Abstract
Needleless devices have been developed to provide anesthesia without injections. Little controlled research has examined the acceptability of needleless devices in pediatric patients. The aims of the study were to compare children’s acceptance and preference for one type of needleless jet injection with classical local infiltration as well as to evaluate the efficacy of the needleless anesthesia. Eighty-seven nonfearful children with no previous experience of dental anesthesia were studied using a split-mouth design. The first dental procedure was performed with the classical infiltration anesthesia. The same amount of anesthetic was administered using the INJEX needleless device in a second session 1 week later, during which a second dental procedure was performed. Patients rated their acceptance and preference for the 2 methods, and the dentist recorded data about the need for additional anesthesia. More negative experiences were reported for the INJEX method. Most (73.6%) of the children preferred the traditional method. Among the 87 treatment procedures attempted following the use of INJEX, 80.5% required additional anesthesia, compared with 2.3% of those attempted following traditional infiltration. Traditional infiltration was more effective, acceptable, and preferred, compared with the needleless INJEX.
Keywords: Local anesthesia, Pediatric dental patients, Needleless anesthesia, Needle-free anesthesia
Dentists aim to carry out procedures with as little pain or discomfort as possible. For invasive procedures, pain control is achieved typically by means of injection of local anesthesia. Although this method is highly effective, it is also the dental procedure that is most often associated with anxiety and negative responses.1–4 For some patients, the injection itself is painful, and thus the procedure that is designed to reduce pain may itself result in fear of receiving dental injections in the future.5 Therefore, dental researchers continue to investigate methods of anesthetizing patients that do not involve the needle. A variety of needleless devices have been developed to deliver anesthesia, relying on pressure to force the anesthetic liquid into oral tissues.6–22
In addition to adequate anesthesia, a needleless method should also be acceptable to patients. Further, before it is likely to replace traditional injection, a needleless method should also be preferred by patients. A number of uncontrolled studies of needleless devices have examined adult and child patients, typically focusing on the anesthetic properties of the device used.6,7,9,13,15,16 In these studies, the percent of patients who obtained sufficient anesthesia with the devices ranged from about 50% to about 90%.6,9,13,15,16 In the case where the needleless method was followed by a traditional dental injection, adequate anesthesia was achieved in all of the patients.7 The results are similarly mixed in terms of the patients’ experiences of the needleless methods and their preference for one method over another. However, since the studies were uncontrolled, it is difficult to evaluate the results.
Three controlled studies of needleless devices have been reported. In an experiment, the needleless method (INJEX) seemed to provide faster anesthetic results, though the difference was not significant.20 The participants were described as “volunteers,” which implies that they were adults.
In the second controlled study, 94 patients aged 2 to 16 years who required 2 similar treatments on either side of the mouth received a traditional injection on one side and the needleless injection (Hypospray) on the other side during the same visit. Eighty-one percent of the children stated that they preferred the needleless technique. When the children were dichotomized by age, there was no relationship between age and method preference. The children’s level of cooperation was also not related to preference. About 5% of the children experienced pain with the needleless injection, while about 1% found the traditional injection painful. Gender effects were not reported.8
Finally, a third study compared a needleless device (INJEX) with traditional injections in 19 children aged 4 to 17 years, none of whom were afraid of the needle. Each patient needed 2 restorations. Using a split-mouth design, the patients first received a restoration after anesthesia was delivered using the traditional injection technique. The second restoration was given after anesthesia was delivered with the needleless (INJEX) method. The dentist rated the children’s facial expressions for pain and the overall demeanor of the child, while the child rated the acceptability of the dentist and dental treatment after each restoration. No significant differences were found. The authors note that some patients preferred one method over the other, but did not provide details. No age or gender effects were reported.21
These 3 controlled studies indicate that needleless devices are often successful in controlling pain.8,20,21 The 2 controlled studies in pediatric patients found evidence that children differ in their preference for the needleless versus traditional injection methods. However, there is less information about the acceptability of the needleless method. It is possible that some children might have had less (or no) experience with injections, which might influence their responses to the needleless devices. However, the authors did not report the anesthetic history of the patients. Dental fear might also influence children’s responses to the devices. While the INJEX study21 excluded fearful children, no information was provided for the fear level in the Hypospray study.8 In addition, since adolescents’ coping skills are more advanced than those of young children,23 it is possible that age may be an important variable to examine in a pediatric population. It would be desirable to investigate age more precisely, rather than to dichotomize this variable as was the case in the Hypospray study.8 Finally, as most research indicates that girls are more fearful than boys,5 it is possible that gender differences may impact children’s impressions of the 2 methods.
The aims of our study were to evaluate the efficacy, acceptance, and preference for the 2 methods in a sample in which all children were nonfearful, had not had an injection previously, and had not had anesthesia previously by any other method. The data collection included age and gender information to be able to examine the possible impacts of these variables.
METHODS
This study was carried out before the local university’s dental school had initiated a formal institutional review board. The study occurred in the context of children’s dental care, and therefore prospective parents received complete information about the design and purpose of the study. In addition, parents were told that, because the INJEX device had no needle (Figures 1 and 2), this method of receiving anesthesia might be easier for their child. Parents were also told that the dental procedures would not occur unless their child was sufficiently anesthetized. Further, parents were informed that their participation was voluntary, and that they could decline to permit their child to be in the study without jeopardizing their child’s status as a dental patient for his/her current dental needs or in the future. All prospective parents consented. A simpler description of the study was given to the children, appropriate for their age. They were told that the dentist would like to use 2 different ways to “put your tooth to sleep.” However, the children were not told that one method would involve a needle, to avoid alarming them. All of the children gave assent to be in the study. The participants were not paid for their time. The parents paid the standard dental fees for the dental treatment their children experienced.
Figure 1.
Transferring the anesthetic solution from the standard cartridge to the INJEX system ampoules.
Figure 2.
The INJEX device with the ampoule, ready for application.
This study was carried out in a private pediatric dental practice in Thessaloniki, a large Greek city. A split-mouth design was used in a sample of 87 nonfearful children (41 girls and 46 boys), 6 to 11 years old (mean age 8.37 years) with no previous experience of dental anesthesia or dental injections.
Detailed information about the use and application of the INJEX device in providing dental anesthesia can be found at the manufacturers’ Web site.24 According to this information, the INJEX device may be used on all primary teeth for procedures such as restorations and extractions. However, the mandibular infiltration has been found less effective than the mandibular block for several dental procedures of lower primary molars in children.25,26 Therefore, in this study we included only children whose dental needs involved upper primary molars or upper and lower incisors and canines, where infiltration anesthesia is effective.3
Each patient had at least 3 primary teeth in need of treatment, and at least 2 of these teeth (each one in a different side of the mouth) required similar dental procedures. The procedures were: extraction, Class I or V restoration (single surface restoration of molar or canine), and Class II or III restoration (multiple surface restoration of molar or canine). The 2 teeth that had similar dental treatment requirements (eg, 2 Class I or V restorations) were treated as part of the study during 2 dental visits. The tell-show-do technique was used in all cases. A rubber dam was placed for all restorative procedures. A matrix and a wooden wedge were used for all Class II and III restorations. Most of the study data were gathered during 2 dental visits scheduled a week apart, during which the first 2 teeth were treated. In a third visit a week later, the child was asked to remember the preceding 2 visits and state his/her preference for the method of anesthesia to be used to treat the third tooth.
The first dental procedure was performed with the classical (needle) infiltration anesthesia, as was done in both of the controlled studies which described their methodologies.8,21 At the first visit, the syringe, all of the parts, and the preparation of the injection, but not the needle, were shown to the patient. During the second session, the INJEX needleless device was used. All of the parts and the preparation of the INJEX were presented at this visit. In addition, the pediatric dentist ensured that the child could hear the “popping” sound of the device when the anesthesia was delivered.
Topical anesthetic gel (benzocaine 20% for 2 minutes) was used in both techniques before the delivery of the anesthesia. The local anesthetic used was articaine 4% with epinephrine 1 ∶ 200,000. Mepivacaine 3%, although frequently used in pediatric practice, was not used because it was found to be unsuccessful in achieving pulpal anesthesia with INJEX in adults.22 The INJEX delivery system utilizes an ampoule containing up to 0.3 mL of anesthetic solution at every application. In order to have the same amount of anesthetic with only 1 application, in both techniques (INJEX or needle), 0.3 mL of anesthetic solution was discharged buccally to the apex and 0.1 mL lingually or palatally according to the indications of the specific tooth. For the infiltration application, the amount of anesthesia was measured in the following method: (a) 1 ampoule of articaine 4% with epinephrine 1 ∶ 200,000 contains 1.7 mL of anesthetic solution and, therefore, 0.3 mL is approximately one sixth of the total solution; (b) the length of the ampoule (which contains 1.7 mL of the anesthetic solution, without the plastic part) is 4.8 cm or 48 mm and, therefore, one sixth of this length (0.8 cm or 8 mm) contains 0.3 mL of anesthetic solution; (c) 8 mm was measured from the plastic part of the ampoule using a ruler, and a narrow line was drawn with a permanent marker on the ampoule; (d) a second line was drawn 2 mm from the first one (2-mm length of the ampoule contains approximately 0.1 mL of anesthetic solution). The pediatric dentist administered the local anesthesia buccally using the same technique as was used for all patients in the practice (buccal infiltration anesthesia, 30-gauge and 10-mm needle, slow administration), until the plastic part of the ampoule reached the first line (approximately 0.3 mL). According to the indications of the specific tooth, lingual or palatal anesthesia was delivered subsequently (approximately 0.1 mL, until the second line). For both techniques (needle and INJEX), 5 minutes were allowed to pass after the local anesthesia had been administered before starting any dental procedure.
During both dental appointments, the patient was told to raise his/her left hand in case of pain during treatment. If the patient indicated that he/she was feeling pain, treatment was interrupted, and additional anesthesia was delivered using classical needle infiltration, as was done in previous studies.13,15
In order to ascertain the acceptability of the anesthetic methods, each child was asked 7 questions about each of the 2 methods. To be as consistent as possible with typical procedures used by dentists to ascertain the comfort level of their patients following the administration of anesthesia, the pediatric dentist asked the child these questions. During the first session, wherein the traditional technique was used, when contact of the needle with the oral tissue was achieved but before the actual delivery of anesthesia, the child was asked: “Do you feel any annoyance or pain?” If the child wished to answer “yes,” he/she raised the left hand. After the completion of the first anesthetic procedure, the children were asked 5 questions about their experience. These included: “Did you feel any annoyance or pain while I put your tooth to sleep?”; “Were you afraid while I put your tooth to sleep?”; “Do you feel any pain right now, after I put your tooth to sleep?”; “Do you feel any stinging right now, after I put your tooth to sleep?”; and “Do you have a bad taste right now, after I put your tooth to sleep?” The child answered “yes” or “no” to each question. (In Greek, a distinction is made between “pain” and a sensation not directly translatable into English. The closest approximation is “stinging.” In Greek, the term refers to a highly unpleasant sensation which, nevertheless, is not considered “pain.”) In addition, the dentist noted whether there was any visible bleeding immediately after the anesthesia. On the following day, each child was reached by phone and asked: “Did you have any annoyance or discomfort after your tooth woke up?” The same 7 questions were asked during and after the second anesthetic administration with the INJEX, 1 week later. The dentist also noted the presence or absence of any visible bleeding immediately after the INJEX administration.
During these 2 dental visits, data were also recorded to indicate the type of procedure (extraction, Class I or V restoration, Class II or III restoration), location of anesthetic administration (buccal, lingual, or interproximal), and type of tooth (incisor, canine, upper first molar, or upper second molar). In order to determine the effectiveness of the anesthetic methods, data were also kept to indicate if any additional anesthesia was required.
One week after the second dental visit, the child returned for additional treatment, and was asked: “Which method do you prefer to put your tooth to sleep? The first one, the second one, both the same, or neither one?” This question was designed to measure the child’s preference for method of anesthesia delivery.
Data were analyzed using the SPSS 12.0 edition software. The proportions of children endorsing each of the negative experiences were examined by the binomial test. Comparisons of these proportions across the 2 anesthetic methods were done with McNemar's test. Gender differences for these were examined with chi-square tests. Age differences were tested with t tests. Preference for the method of anesthesia was examined by chi-square test. The relationship between preference and age was examined by an independent samples t test. The need for additional anesthesia following the INJEX administration was assessed by the binomial test. The relationship between dental procedure, type of tooth, and the need for additional anesthesia was tested by chi-square. More detailed relationships between type of tooth, dental procedure, and whether or not additional anesthesia was needed in 3 different aspects of the teeth are reported by number and percent only, as the high frequency of cells with low counts ruled out using chi-square. For all 2 × 2 chi-square tests, Yates correction was used.
RESULTS
1. Acceptance of Anesthetic Methods
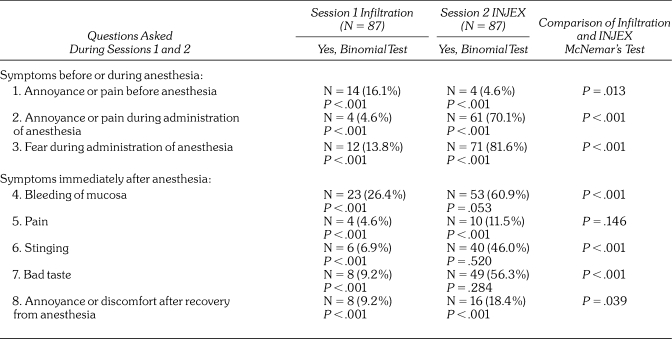
The acceptance of the needle-free jet injection INJEX system for infiltration local anesthesia in comparison with the classical (needle) infiltration anesthesia is presented in Table 1. In general, few children reported any of the negative experiences for the classical (needle) infiltration method (all proportions significantly less than .50, all P values < .001). The most common negative experience was bleeding following the injection, which was experienced by just over 25% of the children. Two of the negative experiences (annoyance or pain during the administration and fear during the administration) were reported by significantly more than 50% of the children following the INJEX administration (P < .001). In addition, there was a trend for significantly more than 50% of the children to have bled following the INJEX administration. A comparison of proportions across both methods revealed that there was no difference in the proportion of children reporting pain immediately after the anesthetic administration. Children were significantly more likely to report annoyance or pain before the administration of anesthesia by the classical (needle) method, compared with the INJEX method (P = .013). Twice as many children reported annoyance or discomfort the following day when the INJEX was used, a difference that was significant at the P < .05 level. Children who received INJEX were significantly more likely to report annoyance or pain during the administration of the anesthetic, fear during the administration, stinging after the administration, and a bad taste after the administration, compared with the classical (needle) condition (all P values < .001). In addition, the dentist noted that the INJEX method resulted in significantly more bleeding (P < .001).
Table 1.
Acceptance of Classical Infiltration Anesthesia and Needle-Free INJEX
Girls were more likely than boys to report bad taste after the classical (needle) method (χ2 = 4.117, df = 1, P = .042). There were no other gender differences for the negative experiences for the classical (needle) method, and none for the INJEX method.
Age was not related to gender. Age was related to fear during administration of anesthesia by the classical method in that younger children were more likely to report fear (t = 1.993, df = 85, P = .049). There was a trend for younger children to report more stinging with the classical method (P = .075). There were no other age differences for the classical method, and none for the INJEX method.
2. Preference for Anesthetic Method
At the third appointment, 64 of the 87 children (73.6%) stated that they preferred the local infiltration with the needle, 11 (12.6%) preferred INJEX, while those who preferred both or none were equally distributed (6 children, or 6.9%, in each group). The preference for classical administration (needle) was significant (χ2 = 110.95, df = 3, P < .001). Gender was not related to preference (χ2 = 1.141, df = 3, P = .767). Age was not related to preference, comparing classical infiltration (needle) versus INJEX only (t = .120, df = 73, P = .905).
3. Effectiveness of INJEX
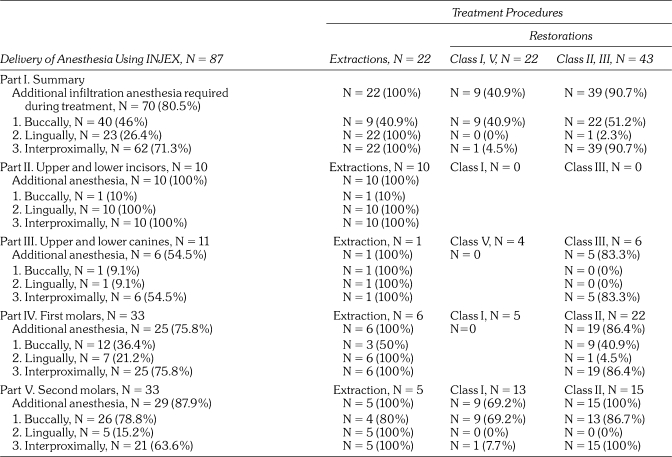
Following the use of INJEX in the second appointment, additional anesthesia (delivered via traditional local infiltration) was required in 70 of 87 cases (80.5%; Table 2, Part I). This was significant by the binomial test (P < .001). Additional anesthesia was required for all of the extractions, most of the Class II and III restorations, and under half of the Class I and V restorations (Table 2, Part I). In particular, extractions and Class II and III restorations were significantly more likely to require the additional anesthesia (χ2 = 30.098, df = 2, P < .001). By contrast, only 2 cases (2.3%) required additional anesthesia in the first treatment session, at which anesthesia had been delivered in the traditional way. Both of these were for extractions.
Table 2.
Anesthetic Effectiveness of Infiltration Anesthesia Using INJEX by Tooth, Aspect, and Type of Treatment
Table 2, Parts II through V, display the need for additional anesthesia separately by type of tooth. These sections of the table also indicate the need for additional anesthesia by type of procedure. Additional anesthesia was needed buccally in approximately equal proportions of extractions, Class I and V restorations, and Class II and III restorations (χ2 = 0.921, df = 2, P = .631). Additional anesthesia was needed lingually significantly more often for extractions, compared with Class I/V and Class II/III restorations (χ2 = 81.978, df = 2, P < .001). Additional anesthesia was needed interproximally for all extractions, 4.5% of Class I and V restorations, and 90.7% of Class II and III restorations. The difference in proportions was significant (χ2 = 81.978, df = 2, P < .001).
The need for additional anesthesia varied significantly by tooth type (incisors, canines, first molars, and second molars; χ2 = 8.747, df = 3, P = .033; Table 2, Parts II–V). Regarding the aspect and type of tooth, additional buccal anesthesia was needed significantly more often for first and second molars, compared with incisors or canines (χ2 = 26.768, df = 3, P < .001). Incisors were significantly more likely to require additional anesthesia lingually, compared with canines, first molars, and second molars (χ2 = 32.152, df = 3, P < .001). There was no significant difference in the proportions of teeth requiring additional anesthesia interproximally (χ2 = 6.797, df = 3, P = .079).
Within the cases that required additional anesthesia, there were significant differences related to the type of tooth and the type of treatment required (χ2 = 38.720, df = 6, P < .001; Table 2, Parts II–V). For example, extractions always needed additional anesthesia regardless of the type of tooth. In cases of Class I or V restorations, additional anesthesia was needed for 69.2% of second molars, while 83.3% of Class III restorations of canines and 86.4% and 100% of Class II restorations of first and second molars, respectively, required additional anesthesia. The detailed results regarding the relationship between dental procedure, type of tooth, and the aspect of the tooth that needed additional anesthesia are presented in Table 2, Parts II through V. Since several of the cells were small, chi-square was not computed.
DISCUSSION
Perhaps the primary reason for development of needleless anesthetic methods is to reduce negative experiences associated with the needle used in traditional infiltration anesthesia.6,8,9,16–19 However, according to the results of this study, these advantages cannot be achieved using INJEX in pediatric patients. In this study, except for annoyance or pain before the actual delivery of anesthesia, in general the needleless system was associated with more negative experiences than the traditional injection technique. When the INJEX was used, a significant percentage of the children reported annoyance or pain and fear during administration of anesthesia, as well as stinging and bad taste immediately after anesthesia; in addition, a small percentage, but twice as many as with the traditional injection, reported annoyance or pain after recovery from anesthesia. Therefore, it is not surprising that the majority of children preferred the traditional technique.
Our results are contrary to other studies, which reported higher levels of acceptance and preference of several needleless injectors other than INJEX (Hypospray, Panjet, Syrijet Mark II, Medajet XL) among mixed populations of children and adults6,7,9,13 or pediatric populations alone.8,15,16 In each of these other needleless devices, the anesthetic delivering segment forms a 45° angle with the main body of the device, while the INJEX system forms a 90° angle.
Acceptance and preference may be associated with the design of the device. According to the information found at the manufacturers’ Web site, the INJEX device may be used on all primary teeth for procedures such as restorations and extractions.24 In order to perform a pain-free extraction of a primary tooth, adequate anesthesia has to be provided in both buccal and lingual aspects of the tooth. Also, for multiple surface restorations of primary molars or canines (Class II or III), the interproximal aspect of the tooth has to be optimally anesthetized (placement of a matrix and a wooden wedge). During this study, in some cases it was difficult to position the device correctly (angle of 90° to the gingival tissue). No problems were noticed during anesthesia of the buccal aspect of the upper and lower anterior primary teeth, while it was almost impossible to adequately use the device for delivering anesthesia on the lingual aspect of these teeth. Also, positioning the device was difficult most often on the buccal aspect of the primary maxillary second molars and the lingual aspect of both the first and second primary maxillary molars. However, no difficulty was noticed in most of the cases for the buccal aspect of the first primary maxillary molar. When the anesthetic delivering segment forms a 45° angle with the main body of the device, this may permit better and easier positioning to the gingival tissue (avoidance of discomfort during positioning the device, proper and complete contact of the entire device’s tip surface with the gingival tissue, which may result in less pressure during administration of anesthesia and less chance of leakage of anesthetic, consequently leading to less bad taste experienced). It is interesting to note that even a device held at a 45° angle may be difficult to position in some areas of the mouth, namely the buccal aspect of maxillary molars and the lingual aspect of the mandibular posterior teeth.13 Thus, it appears that the usefulness of the INJEX system is likely to be limited to those situations in which the device can be positioned at an angle of 90°.
There have been 2 previous controlled studies using INJEX for delivering infiltration anesthesia. However, the first is likely to have been conducted with adults only and does not report patients’ acceptance and preference,20 while the second provides insufficient statistical information regarding preference between traditional and needleless techniques among 19 nonfearful children aged 4 to 17 years.21 These authors report that some children, mainly the younger ones, were apprehensive during administration of needleless injection and some held the hand of their parents, which suggests that some children might have preferred the traditional technique. In addition, a study of different anesthetic agents which used INJEX in adults found that slightly over half of the patients preferred to return to traditional injections in the future, compared with about 18% who preferred the INJEX method.22 Thus, there may be some precedent for the low preference rate we found for the INJEX device.
Despite the differences in design, all needleless systems use pressure to force the anesthetic solution into the tissue very quickly. Because of this, during the delivery of anesthesia a sudden noise and a pressure sensation occur. In this study, a statistically significant percentage of children reported annoyance or pain and fear during administration of anesthesia when INJEX was used. Annoyance or pain is related to the pressure sensation during the administration of anesthesia, and fear may result from the release noise or the pressure. As Geenen et al21 also reported, it is difficult to demonstrate and explain to young children the sensation of the pressure and also the exact noise inside their mouth that the needleless injectors will cause during the administration of anesthesia. These authors reported that some children preferred the needle to the needleless system because of the pressure, and that this was more frequent among younger children. In previous studies, reports from subjects were indicative of fear or pain during receipt of anesthesia via needleless devices (eg, apprehension, “alarm,” “not comfortable,” “little nervous,” “tense, upset,” “afraid,” “panicked,” “scared,” “wary,” “pain during injection,” “fear from the sound of explosion”), which may similarly be due to the pressure or noise.7,9,15–19,21,22,26
In the present study, bleeding of mucosa, stinging and bad taste were significantly higher immediately after anesthesia using INJEX, and a significantly higher percentage of children reported annoyance or discomfort after recovery from anesthesia (self-reported by phone the next day) when INJEX was used. Some of these disadvantages, such as bleeding of mucosa, leakage of anesthetic solution in the oral cavity, and discomfort after anesthesia recovery have also been reported by other authors.6,8,9,15–17,19,21,22 Bleeding of mucosa, stinging immediately after anesthesia, and annoyance or discomfort after recovery are mainly associated with the extremely fast delivery of the anesthetic solution, while the bad taste is due to the difficulty of positioning the device correctly (angle of 90° to the gingival tissue), which results in leaking of the anesthetic into the oral cavity. A study that compared traditional injection with INJEX found that children preferred the former because it was less likely to be associated with a bad taste; however, the authors do not report the location of the teeth treated.21
According to the results of this study, age and gender were not related to acceptance or preference of either anesthesia method. This is consistent with the findings of Schmidt,8 who reported no age differences on method preference, and with those of Saravia and Bush,15 who reported no gender differences on preference. In our sample, a significantly higher percentage of younger children reported fear during administration of anesthesia using the classical technique. This may be explained by the previously noted tendency of individuals to fear dental injections.1–4
In addition to performing less successfully in terms of patient acceptance and preference, the INJEX method was also associated with the inability to achieve anesthetic success, frequently requiring additional anesthesia with the traditional infiltration technique in order to complete the dental treatment. Among the 87 treatment procedures attempted following the use of INJEX, 80.5% required additional anesthesia. Delivery of anesthesia at the buccal aspect of the tooth was partially effective. It was more effective for the anterior than the posterior teeth, and more effective for simple restorations than more complex ones or extractions. Therefore, it can be speculated that delivery of buccal anesthesia using INJEX was effective for soft tissue anesthesia (placement of the rubber dam), but only partially effective for pulpal anesthesia (tooth preparation) and surgical procedures (extractions). The completion of treatments in relation to anesthetic delivery at the lingual and interproximal aspects of the tooth using INJEX was found low except on Class I and V restorations on primary first upper molars and canines, respectively. Therefore, delivery of lingual and interproximal anesthesia using INJEX was partially effective for soft tissue procedures (ability for placement of rubber dam but not for matrix and wooden wedge during Class II and III restorations), but not effective for surgical procedures (extractions).
These findings are in contrast to other studies, which reported higher effectiveness of several needleless injectors.6–9,13,15,16 In each of these studies, the devices’ anesthetic delivering segments form a 45° angle with the main body of the device, permitting better positioning to the gingival tissue, and therefore achieving more adequate anesthesia. Both controlled studies using INJEX report that the system provided adequate anesthesia. However, in one of the studies only maxillary incisors were studied and the type of treatment, if any, is not stated,20 while in the other study, restorations but not extractions were performed and no information is given regarding the type of teeth treated.21 In the present study, the ability to complete the dental treatment using INJEX for delivering anesthesia was found to be higher for those teeth where it was not difficult to position the device properly at the different aspects of the tooth. Therefore, according to the results of this study, using INJEX as a main technique of local anesthesia can be effective for the buccal aspect of upper and lower primary incisors and canines, partially effective for the buccal aspect, but limited to soft tissue anesthesia for the lingual aspect of maxillary primary molars, and ineffective for the lingual aspect of upper and lower incisor teeth.
The amount and concentration of the anesthetic solution, as well as the amount of vasoconstrictor, affect the anesthetic result. For example, a study using Syrijet found that lidocaine at 5% was more effective than at 2% concentration.13 In general, different concentrations and types of anesthetic solutions have been reported (usually lidocaine 2% or articaine 4% with 1 ∶ 50,000–200,000 epinephrine). A study of adult patients receiving anesthesia via INJEX found that mepivacaine 3% did not achieve pulpal anesthesia in any of the patients, while the administration of lidocaine with epinephrine produced pulpal anesthesia in 64% of them.22 In a study using INJEX on 19 children aged 4 to 17 years, the effectiveness of 0.3 mL of anesthetic solution was found to be high. However, the type of anesthesia is not reported.21 In another study using INJEX, maxillary incisors were effectively anesthetized with 0.6 mL of articaine 4%, with 1 ∶ 200,000 epinephrine. However, because the anesthetic delivery ampoule of the system contains up to only 0.3 mL, it can be assumed that 2 applications were delivered.20 According to the present study, 0.3 mL of articaine 4%, 1 ∶ 200,000 epinephrine delivered at the buccal aspect, and 0.1 mL at the lingual aspect of the tooth by the traditional technique were effective for completion of the dental procedures performed on all but 2 primary teeth. Therefore, the amount and type of infiltration anesthetic used in this study was adequate to complete the dental treatment. By contrast, delivering the same amount of anesthetic with INJEX was not as effective. This was most likely due to the difficulty of correctly positioning the device on the gingival tissue, which resulted in insufficient delivery of the anesthesia to the intended area.
The design of our study required that all children received the traditional infiltration technique during their first treatment. It is well known that pain due to inadequate anesthesia can result in the development of dental fear.1–5 The patients in our study had never experienced any local anesthesia in their mouth and needed multiple dental visits in order to complete dental treatment. Thus, to avoid the development of dental fear, for ethical reasons the administration of the highly efficacious infiltration anesthesia was always delivered during the first visit. Similarly, both of the controlled studies using INJEX, which described their methodology, administered traditional anesthesia first.8,21 Nevertheless, it is possible that our design—which restricted recruitment to children who had never had a traditional filtration anesthetic and which required that children receive the 2 methods in the same order—may have influenced the patients’ acceptance and preference for the traditional technique. It is interesting to note that, although younger patients were significantly more likely to experience fear during the traditional injection, age was not related to method preference. Thus, their initial injection experience (with the needle) may not have biased their overall comparison of the 2 methods. In addition, one study found that more adults (who presumably have experienced traditional injections in the past) preferred to return to the traditional method, rather than the INJEX.22
Our study found that children aged 6 to 11 years preferred the traditional needle injection over the INJEX method. While we did not find gender or age differences, it is possible that these might be found with children of other ages. In addition, it is important to note that our sample was restricted to children who had never received anesthesia before, and who were also previously rated as nonfearful. It is possible that needle-phobic children might respond more favorably to needleless methods, and future studies should examine this. With regard to the INJEX device, which requires placement at a 90° angle to the tissue, and therefore seems to be linked to the need for additional administrations of anesthetic for many dental procedures, it would be important to determine whether fearful children do better with one traditional injection of anesthesia, compared with 2 or more needleless administrations in order to achieve sufficient anesthesia.
REFERENCES
- 1.Pinkham J. R. Patient management. In: Pinkham J. R., Casamassimo P. S., Fields H. W., McTigue D. J., Nowak A. J., editors. Pediatric Dentistry: Infancy Through Adolescence. 4th ed. St Louis, Mo: Elsevier Saunders; 2005. pp. 394–413. [Google Scholar]
- 2.Milgrom P., Coldwell S. E., Getz T., Weinstein P., Ramsay D. S. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–766. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 3.McDonald R. E., Avery D. R. Local anesthesia for the child and adolescent. In: McDonald R. E., Avery D. R., editors. Dentistry for the Child and Adolescent. 6th ed. St Louis, Mo: CV Mosby Co; 2000. pp. 294–306. [Google Scholar]
- 4.ten Berge M., Veerkamp J. S. J., Hoogstraten J., Prins P. J. M. Childhood dental fear in the Netherlands: prevalence and normative data. Community Dent Oral Epidemiol. 2002;30:101–107. doi: 10.1034/j.1600-0528.2002.300203.x. [DOI] [PubMed] [Google Scholar]
- 5.Milgrom P., Weinstein P., Getz T. Treating Fearful Dental Patients: A Patient Management Handbook. 2nd ed. Seattle, Wash: University of Washington Continuing Dental Education; 1995. [Google Scholar]
- 6.Margetis P., Quarantillo E., Lindberg R. Jet injection of local anaesthesia in dentistry. U S Armed Forces Med J. 1958;9:625–634. [PubMed] [Google Scholar]
- 7.Kutscher A. H., Zegarelli E. V., Cain E. A., Portway T., Block P., Brottman S. Jet injection as a means of obtaining oral mucosal anesthesia: a preliminary report. J Oral Surg Anesth Hosp Dent Serv. 1964;22:310. [PubMed] [Google Scholar]
- 8.Schmidt D. A. Anesthesia by jet-injection in the practice of pedodontics. J Dent Child. 1966;33:340–345. [PubMed] [Google Scholar]
- 9.Bennett C. R., Monheim L. M. Production of local anesthesia by jet injection. A clinical study. Oral Surg Oral Med Oral Pathol. 1971;32:526–530. doi: 10.1016/0030-4220(71)90315-x. [DOI] [PubMed] [Google Scholar]
- 10.Greenfield W., Karpinski J. F. Clinical application of jet injection to comprehensive pain control. Anesth Prog. 1973;20:110–112. [PMC free article] [PubMed] [Google Scholar]
- 11.Tabita P. V. Side effect of the jet injector for the production of local anesthesia. Anesth Prog. 1979;26:102–104. [PMC free article] [PubMed] [Google Scholar]
- 12.Lehtinen R. Efficiency of jet injection technique in production of local anesthesia. Proc Finn Dent Soc. 1979;75:13–14. [PubMed] [Google Scholar]
- 13.Lambrianidis T., Rood J. P., Sowray J. H. Dental analgesia by jet injection. Br J Oral Surg. 1980;17:227–231. [Google Scholar]
- 14.Sowray J. H. Recent advances in jet injection. Int J Oral Surg. 1981;10(suppl 1):143–145. [PubMed] [Google Scholar]
- 15.Saravia M. E., Bush J. P. The needleless syringe: efficacy of anesthesia and patient preference in child dental patients. J Clin Pediatr Dent. 1991;15:109–112. [PubMed] [Google Scholar]
- 16.Munshi A. K., Hegde A., Bashir N. Clinical evaluation of the efficacy of anesthesia and patient preference using the needle-less jet syringe in pediatric dental practice. J Clin Pediatr Dent. 2000;25:131–136. doi: 10.17796/jcpd.25.2.q6426p853266q575. [DOI] [PubMed] [Google Scholar]
- 17.Wong J. K. Adjuncts to local anesthesia: separating fact from fiction. J Can Dent Assoc. 2001;67:391–397. [PubMed] [Google Scholar]
- 18.Ram D., Peretz B. Administering local anaesthesia to paediatric dental patients—current status and prospects for the future. Int J Paediatr Dent. 2002;12:80–89. doi: 10.1046/j.1365-263x.2002.00343.x. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins J. M., Moore P. A. Local anesthesia: advances in agents and techniques. Dent Clin North Am. 2002;46:719–732. doi: 10.1016/s0011-8532(02)00020-4. [DOI] [PubMed] [Google Scholar]
- 20.Saleh G., Raab W. H-M. Efficiency of a needle-free injector-system for dental local anesthesia. J Dent Res. 2002;81:A-188. [Google Scholar]
- 21.Geenen L., Marks L. A. M., Martens L. C. Evaluation clinique du système INJEX®, un système d’anesthésie locale sans aiguille: une etude d’évaluation de confort. Rev Belge Med Dent. 2004;59:149–155. [PubMed] [Google Scholar]
- 22.Dabarakis N. N., Alexander V., Tsirlis A. T., Parissis N. A., Nikolaos M. Needle-less local anesthesia: clinical evaluation of the effectiveness of jet anesthesia Injex in local anesthesia in dentistry. Quintessence Int. 2007;38(10):E572–576. [PubMed] [Google Scholar]
- 23.Fields L., Prinz R. J. Coping and adjustment during childhood and adolescence. Clin Psychol Rev. 1997;17:937–976. doi: 10.1016/s0272-7358(97)00033-0. [DOI] [PubMed] [Google Scholar]
- 24.INJEX: Needle-free injection systems. http://yourdent.co.il/files/Injex_needle-free-injection-systems.pdf. Accessed January 6, 2010.
- 25.Wright G. Z., Weinberger S. J., Marti R., Plotzke O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatr Dent. 1991;13:278–283. [PubMed] [Google Scholar]
- 26.Oulis C. J., Vadiakas G. P., Vasilopoulou A. The effectiveness of mandibular infiltration compared to mandibular block anesthesia in treating primary molars in children. Pediatr Dent. 1996;18:301–305. [PubMed] [Google Scholar]