Abstract
Granular cell tumors are uncommon but typically histologically benign neoplasms that occasionally behave as malignant tumors. Differentiation of benign granular cell tumors from malignant counterparts with radiographic and/or histologic analysis is crucial for physicians. We retrospectively studied five cases of intramuscular granular cell tumors arising in the lower extremities. All tumors had been histologically diagnosed as benign and were resected with a wide surgical margin. The minimum followup was 1 year (mean, 45 months; range, 12–119 months) after surgery. Four patients had no local recurrence or distant metastasis (at a minimum of 18 months followup), whereas one patient with lymph node metastasis had a recurrence and distant metastasis 3 months after surgery resulting in death. Intramuscular granular cell tumors can be diagnosed based on their characteristic MRI features, such as peripheral high intensity on T2-weighed images, and histologic evaluation. The histologic criteria described by Fanburg-Smith et al. can differentiate malignant granular cell tumors from benign tumors. A wide resection seems suitable for most granular cell tumors in the extremities.
Level of Evidence: Level IV, diagnostic study. See the Guidelines for Authors for a complete description of evidence.
Introduction
Granular cell tumors are uncommon tumors that may arise from a Schwannian lesion, typically occurring in the tongue, breast, skin, and subcutis [5]. Although most granular cell tumors have excellent outcomes after surgical resection [4], 0.5% to 2% may be malignant [4, 5], having poor outcomes with high potential of local recurrence and distant metastasis [6].
Granular cell tumors occurring in deep soft tissue of the extremities are rare [1, 4, 5, 10], especially those of intramuscular origin. The publications in the orthopaedic literature are limited [4, 10, 11]. Although these studies discuss MRI findings specific for granular cell tumors, it still is difficult to differentiate benign from malignant counterparts and these reports did not focus on histologic differentiation of granular cell tumors.
We therefore examined (1) the MRI findings specific to intramuscular granular cell tumors in the lower extremities for the preoperative diagnosis, and (2) the roles of the histologic criteria of Fanburg-Smith et al. [6] for differentiating malignant granular cell tumors from benign counterparts.
Patients and Methods
We retrospectively reviewed five consecutive patients with histologically benign intramuscular granular cell tumors in the extremities between 1997 and 2007 (Table 1). All patient information was obtained from their medical records. Four patients were female and one was male. Their ages ranged from 31 to 54 years, with a mean of 40.2 years at the time of surgery. All five patients presented with a primary symptom of a mass varying from 1 to 6 months in duration. No patients had any pain, and only one had mild tenderness. All patients had only one mass. All five tumors were located in the muscle of the lower extremities. Two tumors were located in the gracilis and the others in the gluteus maximus, the rectus femoris, and the lateral head of gastrocnemius, respectively. One patient had been treated with a large skin incision, intralesional excision of the tumor, and closure of the incision at the prereferral hospital.
Table 1.
Patients’ characteristics
| Patient | Age (years) | Gender | Tumor size (cm) | Location* | Followup (months) | Final disease status |
|---|---|---|---|---|---|---|
| 1 | 31 | Male | 3 | Gracilis | 12 | CDF |
| 2 | 46 | Female | 3 | Gracilis | 13 | CDF |
| 3 | 34 | Female | 4 | Rectus femoris | 119 | CDF |
| 4 | 36 | Female | 6 | Gastrocnemius, lateral head | 36 | CDF |
| 5 | 54 | Female | 7 | Gluteus maximus | 33 | DOD |
* All tumors were located in the muscles; CDF = continuously disease free; DOD = dead of disease.
MRI of the tumor was performed with and without gadolinium administration in all cases. On preoperative MRI, all five tumors showed a signal isointense to the surrounding muscle on T1-weighted sequences (Table 2). Because all tumors were intramuscular, their margins were ill-defined on T1-weighted sequences. On T2-weighted sequences, all tumors had lower signal intensity than fat but slightly higher than muscle. The signal intensity of all tumors was heterogeneous with an ill-defined margin and there was a peripheral rim of high-intensity signal around the tumors. All tumors showed enhanced signal intensity after gadolinium administration. Preoperative chest CT was assessed in three patients with larger tumors (≥ 4 cm), and no metastasis was detected in any of them. One patient had a lymph node metastasis biopsied at the time of surgery; she was the only patient who had previous treatment. All patients were followed up for at least 1 year (mean, 47 months; range, 18–125 months).
Table 2.
MRI features
| Patient | Signal intensity | Peripheral high signal | Gadolinium enhancement | |
|---|---|---|---|---|
| T1-weighted image | T2-weighted image | |||
| 1 | Isointense to muscle | Slightly high to muscle; low to fat; heterogeneous | + | ++ (strongly) |
| 2 | Isointense to muscle | Slightly high to muscle; low to fat; heterogeneous | + | + |
| 3 | Isointense to muscle | Slightly high to muscle; low to fat; heterogeneous | + | + |
| 4 | Isointense to muscle | Slightly high to muscle; low to fat; heterogeneous | + | + |
| 5 | Isointense to muscle | Slightly high to muscle; low to fat; heterogeneous | + | + (weakly) |
We performed an incisional biopsy with the small longitudinal incision under local anesthesia in all cases. Although one patient had lymph node metastasis clinically, all five tumors were diagnosed histologically as benign granular cell tumors.
Subsequently all tumors were excised with wide surgical margins determined by pathologic evaluation.
All specimens from the biopsy and surgery were evaluated histologically in the conventional manner in the clinical setting. In addition, the biopsy specimens were evaluated by an experienced pathologist using the histologic criteria of Fanburg-Smith et al. [6] for the retrospective review in this study. These criteria were based on six histologic features, ie, necrosis, spindling of cells, vesicular nuclei with prominent nucleoli, increased mitotic activity (> two mitoses per 10 high-powered fields), high nucleocytoplasmic ratio, and pleomorphism. Tumors with three or more of these features were diagnosed as malignant, tumors with one to two features were diagnosed as atypical, and tumors with no features were diagnosed as benign.
We followed up all patients every 3–6 months clinically and with MRI of the primary site and CT of the chest after surgical treatment.
Results
MRI showed a characteristic peripheral rim of high-intensity signal around the tumors on T2-weighed images in all five granular cell tumors (Table 2). Conventional histologic analysis revealed all five tumors were diagnosed as benign, including one in a patient treated at a prereferral hospital which was diagnosed twice (biopsy and resected specimens) as benign. However, using the histologic criteria of Fanburg-Smith et al., we found one biopsy specimen from this patient exhibited three features, ie, spindling of cells, high nucleocytoplasmic ratio, and increased mitotic activity, that suggested a diagnosis of malignant granular cell tumor. Specimens from the remaining four patients showed none of the above criteria, thus suggesting benign granular cell tumors.
Four patients had no recurrences and metastasis during a followup between 18 and 125 months. The patient with lymph node metastasis at the time of surgery had local recurrence and lung metastasis 3 months after surgery. She had no history of other neoplasms, hereditary diseases, and other diseases and had no relevant family history. The recurrent tumor was treated with radiotherapy but grew larger. She also was treated with systemic chemotherapy with the regimen of three courses of intravenous administration of ifosfamide and doxorubicin, two courses of intravenous administration of carboplatin and etoposide, seven courses of intravenous administration of cisplatin, and subsequently oral administration of 5-fluorouracil. Despite these chemotherapy regimens, her disease progressed, resulting in death attributable to pulmonary metastases at 21 months after surgery. Representative cases of benign and malignant granular cell tumors are shown (Figs. 1, 2).
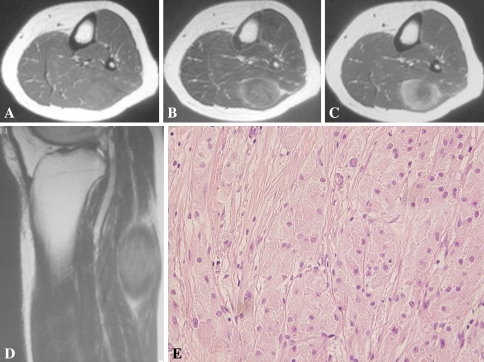
Fig. 1A–E.
The imaging and histologic characteristics of a representative case of benign granular cell tumor are shown. The patient is a 36-year-old man (Patient 4) with a tumor located in the lateral head of the gastrocnemius. (A) An axial T1-weighted MR image shows the tumor with a signal isointense to skeletal muscle. The signal intensity is slightly heterogeneous. (B) An axial T2-weighted image shows the tumor with slightly higher-intensity signal than the skeletal muscle and a heterogeneous signal with ill-defined margins with a peripheral zone of edema. (C) An axial T1-weighted image after gadolinium administration shows the tumor with diffuse enhancement. (D) A sagittal T2-weighted image of the knee shows the tumor with a peripheral heterogeneous high-intensity signal. (E) A histologic specimen shows characteristic sheets of polygonal tumor cells (Stain, hematoxylin and eosin; original magnification, ×400).
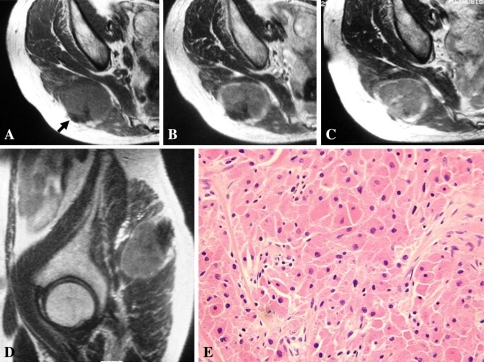
Fig. 2A–E.
The imaging and histologic characteristics of a representative case of malignant granular cell tumor in a 54-year-old woman (Patient 5) are shown. The tumor is located in the gluteus maximus. (A) An axial T1-weighted MR image shows the tumor with a signal isointense to the skeletal muscle. The partial low signal in the tumor indicates the biopsy site (arrow). (B) An axial T2-weighted image shows the tumor with slightly higher-intensity signal than skeletal muscle and a heterogeneous signal with ill-defined margins. High-intensity signal is observed peripherally around the tumor. (C) An axial T2-weighted image of the same level as in (A) after gadolinium administration shows the tumor with diffuse weak enhancement. (D) A sagittal T2-weighted image of the hip shows the tumor with peripheral high-intensity signal. (E) A histologic specimen shows nests of tumor cells with intervening collagen (Stain, hematoxylin and eosin; original magnification, ×400).
Discussion
Granular cell tumors are rare neoplasms, and those of intramuscular origin in the extremities are much more uncommon for orthopaedic surgeons [4, 5, 10]. Approximately 70 cases of granular cell tumors in the extremities have been reported in articles listed in PubMed (search words; “granular cell tumor” and “extremities”; search period; 1973–2008; search date; February 26, 2009); however, most of the studies include only one or two cases. There are only six studies including three or more cases (Table 3). More information regarding these tumors is needed. In this study, we wished to clarify the characteristic MRI findings of intramuscular granular cell tumors for preoperative diagnosis, the roles of histologic evaluation according to the criteria of Fanburg-Smith et al. for differentiating the malignant granular cell tumors from their benign counterparts, and adequate treatment of these tumors.
Table 3.
Reports of granular cell tumor of extremities (three or more cases)
| Study | Number of patients | Number of malignant tumors | Clinical outcome |
|---|---|---|---|
| Thacker et al. [10] (2007) | 3 | 2 | 1 case: malignant, DOD; all others: CDF |
| Chaudry and Calonje [2] (2005) | 11 | Unclear | All cases: CDF |
| Blacksin et al. [1] (2005) | 5 | 1 | All cases: CDF |
| Elkousy et al. [4] (2000) | 10 | 0 | All cases: CDF |
| Morrison et al. [8] (1987) | 5 | 0 | All cases: CDF |
| Fierro and Dorfman [7] (1975) | 3 | Unclear | All cases: CDF; 1 case: amputation of hand |
| Current study | 5 | 1 | 1 case: malignant, DOD; all others: CDF |
DOD = dead of disease; CDF = continuously disease free.
This study had several limitations. First, we had only five patients, but these tumors are extremely rare and thus a large series likely cannot be accumulated in one center. Second, we had a relatively short followup (mean, 47 months; range, 18–125 months), and thus we might not have encountered a late recurrence or metastasis; these can be detected only by further followup. A multicenter retrospective study might address both of these points.
Preoperative MRI is helpful to differentiate this tumor from other soft tissue tumors based on some characteristic findings [1, 4, 11]. All tumors we studied had a signal isointense to surrounding muscles on the T1-weighted sequence. On T2-weighted sequences, we observed lower signal than fat but slightly higher signal than muscles with ill-defined margins. All tumors had heterogeneous signal and high-intensity signal peripherally on this sequence. The heterogeneous features on T2-weighed images might result from differing cell arrangements or the fibrous/collagenous component intervening in the tumor cells in the same tumor and among cases. Peripheral high intensity seemed highly specific to granular cell tumors, especially in those of intramuscular origin. This finding corresponds to the lymphocytic infiltration and inflammation noted at the tumor margin by Blacksin et al. [1]. They found subcutaneous lesions did not show peripheral high signal intensity on T2-weighed images, suggesting the possibility that lymphocytic cells can infiltrate easily around an intramuscular tumor. Many soft tissue tumors show lower-intensity signals than muscles on T1-weighted sequences and higher-intensity signals than muscles on T2-weighted sequences, with some exceptions, such as fibrous tumors, desmoid tumors, giant cell tumors, calcifications, and lipomatous tumors. In our patients, all five granular cell tumors arising in muscles had the same unique intensity signals on MRI as the findings above. Considering these facts, among the various types of soft tissue tumors, the preoperative diagnosis of granular cell tumor can be made by carefully analyzing the MRI findings.
Approximately 0.5% to 2% of granular cell tumors are malignant [4, 5]. They have a higher potential for local recurrence and metastasis with poor prognosis than their benign counterparts [6]. In our study, a biopsy specimen provided sufficient information to diagnose a granular cell tumor. However, a conventional histologic examination could not differentiate malignant granular cell tumors from benign, and moreover, malignancy could not be diagnosed histologically even with the excised specimen. It therefore seems difficult to distinguish malignant granular cell tumors from their benign counterparts in an ordinary manner owing to the similarity of the microscopic pathology. Fanburg-Smith et al. [6] reported histologic criteria for malignant granular cell tumors by analyzing the clinical and histologic information of 73 cases of granular cell tumors. According to their report, based on six features, ie, necrosis, spindling of cells, vesicular nuclei with prominent nucleoli, increased mitotic activity (> two mitoses per 10 high-powered fields), high nucleocytoplasmic ratio, and pleomorphism, tumors with three or more of these features should be diagnosed as malignant and have an approximately 40% risk of causing death, with a high ratio of metastasis and local recurrence. Tumors with one to two features should be diagnosed as atypical. Tumors with no features should be diagnosed as benign and typically have an excellent outcome, with no metastasis and local recurrence after adequate resection. Fanburg-Smith et al. suggested these criteria can distinguish malignant granular cell tumors from benign granular cell tumors and can provide valuable information concerning the prognosis for surgeons and patients. However, the above histologic criteria may have some limitations for application. Fanburg-Smith et al. [6] did not define all features of the criteria in detail. Whether the above features should be observed diffusely or focally and detailed definitions of spindling of cells, higher nucleocytoplasmic ratio, and pleomorphism are unclear, and therefore, evaluation of the positive features of the criteria depends on each pathologist. Despite these concerns, we believe these criteria are helpful for differentiating malignancies from their benign counterparts as we correctly differentiated the four benign from the one malignant tumor using these criteria. In addition, some clinical factors suggest granular cell tumors have malignant potential [5]. Large tumor size (> 5 cm), older age, female gender, deep location (intramuscular), occurrence in the lower extremities, rapid recent growth after an extended period, and local recurrence are reportedly factors [6, 11]. However, these factors only indicate the tumors have a high potential for aggressiveness and are not sufficient to diagnose malignancy. Therefore, there are overlapping features between the benign and malignant tumors in these indicators [10, 12]. To diagnose malignant granular cell tumors, careful consideration of the histologic features and the clinical information is needed.
Surgeons treating granular cell tumors must understand the histologic characteristics of the tumor. The tumors we studied were ill-circumscribed with either no capsules or thin ones microscopically, and from the resected specimens were poorly encapsulated and grossly invading the surrounding muscles. These features may reflect the MRI findings of an ill-defined margin. In addition, as described previously, it is difficult to differentiate benign granular cell tumors from malignant granular cell tumors, even for experienced pathologists. Although the criteria described by Fanburg-Smith et al. [6] were applied carefully, a completely accurate differentiation of malignancy remains difficult. Considering these aspects, granular cell tumors arising in the extremities therefore should be resected with a wide surgical margin. Although all five granular cell tumors in our patients could be excised with a wide surgical margin, in cases in which the tumor is adjacent to a critical structure, such as nerves and vessels, a resection procedure is controversial [3]. Although most granular cell tumors are managed adequately with surgical excision alone, certain granular cell tumors at high risk of malignant behavior might be approached in a manner analogous to the low-grade soft tissue sarcomas; the use of radiation therapy after complete excision has led to limb preservation and better cosmesis [9].
Biopsy specimens in these special cases probably should be sent to a referral center for soft tissue tumors to get a second opinion from a specialized pathologist. When a tumor is diagnosed pathologically as a malignant granular cell tumor, the patient should be sent to the reference center and treated by physicians with this specialty.
We retrospectively reviewed five patients with intramuscular granular cell tumors arising in the lower extremities. Preoperative MRI helped to diagnose granular cell tumors based on their characteristic findings, especially for those of an intramuscular origin. Although the histologic criteria described by Fanburg-Smith et al. [6] provide important information for differentiating malignant granular cell from benign tumors, physicians should give special consideration to the possibility that histologically benign lesions may be malignant in granular cell tumors. We believe a wide resection is suitable for most granular cell tumors in the extremities for cases with a preoperative benign diagnosis.
Acknowledgments
We thank Dr. Satoko Shimada for helpful pathologic evaluation and Eri Ishihara for valuable secretarial assistance.
Footnotes
One of the authors (YN) has received funding from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Grant-in-Aid 20591751 for Scientific Research [C]).
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at Nagoya University Graduate School and School of Medicine and Aichi Cancer Center Central Hospital.
References
- 1.Blacksin MF, White LM, Hameed M, Kandel R, Patterson FR, Benevenia J. Granular cell tumor of the extremity: magnetic resonance imaging characteristics with pathologic correlation. Skeletal Radiol. 2005;34:625–631. doi: 10.1007/s00256-005-0925-8. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry IH, Calonje E. Dermal non-neural granular cell tumour (so-called primitive polypoid granular cell tumour): a distinctive entity further delineated in a clinicopathological study of 11 cases. Histopathology. 2005;47:179–185. doi: 10.1111/j.1365-2559.2005.02192.x. [DOI] [PubMed] [Google Scholar]
- 3.Davis GA. Granular cell tumor: a rare tumor of the ulnar nerve. Case report. Neurosurg Focus. 2007;22:E5. [PubMed] [Google Scholar]
- 4.Elkousy H, Harrelson J, Dodd L, Martinez S, Scully S. Granular cell tumors of the extremities. Clin Orthop Relat Res. 2000;380:191–198. doi: 10.1097/00003086-200011000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Enginger FM, Weiss S. Granular cell tumor. In: Soft Tissue Tumors. Ed 4. St Louis, MO: CV Mosby; 2004:1178–1187.
- 6.Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779–794. doi: 10.1097/00000478-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Fierro FJ, Dorfman HD. Granular cell myoblastoma of the hand: report of three new cases with aggressive behavior in one. Bull Hosp Joint Dis. 1975;36:121–129. [PubMed] [Google Scholar]
- 8.Morrison JG, Gray GF, Jr, Dao AH, Adkins RB., Jr Granular cell tumors. Am Surg. 1987;53:156–160. [PubMed] [Google Scholar]
- 9.Rosenthal SA, Livolsi VA, Turrisi AT., III Adjuvant radiotherapy for recurrent granular cell tumor. Cancer. 1990;65:897–900. doi: 10.1002/1097-0142(19900215)65:4<897::AID-CNCR2820650413>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 10.Thacker MM, Humble SD, Mounasamy V, Temple HT, Scully SP. Case report. Granular cell tumors of extremities: comparison of benign and malignant variants. Clin Orthop Relat Res. 2007;455:267–273. doi: 10.1097/01.blo.0000238786.06231.17. [DOI] [PubMed] [Google Scholar]
- 11.Tsuchida T, Okada K, Itoi E, Sato T, Sato K. Intramuscular malignant granular cell tumor. Skeletal Radiol. 1997;26:116–121. doi: 10.1007/s002560050204. [DOI] [PubMed] [Google Scholar]
- 12.Wieczorek TJ, Krane JF, Domanski HA, Akerman M, Carlen B, Misdraji J, Granter SR. Cytologic findings in granular cell tumors, with emphasis on the diagnosis of malignant granular cell tumor by fine-needle aspiration biopsy. Cancer. 2001;93:398–408. doi: 10.1002/cncr.10143. [DOI] [PubMed] [Google Scholar]