Abstract
Objective:
Anger and other indices of negative affect have been implicated in a stress-induced pathway to relapse. The Alcoholics Anonymous (AA) literature states that reduction of anger is critical to recovery, yet this proposed mechanism has rarely been investigated. Using lagged, controlled hierarchical linear modeling analyses, this study investigated whether AA attendance mobilized changes in anger and whether such changes explained AA-related benefit.
Method:
Alcohol-dependent adults (N = 1,706) receiving treatment as part of a clinical trial were assessed at intake and at 3, 6, 9, 12, and 15 months.
Results:
Findings revealed substantially elevated levels of anger compared with the general population (98th percentile) that decreased over 15-month follow-up but remained high (89th percentile). AA attendance was associated with better drinking outcomes, and higher levels of anger were associated with heavier drinking. However, AA attendance was unrelated to changes in anger.
Conclusions:
Although support was not found for anger as a mediator, there was strong convergence between AA's explicit emphasis on anger and the present findings: Anger appears to be a serious, enduring problem related to relapse and heavy alcohol consumption. Methodological factors may have contributed to the lack of association between AA and anger, but results suggest that AA attendance alone may be insufficient to alleviate the suffering and alcohol-related risks specifically associated with anger.
Anger, irritability, depression, boredom, and other indices of negative affect have all been implicated in a stress-induced pathway to relapse among alcohol and other drug-dependent individuals (Cummings et al., 1980; Greenfield et al., 1998; Marlatt and Gordon, 1980, 1985; Shaham et al., 2003). Such affective symptoms and syndromes may represent long-standing affect regulation difficulties that predate alcohol and drug-use problems. Alternatively, they may have emerged later either independent of, or resulting from, the combined effects of poor nutrition and heavy drinking/drug use on brain structure and neuro-physiological function (Martin et al., 2003; Rourke and Loberg, 1996). Whatever the actual cause, difficulties in affect regulation present recovery challenges for many suffering from addiction.
Substance-use disorder treatments seek to redress these affective difficulties acutely through medical stabilization and pharmacological means, as well as through psychological interventions intended to help restructure cognition and behavior to reduce or buffer the intensity and duration of negative affect. In addition to professional treatment, commonly used evidence-based adjunctive continuing-care resources (Humphreys, 2004; Kelly and Yeterian, 2008), such as Alcoholics Anonymous (AA), place high importance on successful affect regulation to prevent relapse (AA, 1953, 2001). A large number of research studies during the past 25 years have indicated that AA is helpful to many different types of individuals in their recovery efforts (Emrick et al., 1993; Humphreys, 2004; Kaskutas et al., 2002; Kelly, 2003), but the exact reasons why it is helpful have only recently begun to be investigated.
Role of anger in Alcoholics Anonymous's recovery program
A large number of studies have examined the relationship between AA attendance and drinking behavior, but only a handful of studies have specifically examined how AA attendance may actually facilitate recovery. Such studies that have performed appropriate mediational tests (see MacKinnon, 2008) have found that measures of coping, motivation, self-efficacy, social network changes, and spirituality appear to be some of the mechanisms through which AA transmits its beneficial effects (Forceheimes and Tonigan, 2008; Kelly et al., 2009). However, to our knowledge, important affect-related mechanisms that AA itself specifies as critical to recovery have not been formally tested.
From the AA core literature, anger is singled out as a uniquely potent and high-risk emotion for relapse to alcohol use: "Resentment is the number one offender. It destroys more alcoholics than anything else. … If we were to live we had to be free of anger" (AA, 2001, pp. 64, 66). Consequently, a key emphasis in the 12-step program documented in AA's main text, Alcoholics Anonymous (1939, 2001), is to reduce anger and thus reduce the probability of relapse (AA, 2001). In fact, anger is the only construct in the AA literature for which a detailed column-based worksheet is provided to help members document, analyze, and remediate angry thoughts and feelings (AA, 2001).
Prior research with substance-dependent samples has found that negative affect predicts treatment outcome (Greenfield et al., 1998; Marlatt and Gordon, 1980, 1985), but this is not always the case. Specifically, client anger at intake did not predict either frequency or intensity of drinking among outpatient and aftercare clients in Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) during the first 6 months following treatment, a time when most alcohol relapse occurs (Waldron et al., 2001). However, anger in relationship to drinking over time was not reported. Client anger did lead to a differential treatment response in Project MATCH such that more angry clients assigned to motivational enhancement therapy fared significantly better at 1- and 3-year follow-up relative to angry clients assigned to cognitive-behavioral therapy or 12-step facilitation (Waldron et al., 2001). This finding may be related to the nonconfrontational counseling style of motivational enhancement therapy. In a Project MATCH sample, an interaction of therapist confrontation/structure and client anger led to poor drinking outcomes (Karno and Longabaugh, 2003, 2005). Anecdotal reports sometimes portray AA as confrontational, but these may be confusing AA with reports of 12-step-oriented professional counselors. The AA core literature explicitly describes the AA approach as one of respect and explicitly nonconfrontational (AA, 2001). Further research on how anger is related to relapse risk and whether AA attendance can help mitigate that risk could elucidate some of the ways in which AA benefits members and provides a test of one of AA's central recovery hypotheses.
Using a large sample of alcohol-dependent men and women receiving treatment as part of a randomized controlled trial—that is, Project MATCH (Project MATCH Research Group, 1993)—this article examined the relationship between AA attendance, anger, and drinking outcomes. Because anger is an important factor in theories of relapse and recovery (e.g., AA, 2001; Marlatt and Gordon, 1985), as well as interpersonal difficulties and psychological and physical disorders, including alcohol relapse, we first examined the degree to which levels of anger in this alcohol-dependent, treatment-seeking sample differed from the level of anger in the general population. Second, we explored the clinical course of anger over the 15 months of the study follow-up period. Third, we examined the nature of the relationship between anger and AA attendance over time and whether any beneficial effects of AA on drinking might be explained (mediated) by reductions in reported anger. Also, given that the content of the AA 12-step program (AA, 1939)—as explicated in the "Big Book" when first published in 1939 and that remains unchanged in the fourth edition (AA, 2001)—was derived almost exclusively from male alcoholics (AA, 1957), we examined whether gender moderated the influence of AA on anger by reducing anger more for men than for women.
In keeping with the criteria outlined by Kazdin and Nock (2003; Nock, 2007) on enhancing cause-effect conclusions in mechanisms of behavior change, we used lagged hierarchical linear modeling (HLM) to test this purported affective mediator over time, controlling for important static and time-varying covariates. We hypothesized that anger would be significantly elevated among alcohol-dependent individuals, compared with the general population, and that it would decrease over time as a function of reductions in drinking. We also hypothesized that AA attendance would be associated independently with significant reductions in anger over time and that this reduction would partially mediate the salutary effect of AA on subsequent drinking outcomes.
Method
Subjects
There were two samples used in the original Project MATCH trial (N = 1,726): an outpatient sample (n = 952; 72% male) and an aftercare sample (n = 774; 80% male). The aftercare sample was recruited directly following residential treatment. The current study is based on a sample of 1,706 followed through 15 months (n = 746 aftercare subjects; n = 942 outpatient subjects). Overall, outpatients were significantly younger, more residentially stable, and less dependent on alcohol than the aftercare patients (Goodman et al., 1992; Timko et al., 1993). A smaller proportion of outpatients (45%) than aftercare patients (62%) reported prior alcohol-use-disorder treatment. The vast majority of patients in each trial arm (95% in outpatient, 98% in aftercare) met the criteria for alcohol dependence as opposed to alcohol abuse, as assessed using the Structured Clinical Interview for DSM-III-R (Spitzer and Williams, 1985). Although individuals dependent on other drugs (except marijuana) were excluded from the trial, there was a sizable minority of subjects who reported some type of illicit drug use in the 90 days before recruitment (44% in the outpatient arm [n = 417] and 32% in the aftercare arm [n = 247]). Table 1 further describes the characteristics of the sample.
Table 1.
Demographic characteristics, by study arm
| Variable | Aftercare (n = 764) | Outpatient (n = 942) |
| Age, years, M (SD) | 41.9 (11.1) | 38.8 (10.7) |
| Education, years, M (SD) | 13.1 (2.0) | 13.4 (2.1) |
| Female gender, % | 20.3 | 27.3 |
| Ethnicity, % | ||
| White | 80.5 | 79.8 |
| Hispanic | 14.8 | 5.6 |
| Black | 3.5 | 12.3 |
| Other | 1.2 | 2.2 |
| Married/cohabiting, % | 33.8 | 35.7 |
| Employed full time, % | 47.5 | 51.06 |
Recruitment sites
Subjects were recruited at nine clinical research units. The five outpatient clinical research units were located in Albuquerque, NM; Buffalo, NY; Farmington, CT; Milwaukee, WI; and West Haven, CT. The aftercare clinical research units were located in Charleston, SC; Houston, TX; Milwaukee, WI; Providence RI; and Seattle, WA. Outpatient sites recruited subjects from outpatient clinics and directly from the community through advertisements. Aftercare sites included subjects who had been treated in private, public, and Department of Veterans Affairs treatment facilities.
Inclusion/exclusion criteria
Inclusion criteria for the outpatients were current Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R), diagnosis of alcohol abuse or dependence (American Psychiatric Association, 1987); alcohol was the principal drug of misuse; alcohol was used during the 3 months before study entry; the minimum age was 18; and the minimum reading level was sixth grade. Exclusion criteria included the following: a DSM-III-R diagnosis of current dependence on sedative/hypnotic drugs, stimulants, cocaine, or opiates; any intravenous drug use in the prior months; being a current danger to one's self or to others; existing probation/parole requirements that might interfere with protocol attendance; lack of clear prospects for residential stability; inability to identify at least one "locator" person to assist in tracking for follow-up assessments; acute psychosis; or severe organic impairment.
Procedures
Following recruitment, subjects in both trial arms were randomly assigned to one of three individually delivered, psychosocial intervention conditions: cognitive-behavioral therapy (Kadden et al., 1992), motivational enhancement therapy (Miller et al., 1992), and 12-step facilitation (Nowinski et al., 1992). Twelve-step facilitation and cognitive-behavioral therapy consisted of 12 sessions delivered weekly over 12 weeks. Motivational enhancement therapy consisted of four sessions delivered over 12 weeks at Weeks 1, 2, 6, and 12. Study participants were subsequently reassessed at 3, 6, 9, 12, and 15 months following the end of the delivered treatments.
In both study arms, the follow-up rates remained above 90% at all five follow-ups (at 3, 6, 9, 12, and 15 months). This figure includes subjects for whom data from an earlier follow-up were reconstructed at a later follow-up (the frequency of such reconstruction for any given assessment period ranged from 4% to 6% for outpatient participants and from 4% to 8% for aftercare participants). More complete details regarding this trial are available elsewhere (e.g., Project MATCH Research Group, 1997).
Measures
Alcohol use.
Estimates of alcohol consumption were assessed using Form 90 (Miller, 1996; Miller and Del Boca, 1994), an interview procedure combining calendar Timeline Followback methodology (Sobell and Sobell, 1992) and drinking pattern estimation procedures from the Comprehensive Drinker Profile (Miller and Marlatt, 1984). In addition to estimating alcohol consumption for each of the previous 90 days, Form 90 elicits information about drug use, treatment experiences, incarceration, and involvement with AA.
Alcoholics Anonymous attendance.
AA attendance was assessed using Form 90, which captured the number of AA meetings attended at intake and at 3-, 6-, 9-, 12-, and 15-month follow-up time points. The percentage of days attending AA was the variable constructed to examine AA. This was calculated as the number of days a patient attended AA divided by the number of days in the time period covered in that follow-up period (e.g., 90 days) multiplied by 100.
Affect measures.
Anger was assessed using the Spielberger Anger Scale (Spielberger, 1988). This 15-item face valid scale is conceived as a psychobiological construct and measures angry feelings particularly pertaining to feelings of being treated unfairly by others and experiencing frustration (e.g., "I feel angry, " "I feel irritated, " "People who think they are always right irritate me, " and "It makes me furious when I am criticized in front of others").
Statistical methods
Descriptives and data transformation.
Means, standard deviations, and frequencies were calculated for descriptive statistics. Variables were examined for their skewness and kurtosis. Both of the dependent variables (percentage of days abstinent [PDA] and drinks per drinking day [DDD]) and AA attendance variable required transformations. The negatively skewed PDA variable received an arcsine transformation, and the positively skewed DDD variable was given a square root transformation, as was done in the primary MATCH outcome analyses (Project MATCH Research Group, 1997; Tabachnick and Fidell, 2001). AA attendance was also positively skewed and was log-transformed. However, when we ran models with and without the log-transformation of AA attendance, we did not find a difference in the pattern of magnitude or significance of the findings. Thus, for easier interpretability of parameter estimates, we report descriptive statistics using untransformed AA attendance.
Comparing and modeling anger.
We compared measured levels of anger in the current study with the pertinent published norms from the State-Trait Anger Expression Inventory (STAXI) procedures manual using means, standard deviations, and percentile scores. We modeled the clinical course of anger over the course of the follow-up from intake to the 15-month time point using a repeated-measures analysis of variance (ANOVA) with time, treatment assignment, and Time x Treatment Assignment interaction terms included in the model.
Longitudinal lagged controlled analyses.
To examine the relationship between AA attendance, anger, and alcohol-use outcomes across time, we used lagged HLM, with both static and time-varying covariates. Separate HLM models were run for the aftercare and outpatient samples and for each dependent alcohol-use variable (i.e., PDA and DDD) to examine (a) the independent (AA attendance) to dependent variable path, (b) the independent to mediator (anger) path, (c) the mediator to dependent variable path, and (d) the product of the independent variable to mediator, and mediator to dependent variable paths. To make the mediation tests prospective (lagged), we used pairs of time points in which time-varying predictors were used for time-varying outcomes; e.g., AA attendance in the past 90 days at Month 3 to predict anger scores at Month 9, and AA at Month 9 to predict anger at Month 15; similarly, we used anger at Months 3 and 9 to predict drinking outcomes (transformed PDA and DDD) at Months 9 and 15. Static covariates included in these models were age, ethnicity, gender, a Gender x Time interaction, marital status (married/cohabiting vs. not), employment (employed full time in the past 6 months vs. not), number of prior alcohol-related treatments, treatment assignment, treatment site, the relevant intake level of the dependent variable (i.e., anger, PDA, and DDD), and an interaction term between AA attendance and the intake assessment of the dependent variable.
Missing data and imputation.
To address the amount of missing data during follow-up, we used multiple imputation (Little and Rubin, 2002). The amount of data missing for key variables in our analyses for which there were some missing values ranged from 0.05% for baseline AA attendance to 7.8% for drinking data for Months 13-15. Because the missing data patterns were nonmonotone (i.e., many data were intermittently missing), we used the Markov Chain Monte Carlo method for the multiple imputation (Gilks et al., 1996). We performed 10 imputations using the procedures MI and MIANALYZE of SAS 9.1.3 (SAS Institute Inc., Cary, NC). The statistics we report for the variables in our analyses are the averaged results across the 10 imputations. The degrees of freedom for the reported t statistics for each regression coefficient vary from analysis to analysis, given the recommended use of adjusted degrees of freedom (Barnard and Rubin, 1999).
Mediation.
We take the approach to testing mediation described by MacKinnon and colleagues (MacKinnon and Dwyer, 1993; MacKinnon et al., 2002). It represents an improvement over the earlier methods of Judd and Kenny (1981). The MacKinnon method tests directly for the existence of a significant path from variable A through B to variable C by computing a product of the regression coefficients for the A–B and B–C associations. Its statistical power is better than that of competing alternatives (MacKinnon et al., 2002).
Results
The descriptive statistics of demographics of the sample are detailed in Table 1. Most participants were male, White, and single. Table 2 provides descriptive data related to the proportion of patients attending any AA meetings during each follow-up period and the average number of meetings attended. Also, Table 2 shows drinking outcomes and anger scores over time and by treatment arm. As noted in prior published work on this study (Tonigan et al., 2003), the rates of AA attendance were quite high, even among patients assigned to treatments that did not explicitly endorse AA attendance. This was particularly true of patients in the aftercare arm of the trial who had received treatment before study entry (most of which may have endorsed a 12-step model); thus, the effect of specific recommendations to attend AA was more pronounced. As shown, the proportion of patients who attended AA and the rates at which they attended were substantially elevated in the aftercare sample relative to the outpatient sample across all time points, with substantial numbers from both patient groups discontinuing attendance and showing a decline in the rate of attendance over the first year following treatment.
Table 2.
Alcoholics Anonymous (AA) attendance, anger, and alcohol-use outcomes, by study arm
| Aftercare (n =764) |
Outpatient (n = 942) |
|||||||
| Variable | 0 months | 3 months | 9 months | 15 months | 0 months | 3 months | 9 months | 15 months |
| Any AA, % | 81.3 | 84.9 | 56.5 | 53.6 | 38.8 | 46.2 | 29.4 | 30.2 |
| AA, M (SD) | 23.2 (42.2) | 32.4 (32.3) | 19.0 (27.3) | 17.4 (26.1) | 9.8 (33.6) | 11.0 (20.3) | 7.8 (18.9) | 7.7 (18.5) |
| Anger, M (SD) | 30.8 (7.6) | 28.7 (7.6) | 27.7 (7.4) | 27.4 (7.9) | 29.5 (7.2) | 27.0 (6.7) | 26.4 (7.0) | 25.6 (6.6) |
| PDA, M (SD) | 26.7 (29.6) | 90.0 (21.3) | 80.9 (29.9) | 79.5 (31.9) | 34.2 (29.9) | 79.9 (27.3) | 73.9 (31.2) | 72.9 (33.3) |
| DDD, M (SD) | 20.3 (11.9) | 6.0 (9.7) | 6.9 (9.9) | 6.3 (9.4) | 13.5 (8.0) | 7.5 (8.0) | 6.3 (6.6) | 5.8 (6.2) |
Notes: PDA = percentage of days abstinent; DDD = drinks per drinking day.
Anger levels among alcohol-dependent patients compared with the general population
Normative data collected on the total anger scale of the STAXI with adults (Spielberger, 1991) revealed an average mean score of 19.08 (SD = 5.0; N = 5,679). The mean level of anger assessed in this clinical sample overall was substantially elevated relative to the normative data at 30.08 (SD = 7.4; n = 1,351). There was a smaller, but statistically significant, magnitude difference between study arms, with the aftercare patients reporting more anger on average than the outpatients (Maftercare = 30.82 [7.60] vs. Moutpatient = 29.47 [7.25]; t = 4.85, p < .001). A single sample t test with the population norm value entered as the test value revealed a highly significant overall mean difference of 10.99 points (95% CI [10.64, 11.35]; t = 60.29, p < .0001), and this translates into a large standardized effect size (d = 2.1). Compared with the average person's level of anger in the general population, the alcohol-dependent patients in this study scored in the 98th percentile.
Clinical course of anger over time
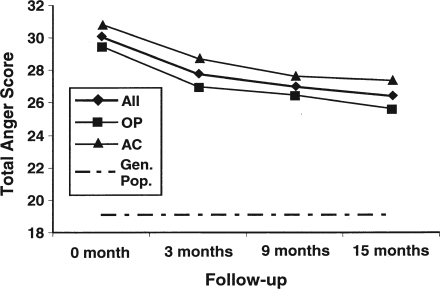
Results from the repeated-measures ANOVA revealed a significant and quite large main effect of change in anger over time for both aftercare (F = 73.73, p < .0001) and outpatient (F = 137.66, p < .0001) participants. However, these significant reductions in anger over time were not found to interact with study arm or treatment assignment (p > .74; Figure 1).
Figure 1.
Total anger scale score as a function of trial arm and time. General population (Gen. Pop.) curve was measured at a single time point only, but is depicted over time for consistency and to highlight the magnitude difference in samples. OP = outpatient; AC = aftercare.
There was a reduction in anger following treatment that continued through 15-month follow-up. There were similar rates of anger reduction across the two arms of the trial, although as noted earlier, the aftercare arm had higher anger on treatment intake. At the end of the 15-month follow-up, anger was at its lowest point (M = 26.40), falling from a 98th percentile rank to an 89th percentile, compared with general population norms. Although reduced, this value remains notably higher than the general population. Also, Spearman rank-order correlation analyses revealed that higher anger was consistently related to more frequent alcohol consumption measured by PDA (rs range: -.08 to -.18, ps .01 to < .0001) and more intensive alcohol use measured by DDD (rs range: .14 to .22, ps < .0001) at every follow-up time point. Anger was, therefore, more strongly associated with intensity, than frequency, of drinking.
Longitudinal mediational analysis: Relationship between Alcoholics Anonymous, anger, and alcohol use over time
To examine the relationship between AA, anger, and alcohol-use outcomes across time we employed lagged, controlled HLM, with both static and time-varying covariates as detailed in the Method section. To deal with the problem of varying amounts of missing data, we used multiple imputation procedures described earlier. We also conducted the more typical, nonimputed, lagged, and controlled HLM analyses, excluding cases with missing values, to compare parameter estimates and inferential results using both methods. As explained in more detail in the following, the two methods did not generally produce differences in the overall pattern of findings but did alter parameter magnitudes and significance levels in some of the estimated relationships between variables.
For mediation to be supported, preliminary requirements are that (a) the independent variable (AA) is significantly related to the outcome (alcohol use), (b) the mediator (anger) is significantly related to the outcome (alcohol use), and (c) the independent variable is related to the mediator (anger). Each of these three elements of the model are described next.
Relationship between Alcoholics Anonymous and alcohol-use outcomes
Table 3 shows the relationship between AA and subsequent (lagged) alcohol-use outcomes (PDA and DDD) for the outpatient and aftercare samples. As anticipated, there were robust associations between more frequent AA attendance and less frequent, and less intense, subsequent alcohol use across time in both study arms. However, there was also a significant AA x Time interaction effect on both DDD and PDA but only among aftercare patients. Follow-up tests of the interaction revealed that the relationship between AA attendance during the MATCH treatment implementation (Months 1–3) and subsequent alcohol use in the past 90 days at the 9-month follow-up (Months 7–9) was comparatively weaker for both PDA (b = 0.0023) and DDD (b = -0.008) than the relationship between AA attendance in the past 90 days at 9-month follow-up and both PDA (b = 0.0048) and DDD (b = -0.0165) at 15-month follow-up (Months 13–15; ps < .0001).
Table 3.
Hierarchical linear modeling results for Alcoholics Anonymous (AA) attendance predicting transformed percentage of days abstinent (PDA) and drinks per drinking day (DDD) for the outpatient and aftercare samplesa
| Variable | b [95% CI] | t (df) | P |
| Outpatient sample | |||
| Baseline PDA | 0.0045 [0.0039, 0.0052] | 13.34 (479) | <.0001 |
| Lagged AA attendance | 0.0044 [0.003, 0.0059] | 5.91 (419) | <.0001 |
| Lagged AA Attendance × Time | −0.0001 [−0.0021, 0.0020] | −0.08 (440) | .9389 |
| Aftercare sample | |||
| Baseline PDA | 0.0028 [0.0020, 0.0035] | 7.11 (421) | <.0001 |
| Lagged AA attendance | 0.0029 [0.0020, 0.0039] | 5.94 (484) | <.0001 |
| Lagged AA Attendance × Time | 0.0025 [0.0010, 0.0040] | 3.35 (456) | .0009 |
| Outpatient sample | |||
| Baseline DDD | 0.0249 [0.0163, 0.0335] | 5.70 (322) | <.0001 |
| Lagged AA attendance | −0.0116 [−0.0163, −0.0069] | −4.84 (393) | <.0001 |
| Lagged AA Attendance × Time | −0.0034 [−0.0100, 0.0032] | −1.02 (400) | .3100 |
| Aftercare sample | |||
| Baseline DDD | 0.0245 [0.0174, 0.0317] | 6.73 (395) | <.0001 |
| Lagged AA attendance | −0.0108 [−0.0143, −0.0073] | −6.02 (463) | <.0001 |
| Lagged AA Attendance × Time | −0.0086 [−0.0140, −0.0031] | −3.09 (369) | .0021 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, treatment assignment, treatment site, Gender x Time, and AA Attendance x Intake Level of Dependent Variable.
Comparing results from imputed and nonimputed HLM model results, the observed magnitude of effects and related significance levels from these imputed analyses were found to be almost identical to the nonimputed analyses.
There were also found to be three static covariates that made significant contributions to these models for both the aftercare and outpatient samples: younger age (ps < .05), being single (ps < .006), and a greater number of prior alcohol treatments (p < .0001) were all independently associated with less abstinence and more intense drinking.
Relationship between anger and alcohol-use outcomes
Table 4 shows the relationship between anger and subsequent PDA and DDD among both groups of patients. As shown, the relationship between anger and subsequent frequency of alcohol use (PDA) was substantially smaller in magnitude among both outpatient (b = -0.004) and aftercare (b = -0.004) patients, compared with the relationship between anger and intensity of alcohol use (DDD), which was larger in magnitude for both outpatient (b = 0.012) and aftercare (b = 0.015) patients. However, these relationships did not quite reach statistical significance at the .05 level (ps range: .07 to .08).
Table 4.
Hierarchical linear modeling results for Alcoholics Anonymous (AA) attendance predicting anger for the outpatient and aftercare samplesa
| Variable | b [95% CI] | t(df) | P |
| Outpatient sample | |||
| Baseline anger | 0.5700 [0.5059, 0.6341] | 17.48 (403) | <.0001 |
| Lagged AA attendance | −0.0023 [−0.0225, 0.0179] | −0.23 (192) | .8217 |
| Lagged AA Attendance × Anger | 0.0008 [−0.0012, 0.0028] | 0.81 (347) | .4186 |
| Lagged AA Attendance x Time | −0.0126 [−0.0403, 0.0152] | −0.89 (213) | .3726 |
| Aftercare sample | |||
| Baseline anger | 0.6098 [0.5393, 0.6803] | 17.03 (270) | <.0001 |
| Lagged AA attendance | −0.0028 [−0.0200, 0.0138] | −0.34 (226) | .7369 |
| Lagged AA Attendance × Anger | 0.0000 [−0.0013, 0.0014] | 0.05 (287) | .9611 |
| Lagged AA Attendance × Time | 0.0028 [−0.0174, 0.0230] | 0.27 (458) | .7858 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, treatment assignment, treatment site, Gender x Time, and AA Attendance x Intake Level of Dependent Variable.
These imputed, controlled, and lagged HLM results again showed a very similar pattern to the results from the nonimputed HLM models, but the relationship between anger and both drinking outcomes was smaller in the imputed analyses, reaching the level of a trend instead of the greater magnitude and significance level (ps < .0001) in the nonimputed HLM results. Given that both estimation methods are not without error, and therefore approximations, it is possible the actual “true” relationship may lie somewhere between these estimates.
Two static covariates also made significant independent contributions to these models: Patients who were single were significantly less likely to be abstinent in both the aftercare arm (b = -0.067, p = .008) and the outpatient arm (b = -0.064, p = .006), and a greater number of prior alcohol treatments was associated with less abstinence but only among aftercare patients (b = 0.023, p = .008). Similarly, for intensity of drinking (DDD), single men drank more heavily (b = 0.191, p = .03), and among aftercare patients, younger age (b = -0.011, p = .005) and a greater number of prior alcohol treatments (b = 0.186, p < .0001) were associated with heavier drinking.
Relationship between Alcoholics Anonymous and anger
Table 5 shows the relationships between AA and anger. As shown, AA was not found to be related to anger among either group of patients (ps > .73). This null finding was very similar in magnitude and significance levels in both the imputed, as well as the nonimputed, HLM model results. Two static covariates were also found to make significant independent contributions to the modeled prediction of anger: White patients had significantly higher anger than non-White patients but only among aftercare patients (b = -0.839, p = .017); and a greater number of prior alcohol treatments was associated with higher anger but only among outpatients (b = 0.401, p < .0001).
Table 5.
Hierarchical linear modeling results for anger predicting transformed percentage of days abstinent (PDA) and drinks per drinking day (DDD) for the outpatient and aftercare samplesa
| Variable | b [95% CI] | t (df) | P |
| Outpatient sample | |||
| Baseline PDA | 0.0045 [0.0038, 0.0052] | 12.99 (476) | <.0001 |
| Lagged anger | −0.0037 [−0.0079, 0.0005] | −1.74 (394) | .0822 |
| Lagged Anger × Time | −0.0010 [−0.0068, 0.0047] | −0.35 (403) | .7247 |
| Aftercare sample | |||
| Baseline PDA | 0.0029 [0.0021, 0.0037] | 7.10 (397) | <.0001 |
| Lagged anger | −0.0037 [−0.0080, 0.0006] | −1.70 (328) | .0896 |
| Lagged Anger × Time | 0.0021 [−0.0039, 0.0081] | 0.69 (413) | .4899 |
| Outpatient sample | |||
| Baseline DDD | 0.0188 [0.0100, 0.0276] | 4.20 (296) | <.0001 |
| Lagged anger | 0.0121 [−0.0017, 0.0259] | 1.73 (257) | .0847 |
| Lagged Anger × Time | 0.0155 [−0.0024, 0.0335] | 1.70 (455) | .0901 |
| Aftercare sample | |||
| Baseline DDD | 0.0235 [0.0160, 0.0310] | 6.18 (357) | <.0001 |
| Lagged anger | 0.0148 [−0.0012, 0.0308] | 1.82 (221) | .0700 |
| Lagged Anger × Time | 0.0047 [−0.0170, 0.0263] | 0.43 (408) | .6699 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, treatment assignment, treatment site, Gender x Time, and AA Attendance x Intake Level of Dependent Variable.
As mentioned earlier, we also wanted to test whether the influence of AA on anger was different for men and women (AA x Gender interaction). In all models, no significant Gender x AA interaction emerged, suggesting that the link between AA attendance and anger does not differ for men and women (b = 0.003, p = .865).
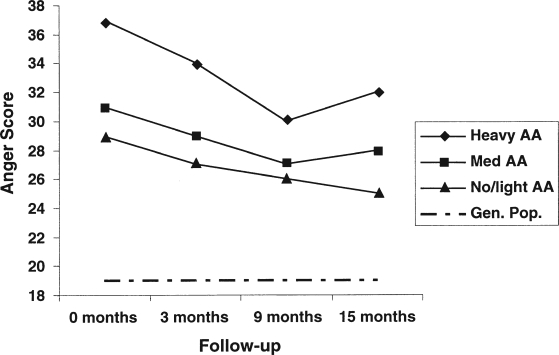
Figure 2 illustrates the change in mean anger scores at treatment intake and at 3-, 9-, and 15-month follow-ups as a function of various levels of AA attendance in the first 3 months. We divided the sample into three AA attendance groups: heavy AA (≥3 days/week), medium AA (≥1 day/ week but <3 days), and no/light AA (<1 day/week). As depicted in Figure 2, patients with the highest anger at treatment intake were significantly more likely to attend AA more frequently (p < .001), but the association between the degree of AA attendance and anger over time was nonsignificant. Consequently, given that one of the paths necessary for mediational testing was not upheld, the notion that AA helps alcohol-dependent individuals to sobriety by decreasing anger was not supported.
Figure 2.
Total anger scale score as a function of Alcoholics Anonymous (AA) attendance and time. General population (Gen. Pop.) curve was measured at a single time point only but is depicted over time for consistency and to highlight the magnitude difference in samples.
Subsidiary analyses: Alcoholics Anonymous involvement and anger as a mediator
Given prior studies that found stronger associations with measures of AA involvement than with frequency of AA attendance (e.g., Montgomery et al., 1995; Weiss et al., 2005), we also examined the relationship between AA involvement (e.g., having a sponsor, working the 12 steps, reading AA literature) and anger. Similar to findings with AA attendance as the predictor, AA involvement was not associated with anger over time. Conclusions should be considered cautiously because of missing data on the AA involvement measure (i.e., 34.5% in aftercare and 48% missing in outpatient).
Discussion
This study examined the psychobiological construct of anger and its relationship to AA attendance and alcohol-use outcomes over the course of 15 months among treatment-seeking individuals enrolled in a large, randomized clinical trial of psychosocial treatments for alcohol dependence. Anger at treatment intake was found to be substantially higher among this alcohol-dependent sample than in the general population, and, although it declined significantly over time, it remained substantially elevated through the final 15-month follow-up. Also, patients higher in anger were more likely to attend AA with greater frequency. The controlled, lagged, longitudinal HLM analyses, with both imputed and nonim-puted data, revealed that AA attendance was robustly related to improved outcome over time, and suggested anger may be more strongly associated with drinking intensity than drinking frequency over time. However, AA was found to be unrelated to anger. Thus, the notion that AA's relationship to sobriety is partially mediated by anger was not supported in the current study.
The level of anger in this alcohol-dependent population is noteworthy for its extent of elevation. According to Spielberger (1991), individuals who score above the 75th percentile are likely to experience anger to a degree that interferes with psychosocial functioning and is likely to negatively affect interpersonal relationships and dispose them to developing psychological and physical disorders. The mean for this sample was at the 98th percentile, and, although it dropped after treatment and in the ensuing 12 months, it fell only to the 89th percentile by Month 15. Because of its significant direct (e.g., elevated blood pressure/hypertension) and indirect (e.g., as a potential precursor to heavy alcohol use) relationships to negative physical and psychosocial health problems, anger's evident enduring tenacity among alcohol-dependent individuals warrants closer clinical attention. Noteworthy, too, was that patients higher in anger attended AA more intensively. This may be indicative of the robust finding that patients with greater addiction severity appear more likely to attend AA following treatment (Emrick et al., 1993; Kelly, 2003; Tonigan et al., 1996), perhaps reflecting more subjective distress and a desire to alleviate it.
Despite the overall average elevations and reductions in anger over time, it did significantly co-vary with heavy alcohol use, as hypothesized. However, the direction of this effect could not be determined in this study. It could be that individuals who drink more heavily and more frequently increase anger directly through the neurophysiological dysregulating impact on brain function (Fish et al., 2002), such as the amygdala (Wrase et al., 2008). Alternately, it may be indirectly related by incurring more personal and interpersonal conflicts related to drinking (Appelberg, 1993) and/or incurring more subjective frustration with their inability to control their drinking and related life circumstances. It could also be that anger leads to increased drinking in an attempt to self-regulate and mitigate the unpleasant subjective experience of anger (Gerard and Kornetsky, 1955; Khantzian, 1985), or it could be a dynamic, reciprocal process. We should note that, in addition to the controlled HLM analyses examining the effect of anger on later drinking, we also conducted analyses examining the effect of drinking on subsequent anger (not shown). Although, in both variations, a connection between the two variables was observed, a stronger connection was found when drinking predicted subsequent anger, suggesting that heavy drinking may exacerbate anger. However, experimental work is needed to clarify the exact nature and direction of this relationship.
As has been shown in prior research on this sample (e.g., Tonigan ., 2003), AA was significantly and independently related to better outcomes over time, irrespective of study arm, the initial treatment condition to which patients were assigned, or whether imputed or nonimputed data models were tested. However, the magnitude of the relationship between AA and subsequent alcohol use was not uniform, becoming stronger as the time since treatment increased. The observed relative increase in covariance over time between AA and alcohol use may be the result of the earlier protective effect of the MATCH treatments that helped offset potentially worse outcomes among non-AA attendees. Alternatively, the interaction could be the result for motivational self-selection, because clients who persisted longer in AA may have been those most strongly motivated to abstain and, therefore, who had better longer term outcomes. Self-selection is an inherent challenge in this type of research. However, our lagged analyses controlling for static and time-varying covariates and averaging effects across time help minimize such biases and strengthen causal conclusions.
Counter to predictions, we found that changes in anger were unrelated to the degree of AA attendance. This is in contrast to the explicit emphasis in AA literature on reducing anger and could be reflecting a reality that, despite the emphatic emphasis in the AA core literature on reducing anger, AA attendance itself does not in fact lead directly to reductions in anger. However, it may be that, although the levels of anger remain quite high, AA helps attendees improve their ability to successfully tolerate anger. Thus, although absolute levels are not changing in response to AA, attendees may improve in their ability to manage anger. Importantly, there are several aspects to anger, such as suppression versus immediate reactivity and appropriate (e.g., assertive communication) versus inappropriate expression (e.g., violent acting out or displacement). AA (1939, 2001) focuses more explicitly on problems with holding on to anger (i.e., "resentment"). Consequently, future research should investigate also the possibility that AA may actually lead to better outcomes by reducing "anger" if one were to use more specific measures of resentment. It may also be that specific AA program involvement (e.g., more targeted work on the 12 steps) will result in more marked anger attenuation. We did not find this to be so in our own analyses with a measure of AA involvement, but conclusions from those findings are limited by a large amount of missing data. Because most AA research has focused on AA attendance, the main focus here was to examine mediators of attendance effects. However, more detailed research regarding the effects of involvement is clearly needed.
Another explanation for the lack of support for this anger mediation hypothesis could be related to the timing of the assessment of anger relative to AA attendance and alcohol-use behavior. Also, given that the explicit AA emphasis on anger was based on AA as practiced in the late 1930s when membership was very small (AA, 1939, 2001), the lack of relationship between AA and anger could reflect more recent shifts in emphasis away from anger remediation with the initial, concentrated AA emphasis on anger becoming more diluted because the fellowship has expanded from less than 100 members into millions.
In conclusion, similar to prior research, our controlled, lagged HLM analyses based on multiply imputed, and nonimputed, data revealed AA attendance was consistently associated with better alcohol outcomes over time. We also found that patients higher in anger were more likely to engage with AA, and the pattern of results suggests that higher anger is associated with more harmful levels of alcohol use, although the exact nature of this relationship warrants further research. This study also found that AA attendance and AA involvement were consistently unrelated to changes in anger over time. Although support was not found for the notion that AA may improve drinking outcomes by reducing anger, there was strong convergence between AA's explicit emphasis on anger (AA, 1939, 2001) and our findings: Anger appears to be a serious and enduring problem among those suffering from alcohol dependence and is consistently related to heavy alcohol consumption. Measurement, sampling, or assessment time-frame factors may have contributed to the lack of association between AA and anger, but results here suggest that, although attending AA is related to better outcomes, AA alone may be generally insufficient to alleviate the suffering and alcohol-related risks specifically associated with anger.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants R21AA016762 (John F. Kelly, principal investigator) and K01 AA015137-04(Maria E. Pagano, principal investigator).
References
- Alcoholics Anonymous. Alcoholics Anonymous: The story of how thousands of men and women have recovered from alcoholism. 3rd ed. New York: Alcoholics Anonymous World Services; 1939. [Google Scholar]
- Alcoholics Anonymous. Twelve steps and twelve traditions. New York: Alcoholics Anonymous World Services; 1953. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous comes of age. New York: Alcoholics Anonymous World Services; 1957. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous: The story of how thousands of men and women have recovered from alcoholism. 4th ed. New York: Alcoholics Anonymous World Services; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., rev. Washington, DC: Author; 1987. [Google Scholar]
- Appelberg K. Alcohol consumption and smoking: Associations with interpersonal conflicts at work and with spouse among 13,869 Finnish employees. Addiction Research. 1993;1:257–267. [Google Scholar]
- Barnard J, Rubin DB. Miscellanea: Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- Cummings C, Gordon JR, Marlatt GA. Relapse: Prevention and prediction. In: Miller WR, editor. The addictive behaviors: Treatment of alcoholism, drug abuse, smoking, and obesity. Elmsford, NY: Pergamon Press; 1980. pp. 291–321. [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: What is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and alternatives. Piscataway, NJ: Rutgers Center of Alcohol Studies; 1993. pp. 41–76. [Google Scholar]
- Fish E, DeBold J, Miczek K. Repeated alcohol: Behavioral sensitization and alcohol-heightened aggression in mice. Psychopharmacology. 2002;160:39–48. doi: 10.1007/s00213-001-0934-9. [DOI] [PubMed] [Google Scholar]
- Forcehimes A, Tonigan J. Self-efficacy as a factor in abstinence from alcohol/other drug abuse: A meta-analysis. Alcoholism Treatment Quarterly. 2008;26(4):480–489. [Google Scholar]
- Gerard D, Kornetsky C. Adolescent opiate addiction: A study of control and addict subjects. Psychiatric Quarterly. 1955;29:457–486. doi: 10.1007/BF01567471. [DOI] [PubMed] [Google Scholar]
- Gilks WR, Richardson S, Spiegelhalter DJ, editors. Markov chain Monte Carlo in practice. New York: Chapman & Hall; 1996. [Google Scholar]
- Goodman AC, Holder HD, Nishiura E, Hankin JR. A discrete choice model of alcoholism treatment location. MedicalCare. 1992;30:1097–1109. doi: 10.1097/00005650-199212000-00003. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Circles of recovery: Self-help organizations for addictions. New York: Cambridge University Press; 2004. [Google Scholar]
- Judd CM, Kenny DA. Process analysis: Estimating mediation in treatment evaluations. Evaluation Review. 1981;5:602–619. [Google Scholar]
- Kadden R, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Hester R, editors. Cognitive-behavioral coping skills therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, Vol. 3, DHHS Publication No. (ADM) 92-1895. Washington, DC: Government Printing Office; 1992. [Google Scholar]
- Karno MP, Longabaugh R. Patient depressive symptoms and therapist focus on emotional material: A new look at Project MATCH. Journal of Studies on Alcohol. 2003;64:607–615. doi: 10.15288/jsa.2003.64.607. [DOI] [PubMed] [Google Scholar]
- Karno MP, Longabaugh R. Less directiveness by therapists improves drinking outcomes of reactant clients in alcoholism treatment. Journal of Consulting and Clinical Psychology. 2005;73:262–267. doi: 10.1037/0022-006X.73.2.262. [DOI] [PubMed] [Google Scholar]
- Kaskutas L, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly JF. Mutual-help for substance use disorders: History, effectiveness, knowledge gaps and research opportunities. Clinical Psychology Review. 2003;23:639–663. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addiction Research and Theory. 2009;17:236–259. [Google Scholar]
- Kelly JF, Yeterian JD. Mutual-help groups. In: O'Donohue W, Cunningham JR, editors. Evidence-based adjunctive treatments. New York: Elsevier; 2008. pp. 61–105. [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Joumal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Little RA, Rubin DB. Statistical analysis with missing data. 2nd ed. Hoboken: John Wiley & Sons; 2002. [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Mahwah, NJ: Lawrence Erlbaum; 2008. [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Determinants of relapse: Implications for the maintenance of behavior change. In: Davidson PO, Davidson SM, editors. Behavioral medicine: Changing health lifestyles. New York: Brunner/Mazel; 1980. pp. 410–452. [Google Scholar]
- Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- Martin P, Singleton C, Hiller-Sturmhofel S. The role of thia-mine deficiency in alcoholic brain disease. Alcohol Research & Health. 2003;27:134–142. [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Motivational interviewing: Research, practice, and puzzles. Addictive Behaviors. 1996;21:835–842. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca F. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;(Supplement No.12):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual for the Comprehensive Drinker Profile. Odessa, FL: Psychological Assessment Resources; 1984. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, Vol. 2, DDHS Publication No. (ADM) 92-1894. Washington, DC: Government Printing Office; 1992. [Google Scholar]
- Montgomery HA, Miller WR, Tonigan JS. Does Alcoholics Anonymous involvement predict treatment outcome? Journal of Substance Abuse Treatment. 1995;12:241–246. doi: 10.1016/0740-5472(95)00018-z. [DOI] [PubMed] [Google Scholar]
- Nock M. Conceptual and design essentials for evaluating mechanisms of change. Alcoholism: Clinical and Experimental Research. 2007;31(Suppl.No. 10):4S–12S. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve-step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIAAA Project MATCH Monograph Series, Vol. 1, DHHS Publication No. (ADM) 92–1893. Washington, DC: Government Printing Office; 1992. [Google Scholar]
- Project MATCH Research Group. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical Experimental Research. 1993;l7:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Rourke SB, Loberg T. The neurobehavioral correlates of alcoholism. In: Nixon SJ, editor. Neuropsychological assessment of neuropsychiatric disorders. 2nd ed. New York: Oxford University Press; 1996. pp. 423–485. [Google Scholar]
- Shaham Y, Shalev U, Lu L, de Wit H, Stewart J. The reinstatement model of drug relapse: History, methodology and major findings. Psychopharmacology. 2003;168:3–20. doi: 10.1007/s00213-002-1224-x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. In: Timeline follow-back: A technique for assessing self-reported alcohol consumption. Measuring alcohol consumption: Psychosocial and biochemical methods. Litten RZ, Allen JP, editors. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory: Professional manual (Research Edition) Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory: STAXI professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Spitzer R, Williams J. Proposed revisions in the DSM-III classification of anxiety disorders based on research and clinical experience. In: Tuma AH, Maser J, editors. Anxiety and the anxiety disorders. Mahwah, NJ: Lawrence Erlbaum; 1985. pp. 759–773. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001. [Google Scholar]
- Timko C, Finney J, Moos R, Moos B. The process of treatment selection among previously untreated help-seeking problem drinkers. Journal of Substance Abuse. 1993;5:203–220. doi: 10.1016/0899-3289(93)90064-i. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors G, Miller WR. The Alcoholic Anonymous Involvement Scale (AAI): Reliability and norms. Psychology of Addictive Behaviors. 1996:75–80. [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor T, Del Boca F, editors. Treatment matching in alcoholism. New York: Cambridge University Press; 2003. pp. 184–204. [Google Scholar]
- Waldron HB, Miller WR, Tonigan JS. Client anger as a predictor of differential response to treatment. In: Longabaugh R, Wirtz PW, editors. Project MATCH hypotheses: Results and causal chain analyses. Washington, DC: Government Printing Office; 2001. pp. 134–148. NIAAA Project MATCH Monograph Series, Vol. 8, NIH Publication No. 01–4238. [Google Scholar]
- Weiss RD, Griffin ML, Gallop RJ, Najavits LN, Frank A, Crits-Christoph P, Thase ME, Blaine J, Gastfriend D, Daley D, Luborsky L. The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence. 2005;77:177–184. doi: 10.1016/j.drugalcdep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Wrase J, Makris N, Braus DF, Mann K, Smolka MN, Kennedy DN, Heinz A. Amygdala volume associated with alcohol abuse relapse and craving. American Journal of Psychiatry. 2008;165:1179–1184. doi: 10.1176/appi.ajp.2008.07121877. [DOI] [PubMed] [Google Scholar]