and tiredness, speech or slowed thinking; 3. Suicidality, including suicidal ideation, plans and attempts; 4. Drug/Illness-related depression, exploring mood changes when ill or after having taken substances; 5. Psychotic features, exploring excessive interpersonal sensitivity and paranoid thoughts; 6. Neurovegetative symptoms, exploring changes in sleep, appetite and sexual function.
3. Data analysis
Demographic and clinical characteristics were compared between patients with and without EPA using the t-test, ANOVA F-test or the chi-square test when appropriate. Time to remission was compared between the two groups using a log-rank test. A log rank test stratified by gender was also carried out. To estimate the hazard ratio of remission within 3 months of treatment in patients with EPA compared with patients without, Cox regression models associated with the likelihood ratio test were performed with adjustment for randomization and for the potential confounding effect of clinical variables. Statistical analyses were performed using SPSS, version 16.0.1.
4. Results
4a. Demographic and clinical characteristics of study participants
Two-hundred and twenty-eight patients were women (73%), and 78 (27%) were men. Seventy-eight (25%) of the 312 study participants reported experiencing significant EPA; 60 of them (76.9%) were women. The demographic and clinical characteristics of participants are provided in Table 1. Participants were, on average, 39 years old, more likely to be female and employed, and had a median educational level of 13 years. Participants with a history of EPA did not differ from the remaining participants on demographic characteristics. Fifty-three participants (17%) reported 1 event, 17 (5.4%) reported 2 different events, and 8 (2.6%) reported 3 different events. Subjects with and without EPA were compared on clinical variables, including age at onset of depression, duration of illness, number of lifetime episodes and HRSD severity scores at study entry. No differences were found on HRSD scores at study entry between the two groups. Conversely, age at onset of the first depressive episode was significantly lower in patients with EPA (23.1±12.2 vs. 29.4±12.6; t-test=3.8, df=306, p<0.001), who showed also a longer duration of depressive illness (16.5±14.7 years vs. 11 9.7±11.1 years, t-test=3.72, df=108.5; p<0.0001), and a higher burden of lifetime comorbidity with Axis-I disorders (69.2% vs 53.8%, χ2 =5.67, p=0.017). While lifetime PTSD accounted for this difference to some extent, (9% in patients with maltreatment and 1.3% in subjects without), when comorbidity was calculated excluding PTSD, the difference between groups remained significant (66.7% vs. 53.8, χ2 =3.92, p=0.048). As expected, GAD and PTSD were significantly more common among participants with EPA. Patients with EPA were more frequent at the Pittsburgh site compared with the Pisa site (37.9% vs. 12.6%; χ2 =26.68 (df=1), p<0.001). The frequency of Axis II diagnoses in the two groups is provided in Table 2. Subjects with EPA were significantly more likely to meet criteria for Cluster A and Cluster C diagnoses. No differences were found for Cluster B diagnoses. Table 3 reports group comparisons of mood spectrum factors. Participants with EPA had higher scores on MOODS-SR factors: ‘depressive mood’ (15.6±5.0 vs. 13.6±5.4; t-test= 2.88, p=0.004), ‘psychomotor retardation’ (11.7±4.6 vs. 9.6±4.6; t-test=3.33, p=0.001), ‘drug and illness-related depression’ (1.3±1.3 vs. 0.6±1.0; t-test=3.70, p<0.0001), and ‘neurovegetative symptoms’ (8.3±2.6 vs. 6.9±2.9; t-test=3.69, p<0.0001), but not on suicidality. Table 4 reports the EPA by study site.
TABLE 1.
Demographic and clinical characteristics of depressed patients with and without a history of Emotional and Physical Abuse (EPA)
| Characteristics | Patients with EPA (n=78) | Patients without EPA (n=234) | Analysis | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t (df=310) | P | |
| Age (years) | 39.2 | 12.8 | 38.9 | 12.0 | Ns | |
| Education (years) | 13.7 | 3.0 | 13.7 | 3.6 | Ns | |
| N | % | N | % | X2 (df=1) | P | |
| Female | 60 | 76.9 | 168 | 71.8 | Ns | |
| Married or partnered | 25 | 32.1 | 98 | 41.9 | Ns | |
| Employed | 56 | 71.8 | 151 | 64.5 | 1.383 | 0.240 |
| Median number of depressive episodes | 3 | 2 | Mann-Whitney Z=1.9 | 0.062 | ||
| Mean | SD | Mean | SD | t (df=310) | P | |
| Age of onset of depression (years) | 23.1 | 12.2 | 29.4 | 12.6 | <0.001 | |
| Duration of Illness | 16.5 | 14.7 | 9.7 | 11.1 | <0.0001 | |
| HAM-D score at baseline | 20.6 | 4.2 | 20.0 | 3.9 | Ns | |
| QIDS score at baseline | 14.1 | 4.4 | 13.0 | 4.4 | 1.8 | 0.072 |
| N | % | N | % | X2 (df=1) | P | |
| Any Axis I Comorbidity | 54/78 | 69.2 | 126/23 | 53.8 | 5.7 | 0.017 |
| Any Anxiety Disorder | 45/78 | 57.7 | 109/23 | 46.6 | 2.880 | 0.058 |
| Panic Disorder | 15/78 | 19.2 | 54/234 | 23.1 | 0.502 | 0.294 |
| GAD | 29/78 | 37.2 | 34/234 | 14.5 | 18.623 | 0.0001 |
| Social Phobia | 7/78 | 9.0 | 19/234 | 8.1 | 0.813 | 0.487 |
| OCD | 3/78 | 3.8 | 9/234 | 3.8 | 0.000 | 0.650 |
| PTSD | 7/78 | 9.0 | 3/234 | 1.3 | 11.158 | 0.003 |
TABLE 2.
Personality Disorders in depressed patients with and without a history of Emotional and Physical Abuse (EPA)
| Characteristics | Patients with EPA (n=78) | Patients without EPA (n=234) | test | |||
|---|---|---|---|---|---|---|
| Personality Disorders (SCID-II)* | N | % | N | % | X2 or Fisher exact test (df=1) | P |
| Any personality disorder (also including depressive, passive-aggressive, NOS) | 41 | 52.6 | 94 | 40.2 | 3.66 | 0.056 |
| Avoidant personality disorder | 19 | 24.4 | 31 | 13.2 | 5.37 | 0.021 |
| Borderline personality disorder | 5 | 6.4 | 13 | 5.6 | 0.08 | 0.779 |
| Dependent personality disorder | 3 | 3.8 | 7 | 3.0 | 0.715 | |
| Depressive personality disorder | 7 | 9.0 | 21 | 9.0 | 0 | 1 |
| Narcissistic personality disorder | 0 | 0 | 2 | 0.9 | 1 | |
| Obsessive-compulsive personality disorder | 18 | 23.1 | 35 | 15.0 | 2.73 | 0.980 |
| Paranoid | 9 | 11.5 | 9 | 3.8 | 6.37 | 0.012 |
| Passive-aggressive | 3 | 3.8 | 6 | 2.6 | 0.696 | |
| Schizoid | 3 | 3.8 | 4 | 1.7 | 0.372 | |
| Histrionic | 0 | 0 | 2 | 0.9 | 1 | |
| Cluster A | 10 | 12.8 | 12 | 5.1 | 5.28 | 0.022 |
| Cluster B | 5 | 6.4 | 16 | 6.8 | 0.017 | 0.896 |
| Cluster C | 34 | 43.6 | 63 | 29.6 | 7.85 | 0.006 |
no patient met criteria for antisocial personality disorder or for schizotypal personality disorder
TABLE 3.
MOODS-SR Lifetime Depressive Factors in depressed patients with and Emotional and Physical Abuse (EPA)
| Characteristics | Patients with EPA (n=78) | Patients without EPA (n=234) | Analysis | |||
|---|---|---|---|---|---|---|
| MOODS-SR Depressive Factors | mean | SD | mean | SD | t (df=310) | P |
| Depressive mood | 15.6 | 4.9 | 13.5 | 5.4 | 2.879 | 0.004 |
| Psychomotor Retardation | 11.7 | 4.5 | 9.6 | 4.7 | 3.333 | 0.001 |
| Suicidality | 2.0 | 1.8 | 1.7 | 1.6 | 1,557 | 0,120 |
| Drug/Illness related depression | 1.3 | 1.3 | 0.6 | 1.0 | 4.301 | 0.0001 |
| Psychotic Symptoms | 4.5 | 2.1 | 4.4 | 2.1 | 0.338 | 0,736 |
| Neurovegetative symptoms | 8.3 | 2.6 | 6.9 | 2.9 | 3,693 | 0.0001 |
TABLE 4.
Emotional and Physical Abuse (EPA) in Patients with Depression
| Pisa Site (n=159) | Pittsburgh Site (n=153) | |||
|---|---|---|---|---|
| Number of EPA | N | % | N | % |
| One EPA | 20 | 100 | 33 | 56.9 |
| 2 EPA | - | - | 17 | 29.3 |
| >2 EPA | - | - | 8 | 13.8 |
| Total | 20/159 | 12.6^ | 58/153 | 37.9^ |
| Type of EPA | EPA at Pisa Site (n=20 EPA in 20 pts) | EPA at Pittsburgh Site (n=97 EPA in 58 pts) | ||
| Emotional | N | % | N | % |
| bullied at school | 1 | 5.0 | 6 | 6.2 |
| father | 1 | 5.0 | 15 | 15.4 |
| mother | - | - | 6 | 6.2 |
| both parents | 2 | 10.0 | 5 | 5.2 |
| stepfather/mother’s boyfriend | - | - | 3 | 3.1 |
| boyfriend/husband | 4 | 20.0 | 6 | 6.2 |
| witnessing a physical abuse | - | - | 2 | 2.0 |
| others emotional EPA | - | - | 4 | 4.1 |
| Physical | N | % | N | % |
| father | - | - | 7 | 7.2 |
| mother | - | - | 5 | 5.2 |
| both parents | - | - | 4 | 4.1 |
| stepfather | - | - | 2 | 2.0 |
| (ex) boyfriend/husband | 4 | 20.0 | 4 | 4.1 |
| others | - | - | 5 | 5.2 |
| Sexual | N | % | N | % |
| father | 3 | 15.0 | 2 | 2.0 |
| mother | - | - | - | - |
| both parents | - | - | 1 | 1.0 |
| Stepfather/mother boyfriend | - | - | 4 | 4.1 |
| other relatives | - | - | 5 | 5.2 |
| (ex) boyfriend/husband | - | - | 3 | 3.1 |
| others | 5 | 25.0 | 8 | 8.2 |
Pearson Chi-Square
Value: 26,681; df=1; Asympt. Sign. (2-sided): p<0.0001
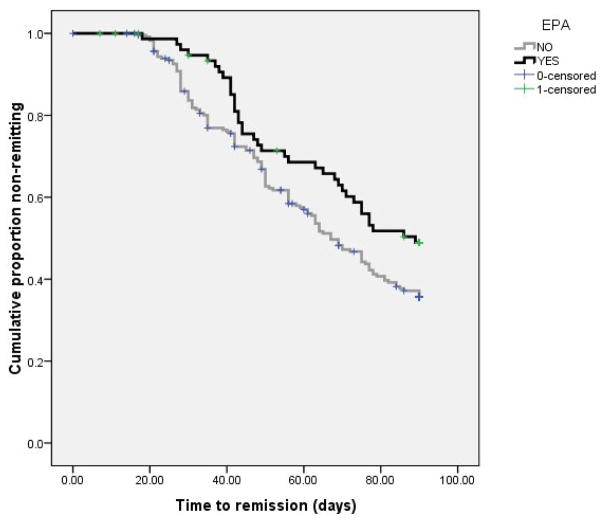
4b. Treatment outcomes
Remission by visit 12 (~90 days of treatment) was achieved by 164 subjects (52.6%). Patients with a history of EPA were less likely to remit, but not significantly (44.9% vs. 55.1%; χ2 =2.47; p=0.116) and were more likely to require combined treatment to achieve remission (44/78; 56.4% vs. 87/234; 37.2%; χ2 = 8.88; df=1; p=0.003). Time to remission was significantly longer (median: 89 vs. 67 days, log-rank 12 test 4.45, p=0.035) in participants with EPA in a Kaplan-Meier survival analysis (Figure 1). Because females were more likely to experience EPA we estimated the survival curves separately in the two genders and found that women with such experiences had a significantly longer time to remission compared with women without (log-rank test 8.06, p=0.005), while this was not the case in men (log-rank test 0.28, p=0.594). The association between EPA and longer time to remission in females remained significant in a Cox regression model with adjustment for randomization (OR=1.68, 95% 1.09–2.59, p=0.018). In a further Cox regression model including EPA (yes/no), randomization, any axis-I disorder, any axis-II disorder, and age of onset as the independent variables, the presence of EPA independently predicted a longer time to remission even after controlling for these potential confounders (OR=1.64, 95% CI 1.07–2.52, p=0.024). We carried out secondary K-M survival analyses to examine the relationship between time to remission, the type of abuse (emotional, physical, sexual) and the number of experiences reported. Patients with emotional (Log-rank=3.281, p=0.07) and physical abuse (Log-rank=3.414, p=0.065) had a borderline significantly longer time to remission, while no evidence of an association with time to remission was found for sexual abuse (log-rank=0.727, p=0.394). We found an indication of a dose-response relationship between the number of EPA and longer time to remission: while the pairwise comparison between patients with 1 vs. no experience approached significance (log-rank of 2.569, p=0.10), that between patients with 2 or more experiences vs. none was significant (log-rank=4.577, p=0.032). Median time to remission (in days) was 67 in patients with no EPA and 78 in patients with 1 EPA. The median time to remission could not be estimated for those with 2 or more experiences because fewer than 50% of them remitted.
Figure 1.
Time to remission in patients with and without EPA.
5. Discussion
The psychological sequelae of EPA are widely described in clinical and non-clinical samples. Reports of physical and sexual abuse in childhood are more frequent in psychiatric patients than in general population, and several studies focused on the long-term psychopathological consequences of childhood traumatic experiences (Swett et al., 1990; Palmer, 1992). The majority of finding relied on retrospective recall, following the hypothesis that the presentation of depression in adulthood might be modulated by the experience of early psychological traumas, such as neglect, physical, sexual or emotional abuse (e.g., Feiring et al., 1998; Bolger & Patterson, 2001; Cohen, et al., 2001). However, there are limitations and gaps in the current state of knowledge on two main topics: the treatment response of depressive episodes in patients with a history of EPA, and the occurrence of specific patterns of depressive symptoms in this subgroup of patients. In our study, we found that patients with major depressive episodes and a history of EPA had a poorer treatment outcome. They had significantly longer time to remission and needed combined treatment more frequently, when compared to patients without EPA. We found that depressed patients with a history of EPA did not differ from those without, on current depression severity (although they developed depression earlier in life and had a longer duration of illness). However, we were interested in elucidating whether a history of EPA such as physical, emotional or sexual abuse was associated with specific symptom clusters of depression. In order to collect information on depressive signs and symptoms over the entire lifetime, we administered the MOODS-SR, Lifetime Version. The MOODS-SR explores not only the typical depressive symptomatology but also atypical symptoms, traits and lifestyles that may characterize both the symptomatic and ‘temperamental’ affective dysregulations that make up both fully syndromal and sub-threshold mood disturbances. These include symptoms that are either isolated or clustered in time and temperamental traits that are present throughout an individual’s lifetime. The between-group comparison of lifetime MOODS-SR factors identified several differences. The lifetime ‘depressive mood’ factor score indicated that depressed patients with EPA were more likely to experience both typical and atypical features of depression during their lifetime. This finding is not surprising, given that patients with EPA showed an earlier age at onset and a longer duration of illness. More interestingly, the ‘psychomotor retardation’ factor and the ‘neurovegetative symptoms’ (including sleep disturbances) factor scores were higher among participants with EPA. This result is in line with a previous study of Levitan and Colleagues (1998) who, as noted above,, found an association between a history of sexual/physical abuse in childhood and the occurrence of major depression with atypical and reverse neurovegetative features, such as increased appetite, weight gain, and hypersomnia.
Harkness and Monroe (2002) also found a relationship between severe levels of childhood adversity or childhood maltreatment (especially sexual abuse) and the presence of neurovegetative symptoms although, in this case, it was the typical neurovegetative symptoms such as insomnia, loss of appetite and loss of interest in sex associated with the endogenous subtype of depression. Difficulties initiating sleep, disrupted sleep, early morning awakening and non-restorative sleep are common among patients with a history of maltreatment, raising the question as to whether they are related to the presence of full-fledged PTSD, to the direct effect of the traumatic event on arousal, or to the occurrence of a depressive episode (Ohayon and Shapiro, 2000). The relationship between EPA and suicidality has been explored in the literature, mainly in the general population, with a number of studies pointing especially to childhood trauma as a predisposing factor to suicidal behavior (Mc Holm et al., 2003), but we did not find any differences in current suicidal ideation or lifetime suicidal attempts between the two groups. These finding is largely explained by the specific inclusion criteria of the study that selected participants with no current suicidal risk. Comparison on Axis-I comorbidity of our sample revealed that patients with a history of EPA had more lifetime comorbidity than those without. As expected, PTSD was more frequent in patients with a history of EPA. Of some interest is the finding of a higher frequency of GAD among patients with maltreatment than among patients without. It is possible that the occurrence of EPA and especially childhood maltreatment exacerbates or triggers a constant state of hyper-arousal and vigilance, both of which constitute core symptoms of GAD. The comparison on Axis II comorbidity showed that subjects with EPA were significantly more likely to meet criteria for Cluster A and Cluster C diagnoses. According to the literature, childhood abuse and neglect are strong risk factors for the development of subsequent personality disorders; vice-versa patients with personality disorders usually have increased rates of childhood maltreatment across a range of abuse types, such as emotional abuse, physical abuse, and neglect (Bierer et al., 2003; Battle et al., 2004). It is noteworthy that the effect of various types of childhood abuse is not confined to clinical populations. Community studies report on the wide presence of ‘sub-clinical personality traits and symptoms’ related to the occurrence of childhood maltreatment (Johnson et al., 1999; Gibb et al., 2001; Johnson et al., 2006; Grover et al., 2007). This suggests a wide spectrum of ‘personality’ outcomes in the wake of maltreatment. Therefore, our results highlight that patients with EPA have an increased proneness to anxiety symptoms, as detected at different levels. The Axis-I, Axis-II and the spectrum assessments all pointed to the lifetime occurrence of anxiety symptoms, personality traits, signs and acquired lifestyles that are long lasting and that may be interpreted in different ways. For example, the presence of anxiety could be one of the consequences of the lifetime occurrence of stressful experiences of varying levels of severity; conversely, early onset symptoms or stable traits of an anxious personality could lower the subjective threshold for the perception of environmental, interpersonal, familial and social events as stressful, and may predispose to the occurrence of depressive symptoms.
Study Limitations
Our results should be interpreted in the light of several limitations. First, information on EPA was gathered retrospectively. Second, information was collected from a sample of patients who were experiencing a depressive episode, and the depressive state itself might have influenced the quality and quantity of recall of negative events, especially for the ‘perceived emotional abuses’ (Brewin et al., 1993; Hardt & Rutter, 2004; Kendall-Tackett & Becker-Blease, 2004).
Regarding the first limitation, we cannot exclude in a systematic manner the possible positive or negative biases, especially in assessing childhood maltreatment. As noted in a recent review by Hardt & Rutter (2004), ‘retrospective reports in adulthood of major adverse experiences in childhood involve a substantial rate of false negatives, and substantial measurement error. On the other hand, although less easily quantified, false positive reports are probably rare’ According to Kendall-Tackett & Becker-Blease (2004), even if prospective designs are usually considered as more rigorous (with less biased sample selection and better measurement of childhood negative experiences) both prospective and retrospective designs may miss survivors who decided to never report their abuse to anyone. Moreover, in prospective studies the more severe abuse may be the unreported ones, given that, when abuse is identified during childhood, it stops. Conversely, when no one knows about ongoing abuse, it can continue, and may even escalate. Given that, prospective findings are suitable, but retrospective findings may measure that specific segment of the population of adult survivors missed by prospective studies (Kendall-Tackett & Becker-Blease, 2004). Concerning the second limitation (Is the depressive state itself influencing the quality and quantity of recall of EPA?) we were aware that especially the early negative memories could have been reinforced during a depressive episode. Nonetheless, several authors pointed out that concern on the general unreliability of retrospective reports is exaggerated and there is little reason to link psychiatric status with less reliable or less valid recall of early experiences (Brewin et al., 1993). However, in order to minimize this risk in our study, we carried out a thorough clinical interview at baseline, in which we addressed the occurrence of interpersonal problems, abuses, and childhood negative experiences. Moreover, at the end of the study, a chart review was carried out with two purposes: 1) to search for instances of EPA reported spontaneously to clinicians after the baseline assessment; 2) to double-check the information obtained at the baseline assessment with the information reported in patients’ charts.
A third limitation is that we did not examine childhood and adulthood abuse separately. This has implications for the generalizability of our findings to theoretical models and prior research examining abuse experienced in exclusively childhood.
Concluding remarks
The relationship between lifetime occurrence of a wide range of mood signs, symptoms and acquired lifestyles, as evaluated by the mood spectrum assessment, and the past experience of EPA is our original contribution in this field. We found that a history of EPA characterizes a subgroup of patients with poorer response to treatment, and more severe mood, energy and neurovegetative rhythm dysregulations, as assessed by the MOODS-SR. We believe that our findings have important clinical implications for the treatment of depressive disorders. For example, individuals who experienced EPA and who are currently experiencing a depressive episode should be offered a combined treatment with IPT and SSRIs, especially when energy and neurovegetative rhythm dysregulations are present. Given this finding, we argue that future work in this area would benefit from a systematic assessment with the mood spectrum approach.
Acknowledgments
The data for this report were drawn from the full study phases of a study entitled: Depression: The Search for Treatment-Relevant Phenotypes. The investigators were: PI: E. Frank (Pittsburgh), CoPI: G.B. Cassano (Pisa). Pittsburgh Co-Investigators: B. Pollock, M.K. Shear, P. Pilkonis, A. Fagiolini, P. Rucci, H. Swartz, D. Kupfer, R. Bies. Pisa Co-Investigators: L. Dell_Osso, M. Mauri, S. Banti, A. Benvenuti, L. Maggi, M. Miniati, A. Papasogli, M. Saettoni, G. Gray.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Abramson LY, Alloy LB, Hankin BL, Haeffel GJ, MacCoon D, Gibb BE. Cognitive vulnerability-stress models of depression in a self-regulatory and psychobiological context. In: Gotlib IH, Hammen C, editors. Handbook of depression. New York: Guilford Press; 2002. pp. 295–313. [Google Scholar]
- 2.Akiskal HS. Searching for Behavioral indicators of Bipolar II in patients presenting with major depressive episodes: the ‘red sign’, the ‘rule of three’ and other biographic signs of temperamental extravagance, activation and hypomania. Journal of Affective Disorders. 2005;84:279–290. doi: 10.1016/j.jad.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Al-Modallal H, Peden A, Anderson D. Impact of physical abuse on adulthood depressive symptoms among women. Issues Ment Health Nurs. 2008 Mar;29(3):299–314. doi: 10.1080/01612840701869791. [DOI] [PubMed] [Google Scholar]
- 4.Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, Sanislow CA, Skodol AE, Gunderson JG, Grilo CM, McGlashan TH, Morey LC. Childhood maltreatment associated with adult personality disorders: findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Personality Disorders. 2004;18:193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- 5.Bernazzani O, Bifulco A. Motherhood as a vulnerability factor in major depression: the role of negative pregnancy experiences. Soc Sci Med. 2003 Mar;56(6):1249–60. doi: 10.1016/s0277-9536(02)00123-5. [DOI] [PubMed] [Google Scholar]
- 6.Bierer LM, Yehuda R, Schmeidler J, Mitropoulou V, New AS, Silverman JM, Siever LJ. Abuse and neglect in childhood: relationship to personality disorder diagnoses. CNS Spectrums. 2003;8:737–754. doi: 10.1017/s1092852900019118. [DOI] [PubMed] [Google Scholar]
- 7.Bifulco A, Brown GW, Harris TO. Childhood experience of care and abuse (CECA): A retrospective interview measure. Journal of Child Psychology and Psychiatry. 1994;35:1419–1435. doi: 10.1111/j.1469-7610.1994.tb01284.x. [DOI] [PubMed] [Google Scholar]
- 8.Bifulco A, Brown GW, Moran P, Ball C, Campbell C. Predicting depression in women: The role of past and present vulnerability. Psychological Medicine. 1998;28:39–50. doi: 10.1017/s0033291797005953. [DOI] [PubMed] [Google Scholar]
- 9.Bolger KE, Patterson CJ. Pathways from child maltreatment to internalizing problems: Perceptions of control as mediators and moderators. Development and Psychopathology. 2001;13:913–940. [PubMed] [Google Scholar]
- 10.Boudewyn AC, Liem LH. Childhood sexual abuse as a precursor to depression and self destructive behavior in adulthood. Journal of Trauma and Stress. 1995;8:445–459. doi: 10.1007/BF02102969. [DOI] [PubMed] [Google Scholar]
- 11.Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: A reappraisal of retrospective reports. Psychological Bulletin. 1993;113:82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- 12.Brown GW, Craig TK, Harris TO, Handley RV. Parental maltreatment and adulthood cohabiting partnerships: a life-course study of adult chronic depression--4. J Affect Disord. 2008 Sep;110(1–2):115–25. doi: 10.1016/j.jad.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Carnelley KB, Pietromonaco PR, Jaffe K. Depression, working models of others, and relationship functioning. Journal of Personality and Social Psychology. 1994;66:127–140. doi: 10.1037//0022-3514.66.1.127. [DOI] [PubMed] [Google Scholar]
- 14.Cassano GB, Benvenuti A, Miniati M, Calugi S, Mula M, Maggi L, Rucci P, Fagiolini A, Perris F, Frank E. The factor structure of lifetime depressive spectrum in patients with unipolar depression. Journal of Affective Disorders. 2009;115 (1–2):87–99. doi: 10.1016/j.jad.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cervilla JA, Molina E, Rivera M, Torres-González F, Bellón JA, Moreno B, Luna JD, Lorente JA, Mayoral F, King M, Nazareth I, Gutiérrez B PREDICT Study Core Group. The risk for depression conferred by stressful life events is modified by variation at the serotonin transporter 5HTTLPR genotype: evidence from the Spanish PREDICT-Gene cohort. Molecular Psychiatry. 2007 Aug;12(8):748–755. doi: 10.1038/sj.mp.4001981. [DOI] [PubMed] [Google Scholar]
- 16.Chalk R, Gibbons A, Scarupa HJ. The multiple dimensions of child abuse and neglect: New insights into an old problem. Washington DC: Child Trends; 2002. [Google Scholar]
- 17.Cicchetti D, Rogosch FA, Toth SL. A developmental psychopathology perspective on depression in children and adolescents. In: Reynolds WM, Johnston HF, editors. Handbook of depression in children and adolescents. Issues in clinical child psychology. New York: Kluwer; 1994. pp. 123–141. [Google Scholar]
- 18.Cohen P, Brown J, Smailes E. Child abuse and neglect and the development of mental disorders in the general population. Development and Psychopathology. 2001;13:981–999. [PubMed] [Google Scholar]
- 19.Colman R, Widom C. Childhood abuse and neglect and adult intimate relationships: A prospective study. Child Abuse & Neglect. 2004;28:1133–1151. doi: 10.1016/j.chiabu.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Fagiolini A, Dell’Osso L, Pini S, Armani A, Bouanani S, Rucci P. Validity and reliability of a new instrument for assessing mood symptomatology: The Structured Clinical Interview for Mood Spectrum (SCI-MOODS) International Journal of Methods in Psychiatric Research. 1999;8:71–82. [Google Scholar]
- 21.Feiring C, Taska L, Lewis M. The role of shame and attributional style in children’s and adolescents’ adaptation to sexual abuse. Child Maltreatment. 1998;3:129–142. [Google Scholar]
- 22.Fogarty CT, Fredman L, Heeren TC, Liebschutz J. Synergistic effects of child abuse and intimate partner violence on depressive symptoms in women. Prev Med. 2008 May;46(5):463–9. doi: 10.1016/j.ypmed.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Frank E, Cassano GB, Rucci P, Fagiolini A, Maggi L, Kraemer HC, Kupfer DJ, Pollock B, Bies R, Nimgaonkar V, Pilkonis P, Shear MK, Grochocinski VJ, Scocco P, Buttenfield J, Forgione RN. Addressing the Challenges of a Cross-National Investigation: Lessons from the Pittsburgh-Pisa Study of Treatment-Relevant Phenotypes of Unipolar Depression. Clinical Trials. 2008;5(3):253–261. doi: 10.1177/1740774508091965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Donovan P, Hogan ME, Cronholm J, Tierney S. History of childhood maltreatment, depressogenic cognitive style, and episodes of depression in adulthood. Cognitive Therapy and Research. 2001;24:425–446. [Google Scholar]
- 25.Gibb BE, Wheeler R, Alloy LB, Abramson LY. Emotional, physical, and sexual maltreatment in childhood versus adolescence and personality dysfunction in young adulthood. Journal of Personality Disorders. 2001;15:505–511. doi: 10.1521/pedi.15.6.505.19194. [DOI] [PubMed] [Google Scholar]
- 26.Gladstone GL, Parker GB, Mitchell PB, Malhi GS, Wilhelm K, Austin MP. Implications of childhood trauma for depressed women: an analysis of pathways from childhood sexual abuse to deliberate self-harm and revictimization. American Journal of Psychiatry. 2004 Aug;161(8):1417–1425. doi: 10.1176/appi.ajp.161.8.1417. [DOI] [PubMed] [Google Scholar]
- 27.Grover KE, Tyrka AR, Carpenter LL, Gagne GG, Feijo Mello AA, Feijo Mello M, Price LH. The Relationship between Childhood abuse and adult personality disorder symptoms. Journal of Personality Disorders. 2007;21:442–447. doi: 10.1521/pedi.2007.21.4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamilton M. A rating scale for depression. Journal of Neurology Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammen C. The generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- 30.Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- 31.Hankin BL, Kassel JD, Abela JRZ. Adult attachment styles and specificity of emotional distress: Prospective investigations of cognitive risk and interpersonal stress generation as mediating mechanisms. Personality and Social Psychology Bulletin. 2005;31:136–151. doi: 10.1177/0146167204271324. [DOI] [PubMed] [Google Scholar]
- 32.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45 (2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 33.Ingram RE, Miranda J, Segal ZV. Cognitive vulnerability to depression. New York: Guilford Press; 1998. [Google Scholar]
- 34.Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Archives of General Psychiatry. 1999;56:600–606. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- 35.Johnson JG, Cohen P, Chen H, Kasen S, Brook JS. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Archives of General Psychiatry. 2006;63:579–587. doi: 10.1001/archpsyc.63.5.579. [DOI] [PubMed] [Google Scholar]
- 36.Joiner T, Coyne JC. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 37.Kendall-Tackett K, Becker-Blease K. The importance of retrospective findings in child maltreatment research. Child Abuse & Neglect. 2004;28:723–727. doi: 10.1016/j.chiabu.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 38.Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Kim YH, Yoon JS. Interactions between life stressors and susceptibility genes (5 HTTLPR and BDNF) on depression in Korean elders. Biological Psychiatry. 2007;62(5):423–428. doi: 10.1016/j.biopsych.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 39.Klerman GL, Weissmann MM. Interpersonal psychotherapy (IPT) and drugs in the treatment of depression. Pharmacopsychiatry. 1987;20:3–7. doi: 10.1055/s-2007-1017067. [DOI] [PubMed] [Google Scholar]
- 40.Levitan RD, Parikh SV, Lesage AD, Hegadoren KM, Adams M, Kennedy SH, Goering PN. Major depression in individuals with a history of childhood physical or sexual abuse: Relationship to neurovegetative features, mania, and gender. American Journal of Psychiatry. 1998;155:1746–1752. doi: 10.1176/ajp.155.12.1746. [DOI] [PubMed] [Google Scholar]
- 41.McHolm AE, MacMillan HL, Jamieson E. The relationship between childhood physical abuse and suicidality among depressed women: results from a community sample. American Journal of Psychiatry. 2003 May;160(5):933–938. doi: 10.1176/appi.ajp.160.5.933. [DOI] [PubMed] [Google Scholar]
- 42.McNally RJ, Perlman CA, Ristuccia CS, Clancy SA. Clinical characteristics of adults reporting repressed, recovered, or continuous memories of childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2006;74:237–242. doi: 10.1037/0022-006X.74.2.237. [DOI] [PubMed] [Google Scholar]
- 43.Nemeroff CB. Early life adversity, CRF dysregulation, and vulnerability to mood and anxiety disorders. Psychopharmacology Bulletin. 2004;38 (Suppl 1):14–20. [PubMed] [Google Scholar]
- 44.Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Comprehensive Psychiatry. 2000 Nov-Dec;41(6):469–478. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- 45.Palmer RL. Effects of childhood sexual abuse on adult mental health. British Journal of Hospital Medicine. 1992;48:9–10. [PubMed] [Google Scholar]
- 46.Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, Egan MF, Mattay VS, Hariri AR, Weinberger DR. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nature Neuroscience. 2005;8:828–834. doi: 10.1038/nn1463. [DOI] [PubMed] [Google Scholar]
- 47.Roberts JE, Gotlib IH, Kassel JD. Adult attachment security and symptoms of depression: The mediating roles of dysfunctional attitudes and low self-esteem. Journal of Personality and Social Psychology. 1996;70:310–320. doi: 10.1037//0022-3514.70.2.310. [DOI] [PubMed] [Google Scholar]
- 48.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB. The 16-item Quick Inventory of Depressive Symptomatology (QIDS) Clinician Rating (QIDS-C) and Self-Report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 49.Stein M, Schork N, Gelernter J. Gene-by-environment (serotonin transporter and childhood maltreatment) interaction for anxiety sensitivity, an intermediate phenotype for anxiety disorders. Neuropsychopharmacology. 2008 Jan;33(2):312–319. doi: 10.1038/sj.npp.1301422. [DOI] [PubMed] [Google Scholar]
- 50.Swett C, Jr, Surrey J, Cohen C. Sexual and physical abuse histories and psychiatric symptoms among male psychiatric outpatients. American Journal of Psychiatry. 1990;147:632–636. doi: 10.1176/ajp.147.5.632. [DOI] [PubMed] [Google Scholar]
- 51.Toth SL, Manly JT, Cicchetti D. Child maltreatment and vulnerability to depression. Development and Psychopathology. 1992;4:97–112. [Google Scholar]
- 52.Trivedi MH, Rush AJ, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, Key T, Biggs MM, Shores-Wilson K, Witte B, Suppes T, Miller AL, Altshuler KZ, Shon SP. Clinical results for patients with major depressive disorder in the Texas Medication Algorithm Project. Archives of General Psychiatry. 2004 Jul;61(7):669–680. doi: 10.1001/archpsyc.61.7.669. [DOI] [PubMed] [Google Scholar]
- 53.Wichers MC, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, Vlietinck R, Delespaul P, van Os J. Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: a momentary assessment twin study. Acta Psychiatrica Scandinavica. 2007;115(6):451–457. doi: 10.1111/j.1600-0447.2006.00924.x. [DOI] [PubMed] [Google Scholar]