Abstract
This study assessed shoulder motion using bone-fixed sensors to quantify scapulohumeral motion during unconstrained raising and lowering of the arm. Electromagnetic tracking devices rigidly fixed to bone pins recorded active scapular and humeral motion. We found a significant difference in the ratio of glenohumeral elevation to scapular upward rotation during arm raising (2.3) and lowering (2.7). Each degree of glenohumeral elevation yielded scapular upward rotation of 0.43° (raising) compared to downward rotation of 0.37° (lowering), across the motion arc. Until 125° of glenohumeral elevation, the scapula internally rotated then externally rotated with further elevation. Scapular upward rotation and posterior tilting progressively increased until maximal elevation. Scapulohumeral rhythm was greatest in the first increment of raising the arm and higher overall when lowering the arm. Understanding these data allows improved evaluation of potential motion abnormalities in patients with shoulder pathology and may improve treatment for restoration of normal shoulder motion.
Keywords: scapulohumeral rhythm, shoulder biomechanics, glenohumeral, scapular motion
Introduction
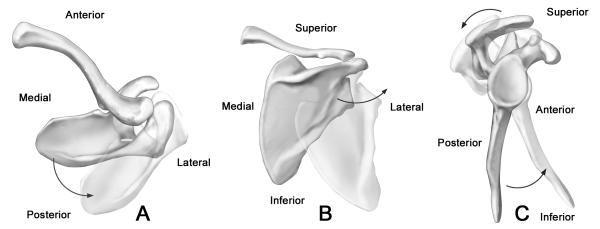
Scapulohumeral rhythm is the relationship between elevation at the glenohumeral joint and scapular upward rotation. To fully understand the spectrum of shoulder problems, it is important to recognize the contribution of scapulothoracic motion to overall “shoulder” motion. When this relationship is altered, it leads to shoulder dysfunction. Current emphasis on core strengthening as a method of improving shoulder pain also implies a contribution from the scapulothoracic articulation.11 New technologies have allowed for three-dimensional assessment of scapular rhythm during active motion. This enables more complete analysis of scapular motion, since the scapula undergoes angular changes with humeral motion in the axial, coronal, and sagittal planes. The description of scapulothoracic and glenohumeral motion beyond the components of scapular upward rotation and glenohumeral elevation can now include scapular internal/external rotation and anterior/posterior tilting, as well as plane of glenohumeral elevation and glenohumeral axial rotation (Figures 1 & 2). Finally, reporting of scapular upward/downward rotation using three dimensional methods is not subject to projection error.
Figure 1.
(A). Scapular internal and external rotation: (superior view right shoulder) Ghosted image represents increased internal rotation. Please note: with increasing internal rotation, the glenoid articular surface internally rotates. (B). Scapular upward rotation (posterior view right shoulder) Ghosted image represents increased upward rotation. Please note: with increased upward rotation, the glenoid articular surface upwardly rotates. (C). Scapular tilting (lateral view right shoulder) Ghosted image represents increased posterior tilting. Please note: with increased posterior tilting, the glenoid rotates posteriorly.
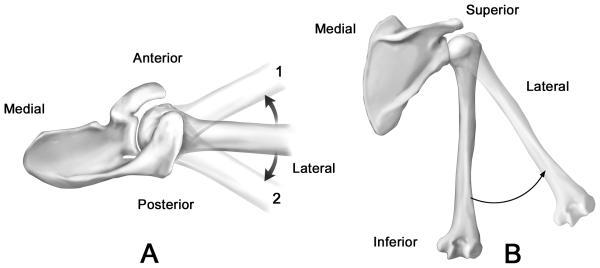
Figure 2.
(A). Plane of elevation (superior view right shoulder) Ghosted images represent 1 anterior and 2 posterior to the plane of the scapula. (B). Glenohumeral elevation angle (posterior view right shoulder) Ghosted image represents increased glenohumeral elevation.
Prior studies of shoulder motion in three dimensions have made use of either skin sensors,12,19,20 palpation methods,3,17,25 or hybrid techniques.1,6,18 Earlier studies using roentgenograms have imaged the shoulder in positions throughout the range of motion in the scapular plane.5, 23 However, these studies are limited by their static nature. Additionally, Doody et al. in their goniometric study and the roentgenographic study by Freedman et al. found that the scapulohumeral rhythm was variable throughout the arc of motion.4,5 The invasiveness of bone pins has limited their use; but substantive reported errors in measurements associated with skin sensors, particularly at higher angles of humeral elevation, limit the precision of surface sensor techniques.9,15 Currently, bone-fixed tracking is the gold-standard for precise shoulder motion measurement.6,7,10,16,22
Past studies have, for purposes of consistency and ease of measurement, limited the measurement of humeral elevation to controlled planes.4,5,8,13,18,19,23 Also, since Inman et al. reported an overall constant scapulohumeral rhythm of 2:1 during humeral elevation in the sagittal (flexion) and coronal (abduction) planes,8 this ratio has been widely accepted despite numerous subsequent studies3-5,18,19 which produced different results in different planes. Inman's study8 is still the landmark study for description of shoulder motion, but it is unclear if there was more than one subject and how the data were collected. As a result, it is difficult to imagine that similar data published today would be so well-received. Newer studies3-5,18,19 provide improved description of samples tested and measurement methods, as well as values for the rhythm during increments of overall motion. Reported ratios ranged from as low as 1.25:1 to as high as 7.29:1 for different increments of motion, with greater variability early in the motion. Finally, activities of daily living do not occur in constrained planes; therefore, we studied a plane which the subject self-selected in order to better replicate actual daily shoulder motion.
The purpose of this study was to quantify the relationship of the scapula and the humerus in three dimensions during unconstrained raising and lowering of the arm overhead. Our null hypothesis was that there is no significant difference in the rhythm between the raising and lowering of the arm or between portions of the range of motion that occur.
Materials and Methods
These results represent a subset of specific motions, not previously published, performed as part of a more comprehensive analysis of shoulder motion in asymptomatic volunteers.16 Informed consent and Human Subjects Institutional Review Board approval at the (blinded for review) were obtained. Subjects between 18 – 60 years old, had no prior shoulder problems, no systemic illness, and a normal clinical shoulder when examined by a licensed physical therapist (initials blinded for review).
Surgical Technique and System Setup
Using fluoroscopy (MiniView 6800 Mobile Imaging System, General Electric Medical Systems, Milwaukee, WI, USA) to guide placement, 2.5 mm terminally-threaded stainless steel pins were inserted under sterile technique with local anesthesia. Pins engaged the far cortex of the scapular spine, distal clavicle, and lateral humerus at the deltoid insertion. All subjects had their arms put through a full range of motion after placement to ensure that no skin tension contributed to pin deflection or limited shoulder motion.
Electromagnetic sensors were rigidly fixed to the bone pins to record active motion. A surface sensor was taped to the sternum as a thoracic reference marker. During testing, the Flock of Birds mini-bird electromagnetic three-dimensional tracking system (Ascension Technology, Burlington, VT) attached to the pins recorded motion. This six degree of freedom sensor allows recording of movement and rotation in all planes at a sampling rate of 100 Hz per sensor. The reported transmitter system resolution is 0.1° and 0.25 mm.2,21 Motion Monitor Software (Innovative Sports Training, Chicago, IL) calculated receiver position and orientation along the transmitter axis as well as relative to other reference frames. Using an integrated digitizing stylus, anatomical landmarks were digitized with the subjects standing relaxed to establish anatomical coordinate systems consistent with the recommendations of the International Society of Biomechanics (ISB) shoulder protocol,27 except that the acromioclavicular joint was used rather than the posterolateral acromion.25 The digitized bony landmarks were then utilized to convert the sensor axes to anatomical axes.
Subjects were instructed to raise their arms as if reaching for an object on a high shelf (Figure 3). No attempt was made to control plane of motion or height of reaching (subjects self-selected their reaching plane and elevated reach position). Two repetitions were completed for each subject with each repetition consisting of raising and lowering of the arm for a three second count.
Figure 3.
Subject elevating arm in overhead reaching.
At the completion of the entire comprehensive shoulder motion study, subjects had the pins removed and their incisions closed. They were seen in follow-up at seven to ten days post-procedure for an incision check. Prior to pin placement, a subset of 6 of the subjects performed the same unconstrained reaching motion using standard surface sensor placements for the humerus and thorax14 to determine the effects of pin placement on the subject's general motion pattern, maximum elevation during reaching over head, and self-selected plane of elevation.
Data Analysis
Angular values for the scapula relative to the thorax were determined using the ISB recommended rotation sequences27 along with a humerus relative to the scapula rotation sequence of glenohumeral elevation angle, plane of glenohumeral elevation, and glenohumeral axial (internal/external) rotation (x, z’, y”, Cardan angles).14 Continuous data were recorded concerning scapular internal rotation, scapular upward rotation, scapular tilting (Figure 1), humerothoracic elevation, glenohumeral elevation (relative to the scapula), glenohumeral elevation plane (anterior or posterior to the scapular plane, Figure 2), and glenohumeral internal/external rotation and were exported from the Motion Monitor software and saved as spreadsheets in Excel (Microsoft, Redmond, WA).
The ratio of glenohumeral elevation relative to scapular upward rotation was determined by calculating the slope of the line using scapular upward rotation as the X value and glenohumeral elevation as the Y value (Excel slope function, calculating the slope of the linear regression line). The ratio was calculated from minimum to maximum humerothoracic angle and maximum to minimum angle of each repetition for each subject, as well as in thirty degree increments (minimum (min) to 30°, 30°−60°, 60°−90°, 90°−120°) during raising and lowering phases of the repetitions. For the purpose of this study, raising was defined as the phase during which the arm was actively raised until maximum elevation. Lowering was considered the phase from maximum elevation to the starting position. Ratios were also calculated for the initial portion of the motion cycle (minimum to 30°), the portion of the cycle described by Inman et al8 as the setting phase for abduction (Table I). During our analysis, values obtained for scapular upward rotation, glenohumeral elevation, and glenohumeral external rotation were actually negative based on axis orientation. These values were multiplied by −1 to facilitate clinical correlation and interpretation. Pain scores from zero to ten on a numerical rating scale were recorded for each movement during this study.
Table I.
Glenohumeral: Scapulothoracic ratios for arm elevation and arm lowering movements for each subject at intervals throughout the arc of reaching overhead motion.
| Subject | Phase | Min-Max | 30°-Max | Min-30° | 30°-60° | 60°-90° | 90°-120° |
|---|---|---|---|---|---|---|---|
| 1 | Raising Lowering |
2.10 2.10 |
2.01 1.68 |
2.31 3.72 |
2.49 2.59 |
1.91 1.52 |
2.30 1.65 |
| 2 | Raising Lowering |
2.11 2.16 |
2.01 1.80 |
6.55 8.37 |
2.18 3.03 |
1.91 1.38 |
2.17 2.01 |
| 3 | Raising Lowering |
2.12 2.15 |
2.03 2.48 |
3.14 2.20 |
1.98 1.40 |
2.49 2.50 |
2.10 3.49 |
| 4 | Raising Lowering |
2.59 2.80 |
2.73 3.14 |
2.15 2.07 |
2.20 2.34 |
3.55 3.05 |
2.5 4.06 |
| 5 | Raising Lowering |
2.48 2.48 |
2.74 3.44 |
1.59 0.96 |
2.10 2.40 |
2.75 3.27 |
2.68 6.28 |
| 6 | Raising Lowering |
1.65 1.43 |
1.48 1.00 |
5.07 2.02 |
2.22 1.60 |
1.60 0.61 |
1.04 1.75 |
| 7 | Raising Lowering |
3.36 3.88 |
3.27 3.65 |
3.86 3.35 |
3.44 4.02 |
3.94 3.13 |
2.64 4.23 |
| 8 | Raising Lowering |
2.27 2.42 |
1.81 1.89 |
7.89 5.43 |
4.16 3.32 |
3.37 1.83 |
1.43 1.61 |
| 9 | Raising Lowering |
2.42 3.36 |
2.30 3.87 |
4.85 0.69 |
2.51 5.47 |
2.53 3.50 |
3.00 3.87 |
| 10 | Raising Lowering |
2.09 2.22 |
2.11 2.17 |
4.58 2.02 |
1.64 1.56 |
2.17 2.43 |
2.31 2.37 |
| 11 | Raising Lowering |
2.38 3.21 |
2.77 4.17 |
1.38 0.31 |
1.58 2.64 |
2.17 3.95 |
4.64 5.03 |
| 12 | Raising Lowering |
2.90 2.97 |
2.45 3.46 |
1.11 0.86 |
1.86 2.79 |
4.17 5.90 |
3.14 4.75 |
|
Mean (+/− sd) |
Raising | 2.37 ± 0.44 | 2.31 ± 0.50 | 3.71 ± 2.15 | 2.36 ± 0.75 | 2.71 ± .85 | 2.50 ± 0.90 |
|
Mean (+/− sd) |
Lowering | 2.60 ± 0.67 | 2.73 ± 1.02 | 2.67 ± 2.31 | 2.76 ± 1.14 | 2.76 ± 1.40 | 3.43 ± 1.54 |
Statistical Analysis
Data values for scapular internal rotation, scapular upward rotation, scapular tilting (all relative to the thorax) and glenohumeral elevation, plane of elevation, and internal/external rotation relative to the scapula were averaged across all subjects at five degree increments. At each increment, descriptive statistics were calculated. Descriptive statistics across subjects were also determined for both the invasive testing and the subset of subjects for whom humerothoracic motion data were available prior to pin placement.
For overall ratio data, incremental ratio data and, angular data, a repeated measure analysis of variance (ANOVA) was calculated (NCSS, Kaysville, UT) with appropriate factors for each. All analyses used a significant alpha level of 0.05 and Tukey adjusted follow-up comparisons for pairwise differences. A Pearson correlation was also computed for the subset of 6 subjects comparing humerothoracic elevation prior to pin placement to values during invasive testing with pins in place.
Results
There were 7 males and 5 females, with an average age, height, and weight of 29.3 years (+/− 6.8), 1.74 meters (+/− 0.08), and 77.5 kilograms (+/− 13.8) respectively. Non-dominant arms were tested for 10 of the 12 subjects, with 3 right and 9 left shoulders undergoing testing. Pain scores averaged 1.4 (range, 0 to 3) on a 10 point scale during measurement and no subjects had to limit their overhead reach due to pain or pin placement. No subject had to stop the investigation due to shoulder discomfort. In addition, none of the subjects had any post-procedure complications. The average humerothoracic plane of elevation chosen by the subjects during overhead reaching was 63.3° (± 7.0°) forward of the coronal plane of the trunk and the average peak elevation was 132.9° (± 9.9°). For the subset of 6 subjects, motion during invasive testing was consistent with motion prior to pin placement. Average plane of elevation and peak elevation during invasive testing were within 2° of these same values when compared to overhead reaching tested prior to pin placement. The correlation (r) between humeral elevation motion with and without pins placed was 0.9, indicating excellent consistency between invasive and non-invasive testing.
Scapulohumeral Rhythm
There was a significant difference (p < 0.04) for the scapulohumeral rhythm between raising and lowering motions (30° to maximum) with glenohumeral elevation to scapular upward rotation ratios of 2.3 and 2.7 respectively (Table I). This difference represents a greater overall scapular contribution during the raising of the arm. For every one degree of glenohumeral elevation, the scapula rotated upward 0.43° across the entire motion arc for overhead reaching and rotated downward 0.37° for every degree the humerus was lowered (p < 0.04). The average scapular upward rotation increased significantly during overhead reaching from 11.4° ± 5.8° to a maximum of 48.6° ± 4.0° (p < 0.05). The glenohumeral elevation values significantly increased from −7.4° ± 5.0° (adducted) at minimum to 96.9° ± 5.5° (abducted) at maximum humerothoracic elevation (p < 0.05).
To determine the relationship between glenohumeral and scapulothoracic motion during different increments of the motion arc, the ratio was also calculated in 30° increments between the starting position and 120° (i.e. min°-30°, 30°-60°, etc; Table I). Ratio differences during increments of motion reflect raising vs. lowering of the arm (p < 0.004). During raising of the arm, the glenohumeral contribution to scapulohumeral rhythm was greatest for the min-30° increment and decreased as the humerothoracic angle increased. In pair-wise follow-up comparisons, the scapulohumeral rhythm during the min-30° increment was significantly higher than the values during the 30°-60° and the 90°-120° motion increments (p<0.05) (Table I).
Additional Scapulothoracic Angular Values
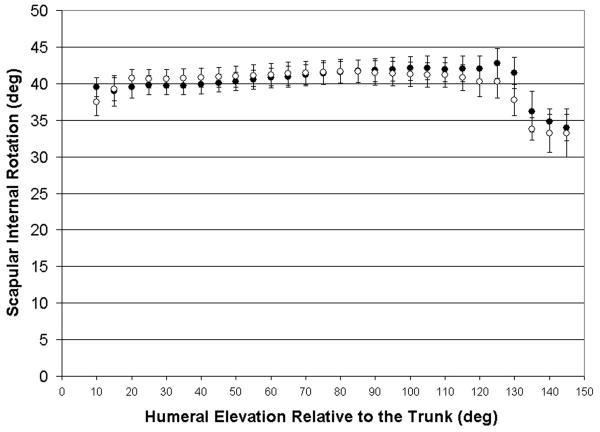
As the arm was raised, the average scapular internal rotation increased from its minimum until the humerothoracic elevation angle reached 125° (Figure 4A). From that point, it decreased until the point of maximum elevation. This pattern was mirrored as the arm was lowered. At 130° of humerothoracic elevation, there was increased scapular internal rotation for arm lowering, followed by a gradual decrease until the minimum humerothoracic elevation. There was no significant difference between raising and lowering the arm for this variable. The minimum value for scapular internal rotation was 33.2° ± 5.2° and the maximum was 42.8° ± 8.7° (p <0.05).
Figure 4A.
Mean scapular internal rotation during humerothoracic elevation with standard error.
●=arm elevation, ○=arm lowering, deg=degrees
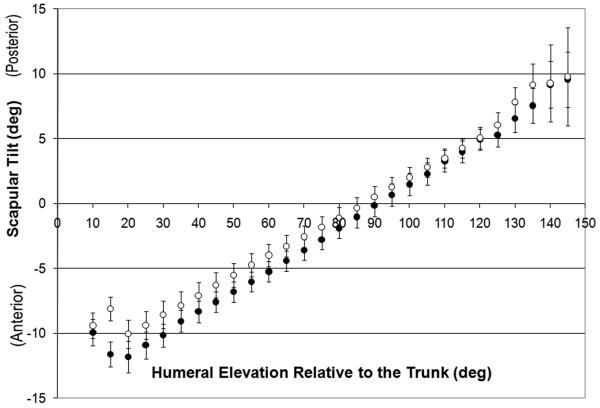
During raising and lowering of the arm, average scapular tilting followed a linear pattern between 20° and the maximum, posteriorly tilting as the angle of humerothoracic elevation increased (Figure 4B). The scapula was maximally tilted 11.8° ± 4.9° anteriorly at 15° of humerothoracic elevation and reached a maximum posterior tilt of 9.8° ± 7.5° at 145° of humerothoracic elevation, resulting in a change of 21.6° of total posterior tilting during overhead reaching of the arm (p < 0.05). Scapular tilting was not significantly different between raising and lowering the arm.
Figure 4B.
Mean scapular tilting during humerothoracic elevation with standard error. Posterior tilting is positive.
●=arm elevation, ○=arm lowering, deg=degrees
Additional Glenohumeral Angular Values
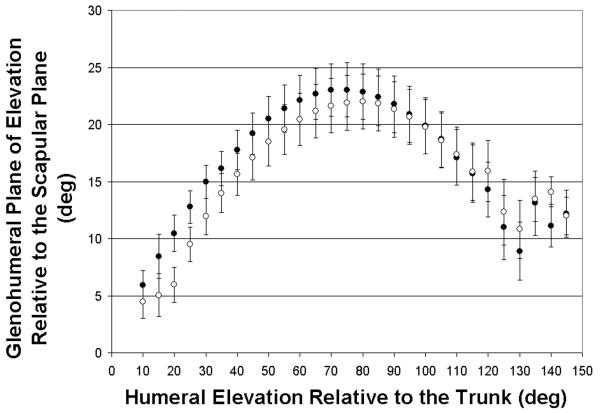
The glenohumeral plane of elevation at the initiation of humerothoracic elevation was slightly anterior to the scapular plane and increased progressively until roughly 70-80° of humerothoracic elevation, reaching a maximum of 23.0° ± 11.6° in front of the plane of the scapula (Figure 5A, significant angular differences, p < 0.05). At 70-80° of humerothoracic elevation, although the humerus continued to be elevated, the plane of glenohumeral elevation moved toward the scapular plane. The minimum glenohumeral plane of elevation was 4.5° ± 4.7° anterior to the scapular plane. The graph for plane of elevation versus humerothoracic elevation had a parabolic shape (Figure 5A). The glenohumeral elevation and lowering motion curves followed this pattern, without significant differences between raising and lowering the arm. Despite the changes in plane of elevation across the total arc of motion, the average glenohumeral plane of elevation remained anterior to the scapular plane throughout the course of both raising and lowering the arm.
Figure 5A.
Mean glenohumeral plane of elevation relative to the scapular plane during humerothoracic elevation with standard error. Anterior to the scapular plane is positive.
●=arm elevation, ○=arm lowering, deg=degrees
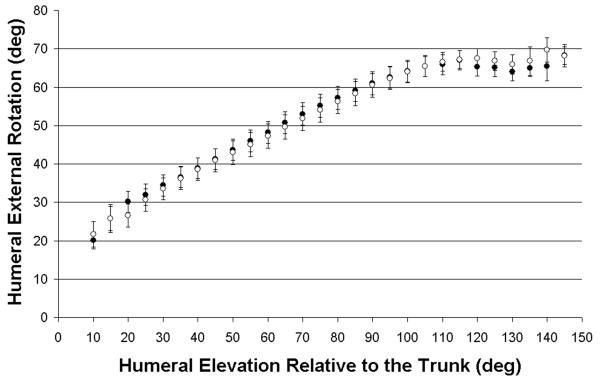
As the arm was elevated from its initial position, the humerus externally rotated with respect to the scapula (Figure 5B). External rotation of the humerus with respect to the scapula plateaued as the arm reached 110° elevation. There was no significant difference in external rotation of the humerus with respect to the scapula between elevation and lowering movements. There was a significant difference between the minimum (20.1° ± 11.4°) and maximum external rotation of the humerus during arm elevation (69.7° ± 6.4°) (p < 0.05).
Figure 5B.
Mean glenohumeral external rotation relative to the scapula during humerothoracic elevation with standard error. External rotation is positive.
●=arm elevation, ○=arm lowering, deg=degrees
Discussion
To fully treat shoulder pathology, it is important to understand three dimensional shoulder motion, since abnormal scapular kinematics are common in various clinical settings.14,26 The profound effect which abnormalities of the scapular rhythm have on the entire shoulder girdle is just beginning to be understood. Overall we found shoulder motion followed a complex but consistent pattern. During elevation, the scapula tilted posteriorly, rotated upward, and rotated externally at the end of the arc of elevation. Concurrently, the humerus elevated and externally rotated relative to the scapula. This rotation of the scapula relative to the thorax has been previously described in the literature.10,18,23 Finally, the plane of humeral elevation relative to the scapular plane increased anteriorly until midway through the elevation, at which point it moved back toward the scapular plane until maximum elevation.
Scapulohumeral rhythm during reaching demonstrated small but significant differences between raising and lowering of the arm overhead, resulting in rejection of the null hypothesis. We found that the ratios between subjects for this range of motion were remarkably well-reproduced, although there tended to be higher standard deviations between subjects during lowering of the arm. Furthermore, we found that the humerus and scapula followed a consistent and predictable pattern of motion relative to each other during overhead reaching. The minimum to 30° increment of motion for raising the arm overhead demonstrated the highest variability. Additionally, it showed the highest ratio in our series. Inman et al8 stated that the 0-30° increment for abduction and the 0-60° increment for flexion were highly variable between subjects and termed it the setting phase. However, they did not provide any ratio data for these setting phases.
Our study found the mean scapulohumeral rhythm from 30° to maximum ranged from 2.3:1 to 2.7:1 when raising and lowering the arm, respectively. We believe that our consistent results are normative data for 3-dimensional overhead reaching that can be used to compare to abnormal scapular kinematics.
The increment of humerothoracic elevation from minimum to 30° proved to have the most variability in our study. Inman et al.8 described similar variability and termed this segment the “setting phase.” However, in Inman et al's study8, there were also differences in the region of variability for forward elevation and abduction. As our study did not control the plane of elevation, this makes direct comparison with prior studies difficult. Doody et al. postulated that the scapula was being stabilized during the early phases of motion when the arm was under the least resistance.4 This may be accurate; however, it may also be true that each individual initiates reaching from a variable scapular rest position or with a different pattern of scapulothoracic muscle activation. After the humerus and scapula are fully engaged, at approximately 30° of humerothoracic elevation, the relationship follows a more consistent pattern. With the exception of the “setting phase,” Inman and his group suggested the glenohumeral joint contributed 2° for every 1° contributed by the scapulothoracic articulation in both abduction and forward elevation. Further studies have led to different conclusions with respect to scapulohumeral rhythm with numbers for the overall ratio ranging from 1.25:1 to 2.5:1.4,5,18,20, 23
Our study has some limitations. First of all, the use of invasive techniques could have caused pain from pin insertion which altered these asymptomatic subjects' shoulder motion. We feel that the subjects' low pain ratings, similar motion ratios, and similar values from non-invasive testing make it highly unlikely that there was any significant alteration of shoulder motion due to pain from the pins. Pin placement, however, did inhibit terminal glenohumeral internal/external rotation in 90° abduction in some subjects, limiting the ability to collect internal/external rotation data on the far end ranges of motion of the shoulder girdle. However, no subjects had limitations in axial rotations of the arm occurring during raising the arm overhead as assessed in this manuscript. Furthermore, there was no bone-marker for thoracic location. Unlike the skin motion over the humerus, clavicle, and scapula, we believe the skin over the sternum is immobile enough to make a skin sensor adequate for location determination. Additionally, this marker is simply a reference point as the sternum is not a moving part of the shoulder girdle during motion. Finally, one could argue that the patient self-selected plane of motion limits the study. In a standard orthopaedic physician assessment, forward flexion range of motion is often assessed as a non-constrained (non-planar) motion overhead.24 The lack of any increase in between subject variation during unconstrained overhead reaching as compared to traditional planar elevation studies4,14,18 suggests that the assessment of unconstrained reaching may be more practical and functional in both the research and clinical settings. Also it is worth noting the average self-selected plane (63°) was slightly closer to a constrained scapular abduction plane of 40° than to a constrained flexion plane of 90°.
Treatment of shoulder pathology requires a solid understanding of the motions of the components of the shoulder girdle during normal activities. The recognition that the scapula has a consistent pattern of motion with shoulder elevation (posterior tilting, upward rotation, and external rotation near the end range of motion) allows a better description of the abnormal motion seen in shoulder pathologies. Numerous studies have tried, in the past, to explore the relationship between the complex motion of the glenohumeral joint and the scapulothoracic articulation. This study sheds further insight into this complex interplay, allowing further understanding and comparison to non-invasive studies which may follow. It is also, to the best of our knowledge, the first study to evaluate scapular rhythm in a subject's self-selected plane, which better mimics the daily activities which are limited by many shoulder pathologies. Furthermore, recognition that there is a difference between the ratios with raising and lowering of the arm may enable better development of eccentric and concentric training programs for improvement of scapular kinematics during recovery from injury and surgery. The higher values determined during lowering the arm may also relate to the anecdotal reporting that excess scapular motion in patients may be easier to observe when patients are lowering rather than raising the arm overhead. Finally, increasing our understanding of the normal movements of the scapula and its relation to the humerus during normal daily activities, such as overhead reaching, could have ramifications for physical therapy programs, post-surgical rehabilitation, and potentially even implant design for pathologies related to abnormal scapular motion. Further research will investigate other motions of the shoulder with other movements, as well as dynamic testing of symptomatic patients.
Acknowledgments
This study was supported by NIH grant # K01HD042491 from the National Institute for Child Health and Human Development (NICHHD). The content is solely the responsibility of the authors and does not reflect the views of NICHHD or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bourne DA, Choo AM, Regan WD, MacIntyre DL, Oxland TR. Three-dimensional rotation of the scapula during functional movements: an in vivo study in healthy volunteers. J Shoulder Elbow Surg. 2007;16:150–162. doi: 10.1016/j.jse.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Bull AM, Berkshire FH, Amis AA. Accuracy of an electromagnetic measurement device and application to the measurement and description of knee joint motion. Proc Inst Mech Eng [H] 1998;212:347–355. doi: 10.1243/0954411981534123. [DOI] [PubMed] [Google Scholar]
- 3.de Groot JH, Brand R. A three-dimensional regression model of the shoulder rhythm. Clin Biomech. 2001;16:735–743. doi: 10.1016/s0268-0033(01)00065-1. [DOI] [PubMed] [Google Scholar]
- 4.Doody SG, Freedman L, Waterland JC. Shoulder movements during abduction in the scapular plane. Arch Phys Med Rehabil. 1970;51:595–604. [PubMed] [Google Scholar]
- 5.Freedman L, Munro RR. Abduction of the arm in the scapular plane: scapular and glenohumeral movements. A roentgenographic study. J Bone Joint Surg Am. 1966;48:1503–1510. [PubMed] [Google Scholar]
- 6.Harryman D, Sidles JA, Harris S. Laxity of the normal glenohumeral joint: A quantitative in vivo assessment. J Shoulder Elbow Surg. 1992;1:66–76. doi: 10.1016/S1058-2746(09)80123-7. [DOI] [PubMed] [Google Scholar]
- 7.Hogfors C, Peterson B, Sigholm G, Herberts P. Biomechanical model of the human shoulder joint – II. The shoulder rhythm. J Biomech. 1991;24:699–709. doi: 10.1016/0021-9290(91)90334-j. [DOI] [PubMed] [Google Scholar]
- 8.Inman VT, Saunders JB, Abbott LC. Observations on the Function of the Shoulder Joint. J Bone Joint Surg. 1944;26:1–26. [Google Scholar]
- 9.Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J Biomech Eng. 2001;123:184–190. doi: 10.1115/1.1351892. [DOI] [PubMed] [Google Scholar]
- 10.Koh TJ, Grabiner MD, Brems JJ. Three-dimensional in vivo kinematics of the shoulder during humeral elevation. J Applied Biomech. 1998;14:312–326. doi: 10.1123/jab.14.3.312. [DOI] [PubMed] [Google Scholar]
- 11.Limpisvasti O, El Attrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg. 2007 Mar;15(3):139–147. doi: 10.5435/00124635-200703000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Lin JJ, Lim HK, Yang JL. Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24:1044–1051. doi: 10.1002/jor.20126. [DOI] [PubMed] [Google Scholar]
- 13.Ludewig PM, Cook TM, Nawoczenski DA. Three-dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J Orthop Sports Phys Ther. 1996;24:57–65. doi: 10.2519/jospt.1996.24.2.57. [DOI] [PubMed] [Google Scholar]
- 14.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 15.Ludewig PM, Cook TM, Shields RK. Comparison of surface and bone-fixed measurement of humeral motion. J Applied Biomech. 2002;18:163–170. [Google Scholar]
- 16.Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91:378–89. doi: 10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–83. doi: 10.2519/jospt.1999.29.10.574. [DOI] [PubMed] [Google Scholar]
- 18.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269–277. doi: 10.1067/mse.2001.112954. [DOI] [PubMed] [Google Scholar]
- 19.McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998;27:125–133. doi: 10.2519/jospt.1998.27.2.125. [DOI] [PubMed] [Google Scholar]
- 20.Mell AG, LaScalza S, Guffey P, Ray J, Maciejewski M, Carpenter JE, Hughes RE. Effect of rotator cuff pathology on shoulder rhythm. J Shoulder Elbow Surg. 2005;14(1 Suppl S):58S–64S. doi: 10.1016/j.jse.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 21.Milne AD, Chess DG, Johnson JA, King GJ. Accuracy of an electromagnetic tracking device: a study of the optimal range and metal interference. J Biomech. 1996;29:791–793. doi: 10.1016/0021-9290(96)83335-5. [DOI] [PubMed] [Google Scholar]
- 22.Pearl ML, Harris SL, Lippitt SB, Sidles JA, Harryman DT, Matsen FA. A system for describing positions of the humerus relative to the thorax and its use in the presentation of several functionally important arm positions. J Shoulder Elbow Surg. 1992;1:113–118. doi: 10.1016/S1058-2746(09)80129-8. [DOI] [PubMed] [Google Scholar]
- 23.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195–201. [PubMed] [Google Scholar]
- 24.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 25.van der Helm FC, Pronk GM. Three-dimensional recording and description of motions of the shoulder mechanism. J Biomech Eng. 1995;117:27–40. doi: 10.1115/1.2792267. [DOI] [PubMed] [Google Scholar]
- 26.Warner JJ, Micheli LJ, Arslanian LE. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moire topographic analysis. Clin Orthop Relat Res. 1992;285:191–199. [PubMed] [Google Scholar]
- 27.Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, et al. International Society of Biomechanics. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]