Abstract
Duodenal duplication cysts are rare congenital malformations. Most symptomatic cases are diagnosed in children and usually present with obstructive findings or bleeding symptoms. Treatment traditionally involves surgical resection, which can be often difficult because of the close proximity of the cysts to the papilla and bilopancreatic confluence. Endoscopic therapy has been used as an alternative to open surgery in a few selected cases. We report a case with a duodenal duplication cyst containing a brown pigmented stone within the cystic lumen. He was visited because of sudden right upper quadrant abdominal pain. An abdominal computed tomography revealed the presence of a cyst with a stone, which was finally removed by endoscopic resection.
Keywords: Duodenal duplication cyst, Brown pigmented stone, Endoscopic therapy
INTRODUCTION
Duodenal duplication cysts (DDC) have been rare congenital malformation that may develop at any level of the gut.1 The estimated prevalence is 1:4,500 to 1:10,000 in the general population.2 Most symptomatic cases are diagnosed in children and usually present with obstructive findings or bleeding symptoms.3 Here we report a case with a DDC containing a brown pigmented stone within the cystic lumen that was treated by endoscopic snare resection.
CASE REPORT
A 52-year old man was hospitalized because of the sudden onset of right upper quadrant abdominal pain and abnormal liver function tests. The medical history and family history were noncontributory. On physical examination, mild abdominal tenderness without rebound was noted in the right upper quadrant of abdomen. The laboratory results showed that ALT was 51 (0-41) IU/L but serum amylase, lipase, CA 19-9, and CEA levels were all within normal range. Serum γ-GT was 85 (8-61) IU/L.
The transabdominal ultrasound suggested a common bile duct stone and gallbladder polyp. Endoscopic ultrasound revealed the presence of a bulging mass like cystic lesion containing echogenic material with posterior acoustic shadowing in the region of the major papilla. However, there was no pathological alteration of the biliary or pancreatic ducts (Fig. 1). A three-dimensional computed tomography confirmed the presence of a cyst with a stone at duodenal ampulla (Fig. 2). Duodenoscope examination showed a soft submucosal tumor-like mass just distal portion to the orifice of the major papilla (Fig. 3). With injection of contrast through the major papillary orifice, the aforementioned submucosal lesion was opacified, and found to contain a round filling defect but biliary or pancreatic duct was not visualized (Fig. 4). The cystic lesion was removed using an endoscopic resection by standard polypectomy snare. The post-resection ulcer recovered uneventfully.
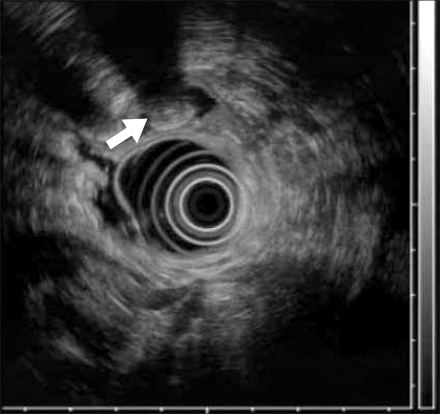
Fig. 1.
Endoscopic ultrasound reveal the presence of a bulging mass like cystic lesion containing echogenic material (arrow) with posterior acoustic shadowing in the region of the major papilla.
Fig. 2.
A three-dimensional computed tomography confirms the presence of a cyst (arrow) with a stone at juxtapapillary area.
Fig. 3.
Duodenoscope examination shows a soft submucosal tumor-like mass in distal portion of the major papilla orifice.
Fig. 4.
With injection of contrast through the major papillary orifice, the aforementioned submucosal lesion is opacified, and found to contain a round filling defect.
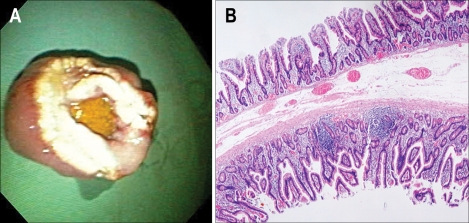
Macroscopically, the tumor measured 2.5×2.5×1.2 cm. The cut surface showed luminal mucosal folds with a brown pigmented stone (Fig. 5A). The microscopic examination revealed an epithelial lining, consisting of duodenal mucosa, on both sides of the specimen. Therefore, the final diagnosis was a DDC (Fig. 5B). At follow up of six months, the patient was well and reported no further episodes of abdominal pain. All laboratory parameters were within normal range.
Fig. 5.
Pathologic findings of endoscopically resected cyst. (A) The tumor is measured 2.5×2.5×1.2 cm. The cut surface shows luminal mucosal folds with a brown pigmented stone. (B) The microscopic examination shows the wall of the cyst inside and outside lined by duodenal epithelium and containing muscular layer (H&E stain, ×5).
DISCUSSION
A duplication cyst is a rare congenital malformation that may develop at any level of the alimentary tract from the mouth to the anus.1 The majority of the DDCs occur in the second portion of the duodenum along the posterior medial wall.4-6 DDC is extremely rare at ampulla of Vater. Symptoms may be vague and diverse, depending on the location of the duplication and include nonspecific pain, distention, dysphagia, jaundice and dyspepsia. A duplication cyst is a spherical tubular structure which possesses a smooth muscle layer, is lined by intestinal mucosa, and is attached to some portion of the alimentary tract.2 Additional different finding between DDC and choledochoceles was that the normal-looking papilla was always found on the proximal side of the protrusion in DDC, whereas, papilla is usually found on the distal side of the protrusion in choledochoceles. The principal distinguishing features between these two conditions are their histological characteristics. DDCs are covered by duodenal mucosa containing a distinct layer of smooth muscle. By contrast, choledochoceles are lined by either a bile duct or gallbladder mucosa and lack a smooth muscle layer.7 The common bile duct may traverse the cyst wall or empty directly with or without the pancreatic duct into the cyst, predisposing to obstruction of the ducts. Rarely, the cyst may contain stones due to biliary stasis or secondary to chronic stasis and alkalinity of intestinal chyme.8 In this present case, the DDC contained a brown pigmented stone.
Treatment involves traditionally surgical resection, which can be relatively difficult because of the close proximity of the cysts to the major papilla and bilopancreatic confluence.9-11 Endoscopic therapy has been used as an alternative to open surgery in a few selected cases.3,4,12,13 No comparative study has been conducted to date. Antaki et al.3 reported that resection of the cyst roof using a standard polypectomy snare or a large incision of the roof of the duplication cyst is probably sufficient for cure. There was only complication about minor bleeding occurred during incision, which was immediately controlled endoscopically with bipolar coagulation and application of two clips. There are some reported cases of a malignancy developing in a DDC.14,15 Compared with surgical resection, endoscopic therapy does not always result in complete ablation of the cyst mucosa. However, avoiding stasis of secretions inside the cyst over a lifetime could hypothetically have a protective effect.3 A repeat endoscopy with follow-up biopsy should be performed in 6 to 12 months after the initial treatment. The present case illustrates a rare condition in which a patient had a duodenal duplication cyst containing a stone. The patient was successfully treated by endoscopic snare resection without complications.
ACKNOWLEGEMENTS
The authors have no commercial association that might be a conflict of interest in relation to this article.
References
- 1.Heiss K. Intestinal duplications. In: Oldham KT, Colombani PM, Foglia RP, editors. Surgery of infants and children: scientific principles and practice. 1st ed. Philadelphia: Lippincott-Raven; 1997. pp. 1265–1274. [Google Scholar]
- 2.Leffall LS, Jr, Jackson M, Press H, Syphax B. Duplication cyst of the duodenum. Arch Surg. 1967;94:30–34. doi: 10.1001/archsurg.1967.01330070032008. [DOI] [PubMed] [Google Scholar]
- 3.Antaki F, Tringali A, Deprez P, et al. A case series of symptomatic intraluminal duodenal duplication cysts: presentation, endoscopic therapy, and long-term outcome (with video) Gastrointest Endosc. 2008;67:163–168. doi: 10.1016/j.gie.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Johanson JF, Geenen JE, Hogan WJ, Huibregtse K. Endoscopic therapy of a duodenal duplication cyst. Gastrointest Endosc. 1992;38:60–64. doi: 10.1016/s0016-5107(92)70335-6. [DOI] [PubMed] [Google Scholar]
- 5.Kim HS, Joo KR, Kim DH, et al. A case of juxtapapillary duodenal duplication cyst manifested by recurrent pancreatitis. Korean J Gastrointest Endosc. 2004;28:218–222. [Google Scholar]
- 6.Park JH, Moon JS, Oh MK, et al. A case of endoscopic unroofing after detachable snare ligation of a duodenal duplication cyst. Korean J Gastrointest Endosc. 2007;35:190–195. [Google Scholar]
- 7.Tajiri H. Choledochocele-containing stones. Am J Gastroenterol. 1996;91:1046–1048. [PubMed] [Google Scholar]
- 8.Prasad TR, Tan CE. Duodenal duplication cyst communicating with an aberrant pancreatic duct. Pediatr Surg Int. 2005;21:320–322. doi: 10.1007/s00383-005-1369-x. [DOI] [PubMed] [Google Scholar]
- 9.Ackerman NB. Duodenal duplication cysts: diagnosis and operative management. Surgery. 1974;76:330–333. [PubMed] [Google Scholar]
- 10.Jo YC, Joo KR, Kim DH, et al. Duodenal duplicated cyst manifested by acute pancreatitis and obstructive jaundice in an elderly man. J Korean Med Sci. 2004;19:604–607. doi: 10.3346/jkms.2004.19.4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niehues R, Dietl KH, Bettendorf O, Domschke W, Pohle T. Duodenal duplication cyst mimicking pancreatic cyst in a patient with pancreatitis. Gastrointest Endosc. 2005;62:190–192. doi: 10.1016/s0016-5107(04)02846-9. [DOI] [PubMed] [Google Scholar]
- 12.Wada S, Higashizawa T, Tamada K, et al. Endoscopic partial resection of a duodenal duplication cyst. Endoscopy. 2001;33:808–810. doi: 10.1055/s-2001-16528. [DOI] [PubMed] [Google Scholar]
- 13.al Traif I, Khan MH. Endoscopic drainage of a duodenal duplication cyst. Gastrointest Endosc. 1992;38:64–65. doi: 10.1016/s0016-5107(92)70336-8. [DOI] [PubMed] [Google Scholar]
- 14.Falk GL, Young CJ, Parer J. Adenocarcinoma arising in a duodenal duplication cyst: a case report. Aust N Z J Surg. 1991;61:551–553. doi: 10.1111/j.1445-2197.1991.tb00289.x. [DOI] [PubMed] [Google Scholar]
- 15.Hata H, Hiraoka N, Ojima H, Shimada K, Kosuge T, Shimoda T. Carcinoid tumor arising in a duplication cyst of the duodenum. Pathol Int. 2006;56:272–278. doi: 10.1111/j.1440-1827.2006.01957.x. [DOI] [PubMed] [Google Scholar]