Abstract
Purpose
There is no clear evidence in the actual literature regarding which of the surgical approaches could bring about the best functional, cosmetic, and radiological outcomes, as well as fewer complications, when an open reduction and pinning of a severely displaced supracondylar humerus fracture is performed. We, therefore, performed a systematic review of the English literature to investigate the existing evidence regarding this issue.
Methods
A MEDLINE and EMBASE databases search was performed to identify articles that focused on the functional, cosmetic, and radiological outcomes, as well as post-surgical complications, regarding different surgical approaches used for open reduction and pinning in severely displaced supracondylar humerus fractures in children. One hundred and ninety-four articles were identified, of which seven were included for review. Data analysis included weighted means for all contingency tables and the Chi-square test. Standardized residues were studied when the Chi-square test was statistically significant. Statistical analyses were conducted using Stata 9.1/SE (StataCorp., College Station, TX) and P-values lower than 0.05 were considered to be statistically significant for all analyses.
Results
For functional outcome, a high frequency of excellent results was found within the lateral and medial approaches, and a high frequency of good results within the anterior approach. A high frequency of poor results was found within the posterior approach. For cosmetic outcome, there was a high frequency of fair results within the posterior and lateral approaches, and a high frequency of poor results within the posterior approach. No statistically significant difference regarding time to union, as well as complications, was found.
Conclusion
Our results suggest that a combined antero-medial approach could be the method which allows the achievement of better functional and cosmetic outcome according to Flynn’s criteria. Time to union, as well as post-surgical complications, should not be an issue regarding surgical approaches used for open reduction and pinning in these fractures.
Keywords: Open reduction and pinning, Surgical approaches, Supracondylar humerus fracture, Outcome, Post-surgical complications
Introduction
Supracondylar humerus fractures (SCHF) are common pediatric injuries [1–4], representing about 3% of all fractures [5, 6], are the second most common fractures [7, 8], the most frequent fractures in children under 8 years of age [1, 7–10], and the most common elbow fractures [9, 11, 12]. Two-thirds of children hospitalized because of an elbow injury have an SCHF [11]. Boys have had a higher incidence of this type of fracture, but the difference in comparison with girls seems to be equalizing, and higher rates in girls have actually been reported in some series [9, 11, 13].
These fractures are classified using the modified Gartland classification [14], and most of them are of extension type [10]. Type III and type IV (described by Leitch et al. [15] as being like fractures with multidirectional instability) are considered to be totally displaced with an incidence of 16.7% [16, 17].
Severely displaced SCHF are challenging injuries to treat [16, 18–20] and entail technically difficult procedures for orthopedic surgeons [7, 10]. There remains controversy in the literature with regards to the definitive management of these type of fractures [16, 21, 22]. The differences among authors relate mainly to the choice between treatment by closed reduction and percutaneous K-wire fixation [7, 23, 24] or open reduction and wiring under direct vision [21, 25, 26].
The literature supports closed reduction and percutaneous pinning as the treatment of choice for these fractures [12, 18, 27–29]; however, they could be associated with various complications, such as neurovascular compromise ranging from 5 to 30% [27, 30, 31], skin problems, compartment syndrome, Volkmann’s ischemia, and cubitus varus with an incidence as high as 60% [16, 23, 32, 33]. Although irreducible fractures are uncommon (mostly due to interposition of the brachialis muscle, median nerve, and brachial artery [20]), 2–12% require open reduction [27, 34]. Surgical exposure can be accomplished by a variety of approaches [21, 35–37]. A surgical approach should permit a safe and rapid reduction, with full anatomic alignment, obtaining adequate functional and cosmetic outcomes, as well as few complications.
There is no clear evidence in the literature regarding which of the surgical approaches could bring about the best functional and cosmetic outcomes, as well as less complications. We, therefore, performed a systematic review of the literature to investigate the existing evidence regarding functional and cosmetic outcomes, as well as post-surgical complications among the different surgical approaches described.
Materials and methods
We performed a systematic review of the literature to identify publications dealing with functional, cosmetic, and radiological outcomes, as well as post-surgical complications in patients with totally displaced SCHF managed with primary open reduction through different surgical approaches. An electronic search of the MEDLINE and EMBASE databases (from January 1990 to December 2009) was conducted, entering the following terms and Boolean operators: “open reduction” AND “supracondylar humeral fractures” AND “children”; “primary open reduction” AND “supracondylar humeral fractures” AND “children”. Only papers in English were included.
Articles were considered eligible if they met the following inclusion criteria: (1) the target population consisted of children with totally displaced SCHF; (2) each study included cases with primary open reduction stabilized with K-wires; (3) different surgical approaches were included, such as: lateral, medial, anterior, posterior, and medial + lateral; (4) functional, cosmetic, and/or radiological outcomes; as well as (5) post-surgical complications, such as: nerve/arterial injury, compartment syndrome, infection, nonunion were described adequately.
Review articles, case reports, expert opinion articles, editorials, letters to the editor, publications on congress proceedings, manuscripts with incomplete documentation of outcomes mentioned above, details of applied procedures, or unpublished series were excluded (Fig. 1).
Fig. 1.
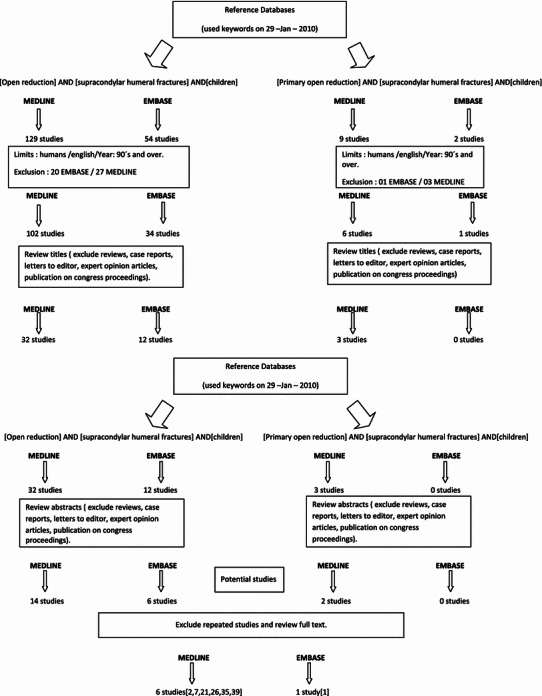
Flowchart showing the literature search strategy followed by the authors. Medline and EMBASE databases were used
The quality of the reviewed manuscripts was evaluated by two assessors (JPM, JRM). They independently classified the reviewed studies for the level of evidence [38] (Table 1) and selected the appropriate studies based on the above criteria.
Table 1.
Demographics of patients in the seven reviewed articles
| Study | Journal | Year | Level of evidence [38] | No. of patients | Surgical approacha | Gender (M/F)b | Age (years)c | Follow-up (months)c |
|---|---|---|---|---|---|---|---|---|
| Kazimoglu et al. [7] | Int Orthop | 2009 | III | 37 | Lateral | M/F:26/11 | 5.9 years (2–12) | 29.5 months (19–62) |
| Kaewpornsawan [2] | J Pediatr Orthop B | 2001 | II | 14 | Lateral | M/F:11/3 | 6.8 years (4.2–9.4) | 5 months (2.5–7.5) |
| Ozkoc et al. [1] | Arch Orthop Trauma Surg | 2004 | III | 44 | Posterior | M/F:25/19 | 10.7 years (3–15) | 35 months (27–46) |
| Ay et al. [35] | J Pediatr Orthop | 2005 | IV | 61 | Anterior | M/F:35/26 | 8.7 years (3–13) | 42 months (12–72) |
| Mulhall et al. [21] | Int Orthop | 2000 | IV | 16 | L:7; M:6; P:1; M + L:2 | M/F:8/8 | 5.9 years (3–10) | 31 months (24–65) |
| Mohammed and Rymaszewski [26] | Injury | 1995 | IV | 10 | M:6; P:2; M + L; 2 | N/A | 7.5 years (4–14)d | 12 months (at least) |
| Kumar et al. [39] | Injury | 2002 | IV | 44 | M:38; A:4; M + L:2 | M/F:34/10 | 8 years (2–14) | 14 months (6–36) |
aSurgical approaches: L lateral, M medial, P posterior, M + L medial and lateral, A anterior
bGender: M male, F female
cValues expressed as means, with ranges in parentheses
dAge and follow-up: mean of the whole study group (32 patients)
Data extracted from these articles were further analyzed for: (1) functional, cosmetic, and radiological outcomes, as well as (2) post-surgical complications according to the surgical approach used for open reduction.
Of the papers initially selected based on the search strategy of this study, seven met the inclusion criteria [1, 2, 7, 21, 26, 35, 39]. The levels of evidence of these studies were II (prospective comparative study) [2], III (retrospective comparative study) [1, 7], and IV (case series) [21, 26, 35, 39]. Two hundred and twenty-six patients were included for the final analysis. Patients were distributed into the different surgical approaches as follows: lateral (58) [2, 7, 21], medial (50) [21, 26, 39], posterior (47) [1, 21, 26], anterior (65) [35, 39], and medial + lateral (6) [21, 26, 39].
To assess the functional outcome, we used Flynn’s criteria (loss of motion), as well as for the cosmetic outcome (carrying angle) [23]. To assess the radiological outcome, we included the time to union. Post-surgical complications described were: compartment syndrome, nonunion, nerve/vascular injury, pin tract infection, and wound issues.
Data analysis
Study participants’ characteristics were summarized according to the result of the systematic review. In order to find differences in associated injuries, functional, cosmetic, and radiological outcomes among different approaches used for open reduction and post-surgical complications, we have calculated weighted means for all contingency tables and the Chi-squared test was performed, studying the standardized residues when the test was statistically significant. When two qualitative variables are analyzed using contingency tables, the Chi-square test is usually used. This test is based on the comparison between the observed frequency and the expected frequency if there was no relationship between both variables. The difference between both values is the “standardized residue”; it has a normal distribution N(0, 1), so if we obtain a value greater than 1.96, we can consider it as being significant with a high frequency (P < 0.05).
Statistical analyses were conducted using Stata 9.1/SE (StataCorp., College Station, TX) and P-values lower than 0.05 were considered to be statistically significant for all analyses.
Results
We identified after our searches, 194 articles (Fig. 1); after applying our eligibility criteria, we had seven papers for systematic review and data synthesis [1, 2, 7, 21, 26, 35, 39].
The patient groups were well matched at baseline for the available demographic data (Table 1). Associated injuries such as nerve/arterial injuries, open fractures, and ipsilateral fractures were described and compared among surgical approaches. There were 23 nerve injuries (10.1%), with radial nerve injury being the most common (11), followed by the anterior interosseous nerve (7), ulnar nerve (2), and diffuse paresthesias (3). Arterial injury (brachial artery) was seen in 15 cases (6.63%). Four open fractures [40, 41] were reported (1.76%; two grade II, one grade I, and one not specified) and ten cases with an ipsilateral fracture (4.42%) were found (Table 2). Weighted means were used for the distribution of these associated injuries into the different groups of surgical approaches, and no statistically significant differences were found (Table 3). A total of 226 patients were included in the analysis.
Table 2.
Associated injuries before open reduction was performed in the seven reviewed articles
| Author | Journal | Year | No. of patients | Nerve injury | Arterial injury | Open fracturea | Ipsilateral fracture |
|---|---|---|---|---|---|---|---|
| Kazimoglu et al. [7] | Int Orthop | 2009 | 37 | 3 (1 ulnar/2 radial) | 0 | 1 (I) | 2 |
| Kaewpornsawan [2] | J Pediatr Orthop B | 2001 | 14 | 2 (anterior interosseous) | 0 | 0 | 0 |
| Ozkoc [1] | Arch Orthop Trauma Surg | 2004 | 44 | 0 | 0 | 0 | 2 |
| Ay et al. [35] | J Pediatr Orthop | 2005 | 61 | 9 (3 anterior interosseous/6 radial) | 7 (brachial artery) | 2 (II) | 5 |
| Mulhall et al. [21] | Int Orthop | 2000 | 16 | 4 (2 median/1 ulnar/1 radial) | 4 (brachial artery) | 0 | 0 |
| Mohammed and Rymaszewski [26] | Injury | 1995 | 10 | 3 (general paresthesia) | 0 | 1 (not specified) | 0 |
| Kumar et al. [39] | Injury | 2002 | 44 | 2 (radial nerve) | 4 (brachial artery) | 0 | 1 |
Table 3.
Associated injuries before open reduction was performed according to surgical approaches
| Surgical approach | Associated injuriesa | |||
|---|---|---|---|---|
| Nerve injury | Arterial injury | Open fracture | Ipsilateral fracture | |
| Lateral | 6.75 | 1.80 | 1.00 | 2.00 |
| Medial | 5.02 | 5.00 | 0.60 | 0.85 |
| Posterior | 0.85 | 0.30 | 0.20 | 2.00 |
| Anterior | 8.18 | 7.50 | 2.00 | 5.10 |
| Medial + lateral | 1.20 | 1.40 | 0.20 | 0.05 |
| P-value | 0.569 | 0.382 | 0.987 | 0.488 |
aContingency table results expressed as weighted means
All articles reported functional, cosmetic, and radiological outcomes, as well as post-surgical complications according to different surgical approaches. Three articles reported results regarding the lateral approach [2, 7, 21], three articles regarding the medial approach [21, 26, 39], three articles regarding the posterior approach [1, 21, 26], two articles regarding the anterior approach [35, 39], and three articles regarding the combined approach (medial + lateral) [21, 26, 39].
In all cases of the studies used for the analysis of the cosmetic, functional, and radiological outcomes, as well as for the post-surgical complications, a primary open reduction was done and no statistically significant difference was found among the different surgical approaches used regarding the associated injuries. The functional and cosmetic outcomes were divided into their subcategories for analysis according to Flynn’s criteria [23] (excellent, good, fair, and poor).
Functional outcome
Four subcategories were evaluated (excellent, good, fair, and poor). Weighted means for the distribution of patients into each subcategory were used and the Chi-square test was used for the assessment of statistical difference. There were three subcategories into which a statistically significant difference was found (excellent, good, poor; Table 4). Standardized residues were used to evaluate the difference among the different surgical approaches within these subcategories. There was a high frequency of excellent results within the lateral and medial approaches (P < 0.05), high frequency of good results (P < 0.05) within the anterior approach, and a high frequency of poor results within the posterior approach (P < 0.05).
Table 4.
Functional outcome according to surgical approach
| Surgical approach | Functional outcomea | |||
|---|---|---|---|---|
| Excellent | Good | Fair | Poor | |
| Lateral | 48.69 | 5.88 | 3.44 | 0.00 |
| Medial | 40.77 | 1.61 | 4.69 | 2.93 |
| Posterior | 23.41 | 6.13 | 4.06 | 13.40 |
| Anterior | 47.27 | 17.09 | 0.45 | 0.18 |
| Medial + lateral | 4.86 | 0.30 | 0.35 | 0.49 |
| P-value | 0.000 | 0.002 | 0.159 | 0.005 |
Functional outcome according to Flynn’s criteria [23]
aContingency table results expressed as weighted means
Cosmetic outcome
As it was done with the functional outcome, weighted means for the distribution of patients into each subcategory were used and the Chi-square test was used for the assessment of statistical difference. There were two subcategories into which a statistically significant difference was found (fair, poor; Table 5). Standardized residues were used to evaluate the difference among the different surgical approaches within these subcategories. There was a high frequency of fair results within the posterior and lateral approaches (P < 0.05) and a high frequency of poor results within the posterior approach (P < 0.05).
Table 5.
Cosmetic outcome according to surgical approach
| Surgical approach | Cosmetic outcomea | |||
|---|---|---|---|---|
| Excellent | Good | Fair | Poor | |
| Lateral | 42.69 | 12.88 | 1.44 | 1.00 |
| Medial | 41.97 | 1.61 | 4.69 | 1.73 |
| Posterior | 33.81 | 6.13 | 5.06 | 2.00 |
| Anterior | 47.27 | 17.09 | 0.45 | 0.18 |
| Medial + lateral | 5.26 | 0.30 | 0.35 | 0.09 |
| P-value | 0.367 | 0.651 | 0.041 | 0.020 |
Cosmetic outcome according to Flynn’s criteria [23]
aContingency table results expressed as weighted means
Radiological outcome assessment included time to union. Weighted means were also used and the Chi-square test was utilized to assess for statistical difference among the surgical approaches. The results were as follows: lateral (4.46 weeks), medial (4.70 weeks), posterior (4.02 weeks), anterior (4 weeks), and medial + lateral (4.70 weeks); there was no statistically significant difference (P = 0.985).
All seven studies commented on complications [1, 2, 7, 21, 26, 35, 39], such as compartment syndrome, nerve/vascular injuries, infections (pin tract infection), and nonunion. Also, wound issues like wound infection and scar problems were commented upon. Weighted means for the distribution of complications into each surgical approach were used and the Chi-square test was used for the assessment of statistical difference. There were no compartment syndromes or nonunions reported; regarding nerve/vascular injuries (P = 0.566) and infections (P = 0.249), there was no statistically significant difference among surgical approaches (Table 6). No vascular injury was reported and the overall rate of nerve injury was 2.21%. The ulnar nerve was the one affected with a higher tendency within the posterior and lateral approaches (cross K-wiring was the construct most often used). The overall pin tract infection rate was 7.96% (18 cases), with a higher tendency of cases within the medial approach. No scar issues were reported and only one case of a superficial wound infection was noted, which resolved with antibiotics.
Table 6.
Post-surgical complications according to surgical approach
| Surgical approach | Complicationsa | |||
|---|---|---|---|---|
| Nerve/vascular injury | Compartment syndrome | Nonunionb | Infectionc | |
| Lateral | 2.00 | 0 | 0 | 2.00 |
| Medial | 0.86 | 0 | 0 | 9.50 |
| Posterior | 2.00 | 0 | 0 | 3.00 |
| Anterior | 0.09 | 0 | 0 | 3.00 |
| Medial + lateral | 0.05 | 0 | 0 | 0.50 |
| P-value | 0.566 | 1.00 | 1.00 | 0.249 |
Discussion
The main aim of the treatment of severely displaced supracondylar fractures is to gain a functional and cosmetically acceptable extremity [7], with no deformity or residual neurovascular deficits [21]. It is the means by which this can be reliably and safely achieved that has caused some controversy. Although closed reduction and percutaneous pinning has been suggested as the preferred treatment [21, 23, 35, 39, 42–44], the technique requires experience and carries risks such as neurovascular complications or incomplete success, which is, in that sense, a reason why open reduction and pinning gain a place within the treatment of these fractures.
Traditionally, open reduction and pinning has been reserved for cases with primary vascular or neural disruption, open fractures, signs of Volkmann’s ischemia, failure of closed reduction, and severe swelling not allowing acceptable reduction [1, 4, 19–21, 33, 45]. Regarding vascular compromise, there is a condition that should be known by surgeons taking care of this type of fracture, which is the “pulseless supracondylar humerus fracture”. In this condition, knowing the status of perfusion of the hand is crucial for the outcome of the patient. In patients presenting with a well-perfused hand, fracture reduction alone is sufficient; however, in those with a poorly perfused hand, the risk for vascular repair is increased [46]. So, if vascular compromise is present, we could manage it with closed reduction if the criterion mention previously are present; otherwise, if an open reduction is necessary, an anterior approach would be of great help because we could have excellent exposure of the structures involved [35].
The main indication in the majority of cases is failure of closed reduction. This could be due to instability of the fracture or the interposition of anatomical structures such as the neurovascular bundle or the brachialis muscle (irreducible fracture) [20].
The overall rate of conversion from closed reduction to open reduction ranges from 3 to 46% [1, 5, 47, 48]. However, there are some authors that reported a rate of 1.3% [47]. Regarding irreducible fractures, some authors reported an open reduction rate ranging from 2 to 12%. We think that an acceptable rate will be the lowest one reported; however, we have to bear in mind that this is a multifactorial issue and rates could vary from one center to another.
Time from injury to surgery has been an issue of controversy regarding its effect on complication as well as open reduction rates. Conditions leading to delay in treatment mainly include severe swelling or skin problems around the elbow and health facility problems [49], such as: availability of a medical facility, surgeon, and anesthesiologist with pediatric capabilities [47]. Some authors advocated that delays in surgery of 6–21 h does not significantly alter complication rates or the need for open reduction in children undergoing surgical treatment of these fractures [47, 50–52]; however, this idea is not widely accepted by other authors, who maintained that there is no difference with regards to the complications rates, even though a significant swelling at presentation and delay in fracture reduction could be important warning signs for the development of a compartment syndrome [53]. Walmsley et al. [54] conducted a retrospective study that included 171 children and found that patients waiting for more than 8 h were more likely to undergo open reduction (33 vs. 11.2%; P < 0.05). And Yildirim et al. [45] concluded that the probability of switching to open reduction increased by a factor of 4 every 5 h beginning 15 h after injury; an open reduction was always necessary after 32 h. Based on these findings, a definitive conclusion is difficult to obtain, even though our recommendation is to treat this type of fracture as early as possible.
In cases in which an open reduction and pinning is justified, there is no clear evidence of which surgical approach could show better functional, cosmetic, and radiological outcome, as well as fewer complications. Trying to find this out, we focus our analysis onto the data extracted from articles based on primary open reduction and pinning with no statistically significant difference regarding the associated injuries. This provides a homogenous study group and the real behavior of the different surgical approaches regarding the outcomes mentioned above, as well as their post-surgical complications.
Our findings regarding the functional outcome show a high frequency of excellent results within the lateral and medial approaches and a high frequency of good results within the anterior approach. The most common reason for a failed reduction is the proximal fragment’s buttonholing through the brachialis muscle [37, 55]. Another factor is the interposition of the joint capsule or periosteum between the fracture fragments [35, 37, 55, 56]; this could be managed through an anterior approach or combined with a lateral or medial method (posterolateral or posteromedial displacement), allowing an anatomical reduction. There is some evidence that fibrosis in the brachialis muscle is the principal obstruction to the restoration of extension [39], and through these approaches, this issue could be managed in an optimum fashion with direct access, producing less damage and a less intense inflammatory response with less scarring tissue formation. Some authors have demonstrated no correlation between stiffness and the type of surgical approach used, especially regarding the posterior approach [22, 39]. However, Gruber and Hudson [36] correlate motion restriction with posterior incisions. Our findings show a high frequency of poor results with this approach; this could be explained based on the fact that, through this approach, anterior structures such as the brachialis muscle as well as neurovascular structures could not be achieved and the effect of a retracted scar localized posteriorly could decrease the range of motion, as mentioned by Gruber and Hudson.
Authors performing open reduction through the lateral and posterior approaches [6, 22, 36, 48, 57] have reported change in carrying angle (cosmetic outcome) as the most frequently encountered complication. These findings correlate with our results with a high frequency of fair results within the posterior and lateral approaches, as well as a high frequency of poor results within the posterior approach. Medial column comminution and internal rotation of the distal fragment predispose to the coronal tilt, which is the main cause of loss of carrying angle [39, 58, 59]; these facts could not be managed adequately through a lateral or posterior approach.
An important finding to highlight is that the time to union is not affected by the surgical approach used; we did not find a statistically significant difference among the surgical approaches.
No surgical approach showed a higher incidence of complications such as compartment syndrome, nonunion, or nerve/vascular injury. There was a higher tendency of ulnar nerve injury among the posterior and lateral approaches. This could be explained because, when using a cross K-wire construct through the approaches mention previously, the ulnar nerve is not under direct vision and is prone to be damaged.
Even though our findings show that complications should not be an issue regarding surgical approaches, we feel that orthopedic surgeons should have some idea on how to solve them if they appear. With regard to vascular injury, 10–20% of patients with a type III supracondylar fracture present with an absent pulse [30, 31, 34]; this condition is called “pulseless supracondylar humerus fracture”. There is controversy about treatment if the pulse does not return but the hand is well perfused. Omid et al. [11] recommend to admit the child to the hospital, elevate the limb slightly, and observe him or her for at least 48 h. Loss of perfusion can occur during this time and necessitate emergent treatment. As mentioned before, if an open reduction is performed, an anterior approach is indicated in order to allow the evaluation of all vital structures at risk for incarceration between fracture fragments [18]. Remember that early repair of the brachial artery is associated with a high rate of symptomatic reocclusion and residual stenosis [11]. Another possible issue could be neurologic injury, with a reported rate ranging from 10 to 20% [60]. The anterior interosseous nerve appears to be the most commonly injured nerve with extension type fractures [4, 11, 53]; this produces motor deficit without sensory changes. However, a complete median nerve transaction has also been reported with both motor and sensory changes [61]. Open reduction and exploration is not necessarily indicated when this injury is associated with a closed fracture because neural recovery generally occurs after 2–2.5 months, but it may take up to 6 months [62]. Compartment syndrome is a rare complication with a rate ranging from 0.1 to 0.3%, however, its consequences are devastating if an appropriate treatment is not performed. Some authors [53] suggested that ecchymosis and severe swelling, even in the presence of an intact radial pulse with good capillary refill, should alert to the possibility of a compartment syndrome; a fasciotomy should be done immediately. Finally, some words about pin tract infection; it could be presented in up to 6.6% of cases [63, 64]. In general, this problem could be solved with oral antibiotics with or without removing the pins [47, 50].
Limitations within our study must be acknowledged. That few studies selected for analysis was a consequence of the strict inclusion criteria used, this permits us to have a more valuable analysis of the effect of surgical approaches used for open reduction by themselves in the different parameters described. However, the number of patients for analysis decreased. There were few patients within the combined approach (medial + lateral); this did not allow us to make conclusions regarding this approach.
Conclusion
Supracondylar humerus fractures in children are very common and is the most common injury of the children’s elbow. Sometimes, an open reduction and pinning is required to obtain an acceptable reduction of these fractures. There are different surgical approaches that can be used for this purpose; however, there is controversy regarding the effect on the functional as well cosmetic outcomes. Our results suggest that a combined antero-medial approach could be the method which allows the achievement of better functional and cosmetic outcomes according to Flynn’s criteria. However, the final decision for performing a surgical approach will depend on the surgeon’s experience, the anatomical structures involved, as well as the characteristics of the fracture.
The time to union as well as post-surgical complications should not be an issue regarding the surgical approaches used for open reduction and pinning in severely displaced supracondylar humerus fractures in children.
Acknowledgments
Disclaimer
The authors did not receive any outside funding or grants in support of their research for or the preparation of this work. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Sources of any support of the work
No special support was received (grant, equipment, drugs).
References
- 1.Ozkoc G, Gonc U, Kayaalp A, Teker K, Peker TT. Displaced supracondylar humeral fractures in children: open reduction vs. closed reduction and pinning. Arch Orthop Trauma Surg. 2004;124:547–551. doi: 10.1007/s00402-004-0730-1. [DOI] [PubMed] [Google Scholar]
- 2.Kaewpornsawan K. Comparison between closed reduction with percutaneous pinning and open reduction with pinning in children with closed totally displaced supracondylar humeral fractures: a randomized controlled trial. J Pediatr Orthop B. 2001;10:131–137. [PubMed] [Google Scholar]
- 3.Aronson DC, van Vollenhoven E, Meeuwis JD. K-wire fixation of supracondylar humeral fractures in children: results of open reduction via a ventral approach in comparison with closed treatment. Injury. 1993;24:179–181. doi: 10.1016/0020-1383(93)90288-H. [DOI] [PubMed] [Google Scholar]
- 4.Cramer KE, Devito DP, Green NE. Comparison of closed reduction and percutaneous pinning versus open reduction and percutaneous pinning in displaced supracondylar fractures of the humerus in children. J Orthop Trauma. 1992;6:407–412. doi: 10.1097/00005131-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Aktekin CN, Toprak A, Ozturk AM, Altay M, Ozkurt B, Tabak AY. Open reduction via posterior triceps sparing approach in comparison with closed treatment of posteromedial displaced Gartland type III supracondylar humerus fractures. J Pediatr Orthop B. 2008;17:171–178. doi: 10.1097/BPB.0b013e3283046530. [DOI] [PubMed] [Google Scholar]
- 6.Minkowitz B, Busch MT. Supracondylar humerus fractures. Current trends and controversies. Orthop Clin North Am. 1994;25:581–594. [PubMed] [Google Scholar]
- 7.Kazimoglu C, Cetin M, Sener M, Aguş H, Kalanderer O. Operative management of type III extension supracondylar fractures in children. Int Orthop. 2009;33:1089–1094. doi: 10.1007/s00264-008-0605-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Battaglia TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop. 2002;22:431–439. [PubMed] [Google Scholar]
- 9.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma. 1993;7:15–22. doi: 10.1097/00005131-199302000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Barlas K, George B, Hashmi F, Bagga T. Open medial placement of Kirschner wires for supracondylar humeral fractures in children. J Orthop Surg (Hong Kong) 2006;14:53–57. doi: 10.1177/230949900601400112. [DOI] [PubMed] [Google Scholar]
- 11.Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121–1132. doi: 10.2106/JBJS.G.01354. [DOI] [PubMed] [Google Scholar]
- 12.Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18:38–42. [PubMed] [Google Scholar]
- 14.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109:145–154. [PubMed] [Google Scholar]
- 15.Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified gartland type-IV fracture. J Bone Joint Surg Am. 2006;88:980–985. doi: 10.2106/JBJS.D.02956. [DOI] [PubMed] [Google Scholar]
- 16.Sadiq MZ, Syed T, Travlos J. Management of grade III supracondylar fracture of the humerus by straight-arm lateral traction. Int Orthop. 2007;31:155–158. doi: 10.1007/s00264-006-0168-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci. 2001;6:312–315. doi: 10.1007/s007760100024. [DOI] [PubMed] [Google Scholar]
- 18.Aronson DC, Meeuwis JD. Anterior exposure for open reduction of supracondylar humeral fractures in children: a forgotten approach? Eur J Surg. 1994;160:263–266. [PubMed] [Google Scholar]
- 19.Yusof A, Razak M, Lim A. Displaced supracondylar fracture of humerus in children—comparative study of the result of closed and open reduction. Med J Malaysia. 1998;53(Suppl A):52–58. [PubMed] [Google Scholar]
- 20.Oh CW, Park BC, Kim PT, Park IH, Kyung HS, Ihn JC. Completely displaced supracondylar humerus fractures in children: results of open reduction versus closed reduction. J Orthop Sci. 2003;8:137–141. doi: 10.1007/s007760300023. [DOI] [PubMed] [Google Scholar]
- 21.Mulhall KJ, Abuzakuk T, Curtin W, O’Sullivan M. Displaced supracondylar fractures of the humerus in children. Int Orthop. 2000;24:221–223. doi: 10.1007/s002640000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sibly TF, Briggs PJ, Gibson MJ. Supracondylar fractures of the humerus in childhood: range of movement following the posterior approach to open reduction. Injury. 1991;22:456–458. doi: 10.1016/0020-1383(91)90128-2. [DOI] [PubMed] [Google Scholar]
- 23.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;56:263–272. [PubMed] [Google Scholar]
- 24.Paradis G, Lavallee P, Gagnon N, Lemire L. Supracondylar fractures of the humerus in children. Technique and results of crossed percutaneous K-wire fixation. Clin Orthop Relat Res. 1993;297:231–237. [PubMed] [Google Scholar]
- 25.Furrer M, Mark G, Rüedi T. Management of displaced supracondylar fractures of the humerus in children. Injury. 1991;22:259–262. doi: 10.1016/0020-1383(91)90001-U. [DOI] [PubMed] [Google Scholar]
- 26.Mohammed S, Rymaszewski LA. Supracondylar fractures of the distal humerus in children. Injury. 1995;26:487–489. doi: 10.1016/0020-1383(95)93594-8. [DOI] [PubMed] [Google Scholar]
- 27.Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop. 2001;21:157–161. [PubMed] [Google Scholar]
- 28.Kasser JR. Percutaneous pinning of supracondylar fractures of the humerus. Instr Course Lect. 1992;41:385–390. [PubMed] [Google Scholar]
- 29.Carcassonne M, Bergoin M, Hornung H. Results of operative treatment of severe supracondylar fractures of the elbow in children. J Pediatr Surg. 1972;7:676–679. doi: 10.1016/0022-3468(72)90278-3. [DOI] [PubMed] [Google Scholar]
- 30.Schoenecker PL, Delgado E, Rotman M, Sicard GA, Capelli AM. Pulseless arm in association with totally displaced supracondylar fracture. J Orthop Trauma. 1996;10:410–415. doi: 10.1097/00005131-199608000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Shaw BA, Kasser JR, Emans JB, Rand FF. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. J Orthop Trauma. 1990;4:25–29. doi: 10.1097/00005131-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Chen RS, Liu CB, Lin XS, Feng XM, Zhu JM, Ye FQ. Supracondylar extension fracture of the humerus in children. Manipulative reduction, immobilisation and fixation using a U-shaped plaster slab with the elbow in full extension. J Bone Joint Surg Br. 2001;83:883–887. doi: 10.1302/0301-620X.83B6.11705. [DOI] [PubMed] [Google Scholar]
- 33.Ababneh M, Shannak A, Agabi S, Hadidi S. The treatment of displaced supracondylar fractures of the humerus in children. A comparison of three methods. Int Orthop. 1998;22:263–265. doi: 10.1007/s002640050255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pirone AM, Graham HK, Krajbich JI. Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1988;70:641–650. [PubMed] [Google Scholar]
- 35.Ay S, Akinci M, Kamiloglu S, Ercetin O. Open reduction of displaced pediatric supracondylar humeral fractures through the anterior cubital approach. J Pediatr Orthop. 2005;25:149–153. doi: 10.1097/01.bpo.0000153725.16113.ab. [DOI] [PubMed] [Google Scholar]
- 36.Gruber MA, Hudson OC. Supracondylar fracture of the humerus in childhood. End-result study of open reduction. J Bone Joint Surg Am. 1964;46:1245–1252. [PubMed] [Google Scholar]
- 37.Rasool MN, Naidoo KS. Supracondylar fractures: posterolateral type with brachialis muscle penetration and neurovascular injury. J Pediatr Orthop. 1999;19:518–522. doi: 10.1097/01241398-199907000-00019. [DOI] [PubMed] [Google Scholar]
- 38.Foad SL, Mehlman CT, Foad MB, Lippert WC (2009) Prognosis following neonatal brachial plexus palsy: an evidence-based review. J Child Orthop (in press) [DOI] [PMC free article] [PubMed]
- 39.Kumar R, Kiran EK, Malhotra R, Bhan S. Surgical management of the severely displaced supracondylar fracture of the humerus in children. Injury. 2002;33:517–522. doi: 10.1016/S0020-1383(02)00031-1. [DOI] [PubMed] [Google Scholar]
- 40.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 41.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Kurer MH, Regan MW. Completely displaced supracondylar fracture of the humerus in children. A review of 1708 comparable cases. Clin Orthop Relat Res. 1990;256:205–214. [PubMed] [Google Scholar]
- 43.Mazda K, Boggione C, Fitoussi F, Penneçot GF. Systematic pinning of displaced extension-type supracondylar fractures of the humerus in children. A prospective study of 116 consecutive patients. J Bone Joint Surg Br. 2001;83:888–893. doi: 10.1302/0301-620X.83B6.11544. [DOI] [PubMed] [Google Scholar]
- 44.Wilkins KE. The operative management of supracondylar fractures. Orthop Clin North Am. 1990;21:269–289. [PubMed] [Google Scholar]
- 45.Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A. Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. J Child Orthop. 2009;3:265–269. doi: 10.1007/s11832-009-0189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi PD, Melikian R, Skaggs DL. Risk factors for vascular repair and compartment syndrome in the pulseless supracondylar humerus fracture in children. J Pediatr Orthop. 2010;30:50–56. doi: 10.1097/BPO.0b013e3181c6b3a8. [DOI] [PubMed] [Google Scholar]
- 47.Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop. 2004;24:245–248. doi: 10.1097/01241398-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 48.Alonso-Llames M. Bilaterotricipital approach to the elbow. Its application in the osteosynthesis of supracondylar fractures of the humerus in children. Acta Orthop Scand. 1972;43:479–490. doi: 10.3109/17453677208991270. [DOI] [PubMed] [Google Scholar]
- 49.Eren A, Güven M, Erol B, Cakar M. Delayed surgical treatment of supracondylar humerus fractures in children using a medial approach. J Child Orthop. 2008;2:21–27. doi: 10.1007/s11832-007-0072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH. The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am. 2001;83:323–327. doi: 10.2106/00004623-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Leet AI, Frisancho J, Ebramzadeh E. Delayed treatment of type 3 supracondylar humerus fractures in children. J Pediatr Orthop. 2002;22:203–207. [PubMed] [Google Scholar]
- 52.Iyengar SR, Hoffinger SA, Townsend DR. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma. 1999;13:51–55. doi: 10.1097/00005131-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, Do TT, Kay RM. Delaying treatment of supracondylar fractures in children: has the pendulum swung too far? J Bone Joint Surg Br. 2008;90:1228–1233. doi: 10.1302/0301-620X.90B9.20728. [DOI] [PubMed] [Google Scholar]
- 54.Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br. 2006;88:528–530. doi: 10.1302/0301-620X.88B4.17491. [DOI] [PubMed] [Google Scholar]
- 55.Archibeck MJ, Scott SM, Peters CL. Brachialis muscle entrapment in displaced supracondylar humerus fractures: a technique of closed reduction and report of initial results. J Pediatr Orthop. 1997;17:298–302. [PubMed] [Google Scholar]
- 56.Kekomäki M, Luoma R, Rikalainen H, Vilkki P. Operative reduction and fixation of a difficult supracondylar extension fracture of the humerus. J Pediatr Orthop. 1984;4:13–15. doi: 10.1097/01241398-198401000-00003. [DOI] [PubMed] [Google Scholar]
- 57.Weiland AJ, Meyer S, Tolo VT, Berg HL, Mueller J. Surgical treatment of displaced supracondylar fractures of the humerus in children. Analysis of fifty-two cases followed for five to fifteen years. J Bone Joint Surg Am. 1978;60:657–661. [PubMed] [Google Scholar]
- 58.Smith L. Deformity following supracondylar fractures of the humerus. J Bone Joint Surg Am. 1960;42:235–252. [PubMed] [Google Scholar]
- 59.Labelle H, Bunnell WP, Duhaime M, Poitras B. Cubitus varus deformity following supracondylar fractures of the humerus in children. J Pediatr Orthop. 1982;2:539–546. doi: 10.1097/01241398-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 60.Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB. Neurovascular injury and displacement in type III supracondylar humerus fractures. J Pediatr Orthop. 1995;15:47–52. doi: 10.1097/01241398-199501000-00011. [DOI] [PubMed] [Google Scholar]
- 61.Spinner M, Schreiber SN. Anterior interosseous-nerve paralysis as a complication of supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1969;51:1584–1590. [PubMed] [Google Scholar]
- 62.Brown IC, Zinar DM. Traumatic and iatrogenic neurological complications after supracondylar humerus fractures in children. J Pediatr Orthop. 1995;15:440–443. doi: 10.1097/01241398-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 63.Boyd DW, Aronson DD. Supracondylar fractures of the humerus: a prospective study of percutaneous pinning. J Pediatr Orthop. 1992;12:789–794. doi: 10.1097/01241398-199211000-00017. [DOI] [PubMed] [Google Scholar]
- 64.Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86:702–707. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]


