Abstract
Background:
Pedicle screw instrumentation of the deformed cervical and thoracic spine is challenging to even the most experienced surgeon and associated with increased incidence of screw misplacement. Iso-C3D based navigation has been reported to improve the accuracy of pedicle screw placement, however, there are very few studies assessing its efficacy in the presence of deformity. We conducted a study to evaluate the accuracy of Iso-C3D based navigation in pedicle screw fixation in the deformed cervical and thoracic spine.
Materials and Methods:
We inserted 98 cervical pedicle screws (18 patients) and 242 thoracic pedicle screws (17 patients) using Iso-C3D based navigation for deformities of spine due to scoliosis, ankylosing spondylitis, post traumatic and degenerative disorders. Two independent observers determined and graded the accuracy of screw placement from postoperative computed tomography (CT) scans.
Results:
Postoperative CT scans of the cervical spine showed 90.8% perfectly placed screws with 7 (7%) grade I pedicle breaches, 2 (2%) grade II pedicle breaches and one anterior cortex penetration (< 2mm). Five lateral pedicle breaches violated the vertebral artery foramen and three medial pedicle breaches penetrated the spinal canal; however, no patient had any neurovascular complications. In the thoracic spine there were 92.2% perfectly placed screws with only six (2%) grade II pedicle breaches, eight (3%) grade I pedicle breaches and five screws (2%) penetrating the anterior or lateral cortex. No neuro-vascular complications were encountered.
Conclusion:
Iso-C3D based navigation improves the accuracy of pedicle screw placement in deformities of the cervical and thoracic spine. The low incidence of pedicle breach implies increased safety for the patient.
Keywords: Navigation, pedicle screw fixation, thoracic and cervical deformity
INTRODUCTION
Pedicle screw instrumentation is the preferred method of posterior stabilization of the spine especially in the presence of deformity.1–3 It has the advantages of three column fixation, improved coronal, sagittal, and rotational correction, lower incidence of implant failures, pseudoarthrosis and fewer requirements of postoperative bracing when compared with conventional hook and wire constructs.4–6
However, pedicle screw instrumentation of the deformed thoracic3,7 and cervical spine is associated with a high rate of pedicle breach (up to 43% for thoracic spine7 and 12% for cervical spine8) and though the ensuing complication rate is low7–9 the potential for disastrous neurovascular injury, remains. Other complications such as loss of fixation of the curve, progression of deformity and pseudoarthrosis may ensue from poor fixation.
Computer navigation has been found to improve the accuracy of pedicle screw fixation in deformed as well as non deformed spine.7,10–16 Most of these studies,10,14,15 however, have the drawbacks of including deformities of the lumbar spine or having deformities from only a small subsection of the study population. Hence these studies are of limited value in assessing the true efficacy of computer navigation. The narrow diameter of the thoracic and cervical pedicles and the proximity of the cord and vertebral artery (in the cervical spine) make pedicle screw insertion challenging. The presence of deformity adds to the difficulty and hence the true efficacy of computer navigation can be gauged by assessing the accuracy of pedicle screw placement in cervical and thoracic spine deformity correction. There are very few studies11–13,17 reporting on the efficacy of computer navigation in the deformity correction. Hence we conducted a prospective study to evaluate the accuracy of screw placement using Iso-C3D navigation in cervical and thoracic spine deformities.
MATERIALS AND METHODS
Seventeen patients with thoracic spine deformity and 18 with cervical spine deformities, who were treated by pedicle screw fixation using Iso-C3D based navigation, were included in the study. Patients with scoliosis of more than 100° or kyphosis exceeding 90° as well as obese patients (weight of more than 100 kg) were excluded from the study group as in these cases it is impossible to centralize the anatomic area of interest in the arc of the movement of the Iso-C3D C-arm. The etiology of the deformities is seen in Tables 1 and 2.
Table 1.
Etiology of thoracic spine deformities
| Etiology | No. of patients (n=17) |
|---|---|
| Adolescent idiopathic scoliosis | 10 |
| Post tubercular kyphosis | 3 |
| Kyphoscoliosis due to neurofibromatosis | 2 |
| Scheurmanns disease | 1 |
| Paralytic scoliosis | 1 |
Table 2.
Etiology of cervical spine deformities
| Etiology | No. of patients (n=18) |
|---|---|
| C1-2 instability | 8 |
| Congenital deformity | 4 |
| Sub axial instability (post traumatic, degenerative) | 3 |
| Ankylosing spondylitis with deformity | 2 |
| Ankylosing spondylitis with pseudoarthrosis | 1 |
All the patients were investigated with radiographs; CT and MRI scan pre-operatively. In cervical spine, MR angiography was done to assess the course of the vertebral artery and rule out any anomalies. In thoracic spine group the mean age of the patient was 19.6±9.3 years (range 10-52 years).The mean Cobb's angle was 62.4°±6° (range 52°-86°) and mean Kyphotic angle was 36.4°±6° (range 30°-74°). In the cervical spine group, the mean age of the patient was 24.2± 6.2 years (range 10-52 years).
Procedure
All cases were operated in the prone position on a carbon top radiolucent table (Fahmed, Germany). After the spine was exposed posteriorly a minimally invasive reference array (MIRA) was attached to the spinous process of a vertebra caudal to the region of interest. The Siremobil Iso-C3D (Seimens, Germany) image intensifier which rotates through an arc of 190° obtained fluoroscopic images of the relevant segments of the spine. It was usually possible to include five to six levels in children and four to five levels in adults in a single fluoroscopic field. The acquired data was transferred to the computer navigation platform-Vector Vision (Spine version 2.0 Brain Lab, Germany) which reconstructed the data to provide real time intra-operative multi-planar images of the vertebra. Accuracy of the images was verified using a pointed tool navigator. The tool navigator was used along with the 3D real-time multi-planar images to determine the entry point, trajectory, length and width of the pedicle [Figure 1]. The dorsal cortex at the identified entry site was removed with a 2.5 mm burr. The pedicle was gently negotiated using a sharp pedicle finder.
Figure 1.
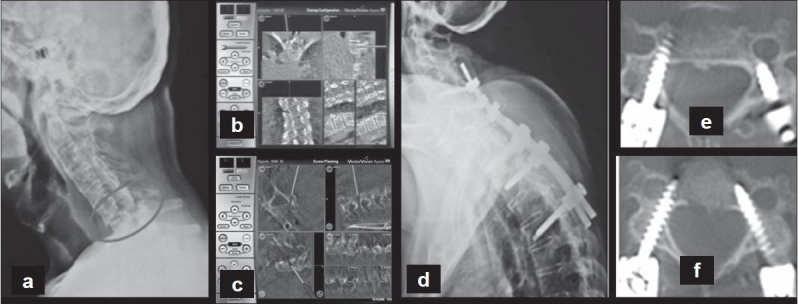
(a) Preoperative lateral radiograph of cervical spine showing a C6-7 chance fracture in a patient with ankylosing spondylitis (b, c) Intra operative navigation images of thoracic and cervical spine- pedicle entry point and trajectory and planning of screws (d, e, f) Postoperative radiograph and CT scan showing the placement of the screws
The direction and depth of the pedicle finder was guided and confirmed frequently using the tool navigator. The length and size of the screws was planned using the tool and “planning a screw” option of the software. Each screw was calibrated and threaded along the pre-tapped pilot hole guided by “autopilot” images. In thinned, and deformed, and sclerosed thoracic pedicles, where transpedicular screw fixation was impossible, an in-out-in technique was used under navigation guidance. Time required for data acquisition was divided by the total number of screws inserted with the same data. This average setup time per screw added to the time taken for actual screw insertion gave the insertion time for that particular screw.
Postoperative CT scans were performed using 2-mm cuts with 1-mm overlap to assess the accuracy of screw placement in all patients. The radiographs and CT scans were analyzed with respect to the breach of the pedicle wall by the screw either medially, laterally, inferiorly, or superiorly [Figure 2]. The distance of the tip of the screw from the anterior or lateral cortex of the vertebra was also measured in axial CT sections. Screw placement was graded on CT as follows [Figure 3]: grade 0, no pedicle perforation; grade 1, only the threads outside the pedicle (less than 2 mm); grade 2, core screw diameter outside the pedicle (2-4 mm); and grade 3, screw entirely outside the pedicle.
Figure 2.
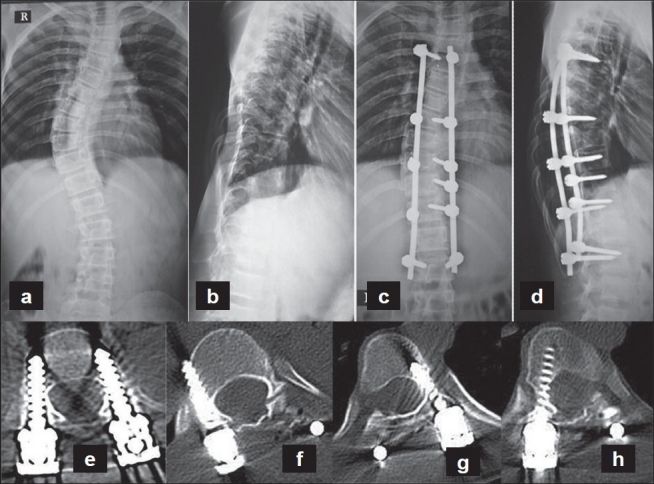
(a-d) Preoperative and post operative radiographs of an adolescent idiopathic right thoracic scoliosis. Computer assisted pedicle screw insertion was performed (e-h). Postoperative axial CT scan sections of the patient showing the placement of the screws
Figure 3.
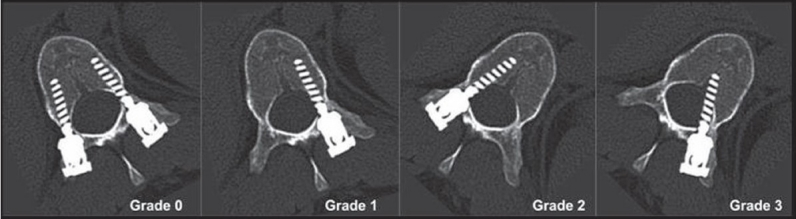
Grading used for pedicle breaches on postoperative CT scan images
RESULTS
A total of 242 thoracic pedicle screws and 98 cervical screws were inserted under navigation guidance. The incidence of pedicle screw breach in thoracic spine was 19/242 (7.8%). Eight patients (3%) had grade 1 pedicle breaches, six patients (2.5%) had grade 2 pedicle breaches and five (2%) had anterolateral vertebral body penetration. Of the 15 screws breaching the lateral pedicle cortex, seven with more than a 4-mm pedicle breach belonged to the planned in-out-in screws, hence these screws were not considered in the analysis of pedicle breaches. The average screw insertion time (includes average data acquisition time per screw) was 2.37±0.72 minutes (range 1.16-4.5) per screw. The mean data acquisition time was 24.6±6.3 minutes (range 16-33). Out of twenty four screws in patients with kyphosis four had pedicle breaches and 10 out of 208 screws in scoliotic deformity had pedicle breaches.
In patients with cervical pedicle screws there were nine pedicle breaches in ninety eight screws (9.2%). The main pedicle breach was on the lateral wall (5/98) followed by medial wall (3/98), superior pedicle (1/98) and anterolateral body breach (1/98). The grade of pedicle breach is in Table 3. Average pedicle screw insertion time in cervical spine was 2.5±0.6 min. In our series there were no incidences of grade 3 pedicle breaches, spinal cord injury or vertebral artery injury due to pedicle breach.
Table 3.
Incidence and grade of pedicle breach
| Pedicle breach | Thoracic (n=242) | Cervical (n=98) | |
|---|---|---|---|
| Superior pedicle wall | Grade-1 | 1 | 1 |
| Grade-2 | 0 | 0 | |
| Grade-3 | 0 | 0 | |
| Inferior pedicle wall | Grade-1 | 2 | 0 |
| Grade-2 | 1 | 0 | |
| Grade-3 | 0 | 0 | |
| Medial pedicle wall | Grade-1 | 1 | 2 |
| Grade-2 | 1 | 1 | |
| Grade-3 | 0 | 0 | |
| Lateral pedicle wall | Grade-1 | 4 | 4 |
| Grade-2 | 4 | 1 | |
| Grade-3 | 7 (planned-in out in technique) | 0 | |
| Anterolateral vertebral body wall | Grade-1 | 2 | 1 |
| Grade-2 | 2 | 0 | |
| Grade-3 | 1 | 0 |
DISCUSSION
Pedicle screw stabilization is bio-mechanically superior to other methods of spinal fixation but screw misplacement has the potential for serious complications such as spinal cord, nerve root, visceral or vessel injury.2,18–21 Though commonly used in the lumbar and non deformed thoracic spine, its use in the deformed thoracic and cervical spine is limited for fear of inadvertent neuro-vascular injury.8 The complex anatomy of the normal cervical spine including the narrow diameter of the pedicles, the variations in the saggital and axial angulations of the pedicles22–25 as well as the anatomical variations in the course24 and size of the vertebral artery make pedicle screw instrumentation a challenging procedure. The presence of deformity and altered anatomy (due to congenital anomalies) further adds to the difficulty.
In the thoracic spine the pedicles are narrow and the canal cord ratio of thoracic spine is low, hence the chance of a pedicle violation causing cord injury is common even in normal thoracic spine.26–30 In the presence of deformity the size and orientation of the pedicles vary considerably between the different vertebrae within the curve, and also between the concave and convex sides of the same vertebrae. The pedicles are frequently thinner and sclerosed, making canal perforation easily possible. The dura is often stretched over the pedicles on the concave side of the curve, and even minor medial violations can damage the cord.6–7,31–32 Hence pedicle screw instrumentation is challenging as there are potential risks of iatrogenic damage to neural or vascular structures.
Pedicle screw insertion is performed either by the conventional technique (using anatomical landmarks with or without fluoroscopy), foramino-laminotomy technique or computer navigation assisted. Clinical and cadaveric studies assessing the conventional technique of pedicle screw placement have reported pedicle violation rates ranging from 5.5 to 54.7% for lumbar and thoracic region with neurologic sequelae ranging from 0 to 7%.7,10,21,33 In the cervical spine it ranges from 6.7 to 12% with neurological sequelae ranging from 0 to 1.7%.8,34–36 The foramino- laminotomy technique has been be used to increase the accuracy of screw placement, however, pedicle violation rates up to 15.9% in the thoracic spine and 55% in the cervical spine have been reported.36–37 The open-lamina technique requires increases surgical exposure of the epidural space, which can potentially result in increased operative time, risk of dural tear, and blood loss.37
Computer navigation is commonly used to guide pedicle screw insertion and studies comparing pedicle screw placement using conventional and computer navigation have demonstrated the superior accuracy of this technology.8,10,12,13,17,36 However, there are very few studies11–13,17 documenting the efficacy of computer navigation in placement of pedicle screws in the deformed cervical and thoracic spine.
Accuracy of screw placement in thoracic spine deformities
Belmont et al.31 reported the clinical accuracy of thoracic pedicle screws in 40 patients of scoliosis and kyphosis, demonstrating a 43% of screw perforation rate. Liljenqvist et al.3 reported on 33 patients of thoracic idiopathic scoliosis and demonstrated a 25% of perforation rate. In both the studies,3,31 despite the high screw perforation rate, there were no neurovascular or pulmonary complications. A study by Laine et al.14 on 100 patients, including small numbers of spinal deformity demonstrated that the screw perforation rate signifcantly decreased from 13.4 to 4.6% with use of computer navigation in thoracic and lumbar spine. In a comparative study on the accuracy of pedicle screw placement in scoliosis between conventional fuoroscopic and computer-assisted surgical techniques, Kotani et al.12 observed a perforation rate of 11% in the conventional group and 1.8% in the navigated group. The results of the present study (7.8% breaches) are lower than those reported using the conventional technique and demonstrate the improved accuracy of computer navigation in the insertion of pedicle screws. The in-out-in technique was used to insert seven screws as a planned procedure. This was done as the pedicles were sclerosed and too thin to accept a screw without a pedicle breech. Here the screw trajectory was not an accidental breach but a well planned trajectory aimed at a secure position of the screw in the body, hence these screws were not included in the accidental breach category.
Accuracy of screw placement in cervical spine deformities
In the present study of the cervical spine region there were nine cases of pedicle breaches (9.2%), but none of the cases had vertebral artery, spinal cord or nerve root injuries. Even when lateral wall perforation occurred, no complications involving the vertebral artery were clinically apparent. It is theorized that the vertebral artery does not occupy the whole of the foramen transversarium, hence minimal violations of the foramen transversarium may not be as risky as was initially thought.35–36 Richter et al.38 reported 8.6% of pedicle screw perforation with conventional technique and 3% with CT based navigation assisted pedicle screw fixation. Though Abumi et al.34 reported only a 6.7% misplacement rate (out of 669 cervical pedicle screws) when using a conventional screw insertion technique this data may not be applicable to other spine surgeons with less experience in cervical pedicle screws. In a comparative study between the conventional and computer navigated technique for cervical pedicle screw insertion by Kotani and Abumi et al.,12 the rate of pedicle wall perforation was significantly lower in the computer-assisted group than that in the conventional group (1.2 and 6.7%, respectively; P<0.05). The screw trajectory in the horizontal plane was significantly closer to the anatomical pedicle axis in the computer-assisted group compared with the manual insertion group (P<0.05). Complications such as neural damage or vascular injury were not demonstrated in the computer-assisted group (compared with 2% in the manual insertion treatment group). This further underlines the fact that computer navigation improves the accuracy of screw placement. The high rate of pedicle breaches seen in the present series may be due to the presence of congenital anomalies.
Even though there are many advantages of computer assisted surgery, the surgeon must be prepared to proceed, in rare instances, without image guidance. In case of severe deformity it is difficult to centralize the patient in both antero-posterior and lateral view in C arm. In gross obesity the arc of C arm cannot move freely around the patient. In case of osteoporosis the image quality will be poor. Moreover, navigation is a computer and software program and the system can crash at any time. Like all image-guidance methods, the Iso-C3D is not a substitute for anatomic knowledge of the spine. The results of this analysis indicate that image guided surgery systems should not be used as a substitute for surgical judgment and experience, but rather as a tool to complement the surgeon.
CONCLUSION
Intra operative Iso-C3D fluoroscopy based navigation improves the accuracy of pedicle screw insertion and reduces the pedicle screw perforations in deformities of cervical and thoracic spine. Its use in very severe deformities (scoliosis >90° and kyphosis >90°) is limited.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: A European view. Eur Spine J. 1997;6:2–18. doi: 10.1007/BF01676569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458–76. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine (Phila Pa 1976) 1997;22:2239–45. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 4.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks: Results in double major curves in adolescent idiopathic scoliosis. Spine. 1997;22:1369–79. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 5.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7–17. [PubMed] [Google Scholar]
- 6.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–6. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 7.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–6. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 8.Richter M, Cakir B, Schmidt R. Cervical pedicle screws:Conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa ) ;30. 1976;2005:2280–7. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 9.Liljenqvist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine (Phila Pa 1976) 2000;25:1247–53. doi: 10.1097/00007632-200005150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Amiot LP, Lang K, Putzier M, Zippel H, Labelle H. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine. 2000;25:606–14. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- 11.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: A meta-analysis. Spine. 2007;32:E111–120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 12.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99:257–63. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 13.Kotani Y, Abumi K, Ito M, Takahata M, Sudo H, Ohshima S, et al. Accuracy analysis of pedicle screw placement in posterior scoliosis surgery: Comparison between conventional fluoroscopic and computer-assisted technique. Spine(Phila Pa 1976) 2007;32:1543–50. doi: 10.1097/BRS.0b013e318068661e. [DOI] [PubMed] [Google Scholar]
- 14.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: A randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–40. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Sautot P. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res. 1998;354:39–48. doi: 10.1097/00003086-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Rajasekaran S, Vidyadhara S, Shetty AP. Iso-C3D fluoroscopy-based navigation in direct pedicle screw fixation of Hangman fracture: A case report. J Spinal Disord Tech. 2007;20:616–9. doi: 10.1097/BSD.0b013e318074f978. [DOI] [PubMed] [Google Scholar]
- 17.Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa ) ;32. 1976;2007:E56–64. doi: 10.1097/01.brs.0000252094.64857.ab. [DOI] [PubMed] [Google Scholar]
- 18.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation: A selected survey of ABS members. Spine (Phila Pa 1976) 1993;18:2231–8. doi: 10.1097/00007632-199311000-00015. discussion 2238-9. [DOI] [PubMed] [Google Scholar]
- 19.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws: Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 1997;22:977–82. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 20.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems: An assessment of transpedicular screw fixation in the cervical spine. Spine (Phila Pa 1976) 1994;19:2529–39. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 21.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–28. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Ebraheim N, Rollins JR, Jr, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine (Phila Pa 1976) 1996;21:691–5. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Ebraheim NA, Xu R, Knight T, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine (Phila Pa 1976) 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 24.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpedicular screw placement in the cervical spine: An analysis of two approaches. Spine (Phila Pa 1976) 1996;21:2317–22. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Stanescu S, Ebraheim NA, Yeasting R, Bailey AS, Jackson WT. Morphometric evaluation of the cervico-thoracic junction:Practical considerations for posterior fixation of the spine. Spine. 1994;19:2082–8. doi: 10.1097/00007632-199409150-00014. [DOI] [PubMed] [Google Scholar]
- 26.Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine (Phila Pa 1976) 1998;23:1566–71. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 27.Ebraheim NA, Xu R, Ahmad M, Yeasting RA. Projection of the thoracic pedicle and its morphometric analysis. Spine (Phila Pa 1976) 1997;22:233–8. doi: 10.1097/00007632-199702010-00001. [DOI] [PubMed] [Google Scholar]
- 28.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine: Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–6. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, et al. Placement of pedicle screws in the thoracic spine: Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–9. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 1987;12:160–6. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Belmont PJ, Jr, Klemme WR, Robinson M, Polly DW., Jr Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine. 2002;27:1558–66. doi: 10.1097/00007632-200207150-00015. [DOI] [PubMed] [Google Scholar]
- 32.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:1399–405. [PubMed] [Google Scholar]
- 33.Xu R, Ebraheim NA, Ou Y, Yeasting RA. Anatomic considerations of pedicle screw placement in the thoracic spine: Roy-Camille technique versus open-lamina technique. Spine (Phila Pa 1976) 1998;23:1065–8. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 34.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–9. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 35.Ludwig SC, Kowalski JM, Edwards CC, 2nd, Heller JG. Cervical pedicle screws: Comparative accuracy of two insertion techniques. Spine (Phila Pa ) ;25. 1976;2000:2675–81. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 36.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: Comparative accuracy of three techniques. Spine (Phila Pa 1976) 2000;25:1655–67. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 37.Rampersaud YR, Lee KS. Fluoroscopic computer-assisted pedicle screw placement through a mature fusion mass: An assessment of 24 consecutive cases with independent analysis of computed tomography and clinical data. Spine (Phila Pa 1976) 2007;32:217–22. doi: 10.1097/01.brs.0000251751.51936.3f. [DOI] [PubMed] [Google Scholar]
- 38.Richter M, Amiot LP, Neller S, Kluger P, Puhl W. Computer-assisted surgery in posterior instrumentation of the cervical spine: An in-vitro feasibility study. Eur Spine J. 2000;9:S65–70. doi: 10.1007/PL00010024. [DOI] [PMC free article] [PubMed] [Google Scholar]


