Abstract
OBJECTIVE
To determine whether evidence-based socioculturally adapted collaborative depression care improves receipt of depression care and depression and diabetes outcomes in low-income Hispanic subjects.
RESEARCH DESIGN AND METHODS
This was a randomized controlled trial of 387 diabetic patients (96.5% Hispanic) with clinically significant depression recruited from two public safety-net clinics from August 2005 to July 2007 and followed over 18 months. Intervention (INT group) included problem-solving therapy and/or antidepressant medication based on a stepped-care algorithm; first-line treatment choice; telephone treatment response, adherence, and relapse prevention follow-up over 12 months; plus systems navigation assistance. Enhanced usual care (EUC group) included standard clinic care plus patient receipt of depression educational pamphlets and a community resource list.
RESULTS
INT patients had significantly greater depression improvement (≥50% reduction in Symptom Checklist-20 depression score from baseline; 57, 62, and 62% vs. the EUC group's 36, 42, and 44% at 6, 12, and 18 months, respectively; odds ratio 2.46–2.57; P < 0.001). Mixed-effects linear regression models showed a significant study group–by–time interaction over 18 months in diabetes symptoms; anxiety; Medical Outcomes Study Short-Form Health Survey (SF-12) emotional, physical, and pain-related functioning; Sheehan disability; financial situation; and number of social stressors (P = 0.04 for disability and SF-12 physical functioning, P < 0.001 for all others) but no study group–by–time interaction in A1C, diabetes complications, self-care management, or BMI.
CONCLUSIONS
Socioculturally adapted collaborative depression care improved depression, functional outcomes, and receipt of depression treatment in predominantly Hispanic patients in safety-net clinics.
Diabetes is associated with a twofold higher risk of comorbid depression compared with the general population, with rates among Hispanics as high as 33% (1). Greater risk of cardiovascular illness, functional disability, mortality, and health service use is found among Hispanics with comorbid depression and diabetes, which is particularly important because Hispanics have a higher prevalence of diabetes compared with non-Hispanic whites (2). Moreover, among diabetic patients, depression is often persistent and severe (2), and among Hispanics, difficulty with diabetes management can contribute to depression (3). However, Hispanics are less likely to be diagnosed or to receive depression care and have lower utilization rates and greater risk of discontinuing antidepressants during the first 30 days of treatment because of side effects, socioeconomic barriers, and cultural preferences for psychotherapy (4).
Glycemic control is worse and complications are high among Hispanics with diabetes (5), in part, explained by inadequate medical and self-care and cultural and economic factors (6). Comorbid depression and diabetes may significantly worsen the course of both disorders, leading to higher complication and mortality rates (7) and total health care expenditures (8). Depression may worsen diabetes outcomes via neurobiological mechanisms (9) and poor adherence to self-care regimens (10). In some, but not all, trials, glucose control has been shown to improve with depression treatment; however, the prevalence of undiagnosed or untreated depression among all diabetic subjects is high (11).
This randomized clinical trial implemented a health services effectiveness trial design to test a collaborative care model aimed at increasing exposure of low-income, predominantly Hispanic diabetic patients (15 non-Hispanics) with comorbid depression to evidenced-based depression psychotherapy and/or pharmacotherapy to examine both depression care receipt and outcomes compared with usual care. We hypothesized that the intervention (INT group) versus enhanced usual care (EUC group) would be associated with improved depressive symptom outcomes, functioning, quality of life, and A1C levels at 6, 12, and 18 months. Sociocultural adaptations (12,13) were aimed at enhancing patient depression treatment engagement and adherence; reducing individual, provider, and system barriers to care; integrating depression and diabetes care; and providing culturally and linguistically competent care.
RESEARCH DESIGN AND METHODS
The study, approved by the University of Southern California Institutional Review Board, was conducted in public community clinics, one of which provides usual primary care, whereas the other offers diabetic patients referred by clinic primary care physicians (PCPs) a program in which diabetes nurse educators provide care coordination, monitoring, and self-management education. Trained bilingual study recruiters identified diabetic patients from medical charts. Patients provided verbal consent to depression symptom screening; eligible patients provided written informed trial consent. Randomization was conducted via a computer-generated random number in blocks of 10, with random assignment number enclosed in sealed envelopes; patients selected one of five sequential envelopes following baseline interview. Clinic PCPs and nursing staff attended a depression treatment didactic session by the study psychiatrist at study onset and a refresher midway.
Intervention model
Key elements in the Multifaceted Diabetes and Depression Program are based on evidence-based practice guidelines for primary care and are responsive to known barriers to treatment among patients in public safety-net clinics. The structured stepped-care algorithm 12-month intervention included 1) problem-solving therapy (PST) provided by bilingual graduate social work diabetes depression clinical specialists (DDCSs) and/or antidepressant medications prescribed by the treating PCP; 2) DDCS monthly telephone follow-up symptom monitoring, treatment maintenance, and relapse prevention; and 3) care and service system navigation by the DDCS and an assistant patient navigator. A psychiatrist and principal investigator (K.E.) provided weekly telephone DDCS supervision, and, if requested, the psychiatrist provided PCP antidepressant medication telephone consultation.
The algorithm was modeled after previous studies (12,13) and aimed to ensure that patients received depression treatment consistent with their preference, clinical presentations, and responses over time. The algorithm included the following: step 1 (weeks 1–8): based on patient preference, patients start PST or antidepressant medication (usually a selective serotonin reuptake inhibitor titrated gradually to therapeutic dose); step 2 (weeks 9–12): patients with partial/nonresponse receive a different antidepressant medication or the addition of antidepressant medication or PST; step 3: patients with full response move to monthly maintenance/relapse prevention telephone monitoring. Nonresponsive patients were considered for additional PST, augmentation of low-dose Trazodone for insomnia, and referral to specialty mental health care.
Sociocultural enhancements (13) included psychoeducation to dispel treatment misconceptions, reduce stigma, and enhance therapeutic alliance; patient choice of first-line medication or PST and family participation; 8–12 PST sessions (plus booster sessions if indicated and a PST open-ended patient support group available up to 12 months posttreatment); PST sessions tailored for literacy and idiomatic content and linking PST problem-solving skills training to enhance diabetes and depression self-management and coping with socioeconomic stress; and patient navigation assistance to facilitate patient-provider communication and financial and social resource access.
Enhanced usual care
EUC patients received standard clinic care and in addition were given patient- and family-focused depression educational pamphlets (Spanish or English) and a community, financial, social services, transportation, and child care resource list. EUC group PCPs were informed of patient depression diagnoses and study participation and could prescribe antidepressant medications or refer patients to community mental health care. Patients could seek mental health treatment.
Data collection
The 20-item Symptom Checklist Depression Scale (SCL-20) (14) was used as a reliable and valid measure of depression in medical populations that has been shown to be sensitive to change in primary care studies (Cronbach α = 0.91). The Patient Health Questionnaire-9 (PHQ-9) was used because it provides a dichotomous diagnosis of major depression, provides a continuous severity score, and has been found to have 73% sensitivity and 98% specificity to a diagnosis of probable major depressive disorder based on structured psychiatric interview (15,16). Thus, patients with a score of ≥10 are considered to have clinically significant depressive symptoms. Two standard questions from the Structured Clinical Interview for DSM-IV were used to assess dysthymia. The Sheehan Disability Scale was used to rate functional impairment on a 10-point Likert scale (17). Health-related quality of life was assessed using the Medical Outcomes Study Short-Form Health Survey (SF-12) Physical and Mental Component Summary norm-based scores standardized to the general U.S. population with a mean (± SD) of 50 ± 10. The SF-12 includes one measure of pain impact that asks respondents to rate pain interference with normal work on a scale (none 1, extreme 5). The Brief Symptom Inventory (18) assessed anxiety. The Summary of Diabetes Self-Care Activities Questionnaire assessed self-reported adherence (19). Diabetes symptoms were assessed using the Whitty 9-item questionnaire, which has been demonstrated to change over time with effective diabetes treatment (20). A1C was obtained from medical records with baseline A1C (last test done before enrollment) and follow-up A1C (last test done within 3 months of each postenrollment outcome); antidepressant medication prescriptions were monitored via medical records and self-report. Also assessed were self-reported weight and height (BMI), diabetes complications, comorbid medical illness, and socioeconomic stress (financial situation, work, unemployment, financial problems, marital/family conflicts, legal and care-giving problems, and community violence worry).
Statistical methods
Intent-to-treat analysis was conducted to evaluate intervention effects. Clinically meaningful improvement of depressive symptoms was assessed as a ≥50% reduction in baseline SCL-20 or PHQ-9; depression remission was assessed by SCL-20 <0.5 or PHQ-9 <5. Logistic regression models were conducted to compare the odds of achieving clinically meaningful improvement (≥50% decrease in depressive symptoms), remission of depressive symptoms, or persistent major depression between enhanced usual care and the intervention at 6-, 12-, and 18-month follow-up. General linear mixed-effects models implemented in SAS Proc Mixed procedure were fitted with longitudinal data from baseline to 18 months to evaluate intervention effects on functional, socioeconomic, and clinical outcomes (21). Unstructured covariance was specified in the mixed-effects model to account for within-patient correlations of repeated observations over time. Fixed effects of time, study group, and their interactions were examined. Both logistic regression and linear mixed-effects models were adjusted for clinic site, baseline depression severity (PHQ-9 score <15 vs. ≥15) and dysthymia, birth place, language, and years in the U.S. (<10 vs. ≥10). Two sensitivity analyses, with the first excluding non-Hispanics and the second excluding type 1 diabetic patients, were conducted. Analyses used SAS software version 9.1 (SAS Institute, Cary, NC).
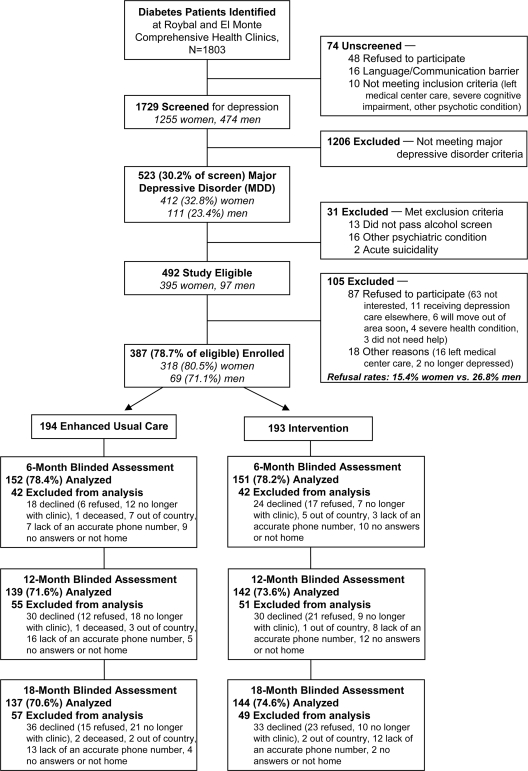
Follow-up study attrition did not vary between groups (21.6% in the EUC group vs. 21.8% in the INT group at 6 months, 28.4% in the EUC group vs. 26.4% in the INT group at 12 months, and 29.4% in the EUC group vs. 25.4% in the INT group at 18 months) or in patients refusing continuing trial participation or no longer receiving care at clinics (10.9, 15.5, and 17.9% at 6, 12, and 18 months, respectively) (Fig. 1). Baseline depression, quality-of-life clinical outcomes, and most demographics were similar between attrition and retention groups. Hot-deck imputation as well as multiple imputations with the predictive model–based approach were implemented in SOLAS software version 3.2 (Statistical Solution, Saugus, MA). Imputed data for depression improvement and functional and clinical outcomes were consistent with results analyzed with all available data, so we report the latter. With 130 patients per group, 80% power was projected to detect a minimum 10% absolute difference in response rates with a two-tailed α level of 0.05. Enrolling 350 patients allowed a 30% attrition rate.
Figure 1.
Study consort chart.
Intervention costs were measured as actual budget-based cost (not charges) for all DDCS and patient navigator services, using actual salary plus 32% fringe benefits. Resulting unit costs were $71 per patient visit (90 min), $35 per DDCS telephone follow-up (45 min), and $10 for each patient navigation call (10–15 min). Estimates included record-keeping time. Additional costs included $10 for relaxation tape, $136 per patient for DDCS communication with PCP, and $21 per patient for clinical supervision.
RESULTS
Sample
Study eligible patients with diabetes were aged ≥18 years and endorsed one of two cardinal depression symptoms more than half the days to nearly every day and scored ≥10 on the PHQ-9, indicating a high likelihood of clinically significant depression. Exclusion criteria were acute suicidal ideation, a score of ≥8 on the Alcohol Use Disorders Identification Test alcohol assessment, recent lithium/antipsychotic medication use, and inability to speak English or Spanish. Of 1,803 diabetic patients, 1,729 (95.8%) were screened (1,255 [72.6%] female); 30% met depression criteria (female 32.8% vs. male 23.4%, P < 0.001). Excluding patients meeting alcoholism criteria, acute suicidality, or other psychiatric condition, enrollment was 80.5% female and 71.1% male (P = 0.04). Of 387 (78.7%) enrolled patients (15 were non-Hispanic), 193 were randomized to the INT group and 194 to the EUC group (Fig. 1).
Baseline demographic, clinical, and functional characteristics are summarized in Tables 1 and 2. Patients were predominantly Latina, foreign born, in the U.S. ≥10 years, unemployed, and had not completed high school. Nearly 98% of patients had type 2 diabetes (eight had type 1 diabetes). Mean A1C levels were 9.05% in the EUC group and 9.01% in the INT group; 80% in the EUC group and 86% in the INT group had one or more diabetes complications. Over 60% had BMIs ≥30 kg/m2 and 83% had one or more comorbid medical conditions. Over 50% of patients had moderate to severe depression (PHQ-9 ≥15); nearly 19% reported a history of depression. Patients from the two study clinics varied significantly with respect to birth place, language use, diabetes treatment, mean A1C levels, self-care management, comorbid medical illness, socioeconomic stress, and depression score.
Table 1.
Baseline characteristics
| Enhanced usual care | Intervention | P * | |
|---|---|---|---|
| n | 194 | 193 | |
| Demographics | |||
| Female | 164 (84.5) | 154 (79.8) | 0.22 |
| Hispanic | 189 (97.4) | 183 (94.8) | 0.18 |
| Aged ≥50 years | 134 (69.1) | 145 (75.1) | 0.18 |
| Foreign born | 182 (93.8) | 170 (88.1) | 0.05 |
| Living in the U.S. ≥10 years | 169 (87.1) | 181 (94.3) | 0.02 |
| Spanish speaking | 175 (90.2) | 152 (78.8) | 0.002 |
| Less than high school education | 166 (85.6) | 151 (78.2) | 0.06 |
| Unemployed | 146 (75.3) | 157 (81.3) | 0.15 |
| Married | 97 (50.0) | 94 (48.7) | 0.80 |
| Study site | |||
| El Monte | 80 (41.2) | 88 (45.6) | 0.39 |
| Roybal | 114 (58.8) | 105 (54.4) | |
| Health insurance/benefits | |||
| Medi-Cal/Medicare | 36 (18.6) | 34 (17.6) | 0.24 |
| County-funded program | 113 (58.2) | 118 (61.1) | |
| None | 41 (21.1) | 41 (21.2) | |
| Socioeconomic stress | |||
| Financial situation getting worse | 59 (30.4) | 83 (43.0) | 0.01 |
| Number of social stressors | 3.15 ± 2.38 | 4.31 ± 2.70 | <0.001 |
| Clinical characteristics | |||
| Forms of diabetes | |||
| Type 1 diabetes | 6 (3.1) | 2 (1.0) | 0.16 |
| Type 2 diabetes | 188 (96.9) | 191 (99.0) | |
| Diabetes duration (years) | 7.97 ± 7.35 | 8.34 ± 7.20 | 0.62 |
| Diabetes treatment | |||
| Oral medication | 139 (71.6) | 129 (66.8) | 0.27 |
| Insulin | 28 (14.4) | 26 (13.5) | |
| Insulin plus oral medication | 20 (10.3) | 33 (17.1) | |
| Diet alone or none | 7 (3.6) | 5 (2.6) | |
| Diabetes complications | |||
| None | 38 (19.6) | 27 (14.0) | 0.36 |
| One | 82 (42.3) | 78 (40.4) | |
| Two | 48 (24.7) | 58 (30.1) | |
| Three or more | 26 (13.4) | 30 (15.5) | |
| Diabetes self-management† | 3.37 ± 1.45 | 3.39 ± 1.45 | 0.89 |
| Whitty-9 diabetes symptoms | 2.15 ± 0.75 | 2.33 ± 0.76 | 0.02 |
| A1C ≥7% | 153 (82.3) | 156 (83.0) | 0.85 |
| BMI ≥30 kg/m2 | 114 (59.4) | 118 (61.8) | 0.63 |
| Comorbid medical illness‡ | 156 (80.4) | 165 (85.5) | 0.18 |
| Sheehan Disability Scale of functional impairment | 5.74 ± 2.84 | 6.30 ± 2.67 | 0.05 |
| Chronic pain | 51 (26.3) | 75 (38.9) | 0.01 |
| Taking pain medication | 40 (20.6) | 63 (32.6) | 0.01 |
| Depression SCL-20 | 1.41 ± 0.70 | 1.70 ± 0.73 | <0.001 |
| Dysthymic disorder | 95 (49.0) | 119 (61.7) | 0.01 |
| History of major depression | 29 (14.9) | 45 (23.3) | 0.04 |
| Taking psychotropic medication | 25 (12.9) | 36 (18.7) | 0.12 |
| Depression/anxiety counseling§ | 20 (10.3) | 29 (15.0) | 0.16 |
Data are means ± SD or frequency (%).
*t test for continuous data or χ2 test for categorical data.
†Diet, exercise, blood glucose testing, and foot care.
‡Hypertension; arthritis; or eye, gastrointestinal, kidney, or heart disease.
§Received from a doctor, social worker, or psychologist, some of whom were also taking psychotropic medication.
Table 2.
Receipt of depression care and clinical, functional, and socioeconomic outcomes
| Enhanced usual care | Intervention | P * | Time-by-group interaction, P* | |
|---|---|---|---|---|
| Antidepressant receipt | NA | |||
| Baseline | 24 (12.7) | 36 (18.9) | 0.08 | |
| Over 12 months | 52 (26.8) | 113 (58.5) | <0.001 | |
| 18-month follow-up | 27 (19.7) | 52 (36.1) | 0.002 | |
| PST or counseling receipt | NA | |||
| Baseline | 20 (10.3) | 29 (15.0) | 0.11 | |
| Over 12 months | 26 (13.4) | 153 (79.3) | <0.001 | |
| 18-month follow-up | 17 (12.4) | 35 (24.3) | 0.01 | |
| Any depression treatments | NA | |||
| Baseline | 30 (15.5) | 43 (22.3) | 0.07 | |
| Over 12 months | 63 (32.5) | 162 (83.9) | <0.001 | |
| 18-month follow-up | 33 (24.1) | 66 (45.8) | <0.001 | |
| Response (50% SCL-20 reduction) | NA | |||
| 6-month follow-up | 55 (36.4) | 86 (57.0) | <0.001 | |
| 12-month follow-up | 59 (42.4) | 88 (62.0) | <0.001 | |
| 18-month follow-up | 60 (43.8) | 89 (61.8) | <0.001 | |
| Remission (SCL-20 <0.5) | NA | |||
| 6-month follow-up | 42 (27.8) | 58 (38.4) | 0.01 | |
| 12-month follow-up | 49 (35.3) | 56 (39.4) | 0.09 | |
| 18-month follow-up | 48 (35.0) | 58 (40.3) | 0.04 | |
| A1C | 0.93 | |||
| Baseline | 9.05 ± 2.22 | 9.01 ± 2.15 | 0.98 | |
| 6-month follow-up | 8.42 ± 2.00 | 8.45 ± 2.06 | 0.85 | |
| 12-month follow-up | 8.59 ± 2.26 | 8.52 ± 2.01 | 0.98 | |
| 18-month follow-up | 8.50 ± 2.17 | 8.34 ± 2.04 | 0.57 | |
| Whitty-9 diabetes symptoms | <0.001 | |||
| Baseline | 2.15 ± 0.75 | 2.33 ± 0.76 | 0.07 | |
| 6-month follow-up | 1.79 ± 0.65 | 1.65 ± 0.59 | 0.003 | |
| 12-month follow-up | 1.69 ± 0.56 | 1.66 ± 0.57 | 0.18 | |
| 18-month follow-up | 1.74 ± 0.64 | 1.79 ± 0.71 | 0.85 | |
| Sheehan Disability Scale of functional impairment | 0.04 | |||
| Baseline | 5.74 ± 2.84 | 6.30 ± 2.67 | 0.47 | |
| 6-month follow-up | 3.55 ± 2.90 | 3.07 ± 2.93 | 0.01 | |
| 12-month follow-up | 3.17 ± 3.04 | 2.93 ± 3.12 | 0.06 | |
| 18-month follow-up | 3.18 ± 2.89 | 3.28 ± 3.13 | 0.40 | |
| Pain impact | <0.001 | |||
| Baseline | 2.66 ± 1.34 | 2.91 ± 1.24 | 0.22 | |
| 6-month follow-up | 2.59 ± 1.33 | 2.23 ± 1.23 | 0.001 | |
| 12-month follow-up | 2.55 ± 1.39 | 2.44 ± 1.32 | 0.12 | |
| 18-month follow-up | 2.36 ± 1.41 | 2.54 ± 1.32 | 0.50 | |
| Physical Component Summary-12 scale | 0.04 | |||
| Baseline | 36.57 ± 9.31 | 34.77 ± 8.88 | 0.26 | |
| 6-month follow-up | 39.32 ± 10.81 | 40.76 ± 11.28 | 0.04 | |
| 12-month follow-up | 40.78 ± 11.68 | 38.81 ± 11.14 | 0.54 | |
| 18-month follow-up | 41.15 ± 10.89 | 39.87 ± 11.70 | 0.76 | |
| Mental Component Summary-12 scale | <0.001 | |||
| Baseline | 34.06 ± 9.63 | 32.27 ± 8.48 | 0.40 | |
| 6-month follow-up | 42.15 ± 12.27 | 46.21 ± 10.33 | <0.001 | |
| 12-month follow-up | 43.60 ± 12.46 | 47.31 ± 11.48 | <0.001 | |
| 18-month follow-up | 43.49 ± 11.66 | 45.10 ± 12.19 | 0.03 | |
| Financial situation getting worse | <0.001 | |||
| Baseline | 0.30 ± 0.46 | 0.43 ± 0.50 | 0.06 | |
| 6-month follow-up | 0.28 ± 0.45 | 0.15 ± 0.35 | <0.001 | |
| 12-month follow-up | 0.24 ± 0.43 | 0.17 ± 0.38 | 0.02 | |
| 18-month follow-up | 0.28 ± 0.45 | 0.36 ± 0.48 | 0.41 | |
| Number of social stressors | <0.001 | |||
| Baseline | 3.15 ± 2.38 | 4.31 ± 2.70 | <0.001 | |
| 6-month follow-up | 2.34 ± 2.07 | 2.53 ± 2.18 | 0.96 | |
| 12-month follow-up | 2.40 ± 2.13 | 2.29 ± 2.14 | 0.19 | |
| 18-month follow-up | 2.39 ± 2.02 | 2.58 ± 2.06 | 0.70 |
Data are means ± SD or frequency (%). See Fig. 1 for the number of patients analyzed. One EUC patient did not complete SCL-20 assessment at 6 months.
*Logistic regression for the first five variables on receipt of depression care and depression outcomes; mixed-effects linear regression was used for the remaining outcomes. The first three variables on receipt of depression care were adjusted for study site, and the rest of the variables were adjusted for study site, dysthymia, baseline depression severity (PHQ-9 <15 vs. ≥15), birth place (U.S. vs. others), language, and years in the U.S. (<10 vs. ≥10 years). NA, not applicable.
Intervention implementation
Over the 12-month intervention, 169 (87.6%) patients completed an initial visit with a DDCS and 162 (83.9%) continued intervention treatment. A total of 104 (53.9%) received both PST and antidepressant medications, and 49 (25.4%) received only PST and 9 (4.7%) received only antidepressant medications. PST participants had a mean (± SD) of 8.7 ± 5.4 sessions. Of 113 INT patients receiving antidepressant medication, 103 patients remained on medication for a mean of 8.8 months over the 12-month intervention, whereas 10 (8.8%) patients discontinued antidepressant medication after 30 days or less. Estimated per-patient intervention costs totaled $820.
Receipt of depression care
INT patients predominantly chose PST first-line treatment. INT versus EUC patients were significantly more likely to receive antidepressant medication and/or counseling/psychotherapy (PST in the INT group) at 12 (all P values <0.001) and 18 (P values 0.01 to <0.001) months (Table 2). Over 12 months, 83.9% of INT patients received depression treatment (49 PST, 9 antidepressant medication, 104 both) versus 32.5% of EUC patients (37 antidepressant medication, 11 self-reported counseling, 15 both). Of patients prescribed antidepressant medication, over 12 months, a dosage increment or change in type of medication was provided to 63 (55.8%) INT versus 10 (19.2%) EUC patients. Thirty-five INT patients attended one or more PST support group sessions. Patient satisfaction with emotional care assessed at the 18-month blinded survey found that INT patients reported significantly greater satisfaction (satisfied to very satisfied) compared with EUC patients (89.5 vs. 77.9%; odds ratio 2.43 [95% CI 1.23–4.77]; P = 0.01).
Depression outcomes
At 6, 12, and 18 months, INT patients were significantly more likely to have a ≥50% reduction in SCL-20 baseline score (57, 62, and 62%) versus EUC patients (36, 42, and 44%) (adjusted odds ratio range 2.46–2.57; P < 0.001) (Table 2). Significant group difference in a ≥50% decrease in PHQ-9 score also was found at each follow-up. Intervention patients had significantly greater odds of depression remission based on SCL-20 <0.5 at 6 and 18 months, with similar trends at 12 months as well as remission at 6 and 12 months based on PHQ-9 <5. Significantly fewer INT than EUC patients had persistent major depression (i.e., PHQ-9 ≥10) at each follow-up. There were no significant interaction effects on depression improvement or remission between study groups and baseline depression severity, sex, language, time in the U.S., education, use of insulin, time with diabetes, glycemic control, or obesity (BMI ≥30 kg/m2) at each follow-up. Significant interactions were observed between study site and study group only for depression remission at 6 months (P = 0.03 for interaction; adjusted odds ratio 4.12 [95% CI 1.81–9.42] for El Monte and 1.28 [0.66–2.49] for Roybal clinic) and between age and study group only for depression improvement at 18 months (P = 0.01 for interaction; 0.87 [0.33–2.27] for patients aged <50 years and 3.80 [2.05–7.02] for patients aged ≥50 years). Analyses were repeated with the Hispanic-only and type 2 diabetic patient samples and the results were identical.
Clinical, functional, and socioeconomic outcomes
There were significant study group–by–time interactions over 18 months in mean diabetes symptoms, SF-12 emotional and physical functioning and pain, Sheehan disability, financial situation, and number of social stressors (Table 2). Comparisons of adjusted mean scores between study groups at 6 months found that INT patients had significantly better emotional functioning and less functional impairment, pain impact, diabetes symptoms, and likelihood of worsening financial situation; significant improvement in financial situation continued at 12 months; and significantly improved Mental Component Summary-12 was still present at 12 and 18 months. No group differences were found in A1C, diabetes complications, mean self-care management scores, or BMI over time or at each follow-up. Again, there were no significant differences in results for Hispanic- or type 2 diabetes–only samples.
Comment
To our knowledge, this is the first randomized controlled trial of collaborative care for predominantly Hispanic patients with diabetes in public safety-net clinics. Findings suggest that a collaborative care model, socioculturally adapted for low-income patients, resulted in significant reductions in depressive symptoms, improvements in emotional and physical functional outcomes, and lower burden of diabetes symptoms and pain compared with enhanced usual care. The importance of study findings is underscored in view of data that Hispanics in the U.S. have the highest estimated lifetime risk for diabetes (males 45.4% and females 52.5%) (22).
In light of known racial/ethnic disparities in receipt of depression care, it is noteworthy that INT patients had significantly higher rates of participation in PST, the length of time in which patients adhered to antidepressant medications, and the degree of satisfaction with the quality of depression care. Providing culturally sensitive acute and maintenance care that includes facilitating access to socioeconomic resources and is organizationally integrated within safety-net care systems is likely to have a marked effect on decreasing disparities in depression care among low-income and Hispanic patients with diabetes.
Despite the improvement associated with the intervention in quality and outcomes of depression care as well as improvements in functioning and decreased diabetes and pain symptom burden, no intervention effect on A1C or self-care management was found. An association between poorer glycemic control and depression has been frequently reported; however, results of treating depression and improving glycemic control are mixed. The trials reporting a change in A1C with improvement of depression were with less representative populations and often compared an evidence-based depression psychotherapy and diabetes education to diabetes education alone (23). There is evidence that Hispanics report self-monitoring of blood glucose as being very difficult (24), while in this study, patients often expressed to the depression care manager that general management of diabetes was socially and economically stressful.
Improving depression symptoms in patients with diabetes in prior collaborative care studies has been shown to be associated in comparisons with usual primary care with a high probability of achieving savings in total ambulatory medical costs (8). The higher costs associated with providing enhanced mental health care were offset by greater savings in medical costs (8). Black et al. (25) found in a large longitudinal study of an aging Hispanic population in the southwestern U.S. that depression markedly increases the risk in patients with diabetes of macro- and microvascular complications, incident physical disability, and mortality. Therefore, further studies are needed to ascertain whether improving outcomes of depression in patients with diabetes could decrease disability, complications, mortality, and medical costs.
Study results are encouraging and are consistent with other recent studies that have found that depression care management improvement strategies are effective over time among low-income and ethnic minority populations (12). Improving treatment of depression by integrating a depression specialist (supervised by a psychiatrist) into primary care along with long-term follow-up may be especially helpful in view of the challenges faced by physicians in community safety-net clinics. Ensuring that linguistic, cultural, and economic factors are incorporated with collaborative care management that includes mental health personnel is also likely to reduce disparities in acceptance and receipt of treatment. Of 17 clinic physicians, clinic medical directors, and nursing staff interviewed, all reported satisfaction with the intervention model, and the sustainability of the model is under active consideration. Our culturally focused recruitment and follow-up outreach efforts are likely to have reduced potential attrition rates that did not vary between study groups and resulted in better-than-usual geographic mobility of the study population in these safety net clinics.
Limitations
Not unique to health services effectiveness trials, our study design may have biased our comparisons in favor of the EUC group. Increased prescription of antidepressant medications over baseline among usual care patients may be attributable in part to the following enhanced usual care design: all patients were screened and clinic physicians were notified of patients meeting study criteria, all physicians participated in the depression care didactic sessions and were given a copy of the stepped-care algorithm, and acutely suicidal patients were referred for further clinical evaluation and treatment. Because the same practitioners treated both intervention and EUC patients, there may have also been a spillover effect on quality of depression treatment. EUC patients may have also benefited from having received the linguistically and idiomatically adapted patient and family educational pamphlets and the information provided on available supportive services. These biases may contribute to an underestimation of the effectiveness of the intervention compared with usual care outside a research trial. Additional limitations include our reliance on self-reports of chronic medical conditions and potentially underreporting of use of antidepressants and psychotherapy.
CONCLUSIONS
Socioculturally and organizationally adapted collaborative care is feasible and effective in improving quality of depression treatment and depressive and functional outcomes in a low-income, predominantly Hispanic population in safety-net clinics. To reduce disparities in depression care, these results suggest that despite organizational obstacles inherent to safety-net clinics, physicians should be aware of the increased risk of depressive symptoms in patients with diabetes and consider ways to routinely screen and implement socioculturally adapted collaborative depression care management.
Acknowledgments
The study is supported by R01 MH068468 from the National Institute of Mental Health (principal investigator, K.E.).
No potential conflicts of interest relevant to this article were reported.
We acknowledge the contributions of Dr. Michael Roybal and Dr. Stanley Leong, clinic medical directors; their staff; and participating patients.
Footnotes
Clinical trial reg. no. NCT00709150, clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 behavioral risk factor surveillance system. Diabetes Care 2008;31:105–107 [DOI] [PubMed] [Google Scholar]
- 2. Lanting LC, Joung I, Mackenbach JP, Lamberts SW, Boostma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients. Diabetes Care 2005;28:2280–2288 [DOI] [PubMed] [Google Scholar]
- 3. Gross R, Olfson M, Gameroff MJ, Carasquillo O, Shea S, Feder A, Lantigua R, Fuentes M, Weissman MM. Depression and glycemic control in Hispanic primary care patients with diabetes. J Gen Intern Med 2005;20:460–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pinto-Meza A, Fernandez A, Serrano-Blanco A, Haro JM. Adequacy of antidepressant treatment in Spanish primary care: a naturalistic six-month follow-up study. Psychiatr Serv 2008;59:78–83 [DOI] [PubMed] [Google Scholar]
- 5. Kirk JK, Passmore LV, Bell RA, Narayan KM, D'Agostino RB, Jr, Arcury TA, Quandt SA. Disparities in A1C levels between Hispanic and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2008;31:240–246 [DOI] [PubMed] [Google Scholar]
- 6. Duru OK, Mangione CM, Steers NW, Herman WH, Karter AJ, Kountz D, Marrero DG, Safford MM, Waitzfelder B. The association between clinical care strategies and the attenuation of racial/ethnic disparities in diabetes care: the Translating Research into Action for Diabetes (TRIAD) Study. Med Care 2006;44:1121–1128 [DOI] [PubMed] [Google Scholar]
- 7. Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, Kinder L, Young B, Von Korff M. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 2005;28:2668–2672 [DOI] [PubMed] [Google Scholar]
- 8. Katon WJ, Russo JE, Von Korff M, Lin EHB, Ludman E, Ciechanowski PS. Long-term effects on medical costs of improving depression outcomes in patients with depression and diabetes. Diabetes Care 2008;31:1155–1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Anand K, Gupta R, Thomas A, Ajilore O, Hellemann G. Focal subcortical biophysical abnormalities in patients diagnosed with type 2 diabetes and depression. Arch Gen Psychiatry 2009;66:324–330 [DOI] [PubMed] [Google Scholar]
- 10. Gross R, Olfson M, Gameroff MJ, Carasquillo O, Shea S, Feder A, Lantigua R, Fuentes M, Weissman MM. Depression and glycemic control in Hispanic primary care patients with diabetes. J Gen Int Med 2005;20:460–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li C, Ford ES, Zhao G, Ahluwalia IB, Pearson WS, Modkad AH. Prevalence and correlates of undiagnosed depression among U.S. adults with diabetes: the Behavioral Risk Factor Surveillance System, 2006. Diabetes Res Clin Pract 2009;83:268–279 [DOI] [PubMed] [Google Scholar]
- 12. Ell K, Xie B, Quon B, Quinn DI, Dwight-Johnson M, Lee PJ. Collaborative care management of depression among low-income patients with cancer: a randomized controlled trial. J Clin Oncology 2008;26:4488–4496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ell K, Katon W, Cabassa L, Xie B, Lee PJ, Kapetanovic S, Guterman J. Depression and diabetes among low-income Hispanics: design elements of a socio-culturally adapted collaborative care model randomized controlled trial. Int J Psychiatry Med 2009;29:113–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a measure of primary symptom dimensions. Mod Probl Pharmacopsychiatry 1974;7:79–110 [DOI] [PubMed] [Google Scholar]
- 15. Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: a systematic review. Gen Hosp Psych 2007;29:388–395 [DOI] [PubMed] [Google Scholar]
- 16. Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med 2006;21:547–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Katon W, Russo J, Dobie R, Sakai C. A randomized trial of nortriptyline for severe chronic tinnitus: effects on depression, disability, and tinnitus symptoms. Arch Intern Med 1993;153:2251–2259 [PubMed] [Google Scholar]
- 18. Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595–605 [PubMed] [Google Scholar]
- 19. Toobert DJ, Hampson SE, Russell E. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000;23:943–950 [DOI] [PubMed] [Google Scholar]
- 20. Whitty P, Steen N, Eccles M, McColl E, Hewison J, Meadows K, Clapp Z, Hutchinson A. A new self-completion outcome measure for diabetes: is it responsive to change? Quality Life Res 1997;6:407–413 [DOI] [PubMed] [Google Scholar]
- 21. Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC, SAS Institute, 1996. [Google Scholar]
- 22. Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA 2003;290:1884–1890 [DOI] [PubMed] [Google Scholar]
- 23. Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Predicting response to cognitive behavior therapy of depression in type 2 diabetes. Gen Hosp Psychiatry 1998;20:302–306 [DOI] [PubMed] [Google Scholar]
- 24. Misra R, Lager J. Ethnic and gender differences in psychosocial factors, glycemic control, and quality of life among adult type 2 diabetic patients. J Diabetes Complications 2009;23:54–64 [DOI] [PubMed] [Google Scholar]
- 25. Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in Mexican Americans with type 2 diabetes. Diabetes Care 2003;26:2822–2828 [DOI] [PubMed] [Google Scholar]