Abstract
Objective
The PROSPECT Study evaluated the impact of a care management intervention on suicidal ideation and depression in older primary care patients. This is the first report of outcomes over a 2-year period.
Method
The subjects (N=599) were older (>=60 years) patients with major or minor depression selected after screening 9,072 randomly identified patients of 20 primary care practices randomly assigned to the PROSPECT intervention or usual care. The intervention consisted of services of 15 trained care managers, who offered algorithm-based recommendations to physicians and helped patients with treatment adherence over 24 months.
Results
Intervention patients had a higher likelihood to receive antidepressants and or psychotherapy (84.9–89% vs. 49–59%) and a 2.2 times greater decline in suicidal ideation than usual care patients over 24 months. Treatment response occurred earlier in intervention patients and continued to increase from the 18th to the 24th month, while there was no appreciable increase in usual care patients during the same period. Among patients with major depression, a greater number achieved remission in the intervention than the usual care group at 4 (26.6 vs. 15.2%), 8 (36% vs. 22.5%), and 24 (45.4% vs. 31.5%) months. Patients with minor depression had favorable outcomes regardless of treatment assignment.
Conclusions
Sustained collaborative care maintains high utilization of antidepressant treatment, reduces suicidal ideation, and improves the outcomes of major depression over two years. These observations suggest that sustained collaborative care increases depression-free days.
Keywords: Geriatric psychiatry, Outcome Studies, Suicide, Mood Disorders-Unipolar
INTRODUCTION
The Institute of Medicine has identified prevention of suicide as a national imperative 1. Despite recent decline in suicides of persons older than 64 years, the suicide rate (14.3/100,000) of older adults remains higher than that of the general population 2. Suicidal ideation and depression are two major risk factors for late-life suicide and targets for prevention 3.
Primary care is a strategic setting for treating geriatric depression and for preventing suicide. Major depression has been identified in 6–9% of primary care patients while more than 17% have less severe depressive symptoms 4. Moreover, 18% of primary care patients with major depression have suicidal ideation 5.
Care management models offered over one year increase utilization of antidepressant treatment and improve outcomes of depression in primary care patients 6,7. Depression in old age is a chronic, relapsing illness, and one-year data alone are insufficient for understanding the impact of care management.
This report presents outcomes of a 2-year intervention by the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT). An early analysis showed greater decline in suicidal ideation and depressive symptomatology and higher response and remission rates in depressed patients receiving the PROSPECT intervention than usual care 6. However, by 12 months, the advantages of intervention were no longer retained.
This paper focuses on PROSPECT’s primary outcomes during the second year of treatment. It tests the hypotheses that depressed patients treated in practices offering the PROSPECT intervention have: 1) greater reduction in suicidal ideation; and 2) better outcomes of depression, i.e. greater decline in depressive symptomatology and higher rates of treatment response and remission than patients of usual care practices over 2 years.
METHOD
Subjects
The study was conducted in 20 primary care practices of urban, suburban, and rural areas. Its procedures were approved by the institutional review boards of participating centers (Cornell, University of Pennsylvania, University of Pittsburgh). The study used a two-stage random sampling design to produce an age stratified (60–74, >74 years) sample of patients with pending appointments with their physicians 6.
Randomization
Ten pairs of practices were formed, each consisting of practices with similar academic affiliation, size, setting, patients, and region. The practices of each pair were randomly assigned to intervention or usual care. Randomization by practice was selected to minimize “contamination” of intervention procedures to usual care.
Intervention
The intervention was offered for 24 months to patients who presented at baseline with a major depression based on DSM-IV criteria, or a minor depression defined as three to four depressive symptoms, a 24-item Hamilton Depression Rating Scale (HDRS) 8 score of 10 or higher, and a duration of at least one month. It consisted of a composite intervention (further described elsewhere 6) implemented by 15 practice-based care managers guided by a treatment algorithm. The care managers were social workers, nurses, and psychologists trained in PROSPECT procedures. They helped physicians to recognize depression, offered algorithm-based recommendations, monitored depressive symptoms and side effects, and provided follow-up over 24 months. The care managers also offered interpersonal psychotherapy (IPT) to patients who refused medication. They saw patients at the practices’ offices but made house calls to patients unable to travel and addressed patient concerns related to treatment adherence.
The algorithm was based on Agency for Health Care Policy and Research (AHCPR) Practice Guidelines modified for use in elderly patients (described elsewhere) 9. The first step of the algorithm was use of citalopram at the target daily dose of 30 mg. to avoid undertreatment. Physicians had the option to prescribe other antidepressants or refer subjects for psychotherapy other than IPT. Research funds covered the cost of citalopram and IPT only. Psychiatrist investigators provided weekly group supervision to care managers and were available by telephone.
Usual Care
Physicians in usual care practices had no assistance but received videotaped and printed material on geriatric depression and its treatment. They were also informed by letter of the patients’ depression diagnosis and suicidal ideation when present.
Systematic Assessment
Diagnoses were based on the Structured Clinical Interview for DSM-IV (SCID-IV) 10. Severity of depression was assessed with the HDRS and cognitive impairment with the Mini Mental State Examination (MMSE) 11. Suicidal ideation was rated with the Scale for Suicide Ideation (SSI) 12. The SSI has sound psychometric properties in younger psychiatric outpatients 12 and has yielded a factor structure for older adults similar to that for younger adults 13. The SSI scores were skewed; 80–90% of patients had a score of 0 (no suicidal ideation) at any assessment point. For this reason, the SSI was treated as a dichotomous variable. We also created dichotomous variables of the three SSI factors 12. The “passive suicidal desire” factor consists of items reflecting precautions to save life, self confidence in ability to commit suicide, and hesitance to reveal suicidal thoughts. The “active suicidal desire” factor consists of the following items: Wish to live, wish to die, reasons for living/dying, wish to make suicide attempt, duration of suicide ideation/wish, frequency of suicide wish, attitude toward suicidal ideation/wish, deterrents to active attempt, reason for contemplating attempt, and expectancy/anticipation of actual attempt. The “preparation” factor consists of items reflecting consideration of method, availability of method, and actualization of attempt. Each subject was assigned to a single SSI factor according to severity based on the following rule. Subjects endorsing a Preparation item were assigned to the Preparation factor regardless of endorsement of items of other factors. Subjects endorsing an Active Suicidal Desire item, but not a Preparation item, were assigned to the Active Suicide Desire factor. Finally, subjects endorsing a Passive Suicidal Desire item, but not a Preparation or Active Suicidal Desire item, were assigned to the Passive Suicide Desire Factor.
Randomization by practice prevented blinded assessment. Nonetheless, raters did not participate in the patients’ treatment and were held to high standards of inter-rater reliability (reported elsewhere 6). Moreover, assessment data were not made available to care managers or clinicians except as required for safety. Patients had in-person interviews at 12 and 24 months and telephone assessments at 4, 8, and 18 months after entry.
Data Analysis
Tests and estimates of intent-to-treat (ITT) differences for outcomes were based on longitudinal models with random effects for clustering by patient, practice, and practice pairs. The ITT sample included all patients with a baseline assessment regardless of treatment and drop-out status during follow-up. Clustering by practice and pairs of practices was negligible and did not impact the analysis. The longitudinal random effects models included main effect and interaction terms that represented ITT contrasts at each of the 4, 8, 12, 18, and 24-month points. The “omnibus” statistic tests for significant ITT contrasts at any one follow-up assessments and is a time by group interaction 14. For continuous outcomes, analyses were based on SAS PROC MIXED. Both Proc NLMIXED and the GLIMMIX macro in SAS were used to employ two- and three-level random effects models, respectively, for binary outcomes. Given group difference in baseline suicidal ideation (20 vs. 31%; P=.02), this variable was controlled for in all ITT analyses. Such adjustment is appropriate under the random effects models. Moreover, all ITT analyses, except that of the longitudinal suicide ideation outcome, were robust to such an adjustment. Results were also robust with respect to random effects assumptions 15. Additional robustness existed in intervention differences in missed assessments and drop-out, without making imputation assumptions such as last-observation-carried forward 16.
RESULTS
Participants’ Characteristics, Dropout and Missed Assessments
The participants’ demographic and clinical characteristics were reported elsewhere 6. Briefly, 71.6% of participants were women, 30.1% were aged 75 years or older, 32.4% belonged to minorities, 3.8% met poverty status, 36.9% were married, and 56.5% lived alone. Their average HDRS score was 18.1 and their MMSE was 27.4. There were no significant differences in demographic or clinical characteristics between the intervention and usual care groups except in suicidal ideation.
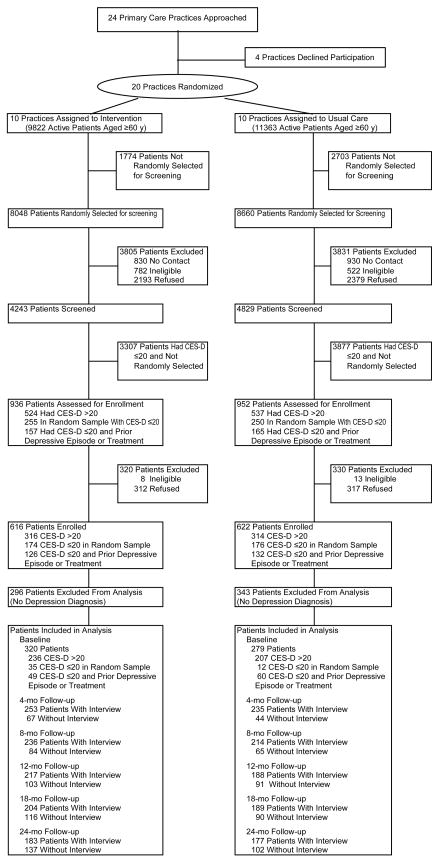
At 24 months, 43% (137/320) of intervention patients and 37% (102/279) of usual care patients failed to have a research assessment (Figure 1). The influence of differences in dropout was assessed by comparing results from our analysis to results under the shared parameter model, which adjusts for such differences. Group assignment did not differ by more than 5%, and P values were not significant. The proportion of missed assessments in the usual care group exceeded that in the intervention group for all assessments with the difference not exceeding 6% points for any assessment. There were no statistically significant differences among intervention and usual care patients who had the 24-month assessment.
Figure 1. Flowchart of Progress Through the Phases of the PROSPECT Trial.
Abbreviation: CES-D: Center for Epidemiologic Studies Depression Scale
Treatment
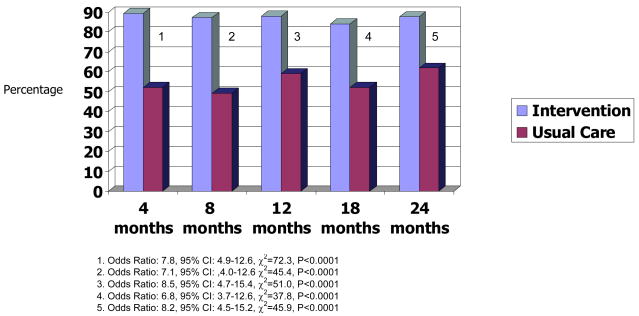
More intervention (84.9–89%) than usual care patients (49–59%) received antidepressant treatment at 4, 8, 12, 18 and 24 months (Figure 2), including antidepressants (p<0.001) and psychotherapy (p<0.001). There were no significant group differences in combination therapy received at 4, 8, 18 and 24 months, but fewer intervention patients received combined treatment at 12 months (Odds Ratio: 0.25, CI: 0.07–0.89, χ2=4.62, p<0.03).
Figure 2.
Percentage of Depressed Older Primary Care Patients Who Received Treatment for Depression, by Assessment Point
Suicidal Ideation, Attempts, Suicide, and Mortality
In the whole group, intervention patients were more likely to report suicidal ideation (endorse any SSI item) at baseline than usual care patients [29.7% (95/320) vs. 20.4% (57/279), P<.01]. By 4 months, the rates of overall suicidal ideation declined more in intervention than in usual care patients [12.8%: from 29.7% (95/320) to 16.9% (42/248) vs. 3.0%: from 20.4% (57/279) to 17.4% (40/229), P=0.02]. By 24 months, there was a 2.2 times greater decline in raw rates of suicidal ideation in intervention compared to usual care patients [Intervention: 18.3% change: from 29.7% (95/320) to 11.4% (20/176) vs. Usual Care: 8.3% change: from 20.4% (57/279) to 12.1% (21/173); P=0.12].
Ninety percent of patients with positive SSI scores at any point over 24 months endorsed only items of the SSI “active suicide desire” factor. For this reason, further analysis focused on the “active suicide desire” factor (Table 1). Adjusting for baseline difference, the omnibus trend testing ITT differences in change of “active suicidal desire” over time showed a trend favoring the intervention in the whole depressed group (P=0.09) and a significant difference among patients with major depression (P=0.04). Intervention patients with major depression had lower “active suicidal desire” than usual care patients at 4, 8, and 24 months. The differences among patients with minor depression were not significant (P=0.86). Due to low frequency, combined rates are presented for the other two SSI factors, “Preparation” and “Passive suicidal desire” (Table 1). Insufficient number of subjects with either of these two SSI factors prevented meaningful statistical analysis.
Table 1.
Rates of Suicidal Ideation Over Time
| No. with Suicidal Ideation/No. Analyzed (%)* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual Care | Odds Ratio | P Value | Omnibus Test** | ||||||
| All depressed patients | N | % | N | % | OR | 95%CI | χ2=9.6 | df=5 | P= .09 | |
| Baseline Active+ | 89/320 | 27.5 | 52/279 | 18.6 | -- | -- | -- | |||
| Preparation++ | 6/320 | 1.9 | 5/279 | 1.8 | -- | -- | -- | |||
| 4 mo Active | 40/248 | 16.1 | 36/229 | 15.7 | 2.2 | 1.0–4.9 | .04 | |||
| Preparation | 2/248 | 0.8 | 4/229 | 1.7 | -- | -- | -- | |||
| 8 mo Active | 40/233 | 17.2 | 39/210 | 18.6 | 3.1 | 1.4–6.8 | .005 | |||
| Preparation | 1/233 | 0.4 | 1/210 | 0.5 | -- | -- | -- | |||
| 12 mo Active | 30/213 | 14.1 | 23/186 | 12.4 | 1.8 | 0.8–4.3 | .18 | |||
| Preparation | 1/213 | 0.5 | 2/186 | 1.1 | -- | -- | -- | |||
| 18 mo Active | 24/200 | 12.0 | 18/181 | 9.9 | 1.5 | 0.6–3.6 | .43 | |||
| Preparation | 1/200 | 0.5 | 0/181 | 0 | -- | -- | -- | |||
| 24 mo Active | 20/176 | 11.4 | 20/173 | 11.6 | 2.1 | 0.8–5.5 | .11 | |||
| Preparation | 0/176 | 0 | 1/173 | 0.6 | -- | -- | -- | |||
| Major Depression | χ2= 11.4 | df=5 | P= .04 | |||||||
| Baseline Active | 74/214 | 34.6 | 43/182 | 23.6 | -- | -- | -- | |||
| Preparation | 5/214 | 2.3 | 5/182 | 2.7 | -- | -- | -- | |||
| 4 mo Active | 34/170 | 20.0 | 28/145 | 19.3 | 2.5 | 1.1–6.2 | .05 | |||
| Preparation | 1/170 | 0.6 | 4/145 | 2.8 | -- | -- | -- | |||
| 8 mo Active | 33/160 | 20.6 | 34/135 | 25.2 | 4.2 | 1.7–10.5 | .002 | |||
| Preparation | 1/160 | 0.6 | 1/135 | 0.7 | -- | -- | -- | |||
| 12 mo Active | 23/146 | 15.8 | 17/117 | 14.5 | 2.2 | 0.8–5.9 | .14 | |||
| Preparation | 0/146 | 0 | 1/117 | 0.9 | -- | -- | -- | |||
| 18 mo Active | 19/134 | 14.2 | 16/113 | 14.2 | 2.1 | 0.7–5.9 | .17 | |||
| Preparation | 0/134 | 0 | 0/113 | 0 | -- | -- | -- | |||
| 24 mo Active | 14/124 | 11.3 | 16/109 | 14.7 | 3.2 | 1.1–9.5 | .04 | |||
| Preparation | 0/124 | 0 | 1/109 | 0.9 | -- | -- | -- | |||
| Clinically significant minor depression only | χ2= 1.9 | df=5 | P= .86 | |||||||
| Baseline Active | 15/106 | 14.2 | 9/97 | 9.3 | -- | -- | -- | |||
| Preparation | 1/106 | 0.9 | 0/97 | 0 | -- | -- | -- | |||
| 4 mo Active | 6/78 | 7.7 | 8/84 | 9.5 | 1.8 | 0.4–8.9 | .47 | |||
| Preparation | 1/78 | 1.3 | 0/84 | 0 | -- | -- | -- | |||
| 8 mo Active | 7/73 | 9.6 | 5/75 | 6.7 | 1.2 | 0.2–6.6 | .81 | |||
| Preparation | 0/73 | 0 | 0/75 | 0 | -- | -- | -- | |||
| 12 mo Active | 7/67 | 10.4 | 6/69 | 8.7 | 1.1 | 0.2–5.7 | .90 | |||
| Preparation | 1/67 | 1.5 | 1/69 | 1.4 | -- | -- | -- | |||
| 18 mo Active | 5/66 | 7.6 | 2/68 | 2.9 | 0.5 | 0.1–3.7 | .46 | |||
| Preparation | 1/66 | 1.5 | 0/68 | 0 | -- | -- | -- | |||
| 24 mo Active | 6/52 | 11.5 | 4/64 | 6.2 | 0.8 | 0.1–4.4 | .74 | |||
| Preparation | 0/52 | 0 | 0/64 | 0 | -- | -- | -- | |||
Abbreviation: CI: Confidence Interval
The discrepancies between 4, 8, 12, 18, and 24-month denominators and Figure 1 are due to incomplete or missing data on the Scale for Suicidal Ideation among some participants who were interviewed at these times.
Omnibus Tests were conducted in order to detect group differences in longitudinal change of Active Suicidal Desire from baseline. Omnibus Tests and Odds Ratios were not computed for Preparation because of its infrequent occurrence.
Active: “Active Suicidal Desire” factor of the SSI
Preparation: “Preparation” factor plus “Passive Suicidal Desire” factor of the SSI
Of all patients with positive responses on the SSI, the most frequently endorsed items were item 2 (31%; wish to die), item 3 (29%; reasons for living/dying), and item 1 (15%; wish to live). While they fall within the “active suicide desire” factor, clinicians may classify these items as “passive suicidal ideation”. The next most frequently endorsed items were item 11 (3.2%; reason for contemplating attempt), 7 (3%; frequency of suicide wish), 4 (2.7%; wish to make suicide attempt), and 12 (2.4%; consideration of method). In each remaining SSI item, endorsement did not exceed 2%.
During the study, two patients attempted suicide in the intervention arm, and three patients in the usual care arm. One of the attempted suicides in the intervention arm resulted in death. Further information on mortality was obtained through death certificates over a period of 5 years after entry to the study. During this time, 60 (44.7/1000 person years) patients of the intervention arm and 55 (49.7/1000person years) patients of the usual care arm died 17. It is possible that some of the deaths after 24 months were due to suicide that was not recorded in death certificates.
Course of Depression
Severity of Depression
The decrease in HDRS from baseline was greater in the intervention than in the usual care group at all assessment points, and the overall omnibus test indicated significance (Table 2). Greater decline in HDRS was also noted in patients with major depression at each assessment point and overall. There were no significant differences in HDRS decline between intervention and usual care patients with minor depression.
Table 2.
Depression Severity Over Time
| Mean (SD) HDRS Score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual Care | Group Difference in Change from Baseline | P Value | Omnibus Test* | ||||||
| All depressed patients | Mean | SD | Mean | SD | Group difference | 95%CI | χ2= 33.6 | df=5 | P< .001 | |
| Baseline | 18.61 | 6.12 | 17.51 | 5.82 | -- | .73 | ||||
| 4 mo | 11.24 | 7.51 | 13.57 | 8.42 | −3.5 | −4.7 to −2.3 | <.001 | |||
| 8 mo | 10.45 | 7.39 | 11.38 | 7.49 | −2.1 | −3.4 to −0.9 | <.001 | |||
| 12 mo | 9.77 | 7.28 | 10.35 | 6.78 | −1.8 | −3.1 to −0.5 | .006 | |||
| 18 mo | 9.73 | 7.94 | 9.76 | 6.82 | −1.3 | −2.6 to 0.04 | .06 | |||
| 24 mo | 8.81 | 7.51 | 9.28 | 6.54 | −1.9 | −3.2 to −0.5 | .007 | |||
| Major Depression | χ2= 33.2 | df=5 | P< .001 | |||||||
| Baseline | 21.05 | 5.74 | 19.72 | 5.54 | -- | .82 | ||||
| 4 mo | 12.59 | 7.74 | 15.87 | 8.40 | −4.6 | −6.1 to −3.0 | <.001 | |||
| 8 mo | 11.69 | 7.93 | 12.85 | 7.27 | −2.4 | −4.0 to −0.8 | .004 | |||
| 12 mo | 10.42 | 7.62 | 11.21 | 7.11 | −1.9 | −3.6 to −0.3 | .02 | |||
| 18 mo | 10.46 | 8.21 | 11.15 | 7.21 | −1.9 | −3.6 to −0.2 | .03 | |||
| 24 mo | 9.53 | 7.84 | 10.43 | 6.70 | −2.2 | −3.9 to −0.5 | .01 | |||
| Clinically significant minor depression only | χ2= 5.2 | df=5 | P= .39 | |||||||
| Baseline | 13.69 | 3.23 | 13.36 | 3.70 | -- | .76 | ||||
| 4 mo | 8.34 | 6.07 | 9.44 | 6.76 | −1.4 | −3.1 to 0.4 | .14 | |||
| 8 mo | 7.81 | 5.23 | 8.72 | 7.20 | −1.5 | −3.3 to 0.4 | .11 | |||
| 12 mo | 8.39 | 6.33 | 8.86 | 5.91 | −1.1 | −3.0 to .8 | .24 | |||
| 18 mo | 8.25 | 7.19 | 7.45 | 5.41 | 0.2 | −1.7 to 2.1 | .86 | |||
| 24 mo | 7.03 | 6.36 | 7.34 | 5.80 | −.7 | −2.7 to 1.3 | .51 | |||
Abbreviations: CI: Confidence interval; HDRS: Hamilton Depression Rating Scale
P values calculated with the Wald statistic adjusting for baseline ideation and HDRS scores
Treatment Response
Response was defined as a reduction of baseline HDRS score by 50% or more. In the whole group, intervention patients had higher overall response rates than usual care patients (omnibus trend χ2(5)= 17.3, P<.004) and at 4, 8, 12, and 24 months. From 18 to 24 months, 7.3 times more intervention patients (9.4%, from 52.9% to 62.3%) responded to treatment than usual care patients (1.3%, from 45% to 46.3%). At 24 months, 35% more intervention patients had met criteria for response of depression than usual care patients. The number needed to treat (NNT) for response rates at 24 months is 6, i.e. the intervention yielded one additional response for every 6th patient. In the subgroup with major depression, intervention patients had higher overall response rates than usual care patients (omnibus trend χ2(5)= 17.3, P<.004) and at 4 (OR: 3.8, 95% CI: 1.8–8.2, p<0.001), 8 (OR: 2.9, 95% CI: 1.4–6.2, p<0.005), and 24 months (OR: 4.9, 95% CI=2.2.–11.2, P<0.001). There was a 9.4% increase in response rate from 18 to 24 months in patients with major depression of intervention practices (from 54.4% to 63.8%) but a 3.2% (from 42.4% to 39.6%) decline in patients of usual care practices. The NNT for response rates at 24 months was 4 patients. There were no significant differences in response rates between intervention and usual care patients with minor depression.
Remission
Remission was defined as an HDRS score lower than 7. In the whole depressed group, intervention had higher remission rates than usual care at 4 and 8 months (Table 3). Usual care remission rates approximated those of intervention at 12, 18 and 24 months. In the major depression group, intervention led to higher remission rates at 4, 8, and again at 24 months but there were no significant differences at 12 and 18 months. At 24 months, 1.44 times more intervention patients had achieved remission than usual care patients (45.4% vs. 31.5%). The NNT showed that the intervention yielded one additional remission for every 7th patient. There were no differences in remission rates between intervention and usual care patients with minor depression.
Table 3.
Depression Remission (HDRS<7) Over Time
| No. with HDRS Score <7/No. Analyzed (%)* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual Care | Odds Ratio | P Value | Omnibus Test* | ||||||
| All depressed patients | N | % | N | % | OR | 95%CI | χ2= 7.6 | df=5 | P< .18 | |
| 4 mo | 82/253 | 32.4 | 59/235 | 25.1 | 1.9 | 1.0–3.6 | .05 | |||
| 8 mo | 97/236 | 41.1 | 68/215 | 31.8 | 2.1 | 1.1–4.0 | .02 | |||
| 12 mo | 87/217 | 40.1 | 62/188 | 33.1 | 1.8 | 0.9–3.6 | .07 | |||
| 18 mo | 89/204 | 43.6 | 72/189 | 38.1 | 1.6 | 0.8–3.1 | .19 | |||
| 24 mo | 91/183 | 49.7 | 75/177 | 42.4 | 1.8 | 0.9–3.5 | .10 | |||
| Major Depression | χ2= 12.0 | df=5 | P< .03 | |||||||
| 4 mo | 46/173 | 26.6 | 23/151 | 15.2 | 3.1 | 1.3–7.5 | .01 | |||
| 8 mo | 58/161 | 36.0 | 31/138 | 22.5 | 2.9 | 1.2–6.9 | .01 | |||
| 12 mo | 53/148 | 35.8 | 38/119 | 31.9 | 1.3 | 0.6–3.1 | .55 | |||
| 18 mo | 55/136 | 40.4 | 36/118 | 30.5 | 2.0 | 0.8–4.8 | .12 | |||
| 24 mo | 59/130 | 45.4 | 35/111 | 31.5 | 2.9 | 1.2–7.0 | .02 | |||
| Clinically significant minor depression only | χ2= 4.5 | df=5 | P= .49 | |||||||
| 4 mo | 36/80 | 45.0 | 36/84 | 42.9 | 1.2 | 0.4–3.0 | .76 | |||
| 8 mo | 39/75 | 52.0 | 37/76 | 48.7 | 1.4 | 0.5–3.7 | .54 | |||
| 12 mo | 34/69 | 49.3 | 24/69 | 34.8 | 2.7 | 1.0–7.8 | .06 | |||
| 18 mo | 34/68 | 50.0 | 36/71 | 50.7 | 1.0 | 0.4–2.8 | .98 | |||
| 24 mo | 32/53 | 60.4 | 40/66 | 60.6 | 0.9 | 0.3–2.8 | .86 | |||
Abbreviations: CI: Confidence interval; HDRS: Hamilton Depression Rating Scale
The discrepancies between 4, 8, 12, 18, and 24-month denominators and Figure 1 are due to incomplete or missing data on the Scale for Suicidal Ideation among some participants who were interviewed at these times.
Differences with respect to longitudinal change since baseline.
DISCUSSION
The principal finding of this study is that depressed patients of practices randomized to the PROSPECT intervention had a higher likelihood to receive antidepressant treatment, a greater decline in suicidal ideation, lower depressive symptomatology, and a higher rate of response over 24 months than usual care patients. At any assessment point, 84.9–89% of intervention patients received antidepressants and/or psychotherapy while only 49–59% of usual care patients were treated for depression. The intervention was most effective in reducing suicidal ideation among patients with major depression. The decline was sharpest in the first 4 months and remained low up to 24 months. Similarly, severity of depression remained lower in intervention than usual care patients throughout the 24 months. Among patients with major depression, a greater number achieved remission in the intervention than the usual care group at 4, 8, and 24 months. The intervention had no advantages among patients with minor depression.
To our knowledge, this is the first study of 24-month depression care management focusing on suicidal ideation and depressive psychopathology in older primary care patients. Its findings are consistent with observations in mixed aged 18 primary care patients, including an intervention of 24-months duration 19. In geriatric patients, the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) Study provided access up to 12 months to a depression care manager 20. Primary care patients receiving the IMPACT intervention were more likely to receive antidepressant treatment than usual care patients and had better depression outcomes. The advantage over usual care was retained 12 months after the end of the intervention, although there was a decline of response and remission rates from 12 to 24 months 21. In contrast, with continuing depression care management the response and remission rates in the intervention arm of the PROSPECT Study remained high or increased.
In most subjects, suicidal ideation was passive as often is the case in depressed primary care patients 22. Even passive suicidal ideation requires attention. Depressed elders with passive suicidal ideation are more likely to have history of suicide attempts, higher scores of hopelessness 23, slower treatment response, and lower rates of response than non-suicidal elders with major depression 24. Passive suicidal ideation has a stronger association with medical comorbidity and service utilization than active suicidal ideation or no suicidal ideation 5. Finally, 35% of patients with suicidal ideation change ideator status during the index episode; passive ideators become active or the reverse 23. Change over time in passive suicidal ideation requires further research to identify treatment responsive and treatment resistant components that may further focus suicide prevention interventions for depressed older primary care patients.
There was one suicide and one suicide attempt in the intervention group, and three suicide attempts in the usual care group. These numbers do not allow statistical study of the relationship of suicidal ideation to suicide or attempts, but underscore the challenge of reducing the risk of suicide in primary care settings. The relationship of reduction in the rate of suicidal ideation, and especially passive or death ideation, to suicide remains to be determined.
Over 24 months, 49.7% of depressed intervention patients achieved remission (HDRS<7). Remission, defined as an almost asymptomatic state, is the optimal outcome because it is associated with low relapse rate and high function 25. Randomized acute antidepressant trials show that 30–40% of patients achieve remission 26. A controlled maintenance treatment trial showed that 65% of elderly patients with major depression remained in remission over 24 months while treated with paroxetine and monthly psychotherapy 27. The remission rate of the PROSPECT intervention was somewhat lower than this figure. Nonetheless, demonstrating that a care management intervention can maintain almost half of depressed primary care patients in remission is evidence of a meaningful level of effectiveness.
While antidepressant prescriptions have been rising, many depressed primary care patients receive no antidepressant treatment 19. Poor treatment adherence further compromises their care 28. In this study, more than 84% of intervention patients received antidepressants or psychotherapy throughout the study, while only 49–59% of usual care patients received any antidepressant treatment.
Depression almost doubles the risk for death in community samples 29. Patients of PROSPECT intervention practices with major depression had lower mortality than those in usual care practices (adjusted hazard ratio: 0.55, 95% CI: 0.36–0.84) over a 52.8 month median follow-up 17, but there were no differences in mortality among patients with minor depression. This observation is consistent with reduced all-cause mortality reported in patients receiving antidepressants over 40 months in the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) study 30.
The benefits of the PROSPECT intervention on suicidal ideation and on depression were limited to patients with major depression. Patients with minor depression had overall favorable outcomes regardless of treatment assignment. At 24 months, only 6.2% of usual care patients had any suicidal ideation and 60.6% had achieved remission of minor depression. Given limited resources, patients with major depression should be the target of a care management intervention.
Limitations of the study include the use of SSI as the sole method for ascertaining suicidal ideation, the lack of information on discrete medical problems of participants, and on specific antidepressant treatments received by each group. Randomization at the practice level compromised the ability to blind raters. Covering the cost of citalopram and IPT limits study of cost as a barrier to treatment. Finally, attrition was relatively high, perhaps because the study enrolled a probability sample consisting of subjects less interested in study participation than help-seeking patients. Nonetheless, probability sampling permits safer generalization of findings. Moreover, the baseline clinical characteristics of those assessed at 24 months were similar to those of the sample initially entered. Finally, taking drop-out into consideration did not influence differences between treatment groups significantly. Another limitation is that suicidal ideation was assessed at single points in time although suicide thoughts wax and wane.
Strengths of this study include its random sampling and a sensitive screening approach designed to identify most patients with depression. These procedures allow generalization of findings to whole practices. Furthermore, the practices were heterogeneous and consisted of small, large, inner city, rural, academic, and privately owned practices. Finally, patients with suicidal ideation, cognitive impairment, and medical burden were included in the sample. Therefore, these findings may be relevant to real-world practices.
Primary care is a strategic point from which to fight suicidality and depression since most elderly patients suffering from these syndromes are treated by primary care physicians. Sustained collaborative care maintains high utilization of antidepressant treatment, reduces suicidal ideation, and increases response and remission rates of major depression over a period of two years. Rising response and remission rates between the 18th and the 24th month underscore the value of long term care. These observations suggest that sustained collaborative care increases both depression-free days and perhaps longevity.
Acknowledgments
Funding/Support: PROSPECT was a collaborative research study funded by the National Institute of Mental Health. The 3 groups included the Advanced Centers for Intervention and Services Research of: Cornell University (PROSPECT Coordinating Center; PI: George S. Alexopoulos, M.D. and Co-PIs: Martha L. Bruce, Ph.D., M.P.H.; Herbert C. Schulberg, Ph.D.; R01 MH59366, P30 MH68638); University of Pennsylvania (PI: Ira Katz, M.D., Ph.D., and Co-PIs: Thomas Ten Have, Ph.D., Gregory K. Brown, Ph.D.; R01 MH59380, P30 MH52129); and University of Pittsburgh (PI: Charles F. Reynolds III, M.D., and Co-PI: Benoit H. Mulsant, M.D.; R01 MH59381, P30 MH52247). PROSPECT was supported by NIMH grants RO1 MH59366, R01 MH059380, RO37 MH51842, and RO1 MH59318, P30 MH68638, P30 MH52247, P30 MH066270; the Hartford Foundation; and Forest Pharmaceuticals, Inc.
Role of the Sponsor: The sponsors provided financial support for the study only and had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or in preparation, review, and approval of the manuscript.
Grant Support: NIMH grants RO1 MH59366, R01 MH059380, RO37 MH51842, and RO1 MH59318, P30 MH68638, P30 MH52247, P30 MH066270; the Hartford Foundation; and Forest Pharmaceuticals, Inc.
Footnotes
Trial Registration: clinicaltrials.gov Identifier NCT00279682
Author contributions: Dr. Alexopoulos had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Alexopoulos, Reynolds, Bruce, Katz, Ten Have
Acquisition of data: Alexopoulos, Reynolds, Bruce, Katz, Raue, Mulsant, Oslin, Ten Have
Analysis and interpretation of data: Alexopoulos, Reynolds, Bruce, Katz, Raue, Mulsant, Oslin, Ten Have
Drafting of the manuscript: Alexopoulos
Critical revision of the manuscript for important intellectual content: Alexopoulos, Reynolds, Bruce, Katz, Raue, Mulsant, Oslin, Ten Have
Statistical analysis: Alexopoulos, Ten Have
Obtained funding: Alexopoulos, Reynolds, Katz
Administrative, technical, or material support: Alexopoulos, Reynolds, Bruce, Katz, Raue, Mulsant, Oslin, Ten Have
Study supervision: Alexopoulos, Reynolds, Bruce, Katz, Raue, Mulsant, Oslin, Ten Have
Financial Disclosures: Dr. Alexopoulos reports having grant support from Cephalon and Forest; having served as a consultant to Scientific Advisory Board of Forest, Sanofi-Aventis, and Novartis; and having been a member of speakers’ bureaus sponsored by Cephalon, Forest, Lilly, Bristol Meyers Squibb, Glaxo, Pfizer, Janssen and being a stockholder of Johnson and Johnson. Dr. Reynolds reports having grant support in the form of pharmaceutical supplies only from GSK, Forest, Lilly, Pfizer, and BMS. Dr. Mulsant reports having grant support from Janssen, Pfizer, and Eli Lilly; having received consultant fees from Lundbeck and Pfizer; having been a member of speakers’ bureaus sponsored by AstraZeneca and Pfizer; and being a stockholder in Akzo-Nobel, Alkermes, AstraZeneca, Biogen Idec, Celsion, Elan, Eli Lilly, Forest, General Electric, Immune Response, and Pfizer. No other authors have financial interests relevant to the subject of the manuscript.
References
- 1.Goldsmith SK. Reducing Suicide: A National Imperative. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 2.Conwell Y, Thompson C. Suicidal behavior in elders. Psychiatr Clin North Am. 2008;31:333–356. doi: 10.1016/j.psc.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153:1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 4.Lyness JM, Caine ED, King DA, Cox C, Yoediono Z. Psychiatric disorders in older primary care patients. J Gen Intern Med. 1999;14:249–254. doi: 10.1046/j.1525-1497.1999.00326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartels SJ, Coakley E, Oxman TE, et al. Suicidal and death ideation in older primary care patients with depression, anxiety, and at-risk alcohol use. Am J Geriatr Psychiatry. 2002;10:417–427. [PubMed] [Google Scholar]
- 6.Bruce ML, Ten Have TR, Reynolds CF, 3rd, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 7.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulsant BH, Alexopoulos GS, Reynolds CF, 3rd, et al. Pharmacological treatment of depression in older primary care patients: the PROSPECT algorithm. Int J Geriatr Psychiatry. 2001;16:585–592. doi: 10.1002/gps.465. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer R, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) Washington, D.C.: American Psychiatric Association Press, Inc.; 1995. [Google Scholar]
- 11.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 13.Witte TK, Joiner TE, Jr, Brown GK, et al. Factors of suicide ideation and their relation to clinical and other indicators in older adults. J Affect Disord. 2006;94:165–172. doi: 10.1016/j.jad.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Ten Have TR, Kunselman AR, Pulkstenis EP, Landis JR. Mixed effects logistic regression models for longitudinal binary response data with informative drop-out. Biometrics. 1998;54:367–383. [PubMed] [Google Scholar]
- 15.Litiere S, Alonso A, Molenberghs G. Type I and Type II Error Under Random-Effects Misspecification in Generalized Linear Mixed Models. Biometrics. 2007;63:1038–1044. doi: 10.1111/j.1541-0420.2007.00782.x. [DOI] [PubMed] [Google Scholar]
- 16.Little R, Yau L. Intent-to-treat analysis for longitudinal studies with drop-outs. Biometrics. 1996;52:1324–1333. [PubMed] [Google Scholar]
- 17.Gallo JJ, Bogner HR, Morales KH, Post EP, Lin JY, Bruce ML. The effect on mortality of a practice-based depression intervention program for older adults in primary care. A cluster randomized trial. Annals of Internal Medicine. 2007;146:689–698. doi: 10.7326/0003-4819-146-10-200705150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katon WJ, Schoenbaum M, Fan MY, et al. Cost-effectiveness of improving primary care treatment of late-life depression. Arch Gen Psychiatry. 2005;62:1313–1320. doi: 10.1001/archpsyc.62.12.1313. [DOI] [PubMed] [Google Scholar]
- 19.Rost K, Nutting P, Smith JL, Elliott CE, Dickinson M. Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ. 2002;325:934. doi: 10.1136/bmj.325.7370.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unutzer J, Katon W, Callahan CM, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. J Am Geriatr Soc. 2003;51:505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 21.Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ. 2006;332:259–263. doi: 10.1136/bmj.38683.710255.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulberg HC, Lee PW, Bruce ML, et al. Suicidal ideation and risk levels among primary care patients with uncomplicated depression. Ann Fam Med. 2005;3(6):523–528. doi: 10.1370/afm.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szanto K, Reynolds CF, 3rd, Conwell Y, Begley AE, Houck P. High levels of hopelessness persist in geriatric patients with remitted depression and a history of attempted suicide. J Am Geriatr Soc. 1998;46(11):1401–6. doi: 10.1111/j.1532-5415.1998.tb06007.x. [DOI] [PubMed] [Google Scholar]
- 24.Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF., 3rd Occurrence and course of suicidality during short-term treatment of late-life depression. Arch Gen Psychiatry. 2003;60:610–617. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- 25.Lecrubier Y. How do you define remission? Acta Psychiatr Scand. 2002;106:7–11. doi: 10.1034/j.1600-0447.106.s415.2.x. [DOI] [PubMed] [Google Scholar]
- 26.Thase ME, Entsuah AR, Rudolph RL. Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors. Br J Psychiatry. 2001;178:234–241. doi: 10.1192/bjp.178.3.234. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds CF, 3rd, Dew MA, Pollock BG, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 28.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003;289:3145–3151. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 29.Bruce ML, Leaf PJ, Rozal GP, Florio L, Hoff RA. Psychiatric status and 9-year mortality data in the New Haven Epidemiologic Catchment Area Study. Am J Psychiatry. 1994;151:716–721. doi: 10.1176/ajp.151.5.716. [DOI] [PubMed] [Google Scholar]
- 30.Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]