INTRODUCTION
Colledge et al. suggested a direct-to-patient health information intervention enhances both patient communication and education, and they recommended that physicians consider the Internet a patient educational tool [1]. However, despite the easy availability of accurate medical information on the Internet, the majority of clinical practices have not successfully incorporated Internet education into clinic workflow.
McMullen suggested physicians might save time, contribute to patient education, and influence patient information seeking by recommending health information websites tailored to a patient's specific condition [2]. D'Alessandro et al. [3] and Siegel et al. [4] used the term “information prescription” to describe a physician-directed Internet health education intervention. In these studies, physicians provided condition-specific, paper-based information prescriptions for patient education and communication. These prescriptions have been tied, in some cases, to Medline Plus [5], a comprehensive, commercial-free, Internet-based consumer health information resource provided by the US National Library of Medicine [4]. Siegel et al. reported modest improvements in patient health information seeking, increased awareness of MedlinePlus, and increased patient interest when receiving an information prescription from a physician [4]. D'Alessandro et al. also found improvements in Internet health information seeking, although only 32% of patients who were given paper information prescriptions had used them during the follow-up period [3]. Ritterband et al. found that an email reminder increased patient compliance with paper information prescriptions by 45% [6].
While the literature suggests that information prescriptions can modestly enhance patient education, studies to date have relied on paper-based prescriptions or verbal recommendations, which might have resulted in limited compliance. To test this hypothesis, the authors created email information prescriptions for selected medical conditions that were specifically tailored with physician-selected links to MedlinePlus. The authors hypothesized that: (1) a physician-directed, condition-specific, email information prescription (using links to the MedlinePlus website) would be favorably evaluated by patients; and (2) intervention patients would be more likely to use MedlinePlus when compared to a control group. The authors also anticipated that a physician-directed, condition-specific information prescription would be favorably received by internists in an ambulatory and a HIV clinic setting.
METHODS
The study was conducted in two consecutive phases, one in which eligible clinic patients were assigned to the control group and one in which they were assigned to an intervention group. During each phase, a research assistant addressed consecutive patients during their appointments in the clinic and informed them of their physicians' participation in the study. Patients who were at least eighteen years of age, had Internet access, retained an email address and voluntarily provided it, and gave consent were included in the study.
The control group received no further intervention and was mailed the study questionnaire one week after the clinic visit. The questionnaire (Appendix, online only) assessed what their health information–seeking behavior was, what information on health education materials they received during the visit, and whether they had heard of, or used, MedlinePlus.
The intervention group participants were informed by their physicians about the health information prescription using a standardized script and were given a form, which indicated their specific health condition, to be taken to the research assistant. Upon receipt of the form, the research assistant obtained consent (including Health Insurance Portability and Accountability Act authorization) and informed patients they would receive a health-related email. The medical librarian emailed this health information prescription within twenty-four hours of their visit. Prior to implementation, twenty-one common medical conditions were selected based on the most common diagnoses seen in each clinic prior to the start of this study, and condition-specific emails were created with input from the participating physicians. Each email contained a condition-specific link to the corresponding health topic page on MedlinePlus and three to four additional links selected from a MedlinePlus search. Patients who did not have one of the twenty-one preselected conditions were not included in the study.
The intervention group received the questionnaire mailed to the control group but with questions added regarding the prescription information and MedlinePlus. The survey was sent two weeks after their clinic visits to provide time for participants to respond to the emailed information prescription request.
All ten board-certified internists practicing in a single general internal medicine ambulatory and HIV clinic agreed to participate in this pilot study. Prior to the intervention, participating physicians and staff attended a presentation by a medical librarian introducing them to MedlinePlus. Participating physicians completed a survey about their reactions and clinical experiences after the intervention was completed. The study was approved by the University of Missouri Health Sciences Institutional Review Board.
A pre-study calculation indicated a sample size of 120 patients in each group was needed to detect a difference of approximately 10% between the control group and intervention group. The authors projected that 60% of enrolled and eligible patients would respond to the survey, so the targeted accrual was 200 patients per group.
RESULTS
Patients
A total of 1,085 patients (556 in the control group and 529 in the intervention group) were approached during their clinic visits to participate in this study. Of these patients, 219 in the control group and 207 in the intervention group met the eligibility criteria. One hundred and one patients in the intervention group and 123 patients in the control group completed and returned the survey, for a return rate of 46% and 59%, respectively. The post-hoc power was 77%, which was due to the somewhat less than anticipated survey return rate.
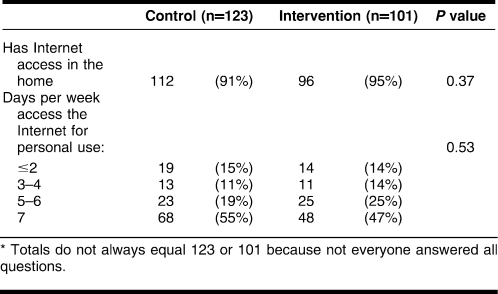
Of the 426 patients who met the eligibility requirement, there were no significant differences between the intervention and control groups in terms of age, gender, race, insurance status, or self-assessed medical conditions. The 224 patients who returned the survey had similar characteristics: most were caucasian (90% compared to 90% of the eligible participants). Patients who returned the survey were highly educated (62% were college graduates or higher), and 93% reported they had Internet access in their home (Table 1). The tables contain the results for both groups in terms of health information–seeking behaviors.
Table 1.
Survey responses: Internet access*
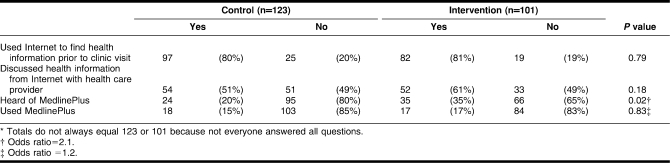
There were no significant differences between the control and intervention patients in Internet use to find health information prior to the clinical visit (P = 0.79) and no differences in discussing health information from the Internet with a health care provider (P = 0.18). Nearly 80% of patients in both groups reported frequent use of the Internet prior to a clinical visit. While a higher percentage of patients in the intervention group had heard of MedlinePlus (20% vs. 35%, P = 0.02), there was no significant difference in the percentage who reported use of MedlinePlus (15% for the control group and 17% for the intervention group; P = 0.83) (Table 2).
Table 2.
Survey responses: Internet use for health information*
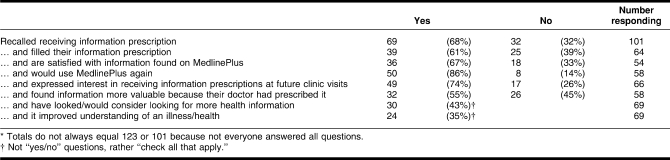
However, while only a small number reported use of MedlinePlus, a considerably greater proportion indicated that they filled the prescription and visited the MedlinePlus Internet site (Table 3). Sixty-nine (70%) indicated they had received the health information prescription, and of these, 39 (61%) had filled it. Of the intervention group subpopulation who filled their health information prescription, 67% of those responding to the question (36 of 54 respondents) indicated they were satisfied with the health information they found on MedlinePlus. When asked if they would use the website again, 86% (50 of 58) responded affirmatively, 74% (49 of 66) reported an interest in receiving health information prescriptions at future clinic visits, 43% (30 of 69) indicated that a health information prescription fostered increased health information seeking, and 35% responding to the question (24 of 69) said the information prescription improved their understanding of an illness or health problem. Finally, 55% (32 of 58) found the information in an information prescription was more valuable because their doctors prescribed it. The contradiction between these responses and answers to the questions on awareness of MedlinePlus might indicate that MedlinePlus use was underreported and/or that individuals were confused by the terms used to refer to the study Internet site.
Table 3.
Survey responses: information prescription*
Anecdotal observations from the research staff (who interacted with control and intervention patients) suggested widespread patient interest from the intervention group in receiving supplementary emailed health information. Some patients requested health information recommendations about conditions not specifically addressed during their office visits. Some patients requested emailed information prescriptions for medical conditions that were not included in the study's standardized, preselected list, and others selected the medical conditions of family members and friends in order to share emailed information prescriptions with them.
Physicians
All study physicians wrote health information prescriptions for patients. Five of the ten participating physicians reported the intervention encouraged patient compliance, reduced office time for patient education, and helped explain difficult concepts, procedures, or medications. Four physicians reported a condition-specific information prescription using MedlinePlus reduced patient anxiety. Three physicians said a MedlinePlus information prescription improved patient compliance and patient communication. To improve future interventions, four physicians recommended expanding the list of twenty-one common medical conditions.
DISCUSSION
The authors hypothesized that a physician-directed, condition-specific email prescription incorporating MedlinePlus would be favorably evaluated by patients and that an intervention group who received such prescriptions would be more likely to use MedlinePlus compared to controls. The findings provide mixed support for the second hypothesis and partially support the first. The expected increase in MedlinePlus use did not occur, although the percentage of persons in the intervention group who reported they had heard about Medline Plus was significantly higher. That only 17% of the intervention group indicated in response to a question that they had used MedlinePlus was notable and inconsistent with other survey responses supporting use of and satisfaction with the email prescription. Two-thirds of the intervention group indicated they received their prescription, and 40% reported they filled it. Of these uses, over two-thirds were satisfied with the information they found on MedlinePlus and 86% reported they would be likely to use MedlinePlus again. Finally, the majority indicated interest in receiving health information prescriptions during future clinic visits and found online prescriptions more valuable because their physicians prescribed them.
These findings are partially consistent with patient findings reported in previous studies [3, 4]. They demonstrate that barriers to the use of health information prescriptions in clinical practice remain despite physician-initiated, condition-specific emails. Attrition in physician participation was not a factor here as in previous studies [7], but the sample size was too small to evaluate whether physician acceptance of an information prescription was consistent with the favorable response reported previously [4]. Other limitations include the highly educated sample and the completion of the surveys by less than half of the eligible subjects.
An information prescription intervention presents some research challenges. Without a validity check, it is difficult to know if patients followed instructions. About half the patients did not recall that they had received an “information prescription.” The term, “information prescription,” is perhaps unfamiliar to patients; future researchers need to explain its meaning to study participants. Problems with terminology may also explain patients' inconsistent responses with regard to using the Internet site versus using MedlinePlus. Careful consideration is needed when encouraging the use of Internet-based resources and the use of specific site resources. Besides email and handwritten options, alternative information prescription delivery approaches need to be assessed, such as encouragement of patients to register on a clinic-based website with links to health information (which potentially provides compliance metric).
CONCLUSION
The findings suggest that patients respond favorably to a physician-directed, condition-specific email prescription, initiated in the context of a routine clinic visit, that relies on health information from a comprehensive Internet-based resource (such as MedlinePlus). Patients who reported they visited the Internet site and used MedlinePlus were satisfied with the health information they received and were enthusiastic about its future use. Further strategies are needed to encourage patients to “fill” an information prescription, to clarify specific targeted Internet sites, and to integrate information prescriptions into a provider's workflow to ensure compliance.
Electronic Content
Footnotes
This project was supported by contract no. HHSN276200700263P from the National Library of Medicine.
A supplemental appendix is available with the online version of this journal.
Contributor Information
Emily Coberly, Associate Professor of Clinical Medicine, MA432 Medical Science Building, School of Medicine, University of Missouri, Columbia, MO 65212 coberlye@health.missouri.edu.
Suzanne Austin Boren, Research Health Scientist, Health Services Research and Development, Harry S. Truman Memorial Veterans' Hospital, Columbia, MO 65212, and Assistant Professor, Department of Health Management and Informatics, School of Medicine, University of Missouri, Columbia, MO 65212 borens@health.missouri.edu.
J. Wade Davis, Assistant Professor, Department of Health Management and Informatics, School of Medicine, and Assistant Professor, Department of Statistics, and Biostatistics Group, School of Medicine davisjwa@health.missouri.edu.
Amanda L McConnell, Librarian, J. Otto Lottes Health Sciences Library amcconnell@lawrence.lib.ks.us.
Rebecca Chitima-Matsiga, Research Specialist, Department of Internal Medicine, School of Medicine chitima-matsigar@health.missouri.edu.
Bin Ge, Statistician, Biostatistics Group, School of Medicine; University of Missouri, Columbia, MO, 65212 geb@health.missouri.edu.
Robert A Logan, National Library of Medicine, Bethesda, MD logan@nlm.nih.gov.
William C Steinmann, Professor of Medicine steinmannw@health.missouri.edu.
Robert H Hodge, Professor of Clinical Medicine; Department of Internal Medicine, School of Medicine, University of Missouri, Columbia, MO 65212 hodger@health.missouri.edu.
REFERENCES
- 1.Colledge A, Car J, Donnelly A, Majeed A. Health information for patients: time to look beyond patient information leaflets. J R Soc Med. 2008 Sep;101(9):447–53. doi: 10.1258/jrsm.2008.080149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McMullan M. Patients using the Internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns. 2006 Oct;63(1–2):24–8. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 3.D'Alessandro D.M, Kreiter C.D, Kinzer S.L, Peterson M.W. A randomized controlled trial of an information prescription for pediatric patient education on the Internet. Arch Pediatr Adolesc Med. 2004 Sep;158(9):857–62. doi: 10.1001/archpedi.158.9.857. [DOI] [PubMed] [Google Scholar]
- 4.Siegel E.R, Logan R.A, Harnsberger R.L, Cravedi K, Krause J.A, Lyon B, Hajarian K, Uhl J, Ruffin A, Lindberg D.A.B. Information Rx: evaluation of a new informatics tool for physicians, patients, and libraries. Inform Services Use. 2006;26(1):1–10. doi: 10.3233/isu-2006-26101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US National Library of Medicine. MedlinePlus [Internet] Bethesda, MD: The Library; 2009 [cited 6 Jul 2009]. < http://www.medlineplus.gov>. [Google Scholar]
- 6.Ritterband L.M, Borowitz S, Cox D.J, Kovatchev B, Walker L.S, Lucas V, Sutphen J. Using the Internet to provide information prescriptions. Pediatrics. 2005 Nov;116(5):e643–7. doi: 10.1542/peds.2005-0404. [DOI] [PubMed] [Google Scholar]
- 7.Leisey M.R, Shipman J.P. Information prescriptions: a barrier to fulfillment. J Med Libr Assoc. 2007 Oct;95(4):435–8. doi: 10.3163/1536-5050.95.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.